AI Revenue Cycle Management Unlocked
Discover how AI revenue cycle management transforms healthcare finances. Learn practical strategies to boost efficiency, cut costs, and improve patient care.
Picture your healthcare organization's revenue cycle. Now, imagine it's not a disjointed series of manual tasks but a smart, self-correcting system. That's the real promise of AI revenue cycle management (RCM). This technology isn't just about simple automation; it digs in to solve the core financial headaches in healthcare, making financial stability a much more attainable goal.
Why AI Is Reshaping Healthcare Finance
Think of the old way of managing revenue as navigating with a paper map. It gets the job done, but it’s slow, tedious, and a single wrong turn can get you completely lost. AI-powered RCM, on the other hand, is like having a real-time GPS that spots financial traffic jams—like a sudden spike in claim denials—and reroutes you to get paid faster.
This is a fundamental shift from just reacting to problems to proactively managing your organization's financial health. Intelligent automation and predictive analytics are no longer nice-to-haves; they're essential for survival and growth in this industry.
The Financial Imperative Driving Adoption
The numbers tell a compelling story. The global market for AI in RCM was valued at around USD 20.63 billion in 2024. Projections show it soaring to USD 70.12 billion by 2030, which is a compound annual growth rate of roughly 24.16%. What's fueling this? A perfect storm of increasingly complex insurance claims and the industry-wide move toward value-based care.
This infographic paints a clear picture of the efficiency gains, showing the stark difference between manual processing and an AI-driven approach.
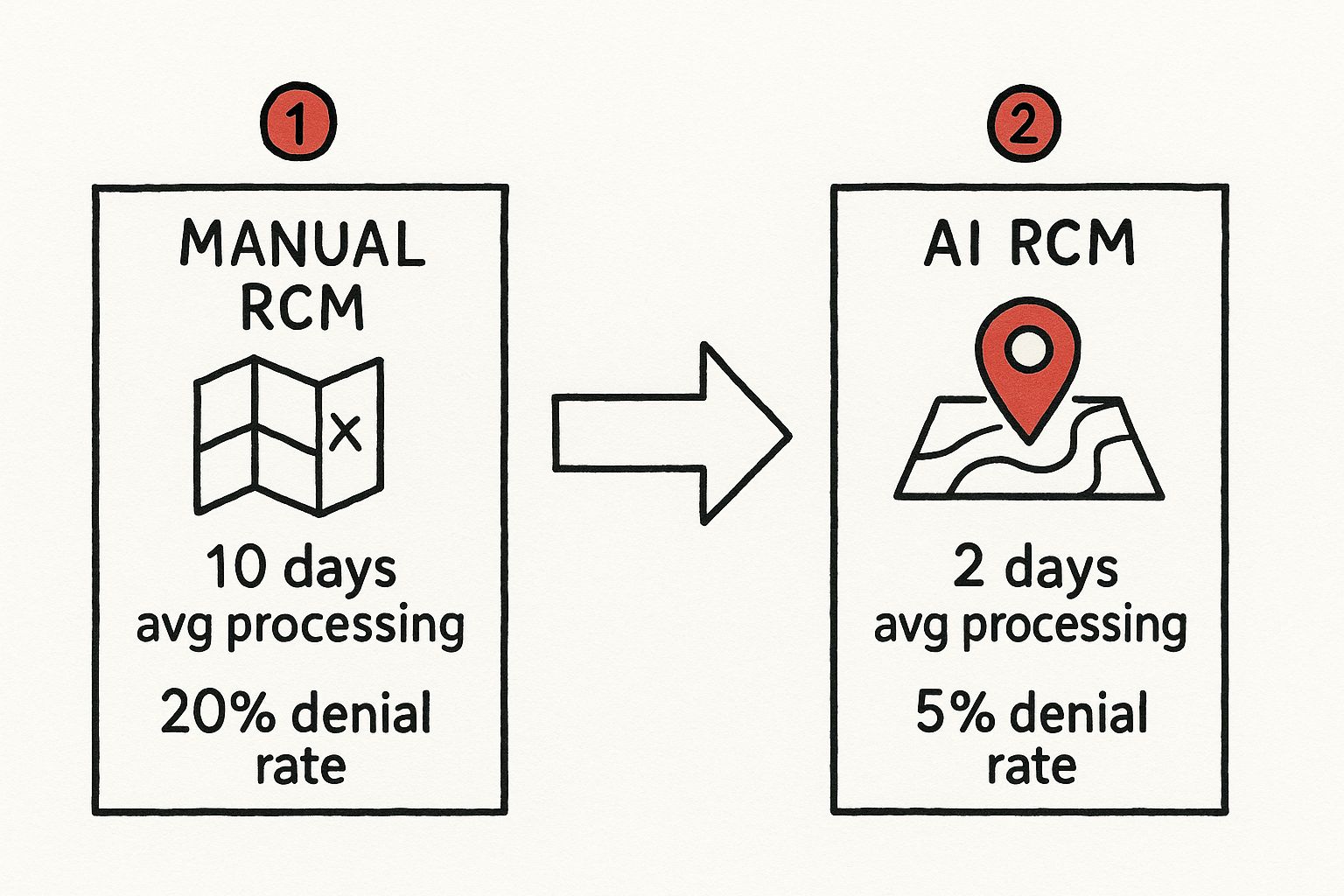
As you can see, AI dramatically shortens the time it takes to process claims and significantly lowers denial rates. The direct result is better, faster cash flow.
A Strategic Shift for Healthcare Providers
