8 Real-World Examples of AI in Clinical Decision Support Systems for 2026
Explore 8 powerful examples of AI in clinical decision support systems, from sepsis prediction to oncology. See how AI is transforming patient care.
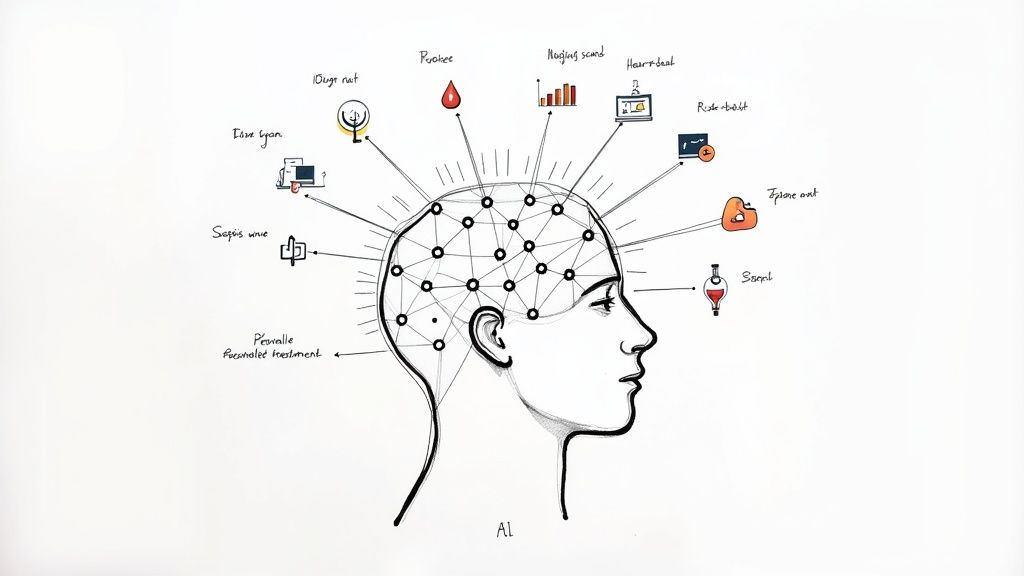
In modern medicine, data is abundant, but actionable insights are precious. Clinicians face a daily deluge of information from electronic health records, imaging scans, and lab results, making it increasingly challenging to connect the dots for optimal patient care. This is where Artificial Intelligence steps in, not as a replacement for human expertise, but as a powerful co-pilot. Clinical Decision Support Systems (CDSS) augmented with AI are transforming how diseases are detected, managed, and treated.
These systems analyze vast datasets at superhuman speeds to identify subtle patterns, predict risks, and recommend personalized interventions. For instance, AI-driven tools like an AI Healthcare Medical Record Analyzer can process vast amounts of patient data, identifying patterns and insights critical for diagnosis and personalized treatment. For healthcare leaders and innovators, understanding the practical applications of these technologies is the first step toward building a smarter, more efficient, and patient-centric future.
This article explores concrete examples of AI in clinical decision support systems, moving beyond the hype to showcase tangible impacts on patient outcomes. From early sepsis detection to precision oncology, these real-world use cases demonstrate the power of well-integrated AI solutions. As you consider how to leverage these advancements, an effective AI strategy is crucial. Developing a clear roadmap, much like the process for a Custom AI Strategy report, ensures that technology adoption aligns with clinical needs and organizational goals. Let's dive into the specific examples shaping the future of medicine.
1. Radiology Image Analysis and Diagnostic Support
Radiology image analysis is one of the most mature and impactful examples of AI in clinical decision support systems. These systems use deep learning algorithms, particularly convolutional neural networks (CNNs), to analyze medical images like X-rays, CT scans, and MRIs. The AI identifies subtle patterns, anomalies, and potential pathologies that may be missed by the human eye, flagging them for radiologist review.
This technology doesn't replace radiologists; it augments their expertise. By automating the initial review and highlighting areas of concern, AI accelerates diagnoses, reduces workload, and improves accuracy. For instance, FDA-approved systems from companies like iCAD and Aidoc can detect signs of stroke or pulmonary embolism on CT scans, automatically prioritizing these critical cases in a radiologist's worklist.
