AI in Medicine and Healthcare: A Practical Guide
Explore how AI in medicine and healthcare is transforming patient outcomes. This guide offers proven strategies and real-world insights for industry leaders.

When people talk about artificial intelligence in medicine, it's easy to picture sci-fi scenarios of robot doctors. But the reality is far more practical and, frankly, more powerful. At its core, AI in healthcare is about using smart algorithms to sift through the mountains of complex medical data we now generate. The goal isn't to replace a doctor's expertise, but to supercharge it.
Think of it as giving clinicians a powerful assistant—one that can spot patterns in patient data, lab results, and medical scans that the human eye might miss. This collaboration turns raw data into life-saving insights, leading to faster diagnoses, more personalized treatments, and smoother hospital operations.
How AI Is Reshaping Modern Medicine
AI has moved well beyond the research lab and is actively reshaping how we deliver care. It's becoming the central nervous system for modern healthcare systems, enabling a fundamental shift from simply reacting to illness to proactively predicting and preventing it. By making sense of information at a scale and speed no human ever could, AI is building a more intelligent, interconnected healthcare ecosystem.
The money follows the momentum. The global AI in healthcare market ballooned from a modest $1.1 billion in 2016 to an impressive $22.4 billion in 2023. That's a jaw-dropping 1,779% increase. With forecasts pointing to a market size of $188 billion by 2030, it’s clear the industry sees AI as essential for tackling medicine’s biggest challenges. A deeper look at these AI in healthcare statistics reveals just how fast this trend is accelerating.
From Data Overload to Clinical Insight
Every day, healthcare facilities are flooded with data from electronic health records (EHRs), CT scans, genomic sequencing, and wearable patient monitors. This is where AI in medicine and healthcare truly shines. AI algorithms are designed to find the needle in the haystack—identifying subtle correlations and early warning signs that are often buried in the noise.
For hospital executives and clinical leaders, this isn't about chasing the latest tech trend. It's about tangible results. Integrating intelligent systems has a direct impact on three critical areas:
- Empowering Clinicians: AI-driven diagnostic tools act as a trusted second opinion for radiologists and pathologists, flagging potential abnormalities in images and tissue samples with incredible precision.
- Improving Patient Outcomes: Predictive analytics can identify which patients are at a higher risk of developing sepsis or being readmitted, giving care teams a chance to intervene before a crisis occurs.
- Driving Operational Efficiency: Routine administrative work—like scheduling appointments, managing claims, and handling billing—can be automated. This frees up staff to focus on what matters most: patient care.
The table below offers a snapshot of how AI is making its mark across different parts of the healthcare landscape.
Key Areas of AI Transformation in Healthcare
This table summarizes the primary domains within healthcare being revolutionized by AI, providing a quick overview of its diverse applications.
| Domain | AI Application Example | Primary Benefit |
|---|---|---|
| Diagnostics | Computer vision algorithms analyzing medical images (X-rays, MRIs) to detect signs of cancer or stroke earlier. | Faster, more accurate diagnoses and reduced workload for radiologists. |
| Drug Discovery | Machine learning models analyzing biological data to identify promising drug candidates and predict their effectiveness. | Shortens the traditionally long and expensive R&D cycle for new medicines. |
| Personalized Medicine | AI analyzing a patient's genetic makeup and lifestyle to recommend tailored treatment plans and preventative care. | Moves away from one-size-fits-all treatments to highly effective, individualized care. |
| Administrative Tasks | Natural Language Processing (NLP) automating data entry from patient records and transcribing clinical notes. | Reduces administrative burden, minimizes human error, and improves operational flow. |
| Predictive Analytics | Models forecasting patient admissions, disease outbreaks, or individuals at high risk for chronic conditions. | Enables proactive resource allocation and preventative health interventions. |
As you can see, the applications are as diverse as they are impactful, touching nearly every aspect of care delivery and management.
A Strategic Imperative for Modern Healthcare
Putting these technologies to work requires a clear, deliberate plan. It all starts with pinpointing your organization's most pressing challenges and identifying which specific AI Solutions can solve them.
