Your Guide to AI in Healthcare
Discover how AI in healthcare is revolutionizing patient outcomes. This guide explores key applications, benefits, and how to implement medical AI.
When you hear "AI in healthcare," it’s easy to picture a scene from a science fiction film. But the reality on the ground is far more practical—and in many ways, more profound. AI isn't about replacing doctors; it's about giving them superpowers. Think of it as an incredibly powerful analytical tool that helps clinicians deliver faster, more accurate, and deeply personalised care to their patients.
The New Reality of AI in Medicine
Intelligent technology has firmly moved from the lab into the clinic, becoming a vital partner for medical professionals. The most helpful way to think about it is not as an autonomous robot surgeon, but as a tireless assistant that can sift through mountains of data—like medical images, patient records, and research papers—to find subtle patterns that the human eye might miss.
This shift is all about enhancing what medical experts already do best. The goal is a genuine partnership. In fact, the most successful AI tools come from a process of AI co creation, where doctors, nurses, and other specialists work directly with developers. This ensures the technology actually solves real-world problems and fits smoothly into the demanding day-to-day workflow of a hospital or clinic.
The Driving Force Behind AI Adoption
So, what’s fuelling this change? AI is gaining traction because it offers real answers to some of the biggest headaches in healthcare. It tackles everything from the endless paperwork that burns out clinicians to the slow pace of medical research.
Here are a few of the key drivers:
- Smarter Diagnostics: AI algorithms are proving to be exceptionally good at analysing medical images. Whether it's an X-ray, CT scan, or MRI, they can often spot the earliest signs of a disease with incredible accuracy, sometimes long before they'd be obvious to a human reviewer.
- Truly Personalised Treatment: By looking at a patient's unique genetic profile, lifestyle, and medical history, AI can help predict how they’ll respond to certain drugs or therapies. This moves us away from one-size-fits-all medicine toward highly individualised treatment plans that just work better.
- A More Efficient Clinic: AI is a game-changer for hospital administration. It can automate tedious but necessary tasks like scheduling appointments, managing records, and processing billing. This frees up precious time for doctors and nurses to do what they entered the profession for: caring for patients.
The momentum is undeniable, and the investment reflects that. In the Netherlands, for example, the AI in healthcare market is expected to rocket from $0.02 billion in 2022 to $0.36 billion by 2030. That’s a compound annual growth rate of 45.72%, driven by a top-tier healthcare system and strong government backing for innovation. You can dive deeper into the numbers with this detailed market analysis.
The real magic of AI in medicine isn't in its technical complexity. It's in its ability to deliver clear, actionable insights that empower clinicians to make better-informed decisions. It’s a force multiplier for human expertise, and that ultimately leads to better outcomes for patients. As we’ll see, this isn’t just a minor upgrade—it’s a fundamental shift in how we deliver healthcare.
How We Got Here: A Brief History of Medical AI
The sophisticated AI tools we see in healthcare today feel like a recent phenomenon, but they didn't just spring into existence. Their story is one of gradual evolution, starting decades ago with systems that were simple by today's standards but absolutely essential for getting us to where we are now. To really grasp what AI can do for medicine, it helps to understand where it came from.
The journey really kicks off in the 1970s with the first "expert systems." These weren't thinking machines in the way we imagine AI now. Think of them more like massive digital flowcharts built on "if-then" logic. A clinician would feed in patient symptoms, and the system would meticulously follow its programmed rules to suggest a possible diagnosis.
These early pioneers were foundational. The development of AI in healthcare has deep roots, with key milestones shaping the medical field across the globe, including here in the Netherlands. From the late 1970s, programs like the consultation system CASNET started helping physicians analyse disease data and consider treatment options. This was quickly followed by diagnostic aids like MYCIN, which helped identify bacterial pathogens, and INTERNIST-1. You can get a much fuller picture by exploring the early medical AI systems and their impact.
From Simple Rules to Learning Machines
The biggest drawback of these first-generation systems was obvious: they were rigid. They couldn't learn or adapt beyond their pre-written rules. The real game-changer was the emergence of machine learning, which finally gave systems the ability to improve themselves over time.
