8 Groundbreaking Applications of AI in Medicine for 2025
Explore the top applications of AI in medicine, from diagnostics and drug discovery to robotic surgery. See how AI is transforming healthcare in 2025.

Artificial intelligence is no longer a futuristic concept; it's actively reshaping patient care, medical research, and hospital operations. The diverse applications of AI in medicine are unlocking unprecedented efficiencies and life-saving insights, moving us toward a future of proactive, personalized, and precise healthcare. As we explored in our AI adoption guide, integrating this technology is becoming a strategic imperative for healthcare providers and requires a clear vision, from initial AI strategy consulting to implementing advanced AI Solutions.
This article dives deep into eight groundbreaking areas where AI is making a tangible impact, supported by real-world use cases that highlight its power. We will break down how AI improves diagnostics, accelerates drug discovery, and enhances patient outcomes. Whether you're considering building new healthcare software development capabilities or implementing workflow automation, understanding these applications is the first step toward harnessing the technology's full potential.
For leaders in healthcare, the challenge is not just technological but also ethical. Integrating these powerful systems responsibly requires careful planning, and understanding AI usage policy considerations is crucial for building trust and ensuring compliance in this sensitive sector. The following examples provide a strategic roadmap for implementing AI effectively, offering actionable insights for transforming clinical and operational workflows. We'll explore the strategic behind-the-scenes details, providing replicable methods for deploying these innovative solutions.
1. Medical Image Analysis and Diagnostics
Medical image analysis is one of the most mature and impactful applications of AI in medicine. This technology leverages deep learning algorithms, specifically Convolutional Neural Networks (CNNs), to interpret medical images like X-rays, CT scans, and MRIs. These systems can identify subtle patterns, abnormalities, and disease markers that may be invisible to the human eye, enabling earlier and more precise diagnoses.
The primary function is to augment, not replace, the expertise of human radiologists. By rapidly screening thousands of images and flagging potential issues, AI acts as a powerful decision-support tool. It significantly reduces the time to diagnosis for critical conditions, minimizes the risk of human error from fatigue, and allows medical professionals to focus their attention on complex cases requiring nuanced judgment. For healthcare organizations, this translates into improved patient outcomes, increased operational efficiency, and a more manageable workload for specialized staff.
Strategic Breakdown and Analysis
Companies like Aidoc and Zebra Medical Vision showcase the technology's real-world impact. Aidoc’s AI, for example, runs in the background of a hospital's imaging workflow, automatically analyzing scans for critical findings like intracranial hemorrhage or pulmonary embolism. When it detects a positive case, it immediately notifies the radiologist.
- Tactical Insight: This "always-on" approach transforms radiology from a reactive to a proactive service. Instead of waiting for a radiologist to review a scan in a queue, the system prioritizes life-threatening cases in real-time.
- Actionable Takeaway: Integrate AI directly into existing Picture Archiving and Communication Systems (PACS) for seamless adoption. A successful AI Product Development Workflow ensures the tool enhances, rather than disrupts, established clinical processes.
Similarly, PathAI has demonstrated that its algorithms can improve the accuracy of cancer diagnosis from pathology slides by up to 85%. This level of precision helps oncologists develop more effective, personalized treatment plans from the outset.
Key Strategic Point: The core value proposition is not just speed, but a quantifiable improvement in diagnostic accuracy. This dual benefit makes a compelling business case for investment in healthcare software development that incorporates AI.
Visualizing Progress in AI Medical Imaging
The following timeline highlights key milestones in the development and adoption of AI for medical diagnostics, showing its rapid progression from research to regulatory approval and significant market growth.
