AI in Medical Healthcare Transformation
Discover how AI in medical applications is revolutionizing patient care. Learn about AI-driven diagnostics, operational efficiency, and future trends.
For a long time, AI in medicine felt like something out of science fiction. That's not the case anymore. It has officially moved from a far-off concept to a practical tool that's actively reshaping patient care and hospital operations.
The key thing to understand is that AI isn't here to replace doctors and nurses. Instead, it's becoming an incredibly powerful partner, augmenting their skills and expertise. This collaboration between human experience and machine intelligence is quickly setting a new standard for what great healthcare looks like.
The New Reality of AI in Medical Care
For healthcare organizations, the arrival of AI means it's time to rethink some long-standing processes. Think about it: AI can analyze massive datasets in a way no human ever could. This allows it to spot subtle patterns in medical images, help predict patient outcomes, or even just streamline the mountain of administrative work that bogs things down.
The real goal is to free up clinicians from tedious, repetitive tasks. By letting AI handle the heavy lifting on data, doctors and nurses can focus on what they do best—making complex decisions and connecting with their patients. You can learn more about how we support this transition in our overview of AI for the healthcare industry.
The Collaborative Future of Medicine
This new chapter in medicine is all about the synergy between skilled professionals and intelligent systems. It’s a partnership where technology amplifies human talent.
The infographic below does a great job of illustrating this dynamic, showing how a clinician's expertise is magnified by AI's analytical power.
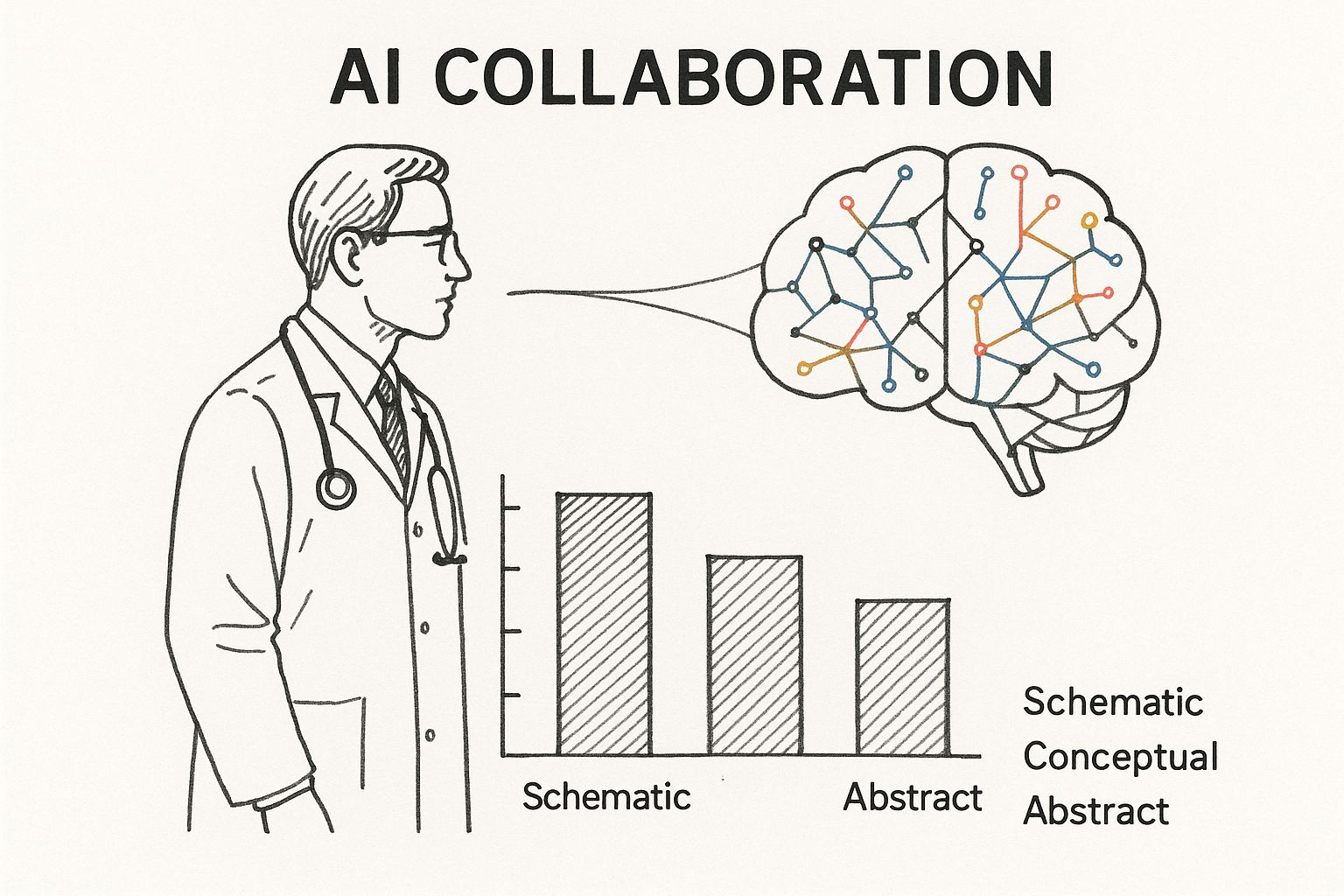
As you can see, the idea is for AI to handle the immense task of processing data, which in turn allows clinicians to apply their experience and empathy where it counts the most. This is the foundation for advancing modern medicine.