Whether you're looking to build a new diagnostic tool with specialized healthcare software development or simply streamline your back-office processes, the journey starts with a smart strategy. Adopting AI isn't just a technical upgrade—it's a fundamental business decision that prepares your organization for the future. You can see how we help clients by exploring our approach to AI in the healthcare industry.
Core Applications Driving Better Patient Outcomes
While the big-picture vision for AI is exciting, its real impact hits home when you see how it’s being used on the front lines of patient care. This is where AI in medicine and healthcare moves from a buzzword to a life-changing tool. These aren't far-off promises; these technologies are already improving diagnostics, tailoring treatments, and steadying the surgeon's hand today.
At its core, this progress comes from AI's almost superhuman ability to process and find patterns in complex medical data. Think of it as a force multiplier for doctors, giving them deeper insights so they can make better, faster decisions. From scanning medical images to flagging at-risk patients, these real-world use cases show how AI is becoming an essential part of the modern clinician's toolkit.
Enhancing Diagnostics with Medical Imaging AI
One of the most mature—and frankly, most impressive—applications of AI is in medical imaging. Radiologists and pathologists spend their days hunting for tiny, almost invisible abnormalities in X-rays, CT scans, and MRIs. It's a high-stakes process that's both exhausting and open to human error.
AI algorithms, trained on millions of past scans, act as a second set of expert eyes. They can spot patterns with incredible accuracy, flagging suspicious areas that might otherwise go unnoticed. An AI might detect the earliest signs of diabetic retinopathy, identify a cancerous nodule in a lung scan, or highlight subtle clues of a stroke. The goal isn't to replace the radiologist but to empower them, freeing them up to focus on the most complex cases and confirm the AI’s findings.
This isn't just happening in a few research labs. By 2024, over half of all healthcare providers were using AI for at least one imaging task. Meanwhile, around 65% of U.S. hospitals now use predictive analytics to forecast patient outcomes and improve preventive care, leading to incredible results like a 50% reduction in hospital readmissions. You can see more compelling numbers in these AI in healthcare statistics.
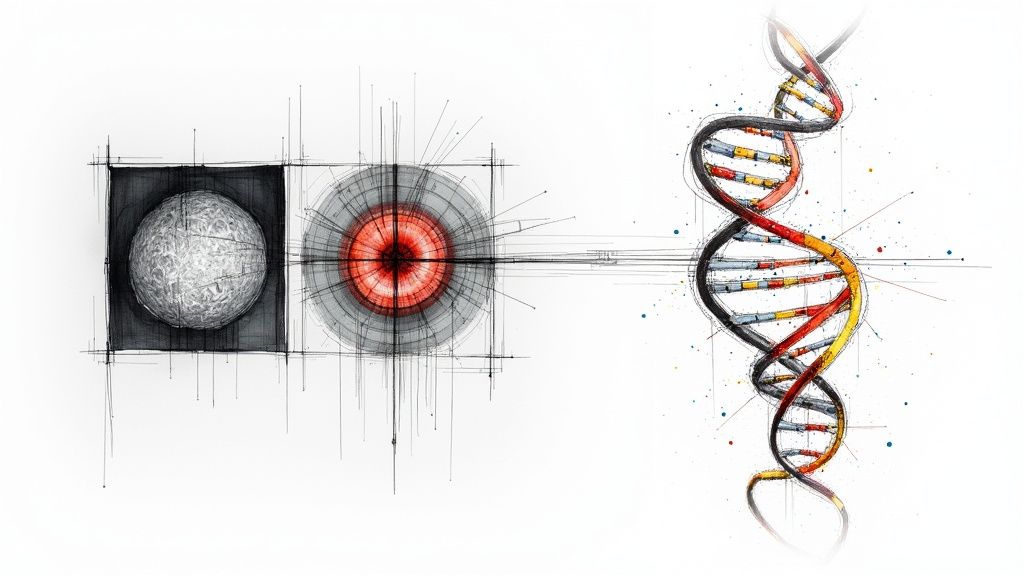
Personalizing Treatment with Genomic Analysis
The old one-size-fits-all approach to medicine is fading fast, and AI-powered genomic analysis is a big reason why. Every person’s unique genetic code affects how they react to diseases and treatments. By sifting through massive genomic datasets, AI helps oncologists and other specialists design treatment plans that are truly personal.
