AI and Medical Diagnosis: A New Era of Healthcare
Explore how AI and medical diagnosis are transforming healthcare. Discover real-world applications, benefits, and challenges of using AI to improve accuracy.

Picture a physician who can spot the nearly invisible, analyze millions of patient files in a flash, and detect the earliest whispers of disease long before a patient feels a single symptom. This isn't a scene from a futuristic movie; it's what's happening right now with AI and medical diagnosis. Artificial intelligence is helping medicine evolve from a reactive discipline to a truly predictive one, giving healthcare professionals powerful new tools and improving lives.
Unlocking a New Era of Predictive Healthcare

The fundamental promise of bringing AI into diagnostics is simple: to enhance human expertise, slash the rate of errors, and deliver better care, faster. These intelligent systems analyze incredibly complex medical images, genetic codes, and clinical notes at a speed no human could ever match, completely reshaping how we think about health. The entire mindset is shifting from waiting for problems to appear to actively getting ahead of them.
This guide will walk you through the key technologies making this possible, their tangible impact, the real-world hurdles to implementation, and what’s next on the horizon. We'll explore how advanced tools are not here to replace doctors but to serve as their indispensable co-pilots in the diagnostic journey.
The Accelerating Pace of Adoption
The move to adopt artificial intelligence in clinical settings isn't just happening—it's accelerating. This boom is a direct result of the technology becoming more mature and regulatory bodies getting on board.
Consider this: in 2023 alone, the U.S. Food and Drug Administration (FDA) gave the green light to 223 AI-enabled medical devices. That's a massive jump from just six approvals back in 2015. This incredible growth shows just how quickly AI is becoming a standard part of clinical practice. On a global scale, the AI-powered medical technology market is expected to skyrocket to nearly $600 billion by 2025, all driven by the demand for smarter diagnostic tools.
The goal is not to replace clinicians but to empower them with tools that can process vast amounts of data, identify subtle patterns, and provide insights that lead to earlier and more accurate diagnoses. This collaborative approach is key to improving patient outcomes.
Core Technologies Driving the Change
At the heart of this shift are a few key AI technologies. Each one plays a unique role in bringing diagnostics into the 21st century, and understanding them helps clarify how AI makes a real difference.
To make this easier to grasp, here’s a quick overview of the key AI technologies transforming medical diagnosis and their primary roles.
Core AI Technologies Powering Modern Diagnostics
AI Technology Primary Diagnostic Application
Machine Learning (ML)
The core engine. ML models learn from massive datasets of medical images or patient data to spot anomalies—like potential tumors—with incredible precision.
Deep Learning
A more advanced subset of ML. It uses complex neural networks to find patterns in unstructured data like MRIs, CT scans, and pathology slides.
Natural Language Processing (NLP)
This gives AI the ability to read and understand human language. NLP can instantly sift through mountains of clinical notes to flag risks or extract key data.
These technologies work together, creating a powerful toolkit for modern medicine. They're the building blocks for the next generation of diagnostic excellence.
For those interested in a broader view, you can find comprehensive insights into healthcare artificial intelligence.
How AI Learns to See What Humans Can't
At its heart, using AI in medical diagnosis is about pattern recognition on a massive scale. We're teaching machines to spot clues in medical data that are far too subtle or complex for the human eye to catch consistently. It’s not magic—it's the result of training powerful algorithms on vast libraries of medical data until they learn to make incredibly accurate predictions. This is where modern AI solutions truly shine, acting as a powerful assistant to even the most seasoned clinicians.
Imagine a deep learning model as a brilliant medical student. Instead of a textbook, it's given millions of real-world case files—X-rays, MRIs, and CT scans—each meticulously labeled by expert radiologists. With every single image it processes, the model learns to connect specific pixel patterns, textures, and shapes with a confirmed diagnosis.
Eventually, it starts picking up on the nearly invisible signals of early-stage disease, much like a veteran doctor develops an intuition for "what doesn't look right." This is how an AI can flag a tiny, suspicious nodule on a scan that might otherwise be missed, offering a critical second look. Our process for building these sophisticated systems is laid out in our AI Product Development Workflow.
