Machine Learning in Healthcare: Transforming Patient Care
Explore how machine learning in healthcare improves outcomes, efficiency, and decision-making with real-world results and practical implementation tips.
When we talk about machine learning in healthcare, we're really talking about a specialized branch of AI where algorithms learn from vast amounts of medical data. Their goal? To find patterns and make predictions that can improve how we care for patients, all without someone having to write specific instructions for every single task.
Think of it as a brilliant assistant for doctors and researchers. It can sift through mountains of complex information—far more than a person could ever process—with incredible speed and accuracy. This capability is paving the way for major advances in diagnostics, personalized medicine, and even how hospitals run.
The AI Revolution Transforming Modern Medicine
Imagine a doctor facing a tough diagnosis. They're trying to connect the dots between thousands of data points for a single patient: lab results, imaging scans, genetic markers, and years of clinical notes. It’s an overwhelming task. This is where machine learning comes in, acting like a tireless and exceptionally well-read medical resident. It’s an algorithm that has, in a sense, studied millions of previous cases, allowing it to spot subtle clues that even a seasoned specialist might overlook. This isn't science fiction anymore; it’s happening right now, actively reshaping patient care.
The real power of machine learning in healthcare is its knack for turning overwhelming, often messy data into clear, actionable insights. For decades, medicine has been a goldmine of information. Now, thanks to powerful computers, we can finally start putting all that data to work.
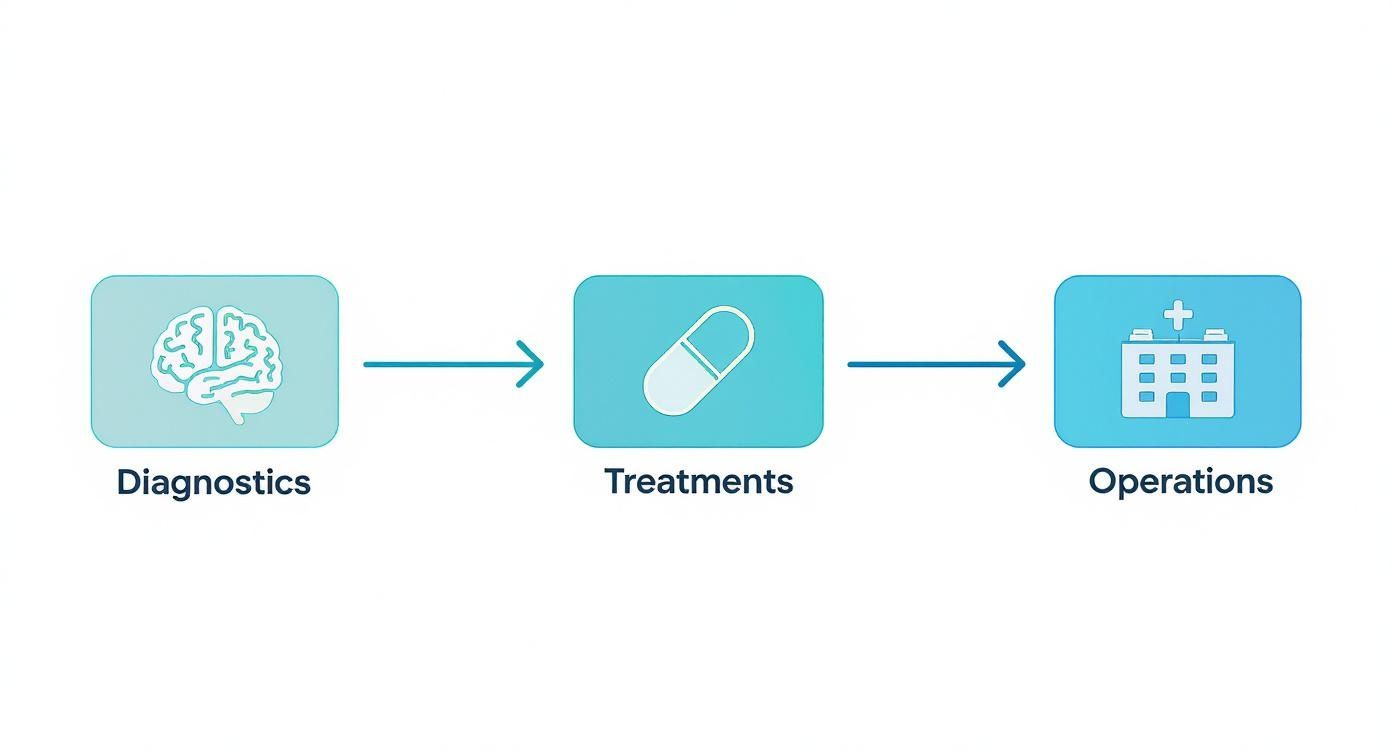
Redefining Patient Care and Operations
The influence of machine learning is being felt everywhere in the healthcare system. From the simple act of scheduling an appointment to creating a sophisticated, long-term treatment plan, ML models are making processes smoother and outcomes better. The applications are as diverse as they are powerful, fundamentally changing the day-to-day work of medical professionals and the experience of their patients.