This monumental shift was powered by two crucial developments:
- A Flood of Data: As health records went digital, we suddenly had enormous datasets perfect for training algorithms.
- Serious Computing Muscle: Processors became powerful enough to actually analyse all that data efficiently.
One of the most significant breakthroughs came in 1986 with DXplain. This system allowed primary care physicians to enter a patient's symptoms and get back a ranked list of likely diagnoses. It started with a database of 500 diseases and eventually grew to over 2,400, proving that machine learning could scale in a way rule-based systems never could. These tools were no longer static; they could evolve.
The Modern Era of Medical AI
The most recent—and arguably most significant—turning point came with deep learning. As a branch of machine learning inspired by the neural networks in our own brains, this is the technology behind today's most incredible medical AI feats, from spotting subtle patterns in MRI scans to forecasting disease outbreaks.
You might remember when IBM's Watson won the game show Jeopardy! back in 2011. It was great television, but it was also a powerful demonstration. It showed that an AI could understand natural human language and search through vast amounts of messy, unstructured data to find a precise answer—a skill with obvious and direct applications in medicine.
This journey from simple rule-followers to complex learning networks shows that AI in healthcare isn't a sudden revolution. It’s the product of decades of patient, iterative work. Each new development has been built on the foundations of the last, taking us from the early days of MYCIN to the intelligent clinical tools we rely on today.
Practical AI Applications Changing Patient Care
AI in medicine is no longer just a futuristic concept whispered about in research labs. It has firmly moved from theory into the treatment room, working alongside clinicians every single day. The real power here isn't about replacing human expertise; it's about amplifying it, offering insights and a level of precision that was simply out of reach before.
Let's look at some of the most significant ways AI is already making a difference for patients and medical professionals. These real-world examples cut through the hype and show the tangible value AI brings to healthcare right now.
Medical Imaging and Earlier Diagnoses
One of the first and most successful fields for medical AI is in analysing images. Think of an AI model as an incredibly diligent assistant for a radiologist, one that has been trained on millions of scans. Its job? To spot patterns that might be too subtle or faint for the human eye to catch on a first pass.
These systems are brilliant at sifting through X-rays, CT scans, and MRIs to flag potential trouble spots with impressive accuracy. For example, certain AI algorithms can detect the earliest signs of lung cancer or diabetic retinopathy long before a patient would ever notice a symptom. This opens the door for much earlier treatment, which is often the single most important factor for a good outcome.
This isn't about building a machine that's 'smarter' than a doctor. It's about creating a collaborative tool. The AI draws the expert's attention to specific areas of concern, acting as a second set of eyes to ensure nothing gets missed and making the whole review process faster. This frees up radiologists to focus their deep expertise where it matters most, helping to reduce burnout and get through more cases.
Predictive Analytics for Proactive Care
Beyond just finding what’s already there, AI is also becoming a powerful tool for predicting what might happen next. By analysing enormous datasets—from electronic health records (EHRs) and genetic markers to lifestyle information—predictive models can pinpoint patients who are at high risk for conditions like heart failure or sepsis.
Imagine a hospital system that gets an alert flagging a patient who is very likely to be readmitted within 30 days of being discharged. With that knowledge, the care team can step in with preventative measures, like scheduling follow-up calls or arranging a home health visit. This proactive approach helps avoid another stressful and costly hospital stay. It's a fundamental shift from reactive to proactive care, and it's one of the core promises of AI in medicine. If you're looking to explore these ideas in your own organisation, our AI ideation workshop is a great place to start.
AI-Guided Robotic Surgery
Robotic-assisted surgery has been a staple in operating theatres for years, but adding AI into the mix elevates it to a whole new level of precision and control. AI algorithms can actively enhance a surgeon's natural abilities by stabilising tiny hand tremors, providing a real-time map of the patient's anatomy, and even automating some of the more repetitive surgical tasks.
