AI in Healthcare Strategy: A Practical Guide to Impact
AI in Healthcare Strategy: Master practical steps to identify use cases, protect data privacy, drive change, and scale AI for real results.
Having a solid AI in healthcare strategy isn't just a nice-to-have anymore; it's essential for staying relevant and leading the pack. We're talking about moving beyond scattered, experimental AI projects and creating a formal plan that truly drives better clinical outcomes and operational efficiency.
Why a Cohesive AI Strategy Is Non-Negotiable
Staring down the immense potential of AI in healthcare can feel like trying to boil the ocean. It’s a lot to take in, but sitting on the sidelines is the biggest risk you can take. This isn’t just about buying new software; it's about fundamentally rethinking how your organization will operate and compete in a field that's changing by the day.
A formal AI in healthcare strategy is your roadmap. It’s what turns abstract ideas into real-world results.
Without a clear plan, you'll likely end up with a collection of isolated pilot projects that show a little promise but never scale up or deliver a meaningful return on investment. A good strategy, on the other hand, ensures every AI initiative—from a small chatbot pilot to a major diagnostic tool—is directly tied to your core goals, whether that's improving patient outcomes, cutting administrative costs, or making better use of your resources.
Moving Beyond Random Acts of AI
The real magic happens when you connect your vision to measurable impact. This means recognizing that successful AI adoption is just as much about your people and processes as it is about the algorithms themselves. When you understand the full scope of using AI in healthcare to boost patient care and efficiency, it becomes crystal clear why a well-defined plan is so critical right now. Think of it as the blueprint for putting powerful AI solutions to work for you.
The healthcare and life sciences sector is already miles ahead of most other industries. Recent data paints a clear picture:
In a wide-ranging survey of over 600 professionals, a staggering 94% reported they are either actively using, piloting, or assessing AI. That level of engagement blows the 50% average AI adoption rate across other industries out of the water.
This isn't just about tinkering, either. The same report found that 81% of these organizations say AI has already helped increase revenue, and nearly half saw a return on their investment within the first year.
The Strategic Imperative
This isn't just a trend; it's a fundamental shift in the competitive landscape. Organizations that are deliberate and strategic with their AI investments are pulling ahead, while those treating it as a side project risk falling behind. As we've seen time and again, a successful journey in the healthcare industry demands careful, thoughtful planning from day one.
To help frame this journey, we've broken down the core components of a successful strategy into a clear, actionable framework. These pillars represent the foundational elements you'll need to get right to build a sustainable and impactful AI program.
Key Pillars of a Successful Healthcare AI Strategy
| Pillar | Objective | Key Considerations |
|---|---|---|
| Problem Identification | Pinpoint high-value use cases that align with strategic goals and offer tangible ROI. | Focus on clinical bottlenecks, administrative waste, or patient experience gaps. Start small and targeted. |
| Data Governance & Privacy | Establish a secure, compliant, and accessible data infrastructure to fuel AI models. | Prioritize PHI/PII protection, data quality, interoperability, and clear access protocols. |
| Clinical & Operational Validation | Rigorously test and validate AI solutions to ensure they are safe, effective, and fit for purpose. | Involve clinicians early and often. Define clear success metrics and conduct phased pilots. |
| Technology & Vendor Selection | Choose the right tools, platforms, or partners that fit your technical ecosystem and goals. | Evaluate build vs. buy options, scalability, integration capabilities, and vendor support. |
| Change Management & Adoption | Prepare your people and processes for AI-driven workflows to ensure successful integration. | Focus on communication, training, workflow redesign, and addressing staff concerns proactively. |
| Scaling & Continuous Improvement | Develop a roadmap for scaling successful pilots and continuously measuring performance. | Establish a governance committee, monitor KPIs, and create a feedback loop for ongoing optimization. |
Each of these pillars is a critical piece of the puzzle. Throughout this guide, we will dive deep into each one, offering practical steps and real-world examples to help you build a strategy that delivers.
Ultimately, a strong strategy is the difference between simply dabbling in new technology and truly transforming your organization. It ensures your AI investments are targeted, scalable, and directly support your core mission of providing exceptional care.