A few key areas are already seeing major changes:
- Predictive Diagnostics: Algorithms can analyze MRIs, CT scans, and other medical images with stunning precision. In many cases, they can spot early signs of diseases like cancer long before the human eye can.
- Personalized Treatment: Instead of a one-size-fits-all approach, ML can analyze a patient’s genetic profile, lifestyle, and medical history to predict which treatments are most likely to work for them.
- Operational Efficiency: Hospitals are using ML to forecast patient admission rates, build better staff schedules, and automate routine administrative work. This frees up clinicians to spend more time where it matters most: with patients.
Machine learning is giving healthcare providers a new set of tools to address some of their oldest challenges: improving diagnostic accuracy, personalizing patient care, and making operations more efficient. It’s about augmenting human expertise, not replacing it.
Ultimately, bringing machine learning into the fold is about building a smarter, more responsive healthcare system. We dive deeper into these real-world uses in our guide on machine learning applications in the healthcare industry.
To give you a quick snapshot, here’s a look at where this technology is making the biggest impact.
Key Areas of ML Impact in Healthcare at a Glance
This table summarizes the primary domains within healthcare being transformed by machine learning, outlining the core function and primary benefit in each.
Domain Core ML Function Primary Benefit
Diagnostics
Pattern recognition in medical imaging and patient data.
Faster, more accurate disease detection and reduced diagnostic errors.
Treatment
Predicting patient responses to therapies based on unique data.
Highly personalized and effective treatment plans.
Hospital Operations
Forecasting patient flow and automating administrative tasks.
Improved resource management and significant cost savings.
As you can see, the applications are practical and directly address some of the most pressing challenges in the medical field today.
How Machine Learning Works in a Clinical Context
To really get a feel for machine learning in healthcare, it helps to step back from the complex math and look at how a model actually functions in a real hospital or clinic. Imagine you're training a new medical resident, but this one can digest millions of patient charts in the time it takes to sip your coffee. It all starts with data—and lots of it.
This information is pulled from everywhere: Electronic Health Records (EHRs), detailed medical images like MRIs and CT scans, genomic data, and even the unstructured notes doctors type up after an appointment. An ML model is then "trained" on this massive dataset. For instance, an algorithm could be fed thousands of retinal scans, some from patients with diabetic retinopathy and others from healthy individuals.
By sifting through all these examples, the model starts to pick up on the subtle patterns linked to the disease. It learns which specific pixels, shapes, and textures are red flags, much like how a veteran radiologist builds an intuitive sense of what to look for over a long career.
This graphic breaks down the typical workflow, showing how ML can touch everything from the first diagnosis to making the hospital run smoother.
As you can see, these models aren't just one-trick ponies. They can be woven into multiple points of a patient's journey, helping to spot diseases early and fine-tune how care is delivered.
The Different Learning Styles of AI
Just like people, not all machine learning models learn the same way. In healthcare, the two most common approaches are supervised and unsupervised learning, and each is built for a different kind of problem.
Supervised learning is a lot like studying with flashcards. You give the model a dataset where the answers are already known—for example, a pile of patient records clearly labeled with whether they were readmitted to the hospital within 30 days. The algorithm’s job is to figure out the relationship between the patient's data (vitals, lab work, medical history) and that known outcome.
- A Real-World Example: A hospital could use a supervised model to predict which patients are most likely to get an infection after surgery. By learning from thousands of past cases, the model can flag at-risk individuals so clinical staff can give them extra attention.
Unsupervised learning is a completely different beast. Think of it as being handed a mountain of unlabeled research papers and told to find the hidden connections. The data has no predefined labels, so the model has to explore it and find its own patterns and groupings.