The momentum behind this shift is impossible to ignore. The global AI healthcare market is on track to blow past $120 billion by 2028. Even now, 86% of healthcare organizations report that they are already using AI extensively to improve their services.
This rapid adoption isn't just hype; it's driven by real, tangible benefits across the entire healthcare spectrum:
- Smarter Diagnostics: AI algorithms can analyze medical images like X-rays and MRIs with incredible precision, often spotting early signs of disease that might be missed by the human eye alone.
- Personalized Treatment Plans: By analyzing a patient's unique genetic makeup and health history, AI can help doctors craft customized treatment plans that are more effective and produce fewer side effects.
- Streamlined Operations: AI is a game-changer for administrative tasks. It can automate scheduling, billing, and record-keeping, which helps cut costs and reduce the all-too-common problem of staff burnout.
At the end of the day, bringing AI into medical settings is about giving providers better tools to improve and save lives. It's about empowering them to do their jobs better, faster, and with more insight than ever before.
How AI Is Sharpening Medical Diagnostics
One of the biggest ways AI is changing healthcare is by giving us a powerful microscope for data. It can sift through massive amounts of information—far more than any human could—to find subtle patterns that would otherwise go unnoticed. This is especially true in medical imaging, where catching something early can make all the difference.

Imagine a radiologist looking at a chest X-ray. Their expertise comes from years of training and experience in spotting abnormalities. Now, think about an AI model trained on millions of scans. It learns to pick up on the faintest signals of a developing tumor or the very first signs of pneumonia, long before they become obvious. This is how we start shifting diagnostics from being reactive to truly proactive.
Seeing Beyond the Naked Eye in Medical Imaging
The real power of AI in imaging is its relentless consistency. It never gets tired at the end of a long shift, and its "eye" for detail is always razor-sharp. For both doctors and patients, this brings some very real benefits.
- Higher Accuracy: AI algorithms can flag suspicious spots on scans with incredible precision, acting as a reliable second set of eyes for radiologists and helping to cut down on human error.
- Faster Diagnosis: By handling the initial review of images, AI helps prioritize the most urgent cases. This can dramatically shorten the anxious wait time for patients needing results.
- Catching Diseases Earlier: AI is brilliant at noticing tiny changes in a series of scans taken over time, which is essential for tracking chronic diseases or catching cancer at its most treatable stage.
This is exactly where tools like our own specialized diagnostic platform, Diagnoo, come into play. They give clinicians the backup they need to make faster, more confident decisions.
By analyzing complex visual data, AI isn't just making old diagnostic methods better; it's unlocking a level of insight that simply wasn't possible before, leading directly to better patient outcomes.
From Pixels to Personalized Medicine
But AI's diagnostic skill isn't just about images. It's also making huge leaps in genomics—the study of a person's complete DNA. The human genome is packed with billions of data points, a mountain of information that's impossible for any person to analyze by hand.
AI algorithms, on the other hand, can chew through all that genetic data to find specific markers linked to diseases like Alzheimer's or certain types of cancer. This allows medicine to move away from a one-size-fits-all approach. For instance, by analyzing a tumor's unique genetic signature, AI can help an oncologist choose the most effective targeted therapy, boosting treatment success while minimizing side effects.