Translating Clinical Notes into Actionable Data
A diagnosis isn't just based on images; it relies heavily on the patient's story buried in clinical notes. Electronic Health Records (EHRs) are treasure troves of information, but it's often unstructured text: doctors' observations, patient histories, and lab reports. This is where another crucial technology, Natural Language Processing (NLP), steps in.
Think of NLP as an incredibly diligent research assistant who can read and comprehend thousands of patient files in seconds. It sifts through all that text to extract the most critical pieces of information.
- Symptom Extraction: It pinpoints and organizes symptoms mentioned in a doctor's free-form notes.
- Risk Factor Identification: The system can automatically flag lifestyle details or family histories that point to a higher risk for certain diseases.
- Timeline Creation: NLP pieces together a patient's complete health journey from scattered entries across different records.
Pulling these details together is vital for creating a comprehensive diagnostic picture. For organizations ready to build these capabilities, our AI Automation as a Service offers a structured path to get there.
By analyzing huge datasets of both images and text, AI models can discover hidden connections that lead to earlier, more accurate diagnoses and highly personalized treatment plans. The entire goal is to transform mountains of raw data into clear, life-saving insights.
From Raw Data to Diagnostic Insight
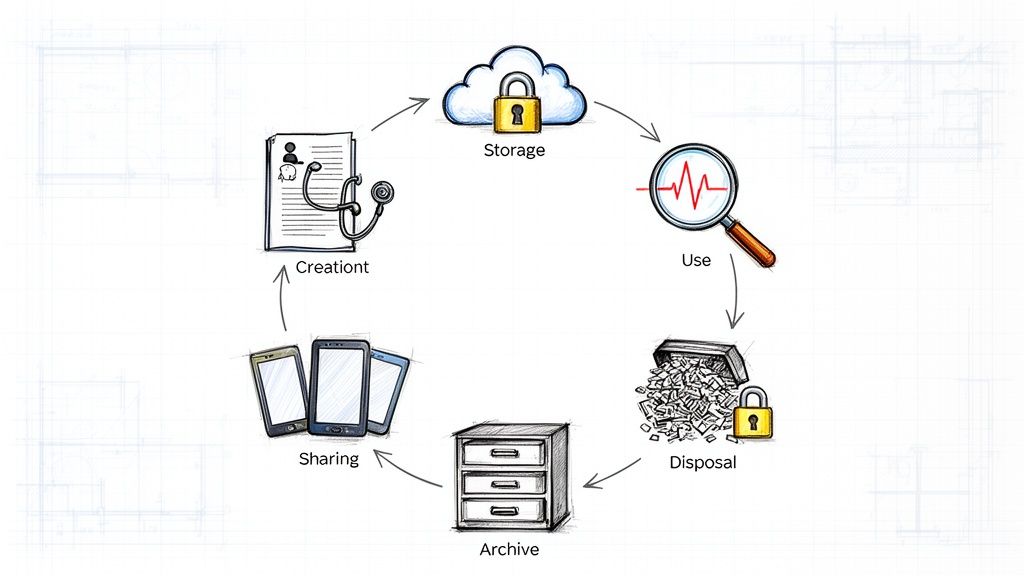
The path from a patient's data to a diagnostic suggestion follows a clear, structured process. It starts with collecting and preparing the data, where medical images and records are cleaned up and standardized for the algorithm. Next comes the heavy lifting: training the AI model, a phase that can require thousands of hours of powerful computation.
Finally, before it ever gets near a real clinical environment, the trained model is rigorously tested against a brand-new set of data to prove its accuracy. This painstaking training and validation process is what ensures the reliability of the insights it provides. You can see how this works in practice by exploring various real-world use cases. These aren't just theories; they are practical AI tools for business that are actively improving healthcare.
This entire journey is guided by a clear plan, which is where our expertise in AI strategy consulting and the experience of our expert team come together to make these complex projects a success.
Real-World Victories in AI Diagnostics
The theory behind AI and medical diagnosis is impressive, but where the rubber really meets the road is in its real-world application. We're seeing AI deliver tangible results across various medical fields, turning vast amounts of data into insights that help clinicians make better, faster decisions. These aren't just hypotheticals—they are success stories happening right now.