Bringing AI into the mix is much more than a technology upgrade; it’s a complete strategic pivot. By taking over the tedious, repetitive tasks, AI frees up your finance teams to concentrate on work that truly requires a human touch. Think complex claim appeals and high-stakes negotiations with payers. This is a core part of modernizing healthcare finance.
To truly appreciate the change AI brings, it helps to see a direct comparison. Here’s a quick look at how the old, manual processes stack up against a modern, AI-powered system.
Traditional RCM vs AI-Powered RCM At A Glance
| Process | Traditional RCM Approach | AI-Powered RCM Approach |
|---|---|---|
| Patient Registration | Manual data entry, high risk of typos and errors. | AI validates patient data in real-time, flagging errors instantly. |
| Prior Authorization | Staff manually calls or faxes payers, a slow and frustrating process. | AI automates submission and status checks, predicting likelihood of approval. |
| Medical Coding | Coders manually review clinical notes, leading to inconsistencies. | Natural Language Processing (NLP) suggests accurate codes directly from notes. |
| Claim Submission | Claims are checked against basic rules, many errors slip through. | AI scrubs claims against millions of payer rules, predicting denials. |
| Denial Management | Staff manually sorts and reworks denied claims one by one. | AI automatically categorizes denials and routes them for appeal with insights. |
| Patient Collections | Generic payment reminders are sent to all patients. | AI predicts a patient's likelihood to pay and customizes outreach. |
This table shows it's not just about doing the same things faster. AI fundamentally changes how the work gets done, introducing a level of precision and foresight that was impossible before.
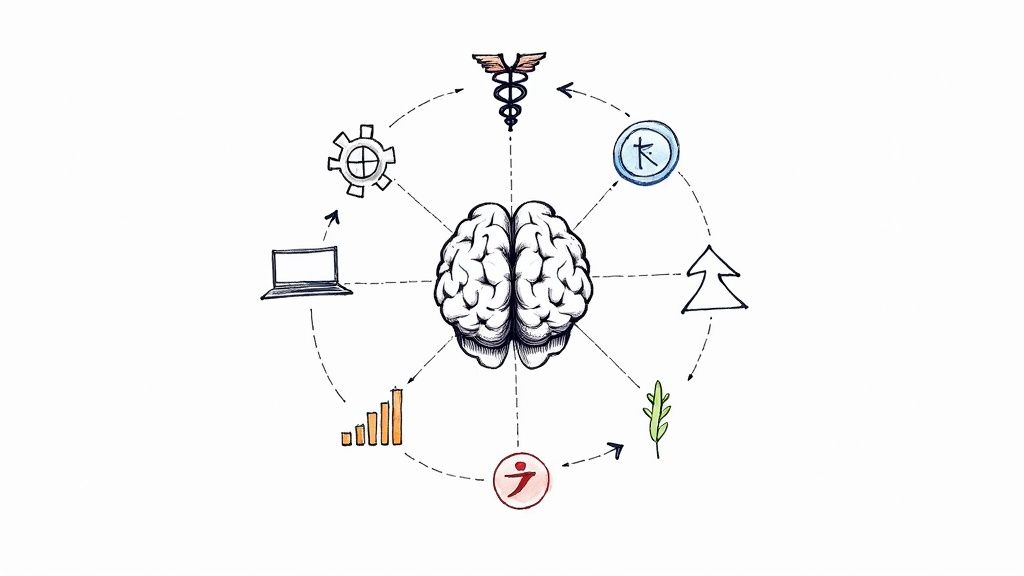
By turning raw data into clear, actionable insights, AI allows organizations to not only plug current revenue leaks but to actually prevent new ones from springing up. It transforms the revenue cycle from a necessary cost center into a strategic asset for financial health.