AI can predict how a specific patient’s tumor will respond to different chemotherapy drugs, allowing clinicians to select the most effective treatment from the start. This not only improves survival rates but also spares patients from the debilitating side effects of ineffective therapies.
This kind of precision medicine used to be slow and incredibly expensive. Today, AI-driven platforms can deliver these insights in a fraction of the time, making personalized care a practical reality for more people.
Predictive Analytics and AI-Powered Robotics
Beyond just diagnostics and treatment plans, AI is fundamentally changing other critical aspects of clinical care.
- Predicting Patient Risk: Machine learning models can scan a patient's electronic health record (EHR) to predict their risk of developing serious conditions like sepsis or heart failure. By flagging high-risk individuals, care teams can step in with preventative measures before a crisis hits. Our own Clinic AI Assistant is one of the AI tools for business designed to help make sense of this kind of data.
- AI-Enhanced Surgical Robotics: In the operating room, AI gives surgeons a new level of precision. These robotic systems can filter out a surgeon's natural hand tremors, provide a magnified 3D view of the surgical site, and execute maneuvers with superhuman delicacy. The results? Less invasive procedures, reduced blood loss, and faster recovery times.
Each of these examples points to the same trend: AI is being woven directly into the clinical workflow, augmenting human expertise, not replacing it. Building a clear plan for implementing these tools, often beginning with AI strategy consulting, is the first step toward unlocking these powerful benefits.
Streamlining Healthcare Operations with AI
While the clinical breakthroughs get most of the headlines, the real engine of any great healthcare system is how well it runs behind the scenes. The problem is, administrative bloat and logistical snags are all too common. They drain time and money that should be going directly to patient care. This is where AI in medicine and healthcare makes a huge practical difference—by taking on the administrative grind.
When you automate the repetitive, rules-based work, you give your highly skilled clinicians and administrators their time back. It’s about letting them focus on the complex, human problems that need their expertise, making the whole system smarter and more efficient.
Optimizing Hospital Flow and Resource Management
Think of a hospital as a small city. Managing patient flow, scheduling surgeries, and juggling critical resources like ORs and ICU beds is a massive logistical puzzle. For years, we've relied on manual planning, which inevitably leads to long wait times, expensive equipment sitting idle, and staff burnout.
AI changes the game by bringing a predictive, dynamic approach to hospital management. Machine learning models can comb through historical data and real-time information to see what's coming next—predicting admissions, forecasting discharge times, and optimizing surgical schedules.
- Smart Scheduling: AI algorithms can shuffle appointments to slash wait times and keep clinicians' schedules full, automatically filling last-minute cancellations and cutting down on no-shows.
- Resource Allocation: Instead of reacting to a crisis, AI can predict the demand for things like ventilators or operating rooms, allocating them proactively to prevent shortages.
- Staff Deployment: AI helps build smarter staffing rosters based on anticipated patient loads. This means you're never caught short-staffed during a rush or overstaffed when things are quiet.
This kind of intelligent coordination helps a hospital move from constantly putting out fires to proactively managing its resources. The result is happier patients and a healthier bottom line.
By automating administrative tasks, AI has the potential to save the U.S. healthcare system over $150 billion annually. That staggering number shows just how powerful the financial incentive is for bringing operational AI into the fold.
Automating the Revenue Cycle
Medical billing and coding are the financial lifeblood of a healthcare organization, but they’re also famously tedious. Human error is common and costly, leading to denied claims and lost revenue. AI, especially Natural Language Processing (NLP), is tailor-made to bring speed and precision to this process.
NLP algorithms can actually read and understand a clinician's unstructured notes, then suggest the correct medical codes for diagnoses and procedures. This drastically cuts down the manual work for coders, boosts accuracy, and gets claims paid faster. It’s a perfect example of how workflow automation can deliver a quick and tangible return.