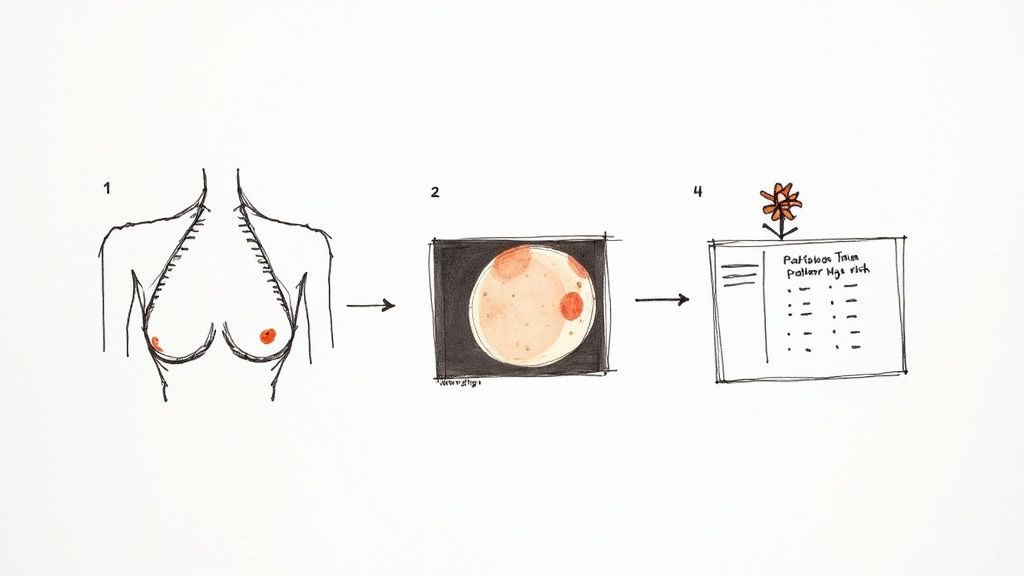
Radiology is a perfect example. AI models, after being trained on millions of mammograms, can spot the earliest signs of breast cancer with an accuracy that often rivals, and sometimes exceeds, that of a human expert. Think of it as a tireless, vigilant assistant, flagging subtle patterns that a busy radiologist might overlook.
This dramatically cuts down on false negatives, giving patients a crucial head start on treatment when it’s most effective. What emerges is a powerful partnership: the AI handles the high-volume screening, freeing up radiologists to apply their deep expertise to the most complex and ambiguous cases.
Revolutionizing Pathology with Precision
Pathology is another area seeing a massive impact. When a pathologist grades a tumor from a tissue sample, there’s always an element of human interpretation. Two highly skilled experts can look at the same slide and come to slightly different conclusions, a variation that can change a patient’s entire treatment course.
AI introduces a new level of objectivity. By analyzing tissue slides at a microscopic level, these algorithms can grade tumors with incredible consistency. This standardizes the diagnostic process, ensuring every treatment plan is built on a foundation of objective, repeatable data. This is where custom healthcare software development shines—by creating tailored tools to solve these specific clinical pain points.
By providing consistent, data-driven analysis, AI tools help standardize diagnostics, reduce human variability, and ultimately lead to more reliable and effective patient care strategies.
For a concrete look at this in action, our own diagnostic tool, Diagnoo, shows how AI can analyze medical data to provide clinicians with supportive insights, streamlining the diagnostic workflow.