Strategic Analysis & Implementation
For leaders considering this technology, the goal is to enhance, not replace, existing workflows. The AI acts as a "second pair of eyes," increasing diagnostic confidence and efficiency. A key business driver is throughput; by prescreening images and prioritizing urgent cases, radiology departments can handle higher volumes without sacrificing quality.
Key Insight: The strategic value of AI in radiology isn't just about finding anomalies. It's about optimizing the entire diagnostic workflow, from image acquisition to final report, by intelligently routing radiologist attention where it's most needed.
Integrating these AI tools for business requires a structured AI Product Development Workflow to ensure the system meshes seamlessly with existing Picture Archiving and Communication Systems (PACS) and clinical protocols.
Actionable Takeaways
Start Small and Validate: Begin with a high-volume, well-defined task like mammogram screening or nodule detection in chest X-rays. Before full deployment, validate the AI's performance on a dataset specific to your institution's patient population and imaging equipment.
Establish Clear Protocols: Define a clear response protocol for AI-generated alerts. Determine how these findings are presented to radiologists and what steps are required for confirmation and reporting.
Track Performance Metrics: Monitor key performance indicators (KPIs) beyond basic accuracy. Track sensitivity, specificity, reduction in report turnaround time, and, most importantly, the impact on clinical outcomes. This data is crucial for demonstrating ROI and driving further adoption.
AI-powered image analysis tools like Diagnoo provide a powerful way for healthcare organizations to leverage their data, improve diagnostic precision, and ultimately enhance patient care.
2. Sepsis Risk Prediction and Early Warning Systems
Sepsis prediction is a critical and life-saving example of AI in clinical decision support systems. These advanced systems continuously analyze vast streams of data from electronic health records (EHRs), including vital signs, lab results, medications, and clinical notes. By applying machine learning models, they detect subtle, multivariate patterns that precede the onset of sepsis, often hours before a patient shows clear clinical signs.
The AI's function is to serve as an early warning system, augmenting the clinical team's vigilance. When the algorithm identifies a high-risk patient, it generates a timely alert, prompting clinicians to assess the patient and initiate early, protocol-driven care like antibiotics and fluid resuscitation. Prominent examples include systems developed by Philips, Dascena, and the in-house models at major institutions like UW Medicine and Mayo Clinic, which have demonstrated reductions in mortality rates and length of stay.
Strategic Analysis & Implementation
For healthcare leaders, the primary goal of implementing a sepsis prediction model is to drive proactive intervention rather than reactive treatment. The core business driver is the significant reduction in mortality, ICU stays, and overall treatment costs associated with severe sepsis and septic shock. By catching the condition early, the system helps prevent catastrophic clinical and financial outcomes.
Key Insight: The strategic power of sepsis AI is not merely in the prediction itself, but in its integration into the clinical workflow to trigger a standardized, rapid response. The alert is the starting point, not the conclusion; its value is realized through the actions it enables.
Successful deployment demands more than just plugging in an algorithm. It requires a thoughtful AI Product Development Workflow to integrate with the existing EHR and to manage the high volume of alerts to avoid clinician fatigue.
Actionable Takeaways
Balance Sensitivity and Specificity: Work with clinical teams to tune the alert threshold. A model that is too sensitive will cause alert fatigue and be ignored, while one that is not sensitive enough will miss critical cases. This tuning process is a crucial step in the initial implementation.
Develop a Clear Response Protocol: An AI alert must trigger a specific, non-negotiable set of actions. Define the clinical workflow for when an alert fires, including who is responsible for assessment, what steps they must take, and the timeframe for intervention.
Monitor for Model Drift: Patient populations and clinical practices change over time. Continuously monitor the model's performance (e.g., precision, recall) on new patient data to ensure it remains accurate and effective, and retrain it as necessary to prevent performance degradation.