For a closer look at the mechanisms behind this, exploring resources on AI-driven financial analytics can offer valuable context. Ultimately, adopting AI in your revenue cycle is a foundational step toward building a healthcare system that is more efficient, financially secure, and better equipped to focus on patients.
A Look at AI's Impact on Core RCM Processes
To really get a feel for how AI is changing revenue cycle management, you have to look under the hood. It’s not about one single, magical fix. Instead, it's a series of smart, targeted improvements that overhaul the entire financial journey, piece by piece. AI breathes new life into each stage, transforming a clunky, manual workflow into something that feels fluid and intelligent.
From the second a patient books an appointment to the day their final payment clears, AI works in the background to head off errors, speed things up, and plug revenue leaks. Let's walk through the key stages to see how this actually plays out in the real world.
Pre-Authorization and Eligibility Checks
So much can go wrong right at the very beginning. Patient registration is notorious for being a source of expensive mistakes that only pop up later. A simple typo in a policy number or a misspelled name can trigger an instant denial weeks down the line. AI acts as your first line of defense.
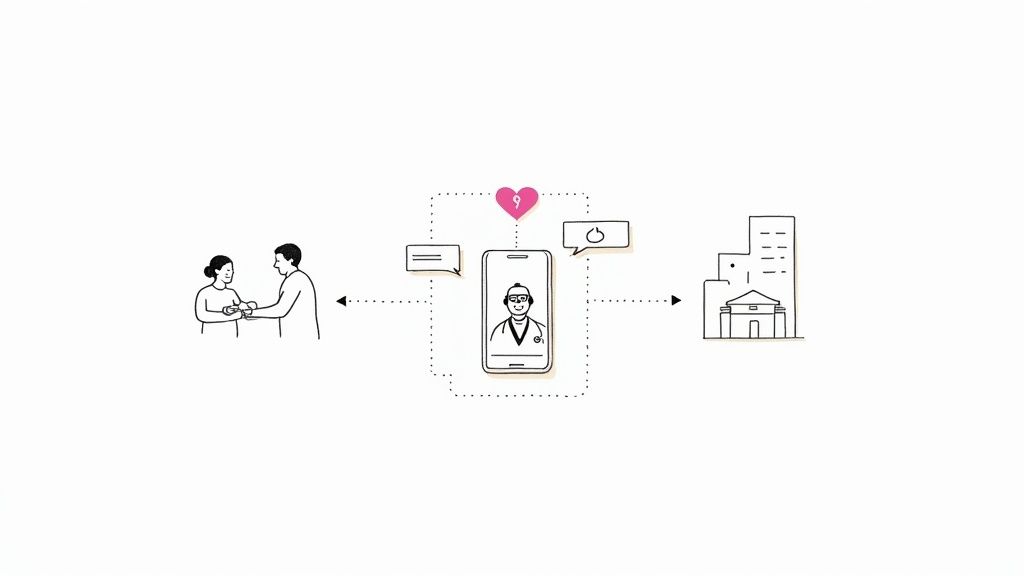
Modern AI systems tap directly into payer databases, verifying a patient's eligibility in real-time. No more guessing games or chasing down coverage details; everything is confirmed before the patient even steps into the exam room.