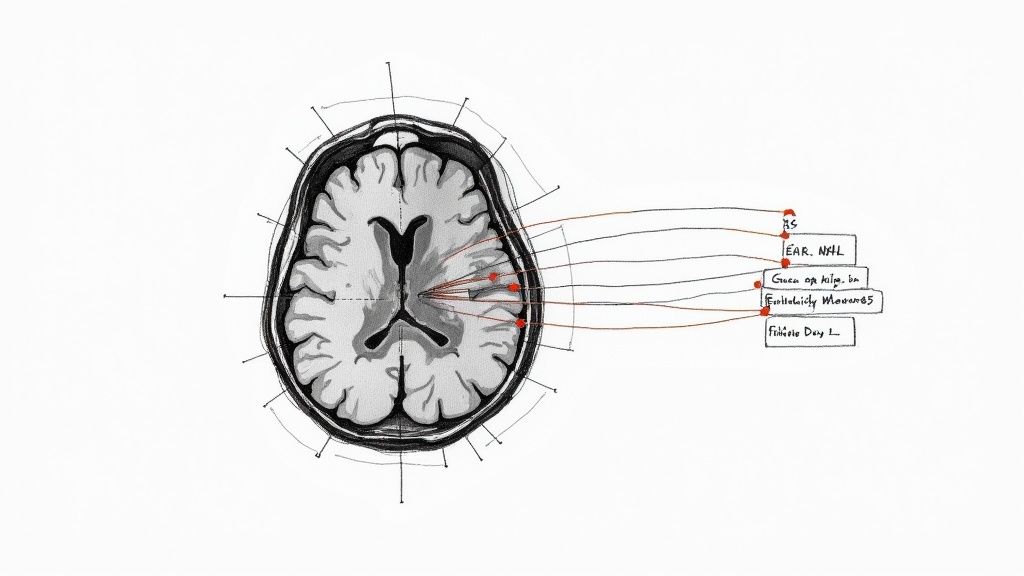
Uncovering Hidden Diseases in Patient Records
It's not all about images. AI's ability to sift through text-based medical records is opening up entirely new frontiers. For years, clinicians have suspected that clues to rare diseases were buried in a patient's electronic health record (EHR), but connecting those scattered dots was a near-impossible manual task.
A groundbreaking AI system named InfEHR, developed by researchers at the Icahn School of Medicine at Mount Sinai, has cracked this problem. It combs through mountains of unstructured notes and data in EHRs, identifying clinical patterns that point to specific conditions. The system turns millions of disconnected data points into a coherent picture, allowing doctors to confirm diagnoses they previously couldn't, which is critical for finding crucial clues for diagnoses.
This kind of deep analysis can flag individuals at high risk for diseases that might have gone undetected for years. It's a huge step forward in proactive medicine, powered by AI's unique ability to find the signal in the noise. Building such a system requires a solid foundation, often starting with powerful internal tooling designed to manage and process huge healthcare datasets securely. These examples make it clear: AI is no longer just a concept. It's a practical, life-saving tool that is actively reshaping modern medicine.
Overcoming the Hurdles of AI in Medicine
Bringing powerful AI into the sensitive world of medical diagnosis isn't as simple as installing new software. The path is filled with serious challenges that go far beyond the tech itself. We're talking about deeply rooted issues in data security, ethics, and the day-to-day realities of a hospital. Getting ahead of these hurdles is the first step toward making any AI initiative a success.
One of the biggest concerns right out of the gate is data privacy and security. Patient health information is about as personal as it gets, and it’s protected by strict regulations like HIPAA. Any AI system handling this data has to be a fortress. That means rock-solid encryption, secure storage, and tight access controls are absolutely non-negotiable.
Then there's the thorny ethical problem of algorithmic bias. An AI is only as good as the data it learns from. If the historical data used for training contains built-in biases—say, disparities in how certain groups were diagnosed—the AI will learn those same biases. Even worse, it might amplify them, leading to a system that's less accurate for minority populations and making health inequities even bigger.
Breaking Down Technical and Trust Barriers
On a more practical level, systems integration can be a nightmare. Many hospitals are still running on older IT systems that were never meant to talk to modern AI platforms. Connecting the old with the new takes serious technical skill and a significant budget. If you don't get this right, your shiny new AI tool ends up being an information island, unable to truly help within the clinical workflow.
But perhaps the most human challenge of all is the infamous "black box" problem. When a sophisticated AI gives a diagnostic suggestion but can't explain why, it creates a massive trust issue. Doctors are trained to understand the reasoning behind their decisions. If they can't see the logic, they're not going to bet a patient's health on the AI's recommendation. It's as simple as that.
The "black box" isn't just a technical puzzle to be solved; it's a fundamental barrier to adoption. If doctors can't trust the how and why behind an AI's suggestion, the technology will remain a fascinating experiment instead of becoming a trusted part of patient care.