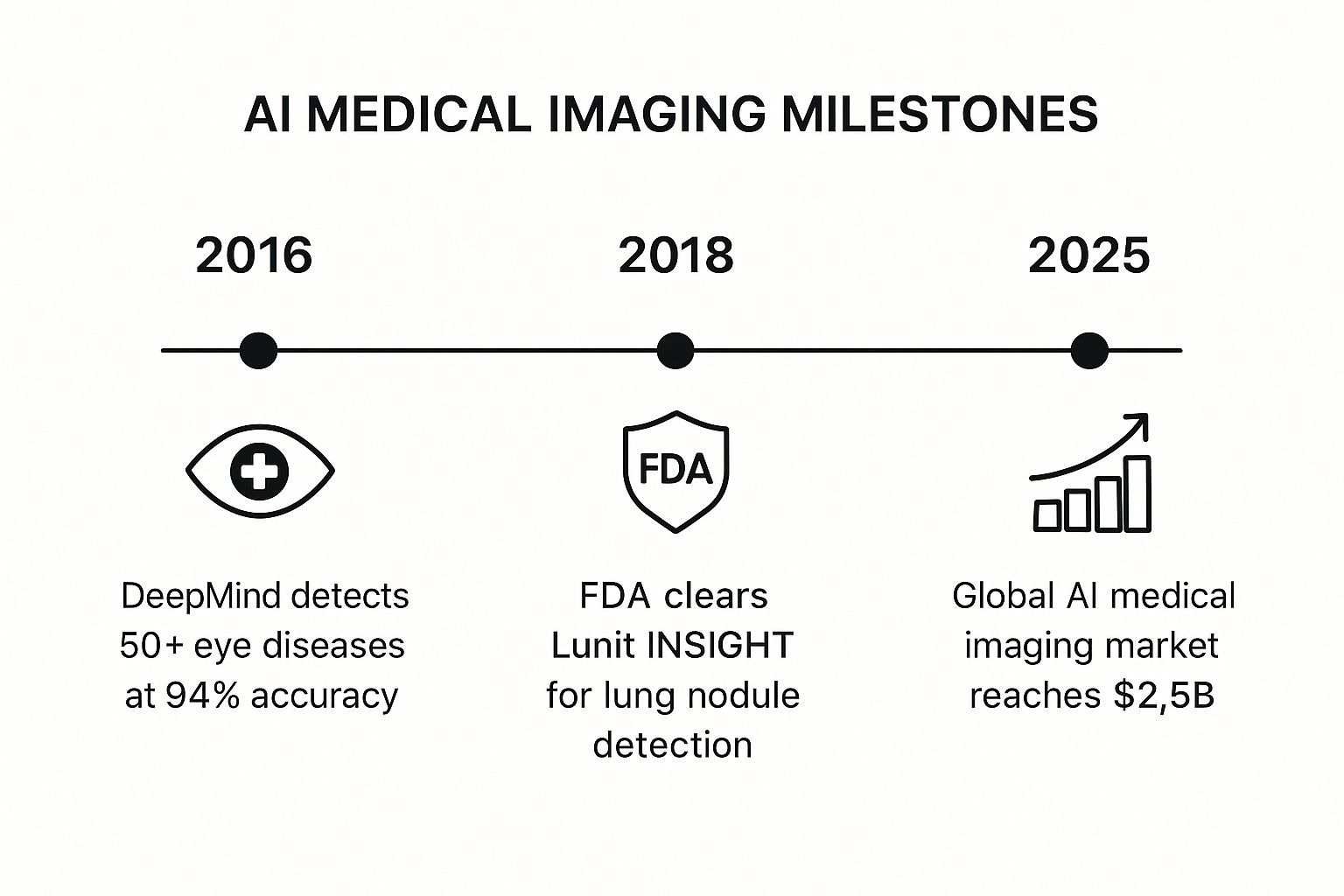
This progression from a groundbreaking accuracy benchmark in 2016 to FDA clearance in 2018 and a projected multi-billion dollar market by 2025 underscores the technology's rapid maturation and commercial viability.
2. Drug Discovery and Development
AI is dramatically reshaping pharmaceutical R&D, positioning itself as one of the most transformative applications of AI in medicine. This technology uses sophisticated machine learning models to analyze immense biological and chemical datasets, accelerating the traditionally slow and costly process of discovering new drugs. By predicting how molecules will behave and identifying promising candidates, AI can compress a development timeline that once took over a decade down to just a few years.
The core function of AI in this domain is to rapidly sift through billions of potential compounds to find those with the highest probability of success. It identifies novel therapeutic targets, optimizes molecular structures for efficacy and safety, and even predicts clinical trial outcomes. This allows pharmaceutical companies to de-risk their pipelines, reduce failure rates, and focus resources on the most viable drug candidates, ultimately getting life-saving treatments to patients faster.
Strategic Breakdown and Analysis
Companies like Insilico Medicine and Exscientia are pioneering this AI-driven revolution. Insilico Medicine famously identified a novel drug candidate for idiopathic pulmonary fibrosis in just 46 days, a process that would typically take years. Their platform uses generative AI to design new molecules from scratch that meet specific therapeutic criteria.