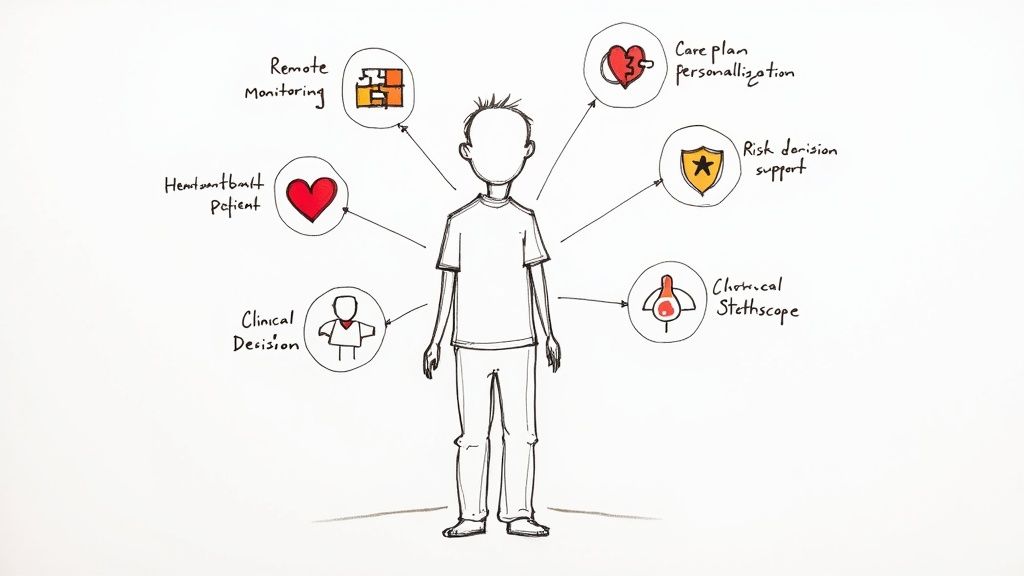
3. Cardiovascular Risk Stratification and Arrhythmia Detection
AI systems are transforming cardiology by analyzing complex cardiovascular data to predict risk and detect abnormalities. This is another powerful set of examples of AI in clinical decision support systems. These models process electrocardiograms (ECGs), patient histories, and other biometric data to identify subtle patterns indicative of conditions like arrhythmias or to forecast long-term cardiovascular risks, such as acute coronary syndrome (ACS).
These AI-powered tools augment the clinician's ability to interpret cardiac data, which is often vast and nuanced. For instance, consumer-facing devices like the Apple Watch and Kardia's portable ECGs use FDA-cleared algorithms to detect atrial fibrillation, empowering patients with early warnings. In clinical settings, companies like GE Healthcare and Philips embed sophisticated AI into ECG machines and patient monitors to provide real-time arrhythmia analysis, allowing for immediate intervention.
Strategic Analysis & Implementation
For healthcare leaders, implementing these systems is about shifting from reactive treatment to proactive risk management. The AI acts as a continuous, vigilant monitor, capable of catching transient events a standard 12-lead ECG might miss. The primary business driver is the reduction of adverse cardiac events and associated hospitalizations through early detection and preventative care, which directly impacts costs and improves patient outcomes.
Key Insight: The strategic power of AI in cardiology lies in its ability to process longitudinal data and detect subclinical signals. It moves the point of care from the hospital to the patient's daily life, creating a continuous feedback loop for managing chronic cardiovascular conditions.
Integrating these systems effectively requires a robust AI Product Development Workflow to ensure data from various sources (wearables, EMRs, clinical monitors) is harmonized and analyzed securely.
Actionable Takeaways
Define the Clinical Use Case: Start by targeting a specific challenge, such as reducing readmissions for heart failure or improving atrial fibrillation detection in an outpatient setting. Align the AI tool with a clear clinical need and workflow.
Prioritize Clinician-in-the-Loop Validation: Always implement a protocol where AI-flagged abnormalities are reviewed by a cardiologist. This builds trust, ensures patient safety, and helps refine the algorithm's performance within your specific patient population.
Measure Outcome-Based KPIs: Track metrics beyond algorithm accuracy. Focus on clinical impact, such as time-to-diagnosis for arrhythmias, reduction in stroke incidence in AFib patients, and patient engagement with monitoring tools. These metrics will demonstrate the true value and ROI of your AI solutions.
4. Oncology Treatment Planning and Prognosis Prediction
Oncology is a data-rich field, making it a prime candidate for one of the most transformative examples of AI in clinical decision support systems. These advanced platforms analyze vast, multimodal datasets, including pathology slides, genomic data, imaging results, and clinical histories. Machine learning models identify complex patterns and molecular profiles to predict cancer prognosis, recommend personalized treatment regimens, and forecast patient response to therapies like chemotherapy or immunotherapy.