Patients feel the same way. A recent study revealed that 70.2% of patients would much rather have an explainable AI model, even if it was slightly less accurate than a black box version. An even larger majority, 72.9%, insisted on a model where the doctor makes the final call. This tells us loud and clear that both patients and physicians need transparency and human oversight. You can explore the full study to see just how important this is to them. A clear path forward often begins with a Custom AI Strategy report to map out these challenges from the start.
Building a Framework for Success
Getting past these obstacles isn't just about having better tech; it's about having a smart, deliberate strategy. This is where getting help with AI strategy consulting can make all the difference. A strategic partner helps you see these challenges coming and build a solid framework to handle them.
A solid framework for AI implementation should include:
- A strict data governance policy to manage privacy and compliance right from the beginning.
- Protocols for detecting and mitigating bias to constantly test and correct for unfairness in the models.
- A phased integration plan to update infrastructure and smoothly connect AI tools with the systems clinicians already use.
- A deep commitment to explainable AI (XAI), choosing models that can clearly show their work.
By tackling these hurdles with a clear plan, as we explored in our AI adoption guide, healthcare organizations can move forward with confidence. The real goal is to implement AI solutions that are not just technically impressive, but are also trustworthy, ethical, and woven seamlessly into the very fabric of patient care.
The Future of Predictive and Personalized Medicine
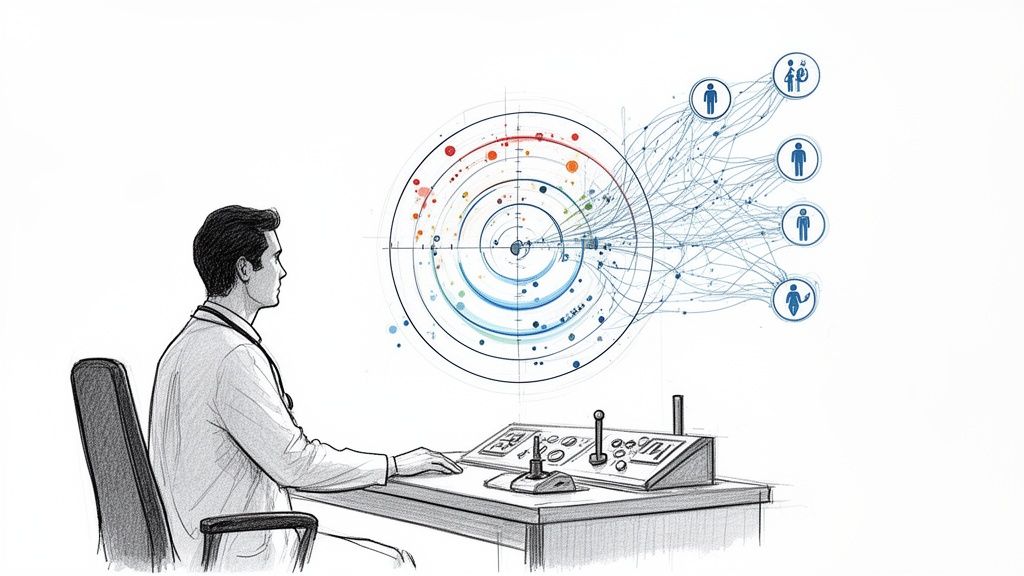
The evolution of AI in medical diagnosis isn't just about making today's methods a little better; it's about flipping the script on healthcare entirely. We're moving away from a model that reacts to sickness and toward one that actively predicts and prevents it. This next chapter is all about forecasting future health risks, not just identifying current illnesses.
At the heart of this shift is predictive analytics. AI models are getting incredibly good at looking at the whole picture of a person—their genetics, lifestyle habits, and clinical history—to calculate the odds of them developing certain diseases years before they might happen.
Think about an AI that can analyze your genetic markers and daily habits to flag a high risk for pancreatic cancer long before a single symptom shows up. This isn't science fiction. Researchers have already built models that can do this with greater accuracy than standard population estimates, all by sifting through millions of patient records to find subtle patterns we'd never spot on our own. This kind of early warning gives patients and doctors the one thing they need most: time. Time to intervene and maybe even change the outcome.
The Dawn of Truly Personalized Medicine
Getting a heads-up on future health risks is just one piece of the puzzle. The real goal is to use that information to craft diagnostic and treatment plans that are completely unique to you. We're leaving the one-size-fits-all approach behind and using AI to tailor medical care to an individual's specific biological makeup.