- Tactical Insight: This "generative chemistry" approach moves beyond merely screening existing compounds. It actively creates new, optimized molecular structures, opening a vast design space that was previously inaccessible to human chemists.
- Actionable Takeaway: To succeed, pharmaceutical companies must integrate AI-powered workflow automation with traditional lab validation. Combining predictive power with empirical testing creates a high-throughput, closed-loop system for rapid discovery and iteration.
Similarly, Exscientia developed the first-ever AI-designed drug to enter human clinical trials. By automating the design process, they significantly reduced the number of compounds that needed to be synthesized and tested, demonstrating massive gains in efficiency and cost savings.
Key Strategic Point: The primary business value is not just speed but a drastic improvement in capital efficiency. By minimizing late-stage failures and optimizing resource allocation, AI provides a powerful competitive advantage in a high-risk industry. Developing a sound AI strategy consulting plan is crucial for this.
3. Predictive Analytics and Early Disease Detection
Predictive analytics is one of the most proactive applications of AI in medicine, shifting the focus from reaction to prevention. This technology uses machine learning algorithms to analyze vast datasets, including electronic health records (EHRs), genetic information, and lifestyle factors. By identifying subtle patterns and hidden correlations, these systems can predict the likelihood of a patient developing a specific disease long before clinical symptoms appear.
The primary goal is to empower clinicians with foresight, enabling early intervention when treatments are most effective and less invasive. Instead of waiting for a condition to manifest, healthcare providers can implement preventative measures or targeted screenings for high-risk individuals. For healthcare organizations, this predictive capability reduces long-term treatment costs, improves patient outcomes, and supports population health management strategies by identifying at-risk cohorts.
Strategic Breakdown and Analysis
Companies like KenSci and Tempus are pioneering this predictive frontier. KenSci’s platform, for instance, can predict the onset of sepsis, a life-threatening condition, 12 to 18 hours before it would be clinically apparent, with a reported accuracy of over 80%. This provides a critical window for intervention that can dramatically reduce mortality rates.
- Tactical Insight: The system integrates directly with existing EHRs, analyzing real-time data streams to generate risk scores. This seamless integration ensures that alerts are delivered within the clinician's existing workflow automation, prompting timely action without disrupting established processes.
- Actionable Takeaway: To deploy predictive models successfully, prioritize data quality and completeness. A robust data pipeline is the foundation for accurate predictions, making investment in data infrastructure as critical as the AI algorithm itself.
Similarly, Tempus utilizes AI to analyze clinical and molecular data, helping oncologists predict cancer progression and select the most effective therapies. By structuring vast amounts of unstructured data, Tempus provides actionable insights that guide personalized treatment decisions.
Key Strategic Point: The strategic advantage lies in transforming historical patient data into a predictive asset. This proactive approach not only improves individual patient care but also provides invaluable data for advancing clinical research and drug development.
Visualizing Progress in Predictive Healthcare
The following timeline highlights key milestones in the development and application of predictive analytics in medicine, showcasing its evolution from identifying risk factors to real-time clinical decision support. This progression illustrates the growing trust in and reliance on AI-driven predictions within clinical settings.
The journey from early risk-scoring models to sophisticated, real-time prediction engines integrated into hospital systems highlights the technology’s increasing importance. The projected market growth underscores its established value and expected expansion across more medical specialties.
4. Virtual Health Assistants and Chatbots
Among the most patient-facing applications of AI in medicine are virtual health assistants and chatbots. These conversational AI systems leverage natural language processing (NLP) to provide 24/7 healthcare support directly to users. They can answer medical questions, perform initial symptom triage, schedule appointments, and even deliver medication reminders, acting as a scalable first point of contact for health systems.
The core function of these assistants is to improve healthcare accessibility and efficiency. By handling routine inquiries and guiding patients to the appropriate level of care, they significantly reduce the administrative burden on human medical staff. This allows clinicians to focus on more complex patient needs while ensuring that users receive immediate, reliable, and evidence-based information, which is a key goal for any organization investing in healthcare software development.
Strategic Breakdown and Analysis
Companies like Ada Health and Woebot exemplify the diverse capabilities of this technology. Ada Health has built a sophisticated symptom checker used in over 130 countries, providing personalized health assessments that help users understand their symptoms and decide on the next steps for care.