Rather than offering a one-size-fits-all approach, these AI systems help oncologists stratify patients based on subtle biological markers. For instance, systems developed by companies like Tempus and Flatiron Health analyze genomic and clinical data to match patients with targeted therapies or relevant clinical trials. This augments the multidisciplinary tumor board's decision-making process, providing data-driven insights that complement clinical expertise.
Strategic Analysis & Implementation
For healthcare leaders, the strategic implementation of AI in oncology focuses on enabling precision medicine at scale. The goal is to move beyond generalized protocols and tailor treatments to each patient's unique tumor biology. A key business driver is the optimization of high-cost therapies; by predicting which patients are most likely to respond, AI can help avoid ineffective treatments, reducing costs and minimizing patient side effects.
Key Insight: The strategic value here extends beyond individual treatment plans. It involves creating a learning health system where outcomes from every patient are fed back into the model, continuously refining its predictive accuracy and generating new insights for future cancer care.
Integrating these systems requires robust data infrastructure capable of unifying structured and unstructured data from various sources, a process that can be streamlined through a structured AI Product Development Workflow.
Actionable Takeaways
Integrate with Tumor Boards: Position the AI tool as a contributor to multidisciplinary tumor board discussions, not a replacement for them. The AI's recommendations should be a data point for expert review, alongside clinical judgment and patient preferences.
Validate Against Evolving Data: Oncology is a rapidly changing field. Ensure a process is in place to continuously validate the AI’s recommendations against the latest clinical trial data and evolving standards of care.
Track Longitudinal Outcomes: Measure success by tracking long-term patient outcomes, not just initial treatment selection. Monitor metrics like progression-free survival, overall survival, and quality of life to validate the AI's predictions and demonstrate tangible clinical value.
AI-driven tools for analyzing complex oncology data, like the pathology-focused PathWise, empower clinicians to make more informed, personalized decisions, fundamentally shifting the paradigm of cancer treatment.
5. Diabetic Retinopathy and Ophthalmic Disease Detection
Detecting diabetic retinopathy and other ophthalmic diseases represents a groundbreaking application and one of the most impactful examples of AI in clinical decision support systems. These systems utilize deep learning algorithms to analyze retinal fundus photographs, identifying subtle signs of conditions like diabetic retinopathy, macular degeneration, and glaucoma with a high degree of accuracy. The AI can screen for these vision-threatening diseases often before a patient notices symptoms, enabling early intervention.
This technology is a force multiplier for public health, particularly in underserved or remote areas where access to ophthalmologists is limited. Systems like IDx-DR, the first FDA-cleared autonomous AI diagnostic, can be operated by non-specialist staff in primary care clinics. The AI provides a diagnostic result in minutes, allowing for immediate referral or reassurance and democratizing access to critical eye screening. Other prominent examples include Google AI's algorithm and Eyenuk's EyeArt system, which have been deployed in thousands of clinical sites globally.
Strategic Analysis & Implementation
For healthcare leaders, deploying this AI is about scaling preventative care and moving diagnostics to the point of care. The business driver is the prevention of blindness through early, accessible screening, which dramatically reduces long-term healthcare costs associated with vision loss. By integrating this screening into routine primary care visits for diabetic patients, organizations can improve adherence to care guidelines and close significant care gaps.
Key Insight: The strategic power of AI in ophthalmology lies in its autonomy. It uncouples a highly specialized diagnostic task from the specialist, enabling widespread, low-cost screening that can fundamentally change public health outcomes for chronic diseases like diabetes.
Integrating this AI requires a well-defined AI Product Development Workflow to establish clear protocols for image acquisition, data privacy, and referral pathways for patients flagged by the system.
Actionable Takeaways
Prioritize Image Quality: Implement rigorous training and protocols for staff on using the fundus camera. Consistent, high-quality images are essential for the AI's diagnostic accuracy. Validate that your imaging equipment and procedures meet the algorithm's requirements.
Establish Clear Referral Pathways: Before going live, create a seamless and reliable process for patients who receive a positive screening result. Define how and when they will be referred to an ophthalmologist for a comprehensive, dilated eye exam and follow-up care.