A New Standard in Diagnostic Performance
The benefits of bringing AI into the diagnostic workflow are clear. As machine learning algorithms get better and better at spotting patterns, they provide more reliable support for clinicians every day. To really see the difference, it helps to compare the old way with the new.
Comparing Traditional vs AI-Powered Medical Diagnostics
This table breaks down the key differences between how diagnostics have traditionally been done and how they look when enhanced by artificial intelligence.
Metric Traditional Diagnostic Methods AI-Powered Diagnostics
Speed
Can take hours or even days, depending on the clinician's workload and the case's complexity.
Delivers an initial analysis in minutes or seconds, flagging critical cases for immediate review.
Accuracy
Relies on individual expertise and is subject to human error or fatigue.
Offers consistently high accuracy, backed by training on massive, diverse datasets.
Scope
Limited to visible patterns and what a clinician already knows.
Can spot subtle, complex patterns across imaging, genomics, and patient history.
Data Handling
Involves the manual review of a limited number of data points at one time.
Processes and connects millions of data points simultaneously to find deeper insights.
Ultimately, bringing AI into diagnostics isn't about replacing doctors. It’s about giving them supercharged tools that amplify their expertise. This partnership between human intuition and machine intelligence is setting a much higher standard of care—one where diagnoses are faster, more accurate, and more personalized than ever before.
Streamlining Hospital Operations with AI
While everyone's talking about AI's flashy role in diagnostics, its real workhorse application is happening behind the scenes, tackling the operational grind of healthcare. Think about the mountain of administrative tasks that slow hospitals down and lead to serious staff burnout. AI is chipping away at that mountain, freeing up clinicians to focus on what they do best: care for patients.
The administrative load in any medical facility is staggering—scheduling, billing, supply chain, bed management, you name it. AI injects a layer of intelligence into these processes, turning manual, error-prone chores into automated, efficient systems. This is where you see the practical power of workflow automation making a tangible difference.
Optimizing the Patient Journey from Start to Finish
One of the first places you'll see an impact is in managing patient flow. Hospitals are in a constant state of juggling acts with appointments, admissions, and discharges. A single snag can create a domino effect, leading to long waits and frustrated people.
AI-powered systems can look at historical patterns and real-time data to smooth out these wrinkles:
- Intelligent Scheduling: Instead of a person trying to fit puzzle pieces together, an AI can manage appointment calendars. It considers doctor availability, room usage, and even a patient's clinical urgency to create a schedule that actually works, minimizing delays.
- Predictive Bed Management: AI models are getting remarkably good at forecasting admissions and discharges. This gives hospitals a heads-up on bed demand, so they can reduce those frustrating bottlenecks when a patient is ready to be transferred but no bed is available.
- Automated Medical Coding: This is a classic time-sink, and human error can be costly. AI tools can scan a clinician's notes and suggest the right billing codes, which means faster, more accurate revenue cycles.
By automating these core operational tasks, hospitals don't just run more smoothly. They create a better, less stressful experience for everyone involved, from the front desk to the patient's bedside. It's about trading administrative friction for more meaningful clinical interactions.
Building a More Efficient Healthcare Ecosystem
The benefits of operational AI ripple out across the entire hospital infrastructure. Take resource management, a constant challenge for any large facility. AI can provide the foresight needed to make smarter calls. Predictive analytics can forecast the need for specific supplies, preventing shortages of critical equipment or medication while also cutting down on the waste from overstocking. It’s a data-driven approach that gets resources exactly where they need to go.
This has a direct, positive effect on staff morale, too. When nurses and administrators are liberated from endless paperwork and scheduling headaches, they feel less overwhelmed and can connect more with their work's purpose. For a deeper dive, check out this expert guide to knowledge management and artificial intelligence.
This isn't just a future-state dream; it's happening now. It’s projected that by 2025, a staggering 80% of hospitals will be using AI to get a handle on both patient care and their own internal tooling. It just makes sense.
Navigating the Hurdles of AI Adoption
While the promise of AI in medical fields is enormous, getting there isn't a simple plug-and-play affair. Healthcare is a uniquely complex and heavily regulated world. Dropping powerful new technology into this environment requires navigating some serious obstacles. From data privacy to clunky old systems, these challenges have to be tackled head-on for any AI project to get off the ground.