Identifying and Prioritizing High-Impact AI Use Cases
Jumping into an AI in healthcare strategy without a clear target is like prescribing treatment without a diagnosis. You wouldn't do it. Instead of getting distracted by every shiny new AI tool that makes headlines, the smart move is to look inward first. You need to pinpoint the exact problems that are crying out for a solution within your own walls.
The best place to start is with a deep-dive audit of your clinical and administrative workflows. Where are the real points of friction? The only way to find out is to talk to your people on the front lines—the nurses, physicians, and admins who live these processes every single day. They’ll tell you where the true bottlenecks are, whether it’s the mind-numbing hours wasted on prior authorizations or the diagnostic delays stacking up in an overloaded imaging department.
Finding the Right Starting Point
Once you've got a list of potential pain points, the real work begins: prioritization. Let's be honest, not all use cases are created equal. Some promise massive clinical breakthroughs but come with a heavy technical lift. Others can deliver quick financial wins with a relatively straightforward implementation.
This is where a simple prioritization matrix becomes your best friend. It helps you cut through the noise and balance competing factors.
Start by scoring each potential project against these core criteria:
Clinical Impact: How much will this genuinely improve patient outcomes, safety, or quality of care? (Think High/Medium/Low)
Financial ROI: What’s the real potential for cost savings or new revenue? (High/Medium/Low)
Technical Feasibility: Do we actually have the data, infrastructure, and skills to pull this off? (High/Medium/Low)
Implementation Speed: How fast can we get a pilot running and see tangible results? (Fast/Moderate/Slow)
This simple framework helps you shift from a sprawling wish list to a focused shortlist of "quick wins." These are the projects that are not only doable but also highly visible. They’re perfect for building momentum and getting crucial buy-in from stakeholders for your bigger AI vision.
This alignment of goals with operational gaps is the bedrock of any AI initiative that actually succeeds.
As you can see, successful AI isn't a magic button you press. It’s a structured process that starts long before a single line of code is written.
Comparing Real-World Scenarios
Let's make this less abstract. Picture your leadership team weighing two potential AI projects, which you can explore in more detail through our library of real-world use cases:
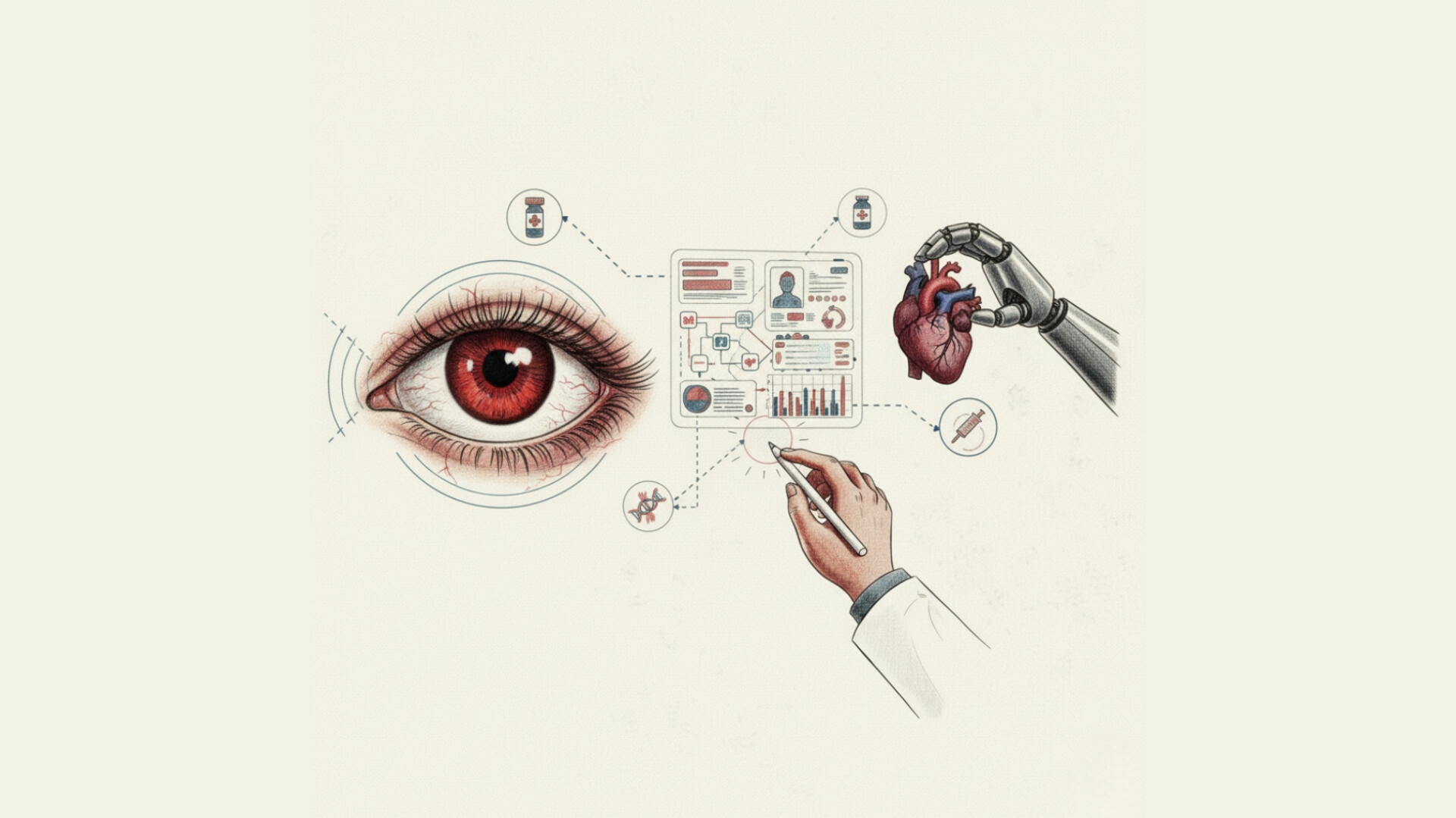