- Tactical Insight: The primary tactic is to provide an accessible, user-friendly interface that builds trust. Ada achieves this by communicating the limitations of the AI and clearly stating when a user should consult a human doctor, managing expectations effectively.
- Actionable Takeaway: A successful implementation requires a robust, medically-validated knowledge base that is continuously updated. Organizations looking to build a similar tool, like a clinic AI assistant, must prioritize medical accuracy and establish clear escalation paths to human providers.
Meanwhile, Woebot Health targets the mental health space, using its chatbot to deliver principles of Cognitive Behavioral Therapy (CBT). Its conversational approach makes mental health support more accessible and less intimidating, with studies showing significant reductions in symptoms of depression and anxiety among its users.
Key Strategic Point: The strategic value here is scalability and de-stigmatization. AI chatbots can provide consistent, private mental health support to millions of users simultaneously, reaching populations that might otherwise avoid traditional therapy.
Visualizing Progress in AI-Powered Virtual Health
The timeline below illustrates the rapid growth and validation of virtual health assistants, from their initial launch to achieving significant user milestones and demonstrating clinical effectiveness.
This journey from initial product launches around 2017 to reaching millions of users and publishing clinically-validated results by 2021 highlights the technology's powerful impact on patient engagement and healthcare accessibility.
5. Robotic Surgery and Surgical Assistance
Robotic surgery represents one of the most advanced and tangible applications of AI in medicine, enhancing surgical procedures with unparalleled precision and control. This technology integrates AI, computer vision, and advanced robotics to give surgeons superhuman capabilities. These systems are not autonomous but act as sophisticated tools that translate a surgeon's hand movements into micro-movements, filtering out tremors and enabling minimally invasive techniques that would be impossible with the human hand alone.
The primary goal is to improve patient outcomes by enabling more complex procedures to be performed through tiny incisions. This approach leads to reduced blood loss, less pain, shorter hospital stays, and quicker recovery times. For surgeons, AI-powered robotic systems provide superior 3D visualization of the surgical site and greater dexterity. For healthcare providers, this translates to higher surgical success rates, fewer complications, and increased capacity to handle complex cases, ultimately boosting the organization's reputation and efficiency.
Strategic Breakdown and Analysis
Intuitive Surgical's da Vinci system is the most prominent example, having been used in millions of procedures worldwide. The system provides surgeons with a magnified, high-definition 3D view and uses tiny wristed instruments that bend and rotate far greater than the human hand. It's a prime example of how AI can augment human skill rather than replace it.
- Tactical Insight: The da Vinci system’s success lies in its ecosystem. It combines the physical robot with extensive training programs, data analytics, and dedicated support, ensuring a high standard of care and effective utilization. This holistic approach makes the technology a platform, not just a product.
- Actionable Takeaway: When implementing surgical robotics, invest heavily in comprehensive surgeon and staff training programs. A phased rollout, starting with more straightforward procedures before tackling complex cases, ensures a safe and effective adoption curve that aligns with your workflow automation goals.
Similarly, newcomers like CMR Surgical with its Versius system are making robotic surgery more accessible. Versius is designed to be modular and portable, allowing it to be moved between operating rooms and integrated into existing hospital workflows more easily than larger, fixed systems.
Key Strategic Point: The core value proposition is expanding the scope and safety of minimally invasive surgery. By reducing physical strain on surgeons and enhancing their precision, these AI-driven systems make complex surgeries more standardized and reproducible, directly impacting patient safety and hospital performance.
6. Personalized Treatment and Precision Medicine
Personalized treatment is one of the most forward-thinking applications of AI in medicine, shifting the paradigm from one-size-fits-all treatments to hyper-targeted therapies. This approach uses machine learning to analyze vast datasets, including an individual's genetic profile, biomarkers, lifestyle factors, and medical history. By identifying complex patterns within this data, AI can predict which therapeutic strategies will be most effective for a specific patient, optimizing drug selection and dosing while minimizing potential adverse reactions.
The core function is to tailor healthcare decisions to each person's unique biological makeup. AI models can sift through genomic data to identify mutations linked to specific diseases, match patients with targeted therapies, and even predict their response to treatment. For clinicians, this provides a powerful tool for creating precise, evidence-based care plans. For patients, it means moving away from trial-and-error medicine toward treatments with a higher probability of success, particularly in complex fields like oncology.