For leaders looking to put this into practice, the options range from developing internal tooling to bringing in a complete AI Automation as a Service provider. To get a better sense of the possibilities, it's worth reading up on how automation can streamline various business processes. By letting AI handle these repetitive chores, you free up your team to focus on patient care and strategic planning. Partnering with the right AI strategy consulting firm can ensure these tools are rolled out in a way that truly makes a difference.
The Real-World Payoff: Why AI in Healthcare Matters
So, why should healthcare leaders actually care about AI in medicine and healthcare? The answer isn't just about keeping up with technology; it's about the tangible, compounding benefits that fundamentally reshape how we deliver and manage care. Think of it in three main pillars: making diagnostics sharper, running hospitals smarter, and giving patients care that’s more personal and proactive.
This isn't just a minor upgrade. By weaving the right AI tools for business into the fabric of our healthcare systems, we can hit new performance benchmarks that were once impossible, building a more resilient and effective system for patients and providers alike.
Sharper Diagnostic Accuracy
One of the first and most powerful wins with AI comes from improving clinical diagnosis. In medical imaging, for example, AI algorithms act as a second set of eyes for radiologists. They can comb through X-rays, MRIs, and CT scans, spotting subtle patterns or tiny anomalies that might signal the early stages of a disease.
Let's be clear: this isn't about replacing doctors. It's about giving them a powerful co-pilot. AI takes some of the immense cognitive load off specialists, letting them focus their expertise on confirming findings and handling the most complex cases. The result? Fewer diagnostic errors and a faster track from spotting a problem to starting treatment, which can make all the difference for patient outcomes.
Driving Down Costs and Boosting Efficiency
Beyond the examination room, AI is a game-changer for the administrative side of healthcare. Using intelligent workflow automation, AI can take over the tedious, repetitive tasks that drain resources—think patient scheduling, medical billing, or even managing pharmacy inventory. This isn't just a time-saver; it has a direct impact on the bottom line.
The numbers tell a powerful story. It's expected that 90% of hospitals will be using AI for early diagnosis and remote patient monitoring by 2025. On the financial side, AI is projected to slash healthcare costs by $13 billion by 2025, proving it's not just a clinical tool but a powerful economic one. As the technology matures, it also promises to help close gaps in healthcare access, especially in underserved areas. You can discover more insights about AI's economic impact in healthcare to see the full picture.
When you automate the routine stuff, you free up your highly trained doctors and nurses to do what they do best: care for patients. This is a huge win for staff morale and care quality, and it's always a central goal of any solid AI strategy consulting effort.
More Personal and Proactive Patient Care
This is where things get truly exciting. AI is helping us shift from a reactive "sick care" model to a genuinely proactive one. By analyzing massive amounts of data from electronic health records, wearable devices, and even genetics, AI can identify patients at high risk for developing chronic conditions like diabetes or heart disease—long before they ever feel a symptom. This opens the door for early, targeted interventions that can prevent serious illness from ever taking hold.
It also allows for incredibly personalized treatment plans. Instead of a one-size-fits-all approach, AI can help predict how a specific patient might respond to a particular drug or therapy. This means we can get patients on the most effective treatment right from the start. Getting the right AI Solutions in place is the first step toward making this future a reality.
To truly grasp the shift, it helps to see a side-by-side comparison.
AI in Healthcare Benefits vs Traditional Methods
Here’s a quick breakdown of how AI-driven approaches stack up against the old way of doing things across key healthcare functions.
| Healthcare Function | Traditional Approach | AI-Enhanced Approach |
|---|---|---|
| Medical Diagnostics | Relies solely on human interpretation of images and data, which can be time-consuming and prone to fatigue-related errors. | AI analyzes medical images (X-rays, CTs) to flag anomalies, providing a "second opinion" that boosts accuracy and speed. |
| Treatment Planning | Based on generalized clinical guidelines and population-wide studies. A "one-size-fits-many" model. | Creates personalized treatment plans by analyzing a patient's unique genetic, lifestyle, and clinical data to predict therapy response. |
| Hospital Operations | Manual scheduling, billing, and inventory management. Often slow, inefficient, and susceptible to human error. | Automates administrative tasks, optimizes patient flow, and predicts resource needs, leading to significant cost savings and efficiency. |
| Patient Monitoring | Periodic check-ups and reliance on patients reporting symptoms. A reactive approach to health issues. | Continuous monitoring via wearables and sensors, with AI predicting health crises before they happen for proactive intervention. |
As you can see, the AI-enhanced approach doesn't just digitize old processes—it fundamentally transforms them to be smarter, faster, and more centered around the individual patient.