Validate on Local Demographics: Test the AI's performance on a data set from your own patient population. This ensures the algorithm is not biased and performs accurately with the specific demographic and clinical characteristics of the community you serve. This step is a critical part of a thorough AI requirements analysis.
6. Acute Kidney Injury (AKI) Prediction and Progression Monitoring
Predicting acute kidney injury (AKI) is a critical and time-sensitive challenge, making it one of the most promising examples of AI in clinical decision support systems. These systems analyze real-time patient data streams, including electronic health records, lab values, vital signs, and medication lists. Using machine learning models, the AI identifies complex patterns that precede AKI onset, often predicting risk hours or even days before standard clinical criteria, like a rise in serum creatinine, are met.
This technology empowers clinicians to intervene proactively rather than reactively. By providing early warnings, the system enables preventive measures such as adjusting medications, optimizing fluid management, and avoiding nephrotoxic agents. For instance, systems developed by Duke University and the U.S. Department of Veterans Affairs have demonstrated the ability to flag at-risk patients in perioperative and intensive care settings, allowing for timely nephrology consults and care adjustments that can prevent or mitigate kidney damage.
Strategic Analysis & Implementation
For clinical leaders, the primary goal of an AKI prediction system is to shift the paradigm from treatment to prevention. The business driver is the significant reduction in costs associated with treating established AKI, which includes longer hospital stays, dialysis, and higher rates of morbidity and mortality. The AI acts as a vigilant, always-on monitor, identifying subtle deteriorations in kidney function that human-led reviews might miss amidst a flood of other clinical data.
Key Insight: The strategic power of AKI prediction AI lies in its ability to translate data into pre-emptive clinical action. It's not just about flagging a risk score; it's about integrating that alert into a standardized clinical workflow that triggers specific, evidence-based interventions.
Deploying such a system demands a robust AI Product Development Workflow to ensure the model is tuned to the organization's specific patient demographics and clinical data infrastructure, enabling reliable and actionable alerts within existing EMR platforms.
Actionable Takeaways
Integrate with Medication Systems: Ensure AI-generated AKI alerts are directly integrated with the electronic prescribing and medication administration record. This allows the system to automatically flag potentially nephrotoxic drugs for review when a patient's risk profile increases.
Develop Tiered Response Protocols: Create clear, tiered clinical protocols based on the AI-generated risk score. A low-risk alert might trigger enhanced monitoring, while a high-risk alert could mandate an immediate nephrology consultation and a review of the patient's fluid balance.
Monitor Leading Indicators: Track process metrics beyond AKI incidence. Monitor the rate of protocol adherence, time-to-intervention following an alert, and changes in prescribing patterns for nephrotoxic agents. These KPIs provide early evidence of the system's impact on clinical practice before outcome data matures.
7. Natural Language Processing for Clinical Note Analysis and Risk Extraction
A significant portion of critical patient data is trapped within unstructured text, like clinical notes, discharge summaries, and specialist reports. Natural Language Processing (NLP) is one of the most transformative examples of AI in clinical decision support systems because it unlocks this data. These systems parse free-text documents to extract key clinical concepts, identify risk factors, and detect potential adverse events that are not recorded in structured fields.
This technology acts as an intelligent layer over the electronic health record (EHR). For example, NLP models can scan a patient's entire history to identify undocumented allergies mentioned in a past consultation note or flag social determinants of health, like housing instability, that are critical for care planning. Major EHR providers like Cerner and Epic are integrating NLP to assist with documentation, while tools like Stanford's MedCAT demonstrate its power in research and clinical concept extraction. For building similar capabilities, organizations often look into custom healthcare software development.
Strategic Analysis & Implementation
For healthcare leaders, NLP represents a bridge between unstructured narrative and actionable data. The primary business driver is risk mitigation; by systematically identifying information like potential drug interactions or contraindications buried in notes, organizations can prevent adverse events and improve patient safety. It also enhances clinical trial recruitment by finding eligible patients based on nuanced criteria described in their records.
Key Insight: The strategic power of NLP is not just text-to-data conversion. It's about creating a comprehensive, longitudinal patient profile that incorporates the rich context and detail from clinician narratives, which is often lost in standardized EHR fields.
Successful implementation hinges on integrating this technology directly into clinical workflows without adding to the documentation burden. A robust AI-powered data extraction engine can automate this process, ensuring that insights are surfaced at the point of care.