AI-Powered Diagnostic Imaging: A tool designed to help radiologists spot early-stage cancers with greater accuracy. The clinical impact? Potentially enormous. But the technical hurdles—requiring massive, pristine datasets and a lengthy clinical validation process—could be significant.
AI for Patient Scheduling Optimization: An algorithm that predicts no-shows and intelligently optimizes appointment slots. The goal is to slash wait times and fill every available slot. The direct clinical impact is more modest, but the financial ROI and speed to deployment are huge.
For an organization just starting its AI journey, the scheduling tool is often the smarter first move. It tackles a clear, nagging administrative problem, proves its value quickly, and builds confidence across the board. This initial success then paves the way for taking on those more ambitious clinical projects down the road.
For instance, a dedicated solution like the Clinic AI Assistant is built to automate these exact scheduling and administrative tasks, making it a perfect low-risk, high-reward starting point.
One of the biggest lessons from early adopters like HCA Healthcare is AI's power to reduce variance in care. By identifying what works best and standardizing it, AI doesn't just bump up the averages—it elevates the quality of care for everyone, ensuring every patient gets the benefit of the highest standard.
Formalizing Your Requirements
Once you've zeroed in on a high-potential use case, it’s time to get specific. You need to clearly define what success actually looks like on paper. This means documenting the project’s requirements, desired outcomes, and the key performance indicators (KPIs) you'll use to measure its impact. A thorough AI requirements analysis is critical at this stage to prevent scope creep and ensure alignment.
By starting with high-impact, achievable projects, your AI in healthcare strategy becomes a self-funding engine for innovation. Each success builds the business case for the next one, ensuring your investments deliver real, measurable value from day one.
Building Your Data and Technology Foundation
Let's be honest: any talk of an AI in healthcare strategy has to start with the data, and most healthcare data is a complete mess. It's often siloed, fragmented, and locked away in systems that don't talk to each other, making it nearly impossible to use for anything truly innovative. Before you even think about deploying an algorithm, you have to get this foundation right.
This starts with putting strong data governance in place. Think of this less as a technical chore and more as the essential framework that ensures every piece of patient information is handled securely and in full compliance with HIPAA. Governance defines the rules of the road: who can access what, how it can be used, and the quality standards it must meet.