Navigating the Challenges of AI Implementation
For all its promise, bringing AI into a real-world medical or healthcare setting is a serious undertaking. The path is filled with hurdles, and any leader needs to go into this with their eyes wide open. We're not just talking about plugging in new software; a successful AI initiative forces you to wrestle with complex issues around data, ethics, cost, and even your organization's culture.
Tackling these challenges head-on is what separates a pilot project that quietly fizzles out from an initiative that delivers real, lasting value. It's all about building a foundation of trust and reliability from the very beginning.
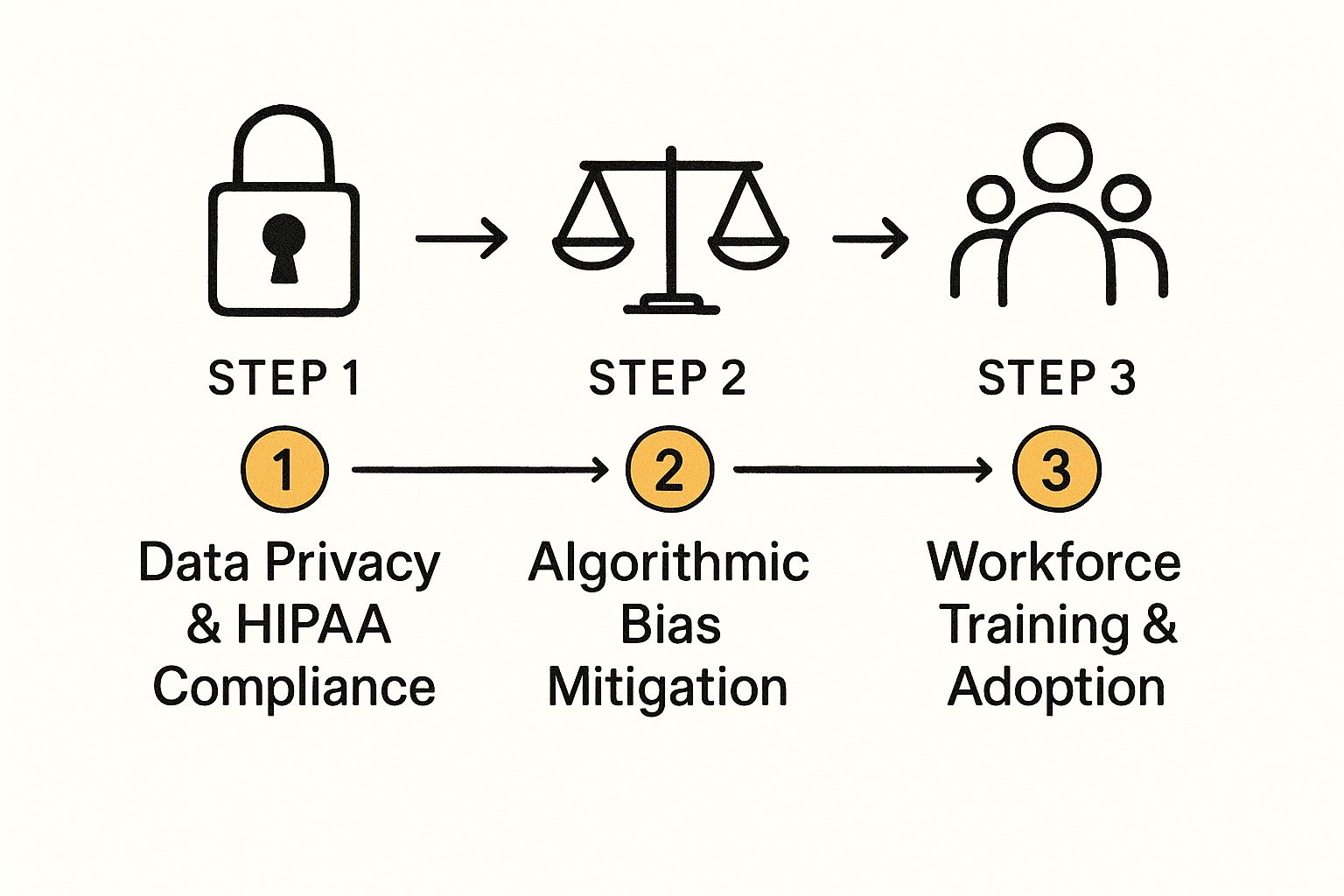
Ensuring Data Privacy and HIPAA Compliance
Patient data is the lifeblood of medical AI. It's also incredibly sensitive and heavily regulated. Any AI tool that even touches Protected Health Information (PHI) has to be rock-solid on its Health Insurance Portability and Accountability Act (HIPAA) compliance. This isn't just a suggestion—it's a legal and ethical bright line.