This means we can design a treatment plan based on how your body will likely respond. For instance, AI can analyze a tumor's genomic data to predict how it will react to different chemotherapy drugs. This helps an oncologist pick the most effective option right out of the gate, improving a patient's chances while sparing them the grueling trial-and-error process. Our AI Product Development Workflow is built to help create these kinds of specific, high-impact applications.
The future of medicine isn't about treating diseases; it's about treating individuals. AI gives us the power to understand each person's unique health landscape, paving the way for care that is as unique as a fingerprint.
Continuous Monitoring Through Wearable Technology
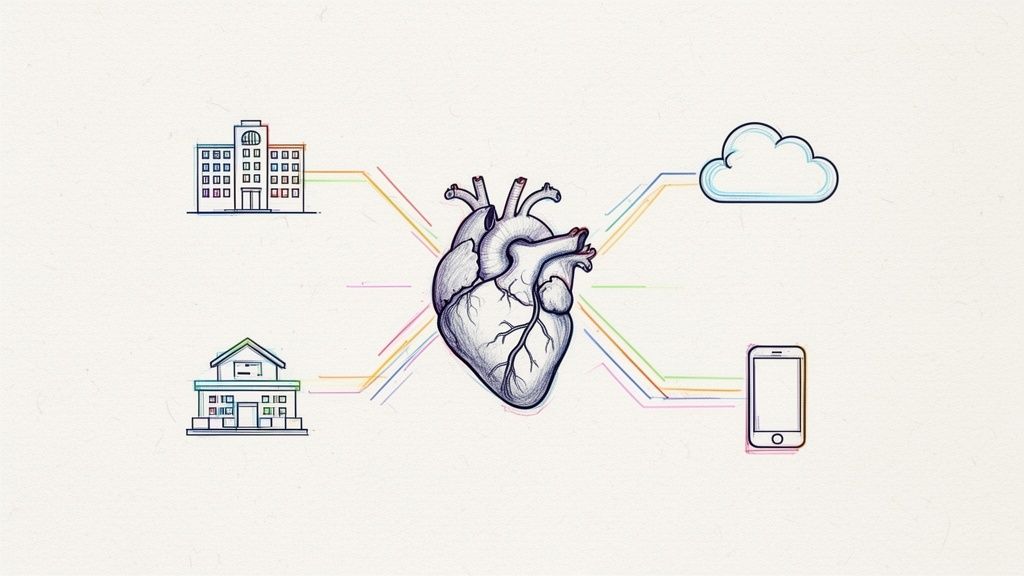
This vision of proactive health is already coming to life, thanks to the explosion of AI-powered wearable devices. The smartwatch on your wrist and the phone in your pocket are no longer just for calls and texts; they're becoming sophisticated, always-on health monitors.
These gadgets are constantly collecting a river of data—heart rate, sleep quality, activity levels, even blood oxygen saturation. This creates a detailed, real-time portrait of your well-being. AI algorithms work in the background, analyzing this constant stream of information to spot tiny deviations from your personal baseline that could signal a problem brewing. An irregular heartbeat detected while you sleep or a slow decline in your daily steps could be the very first whisper of a developing condition.
Imagine combining this with services like at-home blood testing as a personal dashboard for longevity, feeding even more precise data into the system. This creates a powerful feedback loop between your devices and intelligent systems, forming a personalized early-warning network. By turning our everyday gadgets into diagnostic allies, we’re making proactive health monitoring a natural part of daily life—a core idea in modern custom healthcare software development. The future we're building is one where healthcare is preemptive, individualized, and always on.
Your Roadmap to Adopting Diagnostic AI
For healthcare leaders looking to bring AI into their diagnostic workflows, a clear, step-by-step plan is non-negotiable. This isn’t just a simple tech upgrade; it’s a deep shift in how your organization operates and thinks. Real success comes from a thoughtful plan that puts just as much emphasis on your people and processes as it does on the algorithms.
The first move is always strategic. Start by finding one high-impact clinical problem where AI can deliver an obvious win. Don't try to boil the ocean. Instead, focus on a specific bottleneck, like clearing the radiology backlog or getting better at spotting sepsis early. Once you have a target, the next step is a deep dive to define exactly what the technology needs to do.