- A Real-World Example: Researchers could use an unsupervised model to comb through genetic data from thousands of patients. The model might discover entirely new subgroups of a disease that nobody knew existed, potentially leading to breakthroughs in personalized medicine because those subgroups might need different treatments.
Understanding these fundamentals is key. It helps you see how technologies like AI voice recognition in healthcare can fit into the bigger picture, ultimately supporting the experts on the front lines.
From Training to Clinical Decision Support
Once a model is properly trained and tested to make sure it's accurate, it's ready to be integrated into a clinical workflow. It’s important to remember that it doesn't replace the doctor. Instead, it acts as a highly skilled assistant.
It might analyze a patient's X-ray and highlight a few spots that look suspicious, prompting the radiologist to take a closer look. It’s essentially a built-in second opinion.
The goal isn't to create an "AI doctor." It's to build a collaborative system where human expertise is backed by the raw analytical power of machine learning. This partnership helps clinicians make more confident decisions, which ultimately leads to better patient outcomes.
Putting these tools into practice is where the rubber meets the road. A clear, strategic plan is the only way to succeed. The result is a smarter, more efficient healthcare system that’s powered by the insights hidden in its own data.
So, Where is Machine Learning Actually Making a Difference in Healthcare?
Alright, we’ve covered the "how." Now for the exciting part: where is this technology actually being used? The real power of machine learning in healthcare isn't just theory; it’s happening right now in hospitals and clinics, making a tangible difference in patient lives and day-to-day operations. These aren't far-off dreams—they're real-world use cases that are actively reshaping the industry.
And the growth is explosive. The global AI in healthcare market was valued at $11 billion back in 2021. By 2030, it’s projected to hit a staggering $187 billion. That’s not just hype; it signals a seismic shift in how we approach diagnostics, patient care, and the business of medicine. Doctors are getting on board, too. A 2025 survey showed that 66% of physicians now use AI tools, a huge leap from just 38% in 2023. You can read more about this global shift in an in-depth analysis from the World Economic Forum.
Let's look at seven key areas where machine learning is already changing the game.
1. Diagnostic Imaging and Radiology
One of the first and most powerful applications of ML has been in reading medical images. Think about it: radiologists spend decades training their eyes to spot tiny, almost invisible anomalies in X-rays, MRIs, and CT scans. But the sheer volume of images they have to review is immense, which can lead to fatigue. Plus, some patterns are just too subtle for the human eye to consistently catch.
This is where machine learning shines. Models trained on millions of labeled scans can analyze images with incredible speed and accuracy.
- The Problem: An early-stage tumor might just look like a faint shadow, easily overlooked during a busy day of reviewing hundreds of scans.
- The Solution: An ML algorithm can pre-screen these images, flagging any suspicious areas for the radiologist to review more closely. It’s like having a tireless assistant who never gets distracted, catching potential issues that might otherwise be missed. This allows for earlier detection, which is often the key to successful treatment.
This technology doesn't replace the radiologist—it supercharges their abilities. We’ve even explored this ourselves with projects like our proof-of-concept AI for medical imaging, Diagnoo, which shows just how much these tools can boost a clinician's accuracy.
2. Predictive Analytics for Disease Outbreaks
Remember the early days of a pandemic? The chaos, the uncertainty? Predictive analytics aims to get ahead of that. By sifting through massive datasets—hospital admission rates, social media chatter, flight patterns, and more—ML models can spot the faint signals of an impending outbreak long before it becomes a crisis.
By spotting anomalies and predicting transmission routes, machine learning gives public health officials a crucial head start, allowing them to allocate resources, issue warnings, and implement preventive measures before a crisis escalates.
It’s about shifting from a reactive stance to a proactive one, which can save countless lives and prevent healthcare systems from being overwhelmed.
3. Personalized Treatment Plans
For too long, medicine has relied on a "one-size-fits-all" approach. But we know that’s not how our bodies work. Precision medicine, powered by machine learning, is changing that by tailoring treatments to a person's unique genetic code, lifestyle, and medical history.
Imagine an oncologist trying to choose the right chemotherapy. An ML algorithm can analyze the patient’s genomic data, past treatment responses, and other health records to predict which drug regimen is most likely to be effective. This not only improves the odds of success but also helps minimize debilitating side effects. It’s a foundational part of modern healthcare software development, turning patient data into smarter, more personal care.