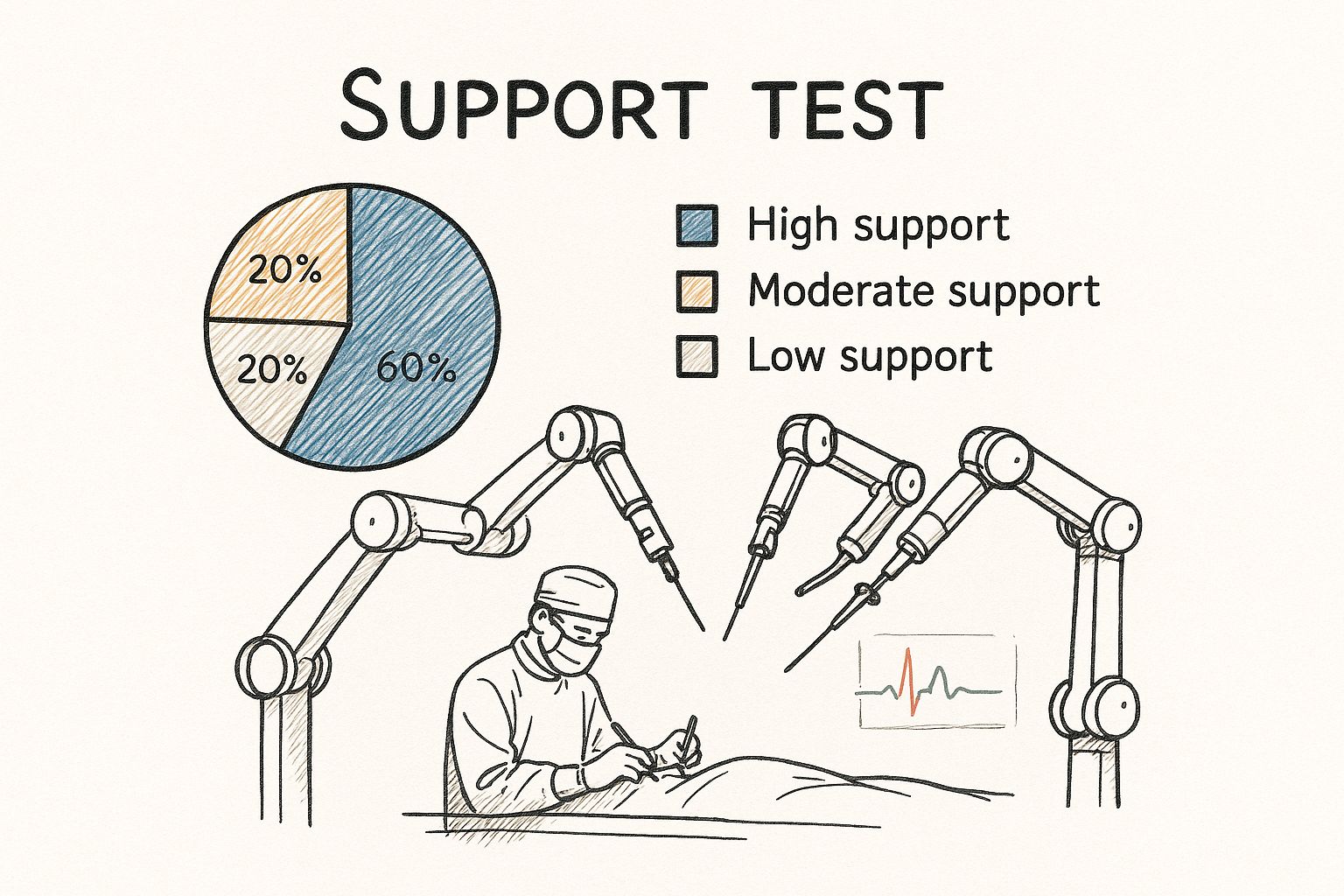
This incredible partnership between human skill and machine precision often leads to smaller incisions, less blood loss, and much quicker recovery times for patients. The AI essentially acts as a co-pilot, making sure every single movement is as steady and accurate as it can possibly be.
To give a clearer picture of how these applications fit into the broader medical world, the table below breaks down their functions and benefits across different fields.