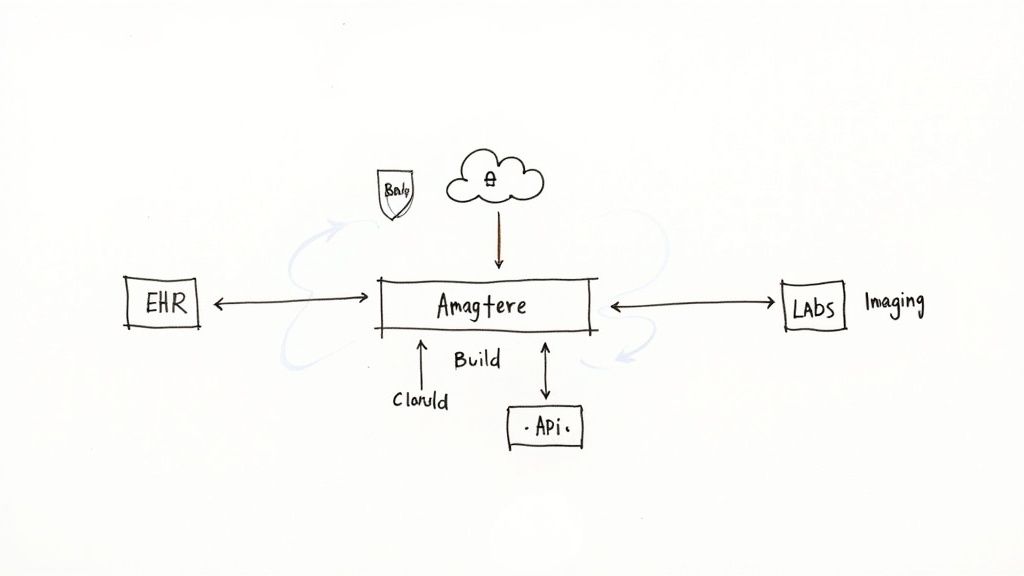
Once the rules are set, the real work begins: unifying all those disparate data sources. This means pulling together information from your Electronic Health Records (EHRs), imaging archives (PACS), lab results, and even billing systems. By cleaning, standardizing, and consolidating this data, you create a single source of truth—the high-quality fuel your AI models will need to run accurately.
The Critical Build vs. Buy Decision
With your data house in order, you’ll quickly run into a major fork in the road: should you build your own AI models from scratch or buy ready-made solutions from a vendor? There’s no easy answer here. The right path really depends on your organization's resources, in-house expertise, and long-term goals. Getting expert advice on AI strategy consulting can save a lot of headaches at this stage.
Building Proprietary Models: This route gives you maximum control and customization. You can develop solutions perfectly tailored to your unique clinical workflows, creating powerful internal tooling that can become a real competitive advantage. The catch? It requires a massive investment in specialized talent, infrastructure, and ongoing maintenance. This is the domain of custom healthcare software development, and it's not for the faint of heart.
Buying Vendor Solutions: Working with a vendor gets you access to proven technology much faster and without the heavy R&D lift. The trade-off, of course, is less customization. When you're looking at third-party AI tools for business, you have to be relentless in assessing their security, scalability, and—most importantly—how easily they'll integrate with your existing systems.
This decision is a big one, especially with the money pouring into this space. In 2023, global spending on AI in healthcare reached $19.3 billion, and projections show it skyrocketing to over $613 billion by 2034. That's a compound annual growth rate of over 40%, signaling a massive wave of both opportunity and competition. You can discover more insights about these AI in healthcare spending projections to get a sense of the scale.
Creating a Scalable Technology Stack
Whether you decide to build, buy, or go with a hybrid approach, your ultimate goal is a tech stack that’s both scalable and flexible. Your infrastructure needs to be strong enough to handle your initial pilots but also have the capacity to expand for enterprise-wide rollouts down the line. If you don't think ahead, you risk getting locked into a system that can’t grow with your ambitions.
A common mistake I see all the time is underestimating the integration effort. A brilliant AI tool that can't communicate with your EHR or billing system is functionally useless. Prioritize solutions with open APIs and a clear integration roadmap from day one.
This foundational work is, without a doubt, the hardest part of bringing an AI in healthcare strategy to life, but it's also the most important. By taking the time to get your data and technology house in order, you're setting the stage for every success that follows. It's so critical that it's a core component of our own AI Product Development Workflow, because we know that great tech can only be built on a solid base.