4. Drug Discovery and Development
Getting a new drug from a lab to a pharmacy is a brutal, decade-plus process that can cost billions. Machine learning is starting to chip away at that timeline and cost. Here’s how:
- Finding Good Starting Points: Instead of years of trial and error, ML can analyze biological data to quickly identify proteins and compounds that are promising drug targets.
- Predicting Success (or Failure): Algorithms can simulate how a potential drug might behave in the human body, helping scientists weed out duds before they sink millions into failed clinical trials.
- Smarter Clinical Trials: ML can even help find the right patients for a trial by quickly sifting through health records to identify people who meet the specific criteria, speeding up recruitment.
5. Administrative Workflow Automation
Let’s be honest—so much of a doctor’s or nurse’s time is eaten up by paperwork. Billing, coding, scheduling, updating records... it's a mountain of administrative work that pulls them away from patients.
AI-powered workflow automation is the answer. ML models can handle these tedious but essential tasks. Think about automatically transcribing a doctor's spoken notes, processing insurance claims without human intervention, or optimizing clinic schedules to cut down on patient wait times. For instance, innovative medical transcription solutions are making clinical documentation faster and far more accurate. Every minute saved on paperwork is a minute that can be spent on patient care.
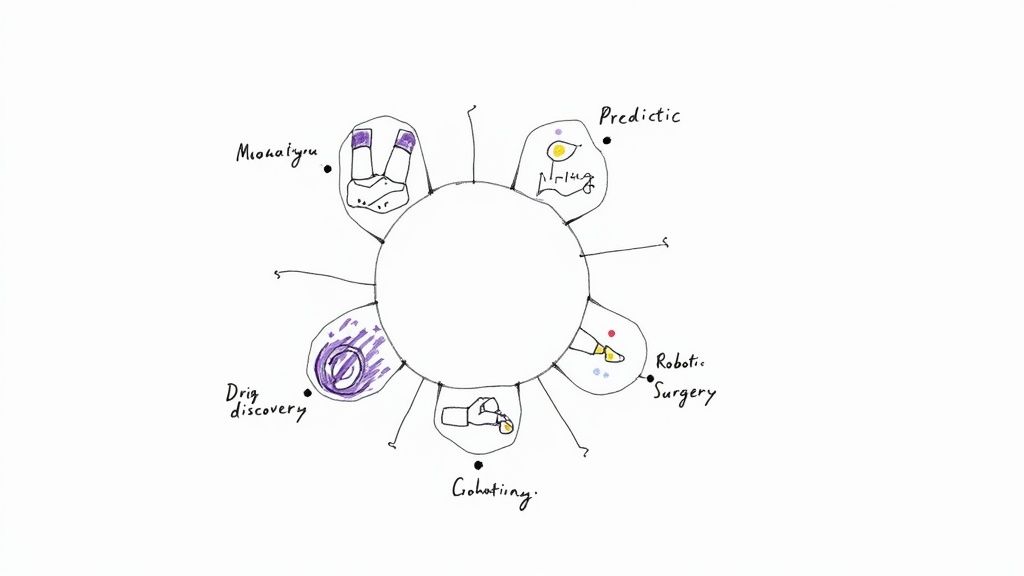
6. Robotic-Assisted Surgery
Precision is everything in an operating room. AI-guided robotic systems are now extending a surgeon's skill, allowing for movements that are steadier and more precise than the human hand alone. These systems can eliminate natural tremors and give the surgeon a magnified, 3D view of the surgical area.
Better yet, ML algorithms can analyze data from thousands of previous surgeries to provide real-time feedback and guidance during a procedure. The result? Less invasive surgeries, faster recovery times, and better outcomes for patients. Building these complex systems requires a rigorous approach, which is why following a proven AI Product Development Workflow is absolutely critical for safety and success.
7. Mental Health Monitoring and Support
Mental healthcare is another area where ML is making a real difference. Not everyone has immediate access to a therapist, but an AI-powered chatbot can offer a first line of support for people struggling with anxiety or depression.
Beyond chatbots, machine learning models are being developed to analyze a person's speech patterns, written text, or even facial expressions to detect subtle changes that might indicate mental distress. This could allow for much earlier intervention, providing help long before a person reaches a crisis point.
Seeing the Real-World Impact of AI
While the possibilities of machine learning in healthcare are exciting, what really matters are the tangible results. Bringing these technologies into a hospital or clinic isn’t just about being modern—it’s about seeing clear, measurable improvements. The gains really boil down to three main areas: better patient outcomes, smoother operations, and serious cost savings.