Comparing AI Applications Across Healthcare Domains
| AI Application | Primary Function | Key Benefit | Impacted Medical Field |
|---|---|---|---|
| Medical Imaging Analysis | Detects anomalies in scans (X-rays, MRIs) | Earlier disease detection, improved accuracy | Radiology, Oncology, Ophthalmology |
| Predictive Analytics | Identifies at-risk patients from health data | Proactive care, reduced readmissions | Cardiology, Public Health, Hospital Admin |
| AI-Assisted Robotics | Enhances surgical precision and stability | Minimally invasive procedures, faster recovery | Surgery (multiple specialities) |
| Drug Discovery | Analyses biological data to find new treatments | Faster, cheaper drug development process | Pharmacology, Biotechnology |
This comparison highlights just how versatile AI has become. It's not a one-size-fits-all solution but a collection of specialised tools designed to solve specific challenges across the healthcare spectrum, from the lab to the operating theatre.
Navigating the Promise and Pitfalls of AI in Healthcare
Bringing AI into the world of healthcare is a massive undertaking, filled with both incredible promise and very real challenges. For any healthcare leader, a successful journey means looking at this technology with open eyes, understanding not just the shiny benefits but also the thorny problems that come with it.
The upside is undeniably powerful. We're already seeing AI systems make more accurate diagnoses than humans in areas like radiology and pathology. Think about the potential there. At the same time, these tools can take on the soul-crushing administrative tasks that contribute heavily to clinician burnout, giving doctors and nurses more time to do what they do best: care for patients. This one-two punch of better accuracy and improved efficiency points to a future of more personalised and effective medicine.
But getting there isn't as simple as installing new software. The path is littered with hurdles that need to be navigated with care. Honestly acknowledging these barriers is the first step to building an AI-powered healthcare system that truly works and earns our trust.
The Major Hurdles to Widespread AI Adoption
Rolling out AI in a clinical setting is far more than a technical challenge; it’s a deeply human one. The biggest obstacles usually boil down to three key areas.
- The Trust and Data Dilemma: Trust is the absolute foundation of medicine. For many patients—and even clinicians—the thought of a machine making life-or-death decisions is deeply unsettling. This anxiety is amplified by legitimate fears about data privacy. AI models are hungry for data, and that data is some of the most sensitive information a person has.
- The Danger of Algorithmic Bias: An AI model is a reflection of the data it learns from. If that data contains historical biases related to race, gender, or income, the AI will not only learn them but can make them even worse. This isn't just a theoretical problem; it could lead to AI tools that are less accurate for certain groups, creating a new layer of inequality in care.
- The Complex Regulatory Maze: Healthcare is, for very good reason, a minefield of regulations. AI adds a whole new layer of complexity that current rules weren't designed for. Organisations find themselves trying to comply with established laws like HIPAA and GDPR while simultaneously guessing what future AI-specific regulations will demand. It's a tough balancing act.
A recent report really puts this into perspective. It confirms AI’s huge potential for improving diagnostics and workflows but also shines a light on a major trust gap. Both patients and doctors are still wary, and that hesitation could significantly slow down how quickly these tools are adopted. You can discover more insights from the Philips Future Health Index to get a fuller picture.
Building Guardrails for Responsible Implementation
The answer to these challenges isn't to stop progress. It's to move forward with purpose and caution. That means putting strong governance and clear ethical lines in the sand before a single algorithm touches a patient's data.
This is where a solid AI strategy framework becomes non-negotiable. This isn’t just a tech document; it’s your organisation’s rulebook. It should clearly spell out your principles for fairness, accountability, and transparency, guiding how AI is chosen, tested, and ultimately used in the clinic.
Think of this framework as the guardrails on a winding mountain road. It gives healthcare leaders a structured way to implement AI that is not only powerful but also ethical and safe. It ensures that every new tool serves the ultimate mission of better patient care while actively managing the risks. By tackling bias, privacy, and trust head-on, organisations can build a solid foundation for using AI successfully for years to come.
Your Roadmap for AI Implementation
So, how do you go from simply understanding AI to actually putting it to work? It’s not about buying the flashiest new tool. A successful AI journey in any healthcare setting starts by zeroing in on a real, persistent problem—a clinical or operational headache that needs a solution.
This section is your practical playbook for turning AI’s potential into tangible results. It’s all about moving from the ‘what’ to the ‘how’.