And for those services that need prior authorization? AI takes over the tedious submission and follow-up process. Instead of your staff spending hours on hold with insurance companies, the system manages the paperwork and keeps checking the status, freeing up your team to handle more critical patient-facing tasks.
Smarter Medical Coding
Getting medical codes right is absolutely essential for getting paid correctly, but it's traditionally a very manual—and often subjective—job. Coders have to sift through complex clinical notes, which leaves plenty of room for human error and inconsistency. This is where a specific type of AI called Natural Language Processing (NLP) really shines.
NLP algorithms are trained to read and actually understand the unstructured text in a clinician’s notes, much like a person would. Based on that analysis, the AI can then suggest the most accurate CPT and ICD codes, even pointing to the exact documentation that supports them. This not only boosts coding accuracy but also helps with compliance by creating a clean, auditable link between the care provided and the bill submitted.
Here's the truly clever part: by sifting through massive amounts of historical claims data, machine learning can spot subtle coding patterns that frequently lead to denials. It flags these potential issues for review before a claim even goes out the door.
Automated Claim Scrubbing
Before any claim is fired off to a payer, it needs a thorough "scrubbing" to check for errors. Older, rule-based systems catch the obvious stuff, but they often miss the tricky, nuanced issues specific to certain payers. AI takes this process to a whole new level.
An AI-powered RCM tool scrubs claims against a gigantic, constantly evolving library of millions of payer-specific rules. It can even predict the likelihood of a denial with scary accuracy, flagging claims with a high chance of rejection and telling you exactly why. Think of it as a digital gatekeeper ensuring only clean, compliant claims make it out, which dramatically boosts your first-pass acceptance rate.
Proactive Denial Management
Even with the best systems, some denials are bound to happen. The old-school approach is to manually sort through denial codes and reasons—a painfully slow process that often leads to missed filing deadlines and, ultimately, lost revenue.
AI completely changes the game here. It instantly categorizes denials by their root cause, whether it's a coding error, a credentialing issue, or something else entirely. It then uses predictive analytics to prioritize which denied claims are most likely to be won on appeal, letting your team focus their energy where it will actually pay off.
The system can even auto-generate appeal letters, pulling in all the necessary documentation and citing the relevant payer policies. This automation not only speeds up the appeals cycle but also turns denial management from a frustrating cost center into a powerful engine for revenue recovery.
The Real-World Benefits of Adopting AI in RCM
So, what does bringing AI into your revenue cycle management actually do for your organization? Beyond the buzzwords and technical specs, the impact shows up where it counts: your bottom line, your daily operations, and your patient relationships. It’s about building a stronger, more resilient financial foundation for your practice.
AI in RCM directly tackles the chronic headaches that have plagued healthcare for years—manual data entry mistakes, disjointed workflows, and painfully slow reimbursement cycles. By fixing these issues, AI strengthens the overall revenue integrity of a healthcare provider. The results are clear and measurable: claims get approved faster, denials drop, and keeping up with regulations becomes easier. This is especially vital in North America, where both healthcare costs and administrative burdens are always under the microscope, as highlighted in recent North American healthcare research.
Driving Substantial Financial Wins
The most immediate and powerful benefits are, without a doubt, financial. When you automate and sharpen key processes with AI, you see a direct impact on net revenue and cash flow.
- Drastically Reduced Claim Denials: Before a claim even leaves your system, AI algorithms check it against millions of payer-specific rules, spotting tiny errors a human might easily overlook. This front-end scrubbing dramatically increases your first-pass acceptance rate, which means you get paid correctly, the first time, far more often.
- Accelerated Cash Flow: Cleaner claims and faster processing naturally lead to quicker reimbursements. AI also automates the follow-up process and helps prioritize which appeals to tackle first, slashing the time claims sit in accounts receivable. This injects cash into your organization when you need it.