Actionable Takeaways
Prioritize High-Risk Use Cases: Begin with applications that have a clear impact on patient safety, such as identifying undocumented allergies, flagging potential medication contraindications, or detecting signs of patient deterioration described in nursing notes.
Implement a Human-in-the-Loop Protocol: NLP is powerful but not infallible. Establish a clear workflow where clinicians review and validate critical findings extracted by the AI before they are added to the structured patient record or trigger an alert.
Validate on Local Data: Before full deployment, validate the NLP model’s accuracy on a representative sample of your own institution’s clinical notes. Clinical language and abbreviations can vary significantly between organizations, affecting model performance.
8. Antimicrobial Stewardship Decision Support
Antimicrobial stewardship is a critical area where AI is providing immense value, making it one of the most important examples of AI in clinical decision support systems. These systems analyze vast datasets, including patient microbiology results, culture sensitivities, renal function, and clinical presentation to recommend the most appropriate antibiotic selection, dosing, and duration. By doing so, they combat the growing threat of antimicrobial resistance.
Machine learning models are trained to predict which patients will respond to narrower-spectrum antibiotics and identify optimal moments to de-escalate or discontinue therapy. This moves beyond simple rule-based alerts to a more nuanced, personalized approach. For example, AI tools used by UnitedHealth Group and academic medical centers like the University of Michigan can analyze patterns in real-time to guide clinicians away from unnecessary broad-spectrum antibiotics, directly reducing the risk of resistant organism development and C. difficile infections.
Strategic Analysis & Implementation
For healthcare leaders, the strategic implementation of these AI systems is about shifting from reactive to proactive stewardship. The AI serves as a vigilant partner to infectious disease specialists and pharmacists, providing data-driven recommendations that reinforce best practices at the point of care. The core business drivers are improved patient outcomes, reduced pharmacy costs, and lower rates of hospital-acquired infections, which carry significant financial penalties.
Key Insight: The strategic power of AI in antimicrobial stewardship lies in its ability to individualize recommendations at scale. It synthesizes complex patient-specific variables that a human cannot process simultaneously, ensuring the right drug is used for the right duration for every single patient, every time.
Successfully integrating these tools requires a robust AI Product Development Workflow that connects the AI to microbiology lab information systems (LIS), the electronic health record (EHR), and pharmacy systems for a seamless flow of information.
Actionable Takeaways
Integrate with Lab and Pharmacy Data: Ensure the system has real-time access to microbiology culture results, sensitivity reports, and patient-specific data like creatinine clearance. This data is the lifeblood of accurate AI-driven recommendations.
Establish a Clinician-in-the-Loop Protocol: Create clear workflows for how AI recommendations are reviewed, approved, or overridden by infectious disease specialists or clinical pharmacists. The AI should augment, not dictate, clinical judgment.
Track Stewardship-Specific KPIs: Monitor metrics beyond antibiotic costs. Track the prevalence of resistant organisms (e.g., MRSA, VRE), rates of C. difficile infection, patient length of stay, and readmission rates for infections. This data will demonstrate the tool's clinical and financial ROI.
Tools that provide this level of insight are essential for modernizing patient safety and resource management, reflecting a sophisticated application of AI Automation as a Service in a clinical setting.