The whole process hinges on a problem-first approach. Instead of asking, "What can we do with AI?", the right question is, "What's our biggest bottleneck, and could AI help us fix it?" This simple shift in thinking ensures every investment is tied directly to a measurable improvement, whether it’s in patient care or organisational efficiency.
From there, the journey unfolds in clear stages, from figuring out if your data is ready to launching small, focused pilot projects to prove the value. Taking it step by step helps to manage risk and, just as importantly, build genuine support among the clinicians and staff who will ultimately use the technology.
Stage 1: Start with a Specific Problem
Before a single line of code is written or any software is bought, you need to identify a very specific use case. What problem are you actually trying to solve? It could be anything from cutting down patient wait times in A&E to getting better at spotting sepsis on a particular ward. The trick is to be precise.
A vague goal like "improve diagnostics" is just too broad to be useful. A much better, more actionable goal is something like, "reduce the turnaround time for preliminary chest X-ray analysis by 40% using an AI co-pilot tool". This clarity gives you a concrete benchmark for success and keeps the entire project focused.
Stage 2: Conduct a Rigorous Readiness Assessment
Once you’ve nailed down the problem, it’s time to look inwards. Do you have the right ingredients for a successful AI project? This reality check should cover three main areas:
- Data Quality and Accessibility: AI models are hungry for data, but they’re picky eaters. They’re only as good as the data they’re trained on. You have to ask: do we have enough high-quality, relevant data? Is it structured and accessible enough for a model to actually use?
- Technical Infrastructure: Do you have the computing power, storage, and security protocols in place to handle an AI system? This isn’t just about servers; it's about making sure you can maintain full compliance with patient privacy regulations like the GDPR.
- Organisational Buy-In: This might be the most important piece of the puzzle. Are your clinicians, IT staff, and leadership all on the same page? Finding a few early champions who truly believe in the project's vision is essential for getting through the inevitable challenges that come with implementation.
The success of any AI initiative in healthcare hinges on a robust AI requirements analysis. This foundational step ensures the chosen solution aligns perfectly with existing clinical workflows and solves the right problem from the outset, preventing costly missteps down the line.
Stage 3: Launch a Focused Pilot Programme
With a clear problem and a solid readiness assessment, it's time to test the waters. A pilot programme is a small-scale, controlled trial of your AI solution in a real-world setting. The goal isn’t to overhaul the entire organisation overnight. It’s simply to prove the concept works and to measure its real impact.
Your pilot needs clear, measurable goals. For instance, you could track changes in diagnostic accuracy, the amount of time saved on administrative tasks, or direct improvements in patient outcomes. Documenting these results gives you the hard evidence you need to make the case for a wider rollout. Many expert teams, like our expert team, see this phase as critical for validating the approach before significant resources are committed.
Stage 4: Evaluate, Refine, and Scale
Once the pilot programme wraps up, the final stage is a thorough and honest evaluation. Did the AI tool actually meet its goals? Crucially, what was the feedback from the clinicians who used it day in and day out? This is the time for honest reflection and refinement.
Based on what you learn, you can make necessary tweaks to the technology or adjust the workflow before even thinking about a wider implementation. With a proven use case and a refined approach in hand, you can then move forward with confidence, scaling the solution to other departments or facilities. This iterative "test and learn" cycle is fundamental to long-term success, turning a promising pilot into a new standard of care.
Here is the rewritten section, crafted to sound human-written and natural.
What’s Next for AI in Medical Science?
When we look at what’s on the horizon for AI in healthcare, it’s clear the most exciting chapters are still being written. The progress we’ve seen so far has laid a solid foundation, but the next wave of innovation promises to go much deeper. We're moving beyond using AI for specific tasks and toward a future where it's a seamless, intelligent layer woven into the fabric of healthcare itself.
Think of it less as a tool and more as a trusted partner for medical professionals, reshaping everything from how we conduct research to how doctors interact with their patients.
Emerging Frontiers in Medical AI
Right now, a few key developments are bubbling up from research labs and are poised to become standard practice. These aren't just incremental improvements; they represent a fundamental shift in what's possible.