Strategic Breakdown and Analysis
Companies like Tempus and Foundation Medicine are at the forefront of this revolution. Tempus leverages AI to structure and analyze massive libraries of clinical and molecular data, making it accessible and useful for physicians. Its platform provides insights that help oncologists make personalized treatment decisions based on a patient's specific tumor profile.
- Tactical Insight: The strategy is to build a proprietary, multimodal database. By integrating genomic, transcriptomic, and clinical data, Tempus creates a comprehensive patient portrait that AI can interpret to recommend tailored therapies.
- Actionable Takeaway: To implement a similar approach, healthcare organizations must invest in data infrastructure that can unify disparate sources. Integrating AI with existing EHR and laboratory systems is critical for creating the holistic datasets needed for effective precision medicine.
Similarly, Deep 6 AI uses natural language processing to analyze unstructured clinical data, like doctor's notes and pathology reports, to match patients with eligible clinical trials in real-time. This accelerates the recruitment process, which is a major bottleneck in drug development, and connects patients with cutting-edge treatments they might otherwise miss.
Key Strategic Point: The value lies in transforming unstructured, real-world data into actionable clinical intelligence. This capability not only improves individual patient outcomes but also accelerates the entire therapeutic research and development cycle. For a deeper look at how AI is shaping the industry, explore our insights on AI's role in the healthcare sector.
7. Remote Patient Monitoring and Wearable Health Devices
Remote patient monitoring (RPM) represents a proactive shift in healthcare, moving from reactive clinical visits to continuous, real-time health management. This is one of the most transformative applications of AI in medicine, leveraging AI-enabled wearable devices and at-home sensors to collect a constant stream of physiological data. Machine learning algorithms analyze this data-including vital signs, activity levels, and sleep patterns-to detect subtle deviations from a patient's baseline that could signal impending health issues.
The core function is to empower providers with early warnings, enabling preemptive interventions before a condition escalates into a critical event. By identifying patterns indicative of health deterioration, these systems help manage chronic diseases like heart failure and diabetes, monitor post-surgical recovery, and support elderly patients living independently. For healthcare systems, this translates into a significant reduction in costly hospital readmissions, improved patient engagement, and the ability to manage larger patient populations more efficiently with existing staff.
Strategic Breakdown and Analysis
Companies like Biofourmis and Current Health (now Best Buy Health) exemplify the power of predictive analytics in remote care. Biofourmis's AI-driven platform has been shown to detect signs of heart failure decompensation over 10 days before a patient typically presents with symptoms, providing a crucial window for intervention. Current Health’s solution has demonstrated the ability to reduce hospital readmissions by over 50% by continuously monitoring at-risk patients after discharge.
- Tactical Insight: The true innovation lies not just in data collection but in intelligent filtering. The AI's ability to distinguish clinically significant alerts from benign fluctuations prevents "alert fatigue," ensuring that clinicians only focus on patients who genuinely need immediate attention.
- Actionable Takeaway: Successful RPM deployment requires integrating the AI data stream directly into care coordination workflows. This ensures that alerts trigger a predefined, effective clinical response, turning raw data into life-saving action through robust workflow automation.
Similarly, the Apple Watch's FDA-cleared ECG app uses algorithms to detect atrial fibrillation (AFib) with up to 98% specificity, empowering millions of consumers to identify a serious heart condition that often goes undiagnosed. This mainstream adoption is rapidly normalizing the concept of continuous, AI-powered health monitoring.
Key Strategic Point: The strategic value of AI in RPM is its ability to make healthcare delivery continuous and predictive rather than episodic and reactive. This fundamental shift improves outcomes while creating a more sustainable and scalable model for chronic care management.
Visualizing Progress in Remote Patient Monitoring
The timeline below illustrates key developments that have propelled AI-powered remote monitoring from a niche concept to a mainstream component of modern healthcare, highlighting its journey from consumer tech to clinically validated systems.
The progression from the first FDA-cleared consumer wearable feature in 2018 to a projected market size exceeding $100 billion by 2027 shows the immense confidence and investment in this technology as a pillar of future healthcare delivery.
8. Clinical Documentation and Administrative Automation
Administrative burden is a primary driver of physician burnout, and automating clinical documentation stands out as one of the most practical applications of AI in medicine. This technology uses Natural Language Processing (NLP) and advanced speech recognition to transform unstructured physician-patient conversations into structured, coded clinical notes. It streamlines a process that traditionally consumes up to half of a clinician's workday, directly combating professional fatigue and improving job satisfaction.