8-Point Comparison: AI in Clinical Decision Support
| AI Application | Implementation Complexity | Resource Requirements | Expected Outcomes | Ideal Use Cases | Key Advantages |
|---|---|---|---|---|---|
| Radiology Image Analysis and Diagnostic Support | High — requires imaging pipelines, PACS integration and regulatory validation | Large curated imaging datasets, GPU compute, radiologist annotations, PACS/EHR integration | Improved detection (≈5–15% gain as second reader), faster reports, reduced workload; risk of false positives | High-volume imaging tasks, triage, second-reader workflows, screening in resource-limited settings | Scalable multi‑modality processing, real‑time lesion detection and segmentation |
| Sepsis Risk Prediction and Early Warning Systems | Medium–High — continuous data streaming and alerting integration with EHR | Continuous vitals, labs, complete EHR data, labeled sepsis outcomes, clinical workflow design | Earlier detection (mortality reductions reported 10–40%), shorter ICU stays; potential alert fatigue | ICU/ward monitoring, hospitals with mature EHRs, early‑warning systems | Time‑to‑event risk scoring and actionable alerts enabling earlier intervention |
| Cardiovascular Risk Stratification and Arrhythmia Detection | Medium — ECG/echo and wearable device integration, waveform analytics | High‑quality ECG/echo datasets, device connectivity, cardiology oversight | Increased arrhythmia detection and faster triage; improved remote monitoring; variable accuracy with signal quality | ED triage, ambulatory/wearable monitoring, screening high‑risk patients | Real‑time waveform analysis, portable/wearable detection, triage support |
| Oncology Treatment Planning and Prognosis Prediction | Very high — multi‑modal data fusion, genomics and pathology integration, multidisciplinary validation | Genomic and pathology data, longitudinal outcomes, expert tumor boards, compute for complex models | Personalized treatment recommendations and prognosis predictions; risk of outdated or biased recommendations | Precision oncology centers, tumor boards, complex treatment planning | Integrates imaging, pathology and genomics for individualized therapy and outcome prediction |
| Diabetic Retinopathy and Ophthalmic Disease Detection | Medium — imaging capture workflows and quality control; possible autonomous deployment | High‑quality fundus images, calibrated cameras, trained capture staff, validated models | Near‑ophthalmologist sensitivity/specificity for screening; expands access and reduces unnecessary referrals | Primary care/pharmacy screening, population screening in low‑resource settings | Autonomous screening at scale, FDA‑cleared options, prevents vision loss via early detection |
| Acute Kidney Injury (AKI) Prediction and Progression Monitoring | Medium — EHR lab and medication integration, trending and alert workflows | Frequent lab monitoring, meds and vitals data, nephrology pathways for escalation | Early AKI identification (30–50% cases before creatinine rise), reduced progression and dialysis need if acted on | ICU, perioperative care, high‑risk hospitalized patients | Early warning enabling preventive measures (fluid/medication adjustments) and reduced AKI severity |
| NLP for Clinical Note Analysis and Risk Extraction | Medium–High — domain‑specific NLP pipelines, de‑identification and model tuning | Large annotated clinical text corpora, privacy controls, transformer compute resources | Extracts concepts from unstructured notes, improves coding accuracy, identifies safety signals; variable accuracy by note type | Coding/billing improvement, pharmacovigilance, population health analytics, documentation assistance | Unlocks narrative data, automates concept extraction and coding, surfaces hidden clinical insights |
| Antimicrobial Stewardship Decision Support | Medium — microbiology LIS and clinical context integration, stewardship workflow alignment | Rapid lab/culture data, susceptibility databases, clinician/ID specialist input | Reduced broad‑spectrum antibiotic use, optimized dosing/duration, decreased resistance and ADRs (with timely lab data) | Hospitals with stewardship programs, labs capable of rapid culture and susceptibility testing | Supports de‑escalation, renal dosing, and targeted therapy to meet stewardship goals |
Integrating AI into Your Clinical Workflow: The Strategic Path Forward
The real-world examples of AI in clinical decision support systems detailed in this article, from radiology and sepsis prediction to oncology and antimicrobial stewardship, illustrate a fundamental shift in healthcare. We are moving beyond theoretical potential and into an era of tangible, data-driven clinical enhancement. These systems are no longer futuristic concepts; they are active components in the modern care delivery model, augmenting human expertise to improve patient outcomes, enhance operational efficiency, and reduce cognitive load on clinicians. The recurring theme across these successful implementations is not just the sophistication of the algorithms, but the strategic, thoughtful integration into existing clinical workflows.
The journey from a promising AI model to a trusted clinical tool is a complex one, demanding more than just technical prowess. It requires a deep understanding of the clinical environment, a robust data infrastructure, and an unwavering commitment to patient safety and data privacy. Organizations that succeed are those that view AI not as a plug-and-play technology, but as a strategic capability that must be carefully cultivated through services like AI strategy consulting.
From Insight to Impact: Key Strategic Takeaways
Reflecting on the diverse applications we've explored, several core principles emerge as critical for success. These are the strategic pillars upon which effective AI-powered clinical decision support is built:
Problem-First, Not Technology-First: The most impactful AI solutions, like the sepsis and AKI prediction models, start with a clearly defined clinical problem. They don't search for a problem to fit a technology. Leaders must prioritize use cases that address significant pain points, such as high mortality rates, diagnostic delays, or resource-intensive manual processes.