Generative AI for Ethical Research: Medical research often hits a wall when it comes to data. You need vast, diverse datasets to train powerful models, but patient privacy is paramount. Generative AI offers a brilliant way around this dilemma by creating high-quality synthetic data. This isn't real patient information, but it perfectly mimics the statistical patterns of real-world data, allowing researchers to explore rare diseases and test new hypotheses without ever accessing sensitive records.
Ambient Clinical Intelligence: Picture a doctor’s appointment where the physician’s full attention is on you, not the keyboard. This is the promise of ambient intelligence. AI-powered systems can listen in the background of a natural conversation, automatically drafting clinical notes, populating forms, and preparing orders. It’s a direct assault on the administrative overload that is a primary driver of clinician burnout.
Deep Integration with Genomics: For years, we've talked about the potential of personalised medicine—care tailored to your specific genetic code. AI is the engine that will finally make this happen at scale. By crunching enormous genomic datasets alongside clinical and lifestyle information, AI models can pinpoint disease risks with uncanny accuracy and recommend therapies that are truly customised to an individual. This is the path to hyper-personalised care.
This isn't just a story about better technology. It's about a new kind of partnership. AI is evolving into a collaborative force that amplifies human expertise at every step, from the lab bench to the patient bedside, reinforcing its role as an indispensable ally for clinicians, not a replacement.
Navigating this next chapter requires both a clear vision and deep expertise. If your organisation is ready to explore these future possibilities, connecting with our expert team can provide the guidance needed to turn these advanced concepts into a practical and impactful reality.
Your Questions About AI in Healthcare, Answered
As we've seen, bringing AI into the clinical world is exciting, but it also raises some very valid questions. Let's tackle a few of the most common ones that come up when people think about the practical side of AI in medicine.
Will AI Make Doctors and Nurses Obsolete?
Absolutely not. Think of AI as a highly specialised assistant, not a replacement. Its real strength lies in sifting through vast amounts of data—think medical images, lab results, and patient histories—to spot patterns that might be invisible to the human eye.
As we explored in our AI adoption guide, this doesn't replace a clinician's judgment. Instead, it takes over the more repetitive, data-heavy tasks. This frees up doctors and nurses to focus on what they're uniquely good at: critical thinking, patient interaction, and providing empathetic, person-to-person care. The best results always come from a partnership, a kind of AI co-creation where medical professionals and developers work hand-in-hand to build tools that truly help.
How Can We Trust AI with Sensitive Patient Data?
Protecting patient privacy is non-negotiable, and it’s the cornerstone of any successful AI initiative in healthcare. Organisations are bound by strict regulations like GDPR and HIPAA, which means implementing robust security from day one. This includes things like end-to-end encryption, tight access controls on who can see what, and frequent security checks. A solid AI strategy framework has data governance woven into its very fabric.
A fascinating technique called federated learning is a great example of this in action. It allows an AI model to learn from data right where it's stored—inside the hospital's secure system—without ever moving the sensitive information. The insights travel, but the data stays put, ensuring patient privacy is maintained while the AI still gets smarter.
What's the First Practical Step for a Hospital to Start with AI?
The first move isn't about buying fancy tech; it’s about having a clear plan. Start by pinpointing a single, specific challenge where AI could make a real difference. Maybe it's speeding up the diagnosis of a particular condition from scans or cutting down the paperwork that bogs down a specific department.
Conducting a thorough AI requirements analysis is essential here. You need to know exactly what you're trying to achieve before you build anything. The smartest approach is to launch a small pilot project. This lets you test the technology in a controlled way, measure its impact, and get your clinical staff on board by showing them real, tangible benefits. A specialised AI Strategy consulting tool can be a huge help in identifying that perfect starting point.
Ultimately, every successful implementation begins with thoughtful AI strategy consulting that connects the technology to clear clinical goals. This ensures your efforts are focused and lead to genuine improvements in patient care. The lessons and successes from these early projects, which can be presented as real-world use cases, become the foundation for all your future AI work.
If you need a hand mapping out your own AI journey, our expert team is here to help you build a clear and effective roadmap.
Ready to turn your AI ideas into scalable impact? Ekipa AI delivers tailored AI strategies and end-to-end execution, helping you uncover transformation opportunities without the costly consulting fees. Get your AI strategy in 24 hours.