A single violation can lead to crippling fines, but the damage to patient trust can be far worse and almost impossible to repair. That's why ironclad data security and privacy protocols have to be baked into your AI project from day one.
One of the smartest ways to handle this is a technique called federated learning. Imagine training an AI model on data from multiple hospitals, but without the raw patient data ever leaving each hospital's secure server. That's what federated learning does. It allows the model to get smarter from diverse datasets while keeping patient confidentiality completely intact. Building out a secure data strategy like this is a core part of effective AI strategy consulting.
Mitigating Algorithmic Bias
An AI model is only as fair as the data you feed it. If your training data carries the same subtle biases that already exist in healthcare—whether they're based on race, gender, or income level—your AI will learn and even amplify them. You could end up with a diagnostic tool that works great for one group of people but fails another, making health disparities even worse.
For instance, an AI trained mostly on data from light-skinned patients might struggle to accurately identify skin cancer on darker skin tones. Making sure AI works for everyone isn't just an ethical nice-to-have; it's a clinical necessity.
To fight this, you have to be deliberate:
- Diversify Your Data: Go out of your way to collect and clean up data from the broadest possible range of patient populations. Your data needs to reflect the real world.
- Audit, Audit, Audit: Constantly test your AI models to see if they're performing differently for various demographic groups. You can't fix what you don't measure.
- Demand Transparency: You need to be able to understand why the algorithm is making its recommendations. This is key to spotting and fixing hidden biases.
Overcoming High Costs and Workforce Training
Let's be clear: implementing AI is a major investment. The price tag isn't just the software license. You have to think about upgrading your data infrastructure, the headache of integrating with your existing EHR, and the ongoing costs of keeping everything running smoothly. For many, just getting the budget approved is the first big mountain to climb.
But the human side of the equation is just as critical. Your doctors, nurses, and staff need to understand what these new tools do and, more importantly, trust them. You can have the most brilliant AI on the planet, but if your team doesn't buy in, it will just gather digital dust.
Getting people on board means you have to actively educate them, showing them how AI Solutions are there to enhance their expertise and automate tedious work, not to replace them. As we explored in our AI adoption guide, a gradual rollout with crystal-clear communication is the best way to build confidence. Helping organizations navigate this critical transition is precisely what our expert team does best.
Your Roadmap for Successful AI Adoption
Knowing the potential of AI in medicine and healthcare is one thing. Actually putting it to work effectively is a whole different ballgame. To get from theory to real-world results, you need a clear, deliberate roadmap.
Without a solid plan, even the most promising AI initiatives can get bogged down by fuzzy goals, unexpected technical hurdles, or a team that just isn't on board. The trick is to take a phased approach, building momentum and proving value with each step. This isn't about a risky, big-bang overhaul; it's about smart, calculated moves that connect the technology to what your organization truly needs.
Laying the Foundation for AI Success
Before anyone writes a single line of code, the real work begins. The foundational stage is all about asking the right questions to make sure your AI project is aimed at solving a problem that actually matters.