Human-in-the-Loop by Design: Successful AI in healthcare is not about replacing clinicians but empowering them. The best systems, from diagnostic imaging assistants to treatment planners, are designed as collaborative tools. They present insights, evidence, and risk scores, but the final decision remains firmly in the hands of the trained medical professional. This approach builds trust and ensures clinical context is never lost.
Data Governance as the Foundation: The performance of any AI model is inextricably linked to the quality and security of the data it's trained on. Establishing rigorous data governance protocols is non-negotiable. This includes ensuring data integrity, managing patient consent, and protecting against the rising threat of infostealer malware and data leaks that specifically target sensitive health information.
Measure, Iterate, and Adapt: The launch of an AI tool is the beginning, not the end. Continuous monitoring of model performance, clinical utility, and user feedback is essential. As we explored in our guide to the AI Product Development Workflow, an iterative approach allows for ongoing refinement and ensures the system remains effective and relevant as clinical practices evolve.
Your Actionable Roadmap for AI Integration
Translating these strategic insights into action requires a clear, phased plan. For business and technology leaders charting a course for AI adoption, the path forward involves several key steps.
Conduct a Strategic Assessment: Begin with a comprehensive AI requirements analysis to identify the most promising opportunities within your organization. Evaluate your data readiness, technical infrastructure, and clinical workflows to pinpoint where AI can deliver the greatest value.
Develop a Pilot Program: Select a high-impact, well-defined use case for a pilot project. This allows you to test the technology in a controlled environment, gather clinician feedback, and build a strong business case for broader implementation with a Custom AI Strategy report.
Engage Clinical Champions: Involve clinicians from the very beginning of the process. Their expertise is invaluable for defining requirements, validating models, and driving adoption. Appointing dedicated clinical champions ensures the solution is built for and with its end-users.
Prioritize Change Management: Technology is only one part of the equation. A comprehensive change management strategy that includes training, communication, and clear workflow integration plans is critical for ensuring clinicians trust and effectively utilize the new AI tools.
The transformative power of AI in healthcare is undeniable. By leveraging these real-world use cases as a blueprint and adopting a strategic, clinician-centric approach, your organization can move from aspiration to application, building a future where technology and human expertise combine to deliver a higher standard of care.
Frequently Asked Questions (FAQ)
What is an AI clinical decision support system?
An AI clinical decision support system (CDSS) is an advanced software tool that uses artificial intelligence, particularly machine learning and natural language processing, to analyze large volumes of patient data. It provides clinicians with real-time, evidence-based recommendations, alerts, and insights to enhance diagnostic accuracy, personalize treatment plans, and improve patient outcomes.
How is AI used in clinical decision-making?
AI assists clinical decision-making by identifying complex patterns in data that humans might miss. For example, it can analyze medical images to detect early signs of disease, predict a patient's risk of developing a condition like sepsis, recommend optimal drug therapies based on genomic data, and extract critical information from unstructured clinical notes. It acts as a co-pilot, augmenting the clinician's expertise.
What are some real-world examples of AI in CDSS?
Key examples include AI systems for radiology image analysis (detecting tumors), sepsis risk prediction in hospitals, cardiovascular arrhythmia detection from ECGs, personalized oncology treatment planning, and autonomous screening for diabetic retinopathy from retinal photos.
What are the main benefits of using AI in clinical decision support?
The primary benefits include improved diagnostic accuracy and speed, earlier detection of life-threatening conditions, personalized and more effective treatment plans, enhanced operational efficiency in hospitals, and a reduction in medical errors. Ultimately, it leads to better patient safety and outcomes.
Are there challenges to implementing AI in healthcare?
Yes, challenges include ensuring data privacy and security, integrating AI tools with existing electronic health records (EHRs), overcoming clinician resistance to new technology, managing potential algorithmic bias, and meeting strict regulatory requirements. A well-defined AI strategy consulting tool can help navigate these complexities.
Ready to move from theory to practice? At Ekipa AI, we specialize in helping healthcare organizations navigate the complexities of AI implementation, from initial strategy to full-scale deployment. Let our expert team help you build a custom roadmap to harness the power of AI and transform your clinical decision support capabilities.