These aren't just buzzwords. They represent real changes that justify the investment in advanced AI Solutions. Let's look at how this actually works on the ground, in both the exam room and the back office.
Better Patient Outcomes
The most important benefit, without a doubt, is the direct effect on patient health. When you give clinicians better tools and deeper insights, you get faster, more accurate diagnoses. This leads to treatment plans that are truly tailored to the individual, which can completely change their prognosis for the better.
Think back to diagnostic imaging. An AI algorithm can pick up on faint patterns in a scan that the human eye might miss, helping to catch diseases like cancer earlier. And we all know that early detection is often the key to successful treatment. It goes further than that, though. By looking at a patient's specific genetic markers and health history, ML models can help doctors pinpoint the therapy most likely to work, cutting down on the exhausting and often discouraging trial-and-error process.
Smoother Day-to-Day Operations
Hospitals are incredibly complex places. The administrative workload can easily bog down doctors and nurses, pulling them away from their primary job. This is where machine learning can make a huge difference by automating routine tasks and taking the friction out of daily processes.
Well-designed internal tooling driven by AI can untangle a lot of common administrative knots. For instance:
- Smarter Scheduling: AI can optimize appointment and surgery schedules to cut down on wait times and make sure rooms and equipment are used effectively.
- Effortless Documentation: It can transcribe a doctor's spoken notes into a patient's record automatically, making sure the information is accurate without tedious typing.
- Predictive Staffing: By forecasting patient flow, hospitals can make sure they have the right number of staff on hand, preventing burnout from understaffing or waste from overstaffing.
By putting smart workflow automation in place, healthcare organizations simply run better. It leads to less stress for the staff and a much better experience for everyone who walks through the door.
The real goal here is to get the administrative clutter out of the way. When AI handles the repetitive tasks, clinicians can focus 100% of their skill and attention on what they do best: taking care of patients.
Big Savings on the Bottom Line
The third piece of the puzzle—cost reduction—often flows directly from the first two. When patients get better faster and operations are more efficient, you naturally spend less. But machine learning also creates savings in other, more direct ways.
Preventive care is a perfect example. Predictive models can identify patients who are at high risk for developing chronic conditions like diabetes or heart disease. This allows for early intervention, which can head off the need for far more expensive treatments down the road.
The financial numbers are compelling. By 2025, it's estimated that AI and machine learning will help trim global healthcare costs by $13 billion. AI-powered chatbots alone are on track to save the industry $3.6 billion in 2025, simply by handling initial patient questions in 42% of major healthcare networks. This potential is what's fueling investment; AI-focused digital health startups pulled in 40% of all digital health funding in the first quarter of 2024. You can discover more insights about these AI healthcare trends to see the full picture.
These figures build a powerful business case for services like AI Automation as a Service. They prove that a solid AI strategy consulting engagement is more than just a tech upgrade—it's a smart financial and operational decision.
Let's Be Realistic: The Hurdles of AI in Healthcare
While the promise of AI in medicine is enormous, getting there isn't as simple as flipping a switch. Bringing machine learning into the real world of patient care is a complex journey, filled with serious obstacles that demand more than just technical know-how.
To build a system that clinicians trust and patients benefit from, you have to tackle these challenges head-on. It’s a balancing act between pushing for innovation and upholding the core responsibilities of medicine. From safeguarding deeply personal patient data to rooting out bias in algorithms, every step is a minefield of complexity.
Data Privacy and Security Are Non-Negotiable
In healthcare, we’re not just talking about data; we're talking about people's lives and their most private information. Regulations like the Health Insurance Portability and Accountability Act (HIPAA) are the absolute baseline for protecting patients, and any AI system has to meet these standards without compromise. The real trick is figuring out how to feed AI models the massive datasets they need to learn without exposing a single patient's identity.
This calls for rock-solid data governance from the very beginning. Techniques like data anonymization are a start, but forward-thinking approaches like federated learning—where the AI model trains on data locally at different hospitals without ever pooling it—are becoming critical. A data breach isn't just a technical glitch; it's a catastrophic breakdown of trust that can damage a hospital's reputation for years.