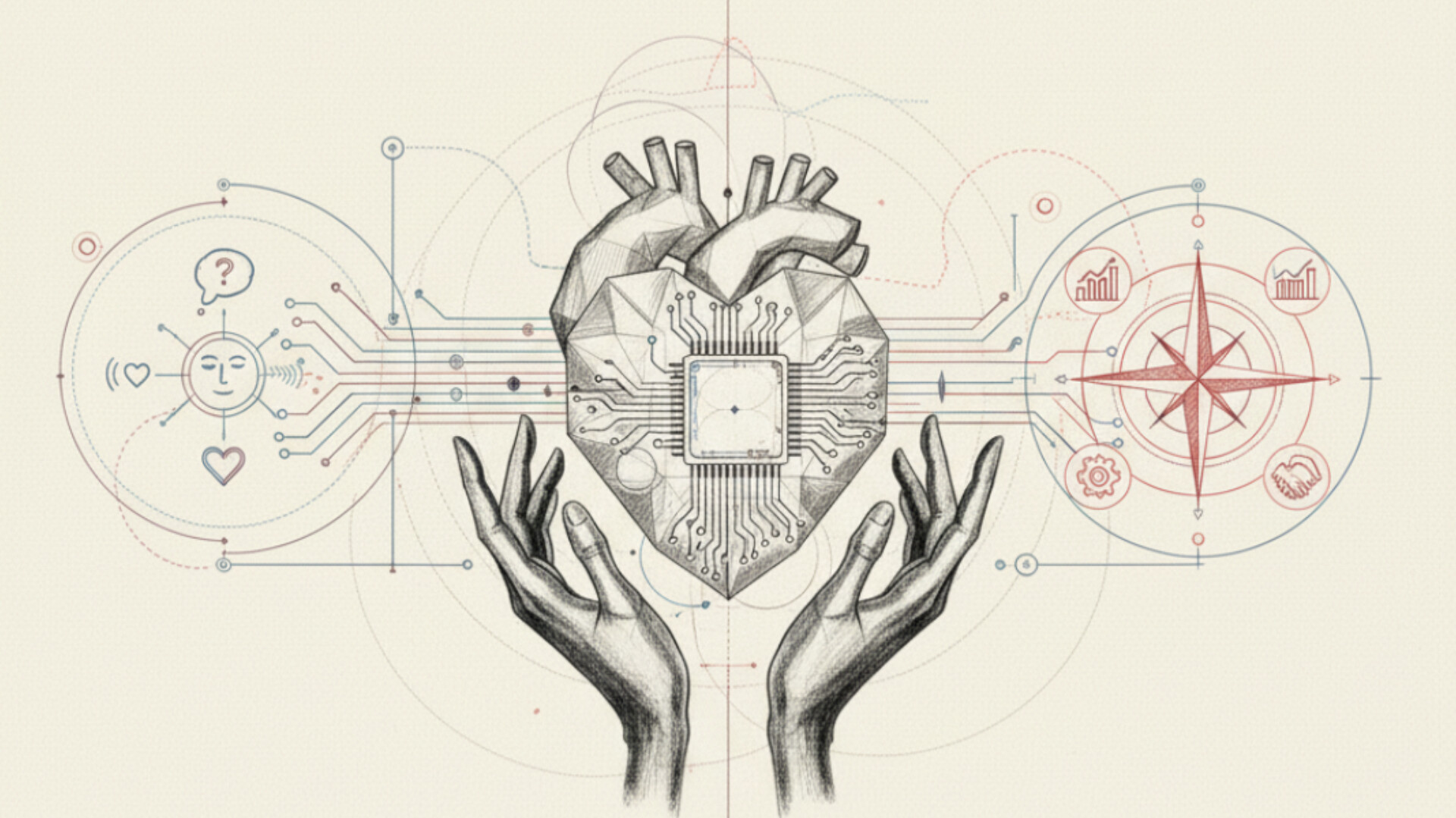
- Define Clear Objectives: Start with "why." What are you trying to achieve? Are you aiming to catch diagnostic errors earlier, cut down patient wait times, or maybe just streamline the billing process? You need to lock in a specific, measurable goal. Think of it as your North Star for the entire project.