The core function of these AI systems is to act as an intelligent scribe, freeing physicians to focus entirely on patient interaction. By automating medical coding, billing, and prior authorizations through AI Automation as a Service, AI significantly reduces administrative overhead and minimizes costly errors. For healthcare organizations, this automation leads to faster revenue cycles, improved documentation accuracy for compliance and analytics, and a dramatic increase in operational efficiency, allowing staff to handle higher-value, patient-facing tasks.
Strategic Breakdown and Analysis
Companies like Nuance Communications (now part of Microsoft) and DeepScribe are at the forefront of this transformation. Nuance’s Dragon Medical One platform, for example, has been shown to reduce documentation time for physicians by as much as 45% by allowing them to dictate notes conversationally, which are then transcribed accurately into the Electronic Health Record (EHR).
- Tactical Insight: The most effective tools are ambient, operating seamlessly in the background of a clinical encounter without requiring active physician management. This "invisible" integration is key to high adoption rates.
- Actionable Takeaway: When implementing these systems, prioritize a seamless connection with existing EHR platforms. An AI-powered data extraction engine can ensure that data captured by the AI is correctly structured and mapped to the right fields in the patient record.
Similarly, Notable Health automates prior authorizations, a notorious bottleneck, reducing patient wait times by over 80%. This directly improves patient access to care and reduces the administrative workload on clinic staff. AI's role in administrative efficiency also extends to automating meeting documentation, with Meeting Minutes AI tools offering practical solutions for smarter note-taking in healthcare settings.
Key Strategic Point: The value extends beyond simple time savings; it lies in creating more complete and accurate clinical data. This high-quality data becomes a strategic asset for population health management, clinical research, and quality reporting initiatives.
Applications of AI in Medicine: 8-Point Comparison
| Application Area | Implementation Complexity | Resource Requirements | Expected Outcomes | Ideal Use Cases | Key Advantages |
|---|---|---|---|---|---|
| Medical Image Analysis and Diagnostics | High: Requires large training data and regulatory approval | High computational power, annotated imaging datasets | Improved diagnostic accuracy, faster image analysis | Radiology, pathology, early disease detection | Reduces errors, enables 24/7 analysis, decreases radiologist workload |
| Drug Discovery and Development | Very High: Complex biological data integration and validation | Extensive biological databases, high computational costs | Shortened drug development timeline, cost reduction | Pharmaceutical R&D, clinical trial support | Accelerates discovery, predicts drug safety, enables repurposing |
| Predictive Analytics and Early Disease Detection | Moderate: Needs interoperable health data systems | Comprehensive patient EHRs, genetic and lifestyle data | Early disease prediction, preventive interventions | Population health, chronic disease management | Reduces costs, supports value-based care, improves outcomes |
| Virtual Health Assistants and Chatbots | Moderate: NLP development and system integration | NLP models, user data, ongoing updates | 24/7 patient support, symptom triage, appointment scheduling | Patient engagement, primary triage | Increases access, reduces ER visits, scalable to millions |
| Robotic Surgery and Surgical Assistance | Very High: Requires specialized hardware and surgeon training | Multi-million dollar equipment, training programs | Increased surgical precision, reduced complications | Minimally invasive surgery, complex procedures | Enhances precision, reduces recovery time, tremor filtration |
| Personalized Treatment and Precision Medicine | High: Genetic data analysis and multi-omics integration | Expensive genetic testing, specialized expertise | Tailored therapies, optimized dosing, fewer side effects | Oncology, rare diseases, clinical trial matching | Improves treatment efficacy, reduces adverse reactions, accelerates trials |
| Remote Patient Monitoring and Wearable Health Devices | Moderate: Device integration and real-time analytics | Wearable devices, data connectivity, monitoring platforms | Continuous health monitoring, early intervention alerts | Chronic disease management, elderly care | Reduces readmissions, empowers patients, lowers healthcare costs |
| Clinical Documentation and Administrative Automation | Moderate: NLP and EHR integration | Speech recognition systems, clinical coding databases | Reduced documentation time, improved billing accuracy | Physician workflow, medical billing | Cuts documentation time, decreases burnout, increases revenue |
Frequently Asked Questions (FAQs)
What is the most common application of AI in medicine?