It’s All About the People: Driving Real-World Adoption
Let’s be honest. You can have the most sophisticated AI in healthcare strategy on paper, but if your front-line staff won't use the tools, it's just an expensive failure. Technology is the easy part. The real challenge—and where most initiatives stumble—is the human side of the equation. Getting your team on board isn't about top-down mandates; it's about turning skepticism into genuine enthusiasm.
This has to start at the leadership level. You need executive sponsors who don’t just sign the checks but actively clear roadblocks and champion the vision. Just as crucial, however, are your clinical champions. Find those respected doctors, nurses, and techs who get it—the ones who see the potential and can vouch for the new tools with their peers. Their word carries more weight than any memo from the C-suite ever will.
Don't Just Announce It, Communicate It
Forget the generic corporate emails. Real communication means getting into the weeds and addressing the real, often unvoiced, fears of your team. Clinicians are probably wondering if this new AI is meant to second-guess their judgment or, worse, eventually replace them. Your IT team is likely bracing for the headache of supporting yet another complex system.
You have to tailor your message:
For Clinicians: Position AI as a partner, not a replacement. Show them how it’s designed to kill the drudgery—the endless documentation and data sifting—so they can spend more time on what actually matters: complex patient care and human interaction. It's about augmenting their expertise, not undermining it.
For IT Staff: Bring them into the tent from day one. Be transparent about how the new AI solutions will plug into your existing tech stack and what resources they'll have. Frame it as a move toward smarter, more sustainable workflows, not just another ticket-generating machine.
For Administrative Teams: Connect the dots directly to their daily grind. Talk about how it will slash manual data entry, automate scheduling chaos, and solve the practical problems they face every single day. This is the core value of services like our AI Automation as a Service.
An executive from HCA Healthcare put it perfectly: involving frontline staff from the start is non-negotiable. It’s the ultimate validation that you’re solving a problem they actually have. Skip this, and you’re building a tool nobody will touch.
From Training Day to Everyday Confidence
Training can’t be a box-checking exercise. A one-hour "how-to" webinar won't cut it. You need to build real confidence. Create learning sessions that mimic actual clinical scenarios, giving people a safe space to play with the tools, make mistakes, and ask questions without feeling pressured.
And remember, adoption isn’t a one-and-done event. It's a process. You need a constant feedback loop so your team feels heard. Set up simple channels—a dedicated Slack channel, quick weekly huddles—where people can flag issues, celebrate small wins, and suggest improvements. This does two things: it provides you with invaluable insights to make the system better, and it shows your team their experience matters. It's a philosophy we bake right into our own AI Product Development Workflow, because technology should serve the people using it, not the other way around.
Ultimately, this is the secret sauce. When people see AI as a supportive colleague that makes their jobs better, adoption stops being a battle. As we’ve covered in our AI adoption guide, this human-centered focus is what separates a successful rollout from a costly misfire. It ensures your AI in healthcare strategy is more than just good tech; it's woven into the very fabric of how you deliver care. This stuff is tricky, and having guidance from our expert team can be a game-changer.
Setting the Guardrails: Governance and Measuring What Matters
An AI in healthcare strategy without clear guardrails and concrete goals is just an expensive guess. Once you’ve figured out which problems you want to solve and have the right technology in place, you have to shift your focus to governance. This isn't about creating red tape; it's about making sure every AI initiative is ethical, safe, and actually helps you achieve your mission.