The Hidden Danger of Algorithmic Bias
One of the most insidious risks in machine learning in healthcare is algorithmic bias. An AI model is a mirror; it only reflects the data it was trained on. If that data is skewed—say, it mostly comes from one demographic—the model will inevitably be less accurate for everyone else. This isn't just a technical flaw; it can actively worsen the health disparities we already struggle with.
For instance, an algorithm trained primarily on images of skin cancer from fair-skinned patients could easily miss the same cancer on darker skin. This isn’t a hypothetical problem. It’s a real, life-or-death issue that demands our full attention.
The only way to fight this is by deliberately training models on diverse, representative datasets. It also means we have to constantly audit our algorithms to see how they perform across different patient groups. This commitment to fairness is a cornerstone of any responsible AI strategy consulting that’s worth its salt.
Untangling the Web of Regulations and Ethics
The rulebook for AI in healthcare is still being written. Getting an AI-powered diagnostic tool approved by a body like the FDA is a grueling, high-stakes marathon. But even beyond the official regulations, we have to grapple with thorny ethical questions. If an AI makes a mistake, who’s responsible? How do we make sure technology enhances—not replaces—the human connection at the heart of patient care?
We're already seeing machine learning jump from the lab to the clinic. Healthcare is actually leading the pack in AI adoption, with 27% of U.S. health systems using domain-specific AI tools, a figure that dwarfs the 9% adoption rate across the wider economy. But this progress is patchy. AI is working wonders for administrative tasks, but its use in clinical areas like risk prediction and medical imaging is getting a more mixed reception. There's still a healthy dose of skepticism about whether these tools are truly reliable when it matters most. You can learn more about these healthcare AI adoption findings to get a better sense of where things stand.
The Practical Headaches: Cost and Technical Debt
Finally, there are the nuts-and-bolts challenges. Many hospitals are running on legacy IT systems that were never designed for the kind of data onslaught that machine learning requires. Trying to bolt a sophisticated AI platform onto an outdated infrastructure is often a technical nightmare—and an incredibly expensive one.
The upfront investment in talent, technology, and training is significant. That's why having a crystal-clear business case and a phased rollout plan is absolutely essential. Kicking things off with a well-defined pilot project can prove the value of the technology, build crucial buy-in from staff, and ensure that every dollar spent delivers a real return.
Your 5-Step Roadmap to Implementing Machine Learning
Knowing what machine learning can do is one thing; actually putting it to work in a clinical setting is another challenge entirely. Jumping in without a clear plan is a recipe for wasted resources and projects that never get off the ground, as we explored in our AI adoption guide.
This strategic roadmap lays out a practical, five-stage process. It's designed to help you build momentum, prove value early, and avoid common pitfalls along the way.
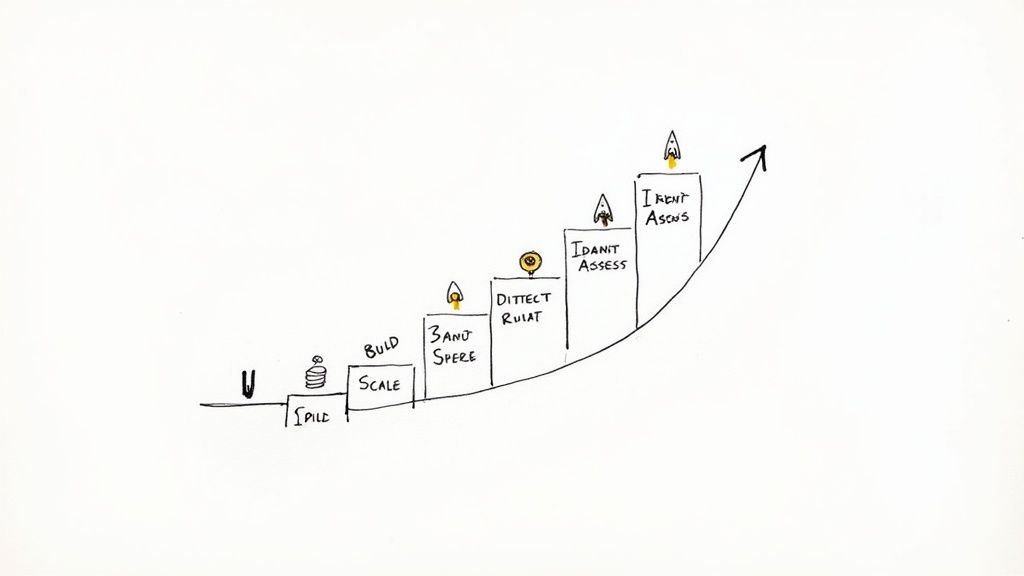
A Framework for Real-World Success
Think of this as a blueprint for moving from a promising idea to a scalable solution that makes a real impact. Each step logically builds on the one before it.