Medical image analysis is one of the most mature and widely adopted applications of AI in medicine. AI algorithms excel at detecting patterns in X-rays, CT scans, and MRIs to help radiologists identify diseases like cancer or stroke with greater speed and accuracy.
How is AI used for patient care?
AI directly impacts patient care through personalized treatment plans, early disease prediction, and virtual health assistants. For example, AI can analyze a patient's genetic data to recommend the most effective cancer therapy or power a 24/7 chatbot to answer health questions and triage symptoms.
What are the main challenges of implementing AI in healthcare?
The primary challenges include ensuring data privacy and security (HIPAA compliance), integrating AI tools with existing Electronic Health Record (EHR) systems, overcoming regulatory hurdles for new medical devices, and addressing potential biases in AI algorithms that could lead to health disparities.
Can AI replace doctors and other healthcare professionals?
No, the goal of AI in medicine is to augment, not replace, human professionals. AI serves as a powerful decision-support tool, automating repetitive tasks, analyzing complex data, and providing insights to help clinicians make faster, more informed decisions. The empathy, critical thinking, and nuanced judgment of a human provider remain irreplaceable.
Bringing AI-Powered Healthcare into Your Practice
Throughout this deep dive into the diverse applications of AI in medicine, a clear and consistent theme emerges: artificial intelligence is no longer a futuristic concept but a present-day catalyst for transformation. We've journeyed from the microscopic precision of AI in drug discovery and personalized treatment plans to the macroscopic efficiency it brings to administrative automation and operational logistics. The overarching takeaway is that AI integration is not about replacing human expertise but augmenting it, creating a powerful synergy that enhances diagnostic accuracy, accelerates research, and personalizes patient care at an unprecedented scale.
The examples we've explored, from AI-powered medical imaging analysis that detects diseases earlier to virtual health assistants that improve patient engagement, showcase a strategic shift. Healthcare organizations are moving beyond isolated pilot projects to build comprehensive ecosystems where data-driven insights inform every decision. This evolution from tactical implementation to strategic integration is the key differentiator for institutions leading the charge in modern healthcare.
Key Takeaways and Your Strategic Next Steps
To translate these insights into a tangible advantage for your organization, it's crucial to distill the core lessons. The most successful applications of AI in medicine are not born from chasing technology but from a relentless focus on solving specific, high-impact problems within the healthcare value chain.
Here are the actionable steps to begin your journey:
- Identify Your Core Challenge: Before exploring any AI tools for business, pinpoint your most pressing operational or clinical bottleneck. Is it diagnostic delays, administrative overhead, or the challenge of managing chronic diseases? A clear problem statement is the foundation of a successful AI initiative, which can be refined with a Custom AI Strategy report.
- Start with Data-Rich, High-Impact Areas: Begin with applications where you have access to high-quality, structured data, such as medical imaging or clinical trial results. Early wins in these areas can build momentum and demonstrate ROI, paving the way for more complex projects.
- Prioritize Augmentation, Not Just Automation: The most valuable AI systems empower your clinical staff, not replace them. Focus on developing internal tooling that reduces cognitive load, automates repetitive tasks through workflow automation, and provides decision support, freeing up professionals to focus on critical thinking and patient interaction.
- Develop a Scalable AI Roadmap: A successful AI strategy is not a one-off project. It requires a long-term vision. This involves building a robust AI Product Development Workflow and considering how individual solutions will integrate into a larger, cohesive intelligence layer across your organization. As we explored in our AI adoption guide, a phased approach is critical for sustainable success.
By focusing on these strategic pillars, you can navigate the complexities of AI adoption and unlock its profound potential. Whether you're a hospital administrator looking to optimize resource allocation, a pharmaceutical leader aiming to shorten drug development cycles, or a clinician seeking to deliver more precise care, the principles remain the same. The future of healthcare is intelligent, and mastering these applications of AI in medicine is no longer optional; it's essential for competitive advantage and, most importantly, for advancing patient outcomes. Building this future requires a blend of medical expertise, technological prowess, and strategic foresight, a journey best undertaken with a knowledgeable partner.
Ready to move from theory to implementation? Ekipa AI specializes in crafting and executing bespoke AI strategies for the healthcare sector, turning complex challenges into data-driven solutions. Explore our AI Solutions or schedule a consultation with our expert team to discover how we can help you build the future of intelligent healthcare, today.