Successfully bringing AI into a clinical setting is all about smart planning and execution. This is especially true when it comes to implementing effective change management processes. It’s not just about the tech—it's about getting your people and your workflows ready for a new way of doing things.
Ensuring Data Privacy and Security
In healthcare, nothing is more sacred than patient data. Any AI system that touches this information has to be built on a bedrock of iron-clad security and rigid compliance with regulations like HIPAA. There's simply no room for error.
Here's the catch: AI models, especially machine learning algorithms, are hungry for data. They need massive amounts of it to learn and become effective. This creates a high-stakes balancing act. How do you feed the AI the data it needs to perform without ever putting patient confidentiality at risk?
This is where strong governance comes into play. Key strategies include:
- Data Anonymization: This involves scrubbing all personally identifiable information from datasets before the AI ever sees them.
- Federated Learning: A clever approach where the AI model is trained on-site at a local hospital or on a device, meaning the sensitive data never leaves its secure home.
- Strict Access Controls: Making sure that only the right people have the keys to the AI systems and the data they handle.
The Risk of Algorithmic Bias
An AI is a reflection of the data it learns from. If that data is biased or isn't diverse, the AI's decisions will be just as skewed. In a hospital, that’s not just a flaw—it's dangerous. It could lead to misdiagnoses or poorer outcomes for underrepresented groups of patients.
Think about it: an AI trained to spot skin cancer almost exclusively on data from light-skinned individuals might completely miss it on darker skin tones. Fighting this bias demands a conscious effort to source inclusive data and constantly check the model for fairness. As we explored in our AI adoption guide, trust in AI starts with making sure it works for everyone.
Overcoming bias isn’t just a technical problem; it's an ethical imperative. It demands a conscious effort to build and validate AI tools with diverse, representative datasets to ensure equitable care for all patients.
Integrating with Legacy Systems
Walk into most hospitals, and you'll find IT systems that have been running for decades. These legacy platforms were never built to talk to modern, cloud-based AI tools. Trying to connect them can feel like plugging a USB-C cable into a floppy disk drive—they just don't speak the same language.
This integration headache is one of the biggest roadblocks out there. It causes delays, balloons budgets, and creates a lot of frustration. The only way through it is with a solid technical plan, which often means building custom software bridges to connect the old with the new. This is exactly where deep AI strategy consulting becomes invaluable. A good strategy anticipates these issues and maps out a phased integration that won't bring daily operations to a halt. Working with a team that has real experience in healthcare software development ensures you get these tricky integrations right from day one.
Your Roadmap to Integrating Medical AI
Bringing AI into a medical setting isn't a flip-of-a-switch event; it's a carefully planned journey. For healthcare leaders looking to get started, having a clear roadmap can turn a daunting challenge into a series of achievable steps. The idea is to move deliberately from an initial idea to a fully integrated system, making sure each step builds on the last.
But this process doesn't start with technology—it starts with strategy. Before you even think about algorithms, you have to pinpoint the specific, high-impact problems you need to solve. Are you trying to cut down diagnostic wait times? Make patient scheduling less of a headache? Or get a better handle on bed management? Zeroing in on clear pain points ensures your first AI projects deliver real, tangible results.
Phase 1: Identify High-Impact Use Cases
The smartest AI integrations start small and focused. Instead of trying to overhaul everything at once, find a few key areas where AI can make the biggest impact with the least amount of friction. A great way to get ideas is to explore established real-world use cases to see what’s already working out there.
Here are a few good places to start looking:
- Administrative Drag: Think about all the repetitive, time-sucking tasks. Using AI for medical coding, scheduling appointments, or handling billing can free up your staff and deliver a quick, measurable return through workflow automation.
- Clinical Support: Focus on tools that assist clinicians, not replace them. An AI-powered image analysis tool that flags potential issues for a radiologist to review is a perfect example of technology amplifying human expertise.
- Operational Bottlenecks: Where do things get stuck in your facility? Predictive analytics can help manage patient flow or resource allocation, improving both efficiency and the patient experience almost right away.
This initial discovery phase is everything. A deep understanding of your organization's unique needs will guide every decision you make down the line, from data preparation to choosing the right partner. It's the absolute foundation of effective AI strategy consulting.