- Pinpoint a High-Impact Problem
- Don't try to boil the ocean. Instead of a vague goal like "improving diagnostics," get specific. Zero in on a known bottleneck, like reducing the high rate of false positives in mammogram screenings or automating the tedious process of filling out patient intake forms. The best starting points are always clear, measurable pain points.
- Get Real About Your Data
- An ML model is only as smart as the data it’s trained on. Period. Take a hard look at the quality, accessibility, and security of your data sources. Do you have a clean, well-structured dataset that's directly relevant to the problem you just identified? This step is absolutely fundamental—getting it wrong can derail the entire project.
- Build or Bring In the Right Expertise
- You need people who know what they're doing. This could mean upskilling your current IT staff, hiring dedicated data scientists, or partnering with an outside firm that specializes in healthcare AI. Working with an experienced partner can give you the skills you need right away, sidestepping the long and competitive hiring process.
- Run a Pilot Project
- Before you go all-in on a system-wide rollout, test your solution in a controlled environment. A pilot project is your chance to validate the model's accuracy, get crucial feedback from clinicians who will actually use it, and build a rock-solid business case for wider adoption.
A successful pilot is your single best tool for getting buy-in from leadership and other stakeholders. It transforms abstract potential into tangible proof, making it much easier to secure the budget and support needed for the next phase.
- Scale Up—But Do It Responsibly
- Once your pilot has proven its worth, you can start the process of scaling the solution. This means carefully integrating the model into existing clinical workflows and, just as importantly, monitoring its performance relentlessly to ensure it stays accurate, reliable, and fair over time. A well-defined implementation support process is essential for navigating this final, critical phase.
This roadmap gives you a clear path forward. By following these steps, you can move from theory to practice with confidence.
FAQs on Machine Learning in Healthcare
As machine learning finds its footing in healthcare, it's sparking a lot of questions. How does it work? What does it mean for patients? What are the real-world limits? Let's clear up some of the most common ones.
Is Machine Learning the Same as AI in a Hospital?
Think of Artificial Intelligence as the big picture—the whole field of building smart machines that can think or act like humans. Machine learning is a crucial part of that picture. It's the specific technique that allows a system to learn from data and make predictions without being explicitly told what to do for every single situation.
So, in a hospital, the broad idea of a "smart diagnostic tool" is AI. But the engine that makes it smart—the algorithm that has analyzed thousands of scans to learn how to spot the faint signs of a tumor—that's machine learning. It's the practical application that brings broader AI Solutions to life.
What's the Biggest Ethical Hurdle with Using ML for Diagnosis?
The single biggest concern is algorithmic bias. If a machine learning model is trained on data that mostly comes from one demographic, it might not work as well for others. This can happen if the training data isn't diverse enough to reflect the entire patient population.
The result? The model could be less accurate for underrepresented groups, accidentally making existing health inequities even worse. Tackling this means being incredibly deliberate about fairness, from gathering diverse data to constantly monitoring the model after it's deployed. This is a non-negotiable part of any responsible AI strategy consulting.
Can a Small Local Clinic Actually Use Machine Learning?
Absolutely. You don't need to be a massive hospital network to see the benefits. While large-scale diagnostic AI can be expensive, many cloud-based AI tools for business are now affordable and accessible. A small clinic doesn't need its own army of data scientists.
Here’s how they can get started:
- Automating the Front Desk: Using ML to streamline appointment scheduling and handle billing.
- Running a Tighter Ship: Optimizing everything from medical supply inventory to staff schedules.
- Smarter Screening: Using simple tools to perform a first pass on data before a human expert takes over.
These kinds of practical uses help smaller practices improve how they operate and deliver care. It proves machine learning has a place everywhere, not just in major medical centers.
Figuring out where to start can feel overwhelming, but you don't have to do it alone. A quick chat with our expert team can help chart a clear course for bringing these powerful tools into your organization, no matter its size.
At Ekipa AI, we specialize in turning healthcare challenges into AI-powered opportunities. Our platform is designed to help you build and execute an AI strategy that delivers real, scalable impact. From initial strategy to hands-on implementation, our expert team is here to guide you.