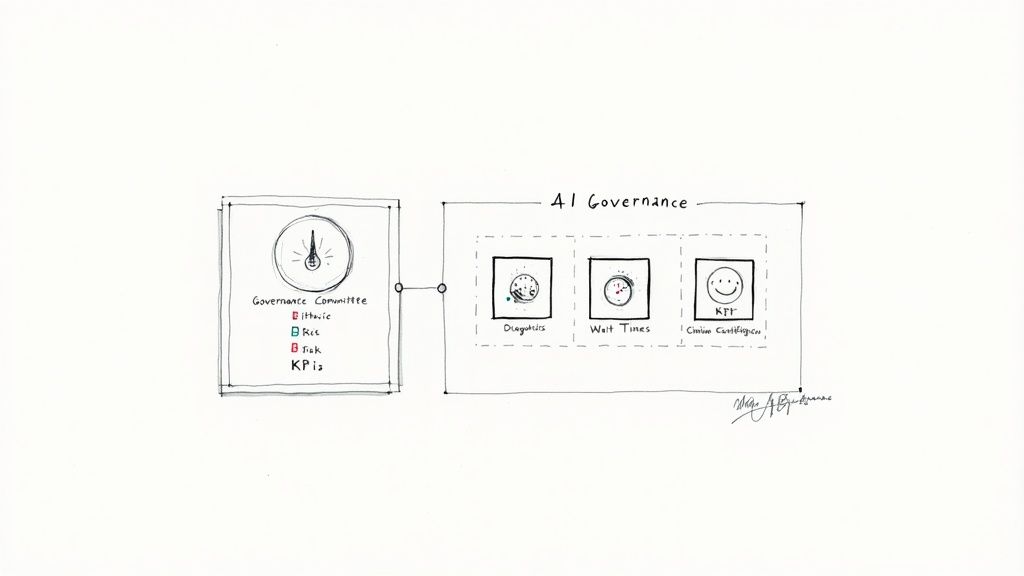
The best way to start is by forming a dedicated AI governance committee. This can't be siloed in the IT department. You need a cross-functional team at the table—clinical leaders, legal and compliance experts, data scientists, and key administrators. Their job is to oversee the entire lifecycle of your AI tools, from development to retirement, managing risks and ensuring everything you deploy is fair and trustworthy.
Getting this right is foundational. For a deeper dive, it's worth understanding the importance of Artificial Intelligence governance as it truly acts as the strategic conscience for your entire AI program.
Defining KPIs That Truly Matter
I've seen too many projects get bogged down in technical metrics. An algorithm with 99% accuracy is completely useless if it doesn't improve patient care, make a clinician's job easier, or smooth out a clunky operational workflow. Your key performance indicators (KPIs) have to reflect real-world impact.
It’s time to move beyond the technical jargon and focus on what matters to your staff and your patients.
Clinical Outcomes: Are you actually reducing diagnostic errors? Are readmission rates dropping? Can you identify at-risk patients sooner than before? These are the tangible improvements that count.
Operational Efficiency: Look at the workflow. Have patient wait times decreased? Are you saving your staff hours of administrative drudgery? Is resource scheduling more intelligent?
Patient & Clinician Satisfaction: Don't forget the human element. Use surveys and direct feedback to find out if these new tools are a help or a hindrance to the people using them every day.
These are the numbers that tell a compelling story to leadership and justify further investment. You absolutely have to establish a baseline for these metrics before you flip the switch on any AI tool.
The Ongoing Mandate of Model Validation
Here’s something many organizations forget: launching an AI model is the starting line, not the finish. These systems aren't static. They can "drift" over time as your patient demographics shift or clinical practices evolve. This means ongoing validation isn't optional—it's a critical part of your governance.
You need a process for regularly checking that your models are still accurate, fair, and free from bias. This is an active, continuous effort, not a one-time checkup. It’s all about building and maintaining trust in the technology for the long haul.
A model trained on data from one demographic might perform poorly when applied to another. Continuous validation ensures your AI tools serve all patients equitably and safely, preventing the amplification of existing health disparities.
The pace of change here is staggering. Recent research shows 22% of healthcare organizations have now implemented domain-specific AI solutions, a sevenfold jump in just one year. With adoption this rapid, strong governance is more critical than ever to keep things on the right track.
Putting all these pieces together can feel overwhelming. For organizations that need a clear path forward, a structured Custom AI Strategy report can help formalize this entire framework. Likewise, a dedicated AI Strategy consulting tool can offer the templates and expert guidance to get this done right, ensuring your AI in healthcare strategy is built on a foundation of trust and real results. Without it, you’re just flying blind.
Scaling Your AI Initiatives from Pilot to Enterprise
A successful pilot is a great start, but it's just that—a start. The real, system-wide impact of your AI in healthcare strategy only comes when you scale those initial wins across the entire organization. This is where you graduate from isolated experiments to an enterprise-wide shift that delivers consistent, measurable value.