Phase 2: Plan a Phased Rollout with Pilot Projects
Once you’ve locked onto a promising use case, it’s time to launch a pilot project. Think of a pilot as a small-scale, controlled experiment. It’s designed to prove the technology's value and iron out the kinks before you commit to a full-scale rollout. This is your chance to score a clear win and get crucial buy-in from everyone, from clinical staff to the C-suite.
A well-run pilot project is both a proof-of-concept and a priceless learning opportunity. It keeps risk low while showing concrete benefits early on, which is the best way to build momentum for long-term success.
This phased approach is central to a successful AI Product Development Workflow. It lets your organization adapt and learn without throwing daily operations into chaos. One non-negotiable part of this phase is a thorough data readiness assessment. AI models are only as good as the data they learn from, so you have to ensure your data is clean, accessible, and relevant.
Phase 3: Choose the Right Partners and Technology
With a successful pilot in your back pocket, you’ll have the credibility and momentum to scale up. Now is the time to select your long-term technology partners and the right AI tools for business. Your decision should be guided by your specific needs, how well the new tech can integrate with your existing systems (like your EHR), and the level of support the vendor provides.
Whether you need a Custom AI Strategy report to guide your thinking or end-to-end healthcare software development, it's critical to partner with a team that gets both AI and the unique pressures of the medical world.
Finally, never forget the human element. Change is hard, and solid change management is essential. A successful rollout includes training and ongoing support to make sure your clinical staff feels confident and empowered by the new technology, not threatened by it.
Ultimately, the goal of implementing AI Solutions is to create a system where technology and human expertise work together, seamlessly. By following a structured roadmap, you can navigate the complexities and unlock AI's full potential to improve patient care. And to make this journey a success, you need the right people in your corner—which is why working with our expert team can make all the difference.
Frequently Asked Questions About AI in Medical Fields
Whenever we talk about bringing AI into medical settings, many questions arise from doctors, administrators, and patients alike. Understanding what this technology can and cannot do is crucial for building trust and ensuring responsible adoption. Here are answers to some of the most common questions.
Will AI Replace Doctors and Nurses?
No. The primary goal of AI in medicine is not to replace clinicians but to augment their abilities. AI excels at processing vast amounts of data and handling repetitive tasks, which frees up healthcare professionals to focus on critical thinking, complex decision-making, and empathetic patient care—skills that are uniquely human. AI acts as a powerful assistant, enhancing expertise rather than rendering it obsolete.
What Are the Biggest Ethical Concerns with AI in Healthcare?
The main ethical concerns revolve around data privacy, algorithmic bias, and accountability.
- Data Privacy: AI models require large datasets, making the protection of sensitive patient information paramount. This involves strict governance, data anonymization, and adherence to regulations like HIPAA.
- Algorithmic Bias: If an AI is trained on non-diverse data, its predictions may be inaccurate for underrepresented populations, potentially worsening health disparities.
- Accountability: Determining responsibility when an AI-assisted diagnosis is incorrect—whether it lies with the developer, the hospital, or the clinician—is a complex legal and ethical challenge.
How Can a Small Clinic Start Using AI?
Smaller practices can begin by implementing solutions with a high impact and low complexity. A good starting point is AI Automation as a Service for administrative tasks like scheduling, billing, and patient communications. These tools often integrate with existing practice management software, offering a quick return on investment by improving workflow automation. Another approach is to start a small pilot project focusing on a specific clinical need, such as an AI tool for image analysis.
What Is the Difference Between AI and Machine Learning in Medicine?
Artificial Intelligence (AI) is the broader concept of creating intelligent systems capable of performing tasks that typically require human intelligence. Machine Learning (ML) is a subset of AI where systems learn from data to identify patterns and make decisions without being explicitly programmed. Most practical medical AI applications today, such as diagnostic tools that analyze scans, are powered by machine learning algorithms.
The journey to weaving AI into healthcare is full of exciting opportunities and important decisions. Partnering with our expert team can give you the clarity and strategic direction you need to navigate this journey successfully, making sure technology always serves the ultimate goal: improving human health.
At Ekipa AI, we specialize in turning complex AI opportunities into scalable, real-world impact. Our next-generation strategy platform helps you uncover and execute your AI transformation, delivering tailored strategies without the traditional consulting overhead. Learn how we can help you build your AI roadmap at https://www.ekipa.ai.