- Conduct a Data Readiness Assessment: AI runs on data. Simple as that. You have to take a hard look at the quality, quantity, and accessibility of your data. This means digging in to find gaps, hidden biases, and inconsistencies, all while making sure your data handling is strictly HIPAA-compliant.
- Build a Cross-Functional Team: An AI project isn't just an IT thing. To make it work, you need clinicians, data scientists, IT specialists, and administrative leaders all in the same room. This mix of perspectives ensures the solution is not only clinically relevant and technically solid but also practical for day-to-day operations.
From Pilot Project to Scalable Impact
With a solid foundation in place, it's time to get moving. The best way to start is with a focused pilot project. This lets you test your ideas, learn fast, and build support across the organization before you go all-in on a massive rollout.
- Launch a Targeted Pilot Project: Pick one of your key objectives and launch a small-scale pilot. This controlled experiment is your chance to measure the impact, get real feedback from users, and iron out any wrinkles in the tech and workflow. Nailing the pilot often requires a detailed process, much like the one we map out in our AI Product Development Workflow.
- Plan for Scale with Ethical Governance: Once your pilot starts showing real value, you can begin thinking bigger. This is where you build a strong governance framework to handle everything from data privacy and monitoring for algorithmic bias to navigating the tricky ethical questions that will inevitably come up.
This visual guide breaks down some of the core ethical pillars that must be addressed as you scale.
Getting these steps right—from protecting patient data to helping your workforce adapt—is what turns a promising pilot into a capability that benefits the entire organization. It's a complex path, but one that can lead to incredible outcomes when navigated with a clear strategy and expert guidance.
FAQs: Answering Your Questions About AI in Medicine and Healthcare
Will AI replace doctors and other healthcare professionals?
This is one of the most common concerns, and the answer is a definitive no. AI is designed to be a powerful tool that augments, rather than replaces, human expertise. It excels at analyzing vast amounts of data to detect patterns that might be invisible to the human eye, handling repetitive administrative tasks, and providing data-driven insights. This partnership frees up clinicians from tedious work, allowing them to focus on what they do best: complex decision-making, patient interaction, and providing compassionate care.
What are the biggest ethical concerns with using AI in medicine?
The ethical landscape of AI in healthcare is complex. Key concerns include:
- Data Privacy: Ensuring that sensitive patient data is protected and used in compliance with regulations like HIPAA is paramount.
- Algorithmic Bias: If AI models are trained on biased data (e.g., data from a specific demographic), they can perpetuate and even amplify existing health disparities.
- Accountability: Determining responsibility when an AI-driven recommendation leads to an adverse outcome is a significant challenge, involving clinicians, developers, and institutions.
How can a smaller hospital or clinic start implementing AI?
You don't need a massive budget to begin. The key for smaller organizations is to start with a specific, well-defined problem where AI can deliver clear value. Focus on a high-impact use case, such as automating patient scheduling, streamlining medical billing, or using a simple diagnostic aid. Launching a targeted pilot project allows you to prove ROI, gain buy-in from your team, and learn valuable lessons before committing to a larger-scale implementation. Partnering with an AI strategy consulting firm can help identify these low-hanging-fruit opportunities.
What kind of data is needed to train medical AI models effectively?
The effectiveness of any AI model is directly tied to the quality and diversity of its training data. For medical AI, this typically includes:
- Electronic Health Records (EHRs): Rich with patient histories, diagnoses, and treatment outcomes.
- Medical Imaging: Large datasets of X-rays, MRIs, and CT scans.
- Genomic Data: DNA sequences for personalized medicine.
- Real-World Evidence: Data from wearables and patient monitoring devices.
Crucially, this data must be clean, accurately labeled, and representative of diverse patient populations to avoid building biased and ineffective models.
Ready to build your AI roadmap and turn these insights into action? Ekipa AI delivers a Custom AI Strategy report in just 24 hours, helping you identify and prioritize high-impact AI opportunities without the high cost of traditional consultants. Talk to our expert team today to get started.