This infographic paints a picture of where medicine is headed—a future driven by predictive, personalized, and continuous care.
You can see the natural progression here, moving from using data to forecast health problems to customizing treatments and keeping a constant watch on patient health.
Building the Foundation for Implementation
With a clear goal in mind, the focus shifts to getting the basics right. Data readiness is absolutely critical. Your data has to be clean, organized, and accessible for an AI model to learn from it properly. At the same time, you have to manage the cultural change with your clinical teams. This means bringing clinicians into the conversation from day one, listening to their concerns, and showing them how AI is a tool to support them, not replace them.
Taking a pilot-first approach is almost always the smartest way to go. Launching a small-scale pilot project lets you prove real value, get key stakeholders on board, and smooth out the rough edges before you go all-in. It’s an iterative way to build momentum and confidence.
The success of any diagnostic AI initiative is determined long before a single line of code is written. It starts with a clear strategic vision, buy-in from everyone involved, and a deep understanding of the clinical problem you’re trying to solve.
Your Path Forward with Expert Guidance
Making your way through this complex landscape takes a mix of clinical know-how and technical skill. Choosing the right technology partner is one of the most important decisions you'll make. You need a team that gets the subtleties of healthcare and can turn your clinical needs into a reliable AI solution. For an administrative starting point, our Clinic AI Assistant can help manage patient intake and scheduling, which frees up your staff for more critical work.
A solid plan, backed by expert guidance, is what turns a promising idea into something that actually works. The journey starts with that first step, and for those ready to take it, we're here to help you move from initial vision to real-world impact, making sure your organization is ready for what's next in medicine.
Your Questions Answered: AI in Medical Diagnosis
It’s natural to have questions about how AI fits into the world of medicine. Let's tackle some of the most common ones to clear up the picture of where this technology stands today.
Will AI Replace Doctors and Radiologists?
The short answer is no. The real aim isn't replacement but collaboration. Think of AI as an incredibly sharp co-pilot for clinicians, handling the heavy lifting of data analysis with speed and precision that humans simply can't match.
This allows doctors and radiologists to dedicate their time to what they do best: applying critical judgment, connecting with patients, and piecing together complex treatment plans. The best outcomes happen when a physician and an AI work together—the tech provides deep insights, but the doctor always makes the final call. This collaborative approach is at the heart of the tools we see from leading AI solutions providers.
How Is the Accuracy of Diagnostic AI Ensured?
You're right to ask about accuracy, and the process is incredibly rigorous. It’s a multi-layered system of checks and balances that starts long before an AI tool ever sees a real patient. First, the models are trained on massive, diverse, and meticulously curated datasets to avoid building in biases.
From there, the AI is put through its paces, tested extensively against gold-standard clinical benchmarks and reviewed by panels of expert physicians. Finally, regulatory bodies like the FDA have stringent approval gauntlets. They require hard evidence of both safety and effectiveness before any AI-powered medical tool can be cleared for clinical use.
It's a common myth that diagnostic AI operates in a black box without any oversight. The truth is, every FDA-approved tool has been through layers of scientific and regulatory validation to prove it's both safe and reliable for patient care.
What Are the First Steps for a Hospital to Adopt AI?
Jumping into AI without a plan is a recipe for frustration. The journey should begin with a specific goal. Instead of a vague "we need AI," a hospital should identify a concrete problem it wants to solve, like spotting sepsis earlier or clearing the backlog of mammogram readings. As we explored in our AI adoption guide, a focused starting point is critical.
Once you have a target, the next step is a realistic look at your data infrastructure. An AI requirements analysis can give you a clear picture of your readiness. Starting with a manageable pilot project is the smartest move—it proves the value, gets clinical staff on board, and builds momentum. Working with an expert in AI strategy consulting can help navigate these steps, turning a good idea into a clinical reality. If you're wondering where to start, our expert team is here to guide you.
Ready to see how AI could reshape your organization's diagnostic capabilities? At Ekipa AI, we specialize in identifying high-impact opportunities and creating a clear path forward. Get your Custom AI Strategy report in just 24 hours and begin your journey. Talk to our expert team to learn more.