- Lowered Operational Costs: Think about all the time spent on repetitive tasks like data entry, verifying eligibility, or posting payments. Automating this work frees up your staff for more strategic, high-value activities, ultimately lowering the overhead costs tied to billing and collections.
Boosting Operational Efficiency
AI doesn’t just crunch numbers better; it fundamentally changes how your team operates. By offloading the administrative grind, it creates a much more productive and effective work environment.
Think of AI as a force multiplier for your staff. It handles the high-volume, low-complexity work, letting your skilled professionals concentrate on complex appeals, negotiating with payers, and financial strategy—the stuff that truly requires human insight.
This shift makes a huge difference. When you rescue your team from monotonous tasks, morale goes up and burnout goes down. Plus, with AI ensuring every step is handled with consistency and accuracy, your organization can more easily stay compliant with the constantly changing world of healthcare regulations. This is one of the biggest wins you get from smart workflow automation in your RCM.
Creating a Better Patient Experience
A patient’s financial journey is a huge part of their overall perception of care. A confusing or frustrating billing process can ruin an otherwise positive clinical experience. AI-powered RCM helps create a financial interaction that’s smooth, transparent, and builds trust.
For instance, AI can give patients an accurate, real-time estimate of their out-of-pocket costs before a procedure. This simple act of transparency gets rid of surprise bills and helps patients plan. The result? Happier patients, better collection rates, and a stronger reputation. The right AI tools for business can transform a common point of friction into a real competitive advantage.
AI in Action: Real Stories from the Healthcare Trenches
It's one thing to talk about theory, but it’s another to see AI revenue cycle management in the wild. This is where the real "aha!" moments happen. So, let's step away from the abstract and look at a few concrete examples of how healthcare providers are tackling their biggest RCM headaches head-on. These aren't just hypotheticals; they're real-world snapshots of what happens when AI gets to work.
Case Study 1: The Large Hospital System
Picture a sprawling, multi-state hospital system. They were processing thousands of complex claims every single day and, frankly, they were drowning. Their denial rate was sitting at an alarming 18%, and their Days in Accounts Receivable (A/R) had ballooned past 60. With that kind of volume, trying to manually review everything was a losing battle, and their old software just couldn't keep pace with the constant shifts in payer rules.
They decided to bring in an AI-powered RCM platform, and the shift was immediate and powerful. The AI started acting as a gatekeeper, scrubbing every single claim before it went out the door and flagging potential denials using predictive analytics. It didn't stop there. The system also automated the entire denial management process, sorting rejected claims and pushing the appeals most likely to succeed to the top of the pile.
The Result: In just six months, the hospital’s denial rate plummeted from 18% to a much healthier 6%. Their Days in A/R dropped to an average of 38. That change unlocked millions in accelerated cash flow, proving AI can handle immense complexity at scale.
Case Study 2: The Specialty Clinic
Now, let's zoom in on a specialty orthopedic clinic. Their problem wasn't the sheer number of claims, but their complexity. They performed highly specific and intricate procedures, and even tiny inaccuracies in CPT codes led to constant underpayments and denials. They were leaving a lot of money on the table, and their small admin team was completely overwhelmed.
This clinic adopted a highly focused AI tool that used Natural Language Processing (NLP) to get their coding right. The AI would read the surgeons' detailed operative notes and suggest the most precise codes, ensuring the final claim perfectly matched the complexity of the care delivered. It wasn't about replacing their coders; it was about giving them an incredibly smart assistant.
By doing this, the clinic started capturing revenue they had previously written off. Their average reimbursement per procedure jumped by 12%. For a closer look at these kinds of financial turnarounds, this practical guide to harnessing AI for financial analysis offers some great insights.
Case Study 3: The Small Independent Practice
Finally, think about a small primary care practice with just two physicians. They didn't have the budget for a big administrative staff and found themselves bogged down by the basics of billing. Their collection rate was suffering, and the doctors were losing precious time to paperwork that could have been spent with patients.
Their solution was to use an AI automation service on a subscription basis, which gave them access to powerful tools without a huge upfront cost. This service put patient eligibility checks, claim submissions, and payment posting on autopilot. It even handled patient collections with automated, personalized reminders.