Moving beyond a single successful pilot isn’t accidental; it demands a deliberate plan. This means building out the technical backbone for growth—think robust cloud infrastructure and flexible APIs that let new tools plug into your existing systems without a massive headache. If you don't lay this foundation first, your expansion will quickly hit a dead end.
Creating a Blueprint for Growth
The technology is one piece of the puzzle, but the strategic elements are arguably even more important. You can't have every department reinventing the wheel. Effective scaling requires standardizing the workflows that you've proven work, updating policies to reflect new AI-driven processes, and creating a central governance body—often called a Center of Excellence—to drive best practices and keep quality high.
This central team acts as the nervous system for your AI efforts, ensuring every part of the organization is aligned and preventing the kind of fragmented, siloed work that stalls so many great ideas.
"It’s about variance reduction. How can we reduce variance and in doing so improve the consistency with which we deliver the highest level of care to our patients?” - HCA Healthcare Executive
That quote gets right to the heart of it. The goal of scaling is to make excellence the standard, not the exception.
A Continuous Cycle of Improvement
The road from pilot to enterprise isn’t a one-and-done project. It's a constant cycle of implementing, measuring, and refining. Every initiative you scale will generate fresh data and new insights. You have to feed that information back into your strategy to find the next opportunity for improvement. This iterative loop is what builds a genuinely intelligent and adaptive healthcare organization over the long haul.
It's a complex journey that requires the right partners and a clear vision. Navigating the technical and organizational hurdles of scaling is a major undertaking, but it's the final, crucial step to getting the full value from your AI investments. Our structured AI Product Development Workflow is built to guide organizations through this very process, ensuring a promising pilot can become an enterprise-wide success.
Answering the Tough Questions About Your Healthcare AI Strategy
Diving into an AI strategy for your healthcare organization is bound to bring up some big, important questions. Let's be honest, it's a complex field. Getting clear, no-nonsense answers is the best way to cut through the noise and feel confident about the path ahead.
Here are a few of the most common questions I hear from healthcare leaders and my take on how to tackle them.
Where on Earth Do We Start?
This is the big one. The single most important first move is to get the right people in the room. You need to assemble a cross-functional steering committee—think of it as your AI brain trust. This isn't just an IT project; you need clinicians, administrators, IT pros, and executive sponsors all at the same table.
Once you have your team, their first job is to agree on your core goals. What are the biggest headaches you're trying to solve? Don't try to boil the ocean. Instead, pick two or three high-impact problems where AI could make a real, measurable difference. Think about persistent issues like patient no-shows or frustrating delays in diagnostic imaging workflows. By starting small and focused, you build momentum. This approach is a cornerstone of what we discuss in our broader AI adoption guide.
How Do We Handle Patient Data Privacy?
Patient data privacy isn't just a priority; it's a foundational, non-negotiable requirement for any AI solution in healthcare. This has to be baked into your strategy from day one, not bolted on as an afterthought. You absolutely must build a rock-solid, HIPAA-compliant data governance framework.
What does that look like in practice?
De-identify everything you can. Use anonymized or de-identified data for training your models whenever possible.
Lock down access. Implement strict, role-based access controls. Not everyone needs to see everything.
Run constant security drills. Regular security audits are your best friend for finding and plugging holes before they become major problems.
Vet your vendors. If you're working with a third-party AI provider, make sure they have verifiable, healthcare-specific compliance certifications. Ask for proof.
How Do We Actually Measure the ROI?
You can't prove the value of your AI investments if you don't define what success looks like from the very beginning. Measuring the return on investment (ROI) means setting clear metrics before you flip the switch on any new system.
Establish a pre-AI baseline for your key performance indicators (KPIs) so you can show a clear "before and after" picture. The most compelling business cases demonstrate value across the board:
Financial Wins: Are you seeing reduced operational costs? Is revenue capture improving from more efficient billing cycles?
Clinical Impact: Can you point to better diagnostic accuracy? Have patient readmission rates dropped?
Operational Gains: Are you saving administrative hours? Is the time it takes to schedule an appointment going down?
This process is complex, but it’s the only way to build a sustainable, impactful AI program. If you need help turning these strategic pillars into an actionable plan, our expert team is here to guide you every step of the way.