This smart use of automation helped the small practice run with the efficiency of a much larger organization. Their collection rate shot up by over 20%, and the physicians got back to focusing on what they do best: caring for patients. These stories show that with the right strategy, AI can deliver incredible results no matter the size of your practice. It all comes down to finding the right tool for your specific challenge.
A Practical Roadmap to Implementing AI in Your Revenue Cycle
Ready to make a change? Moving to an AI-powered RCM system isn't just about flipping a switch on new software. It’s a fundamental shift in how your organization approaches its financial health. A thoughtful, well-planned implementation is the key to a smooth transition, getting the most out of your investment, and bringing your team along for the ride.
Think of this as your roadmap. By breaking the journey down into clear, manageable steps, you can navigate the path to a smarter, more efficient revenue cycle without falling into common traps.
Start With an Honest Look at Your Current Process
Before you even think about looking at AI vendors, you need to look inward. The first step is to get brutally honest about your biggest RCM headaches. Are you constantly fighting a mountain of claim denials? Is verifying patient eligibility a daily source of frustration and delays? Or is your team just buried under the weight of mind-numbing manual tasks?
It's time to dig deep into your current workflows and metrics:
- Dissect Your Denial Data: Find out exactly why claims are being rejected. Pinpoint the most common reasons and trace them back to their source in your process.
- Know Your Numbers: Establish a clear baseline for your Days in A/R, first-pass acceptance rate, and collection rates. You can't measure improvement if you don't know where you started.
- Talk to Your Team: Your billing and coding staff are on the front lines every single day. They know where the real bottlenecks are. Their insights are pure gold.
This initial assessment is the foundation of your entire strategy. It ensures you're shopping for a solution that solves the problems you actually have.
Get Your Data House in Order
AI is fueled by data. The cleaner and more organized your data, the smarter and more effective your AI tools will be. Before you bring in any new system, you have to get your data infrastructure ready. This means cleaning up inconsistencies in patient records, creating standard rules for data entry, and making sure your EHR and billing systems can talk to each other.
Think of it this way: You wouldn't build a million-dollar house on a cracked and crumbling foundation. In the same way, you can't expect an AI system to produce accurate, reliable results if you feed it messy, inconsistent data. Getting serious about data hygiene isn't optional; it's essential.
Choosing the Right AI Partner
Picking a vendor is one of the most critical decisions you'll make. Not all AI solutions are the same. You need a partner who understands more than just technology—they need to live and breathe healthcare finance. Look for a vendor with rock-solid HIPAA compliance, the ability to integrate smoothly with your existing systems, and a proven history of success.
The market data backs this up. Providers are clearly looking for expert guidance, not just software off the shelf. In 2023, services like consulting and managed RCM accounted for about 58.2% of the market. It shows that organizations value having an expert in their corner. At the same time, integrated AI platforms that can handle the entire RCM process—from coding to denials—hold a massive 63.5% market share, proving that a comprehensive system is what most organizations want. Read more on RCM market trends here.
Lead Your Team Through the Change
Don't forget the human side of this equation. As we explored in our AI adoption guide, successful technology adoption is all about people. It's crucial to frame AI as a tool that empowers your team, not one that replaces them. Show them how it will free them from tedious, repetitive tasks so they can focus on more complex, valuable work that requires their expertise.
Clear communication and proper training are what turn skepticism into genuine enthusiasm. Getting help from an AI strategy consulting firm to understand the full AI Product Development Workflow can make all the difference in ensuring a smooth rollout and a great return on your investment.
Finding the Right Partner to Maximize Your ROI
Picking the right AI technology for your revenue cycle is a big decision, but it's only half the battle. The partner you choose to bring that technology to life is what really dictates whether you succeed and see a real return on your investment. This isn't just about hiring a vendor; it's about forming a strategic alliance focused on your organization's financial health.
When we talk about the ROI of AI solutions, it’s easy to get fixated on the initial cost savings. And yes, reducing operational overhead is a great start. But the true value is found in the long-term wins: sustained revenue growth, a permanent drop in denial rates, and even better patient satisfaction scores because the financial journey has become clearer and less frustrating.
What to Look for in an AI Partner
Let's be clear: not all partners are created equal. You need someone who gets both the intricacies of artificial intelligence and the immense financial pressures unique to healthcare. As you evaluate your options, use this checklist to cut through the noise:
- Deep Healthcare Expertise: Do they actually speak your language? They need to understand the nuances of medical billing, labyrinthine payer rules, and strict HIPAA compliance. A tech-first approach just won't cut it.
- A Proven Track Record: Don't just take their word for it. Ask for concrete real-world use cases and talk to their clients. Can they show you measurable improvements in key RCM metrics for organizations like yours?
- Scalability and Flexibility: The solution has to grow with you. Whether you're a small clinic or a sprawling hospital system, the platform must adapt to your changing needs without a complete overhaul.
- Seamless Integration: How well will their system play with your existing Electronic Health Record (EHR) and other internal tooling? A clunky integration can create more headaches than it solves, quickly turning your investment into a liability.
Off-the-Shelf vs. a Custom Strategy
So, do you buy a ready-made solution or build something custom? The right answer really depends on the specific problems you're trying to solve.
For many healthcare organizations, a powerful off-the-shelf product with robust features like automated claim scrubbing and denial management is the perfect fit. These platforms get you up and running quickly with proven capabilities.
However, if your challenges are highly specific—maybe you're dealing with complex multi-specialty coding or a web of unique payer contracts—a one-size-fits-all tool will likely fall short. This is where investing in a Custom AI Strategy report makes sense. Guided by AI strategy consulting, this approach digs deep to identify your exact pain points and maps out a solution built just for you. For those who need a truly tailored platform, working with a firm specializing in healthcare software development can unlock the most value.
A true partner doesn't just sell you software and walk away. They stick around. They help you analyze performance data, fine-tune your workflow automation, and adapt as the healthcare landscape inevitably changes. That’s how you ensure your AI investment keeps paying dividends for years to come.
Ultimately, you're looking for a guide. Our expert team is here to walk you through every step, from the initial assessment to full-scale implementation and beyond, making sure your AI-powered RCM initiative delivers on its promise.
FAQs About AI in RCM
1. Will AI Replace Our Medical Billing and Coding Staff?
Absolutely not. It's better to think of AI as a powerful assistant that supercharges your team's skills. It handles the high-volume, repetitive tasks that bog people down—like data validation and initial claim checks. This frees up your highly skilled staff to focus on the complex work that requires a human brain, like navigating tricky appeals, analyzing denial trends, and negotiating with payers. The goal is to elevate your team, not replace it.
2. How Secure Is Patient Data in an AI RCM System?
Security is non-negotiable. Any reputable AI RCM platform is built from the ground up to be fully HIPAA compliant. They use modern security measures like end-to-end data encryption, strict access controls, and constant monitoring to protect sensitive information. When you’re vetting a partner, demand total transparency about their security protocols and compliance certifications. In many cases, today's AI systems offer a far higher level of security than older, on-premise software.
3. What Is a Realistic Timeline for AI RCM Implementation?
This really depends on the size of your organization and how much you want to tackle at once. A focused pilot program, say for automating denial management, can be up and running in 2-4 months. A full, end-to-end RCM overhaul is a bigger project, typically taking anywhere from 6-12 months. The smartest way to go is a phased rollout. Start with the areas that promise the biggest and fastest wins. This approach lets your team get comfortable with the new tools and see real, positive results early on.
4. How Much Technical Expertise Do We Need In-House?
Probably less than you think. The new wave of AI RCM solutions, particularly those delivered through AI Automation as a Service, are designed for the people who will actually use them—your non-technical RCM staff. A good technology partner handles the heavy lifting of implementation, integration with your existing systems, and ongoing maintenance. Your team’s job isn't to become IT experts; it's to use the insights and automated workflows to do their jobs better.
At Ekipa AI, we turn your AI ambitions into scalable impact. Our platform delivers a tailored AI strategy in 24 hours, helping you uncover and execute transformation opportunities without the costly consultant price tag. Discover how Ekipa can accelerate your AI journey today.