AI Usage in Medical Field A Practical Clinic Guide
Discover practical AI usage in medical field, from diagnostics to operations. Learn benefits, challenges, and how to implement AI in your clinic.
Artificial intelligence isn't just a buzzword in medicine anymore—it's actively changing how we diagnose illnesses, treat patients, and run our clinics. What was once theoretical is now becoming a practical set of tools used daily to improve patient outcomes and make our healthcare systems work better.
To get this right, many organizations are working with experts to build effective AI solutions that fit right into their existing workflows without causing disruption.
How AI Is Reshaping Modern Medicine
AI has officially moved out of the lab and into the clinic. This is a huge shift, giving doctors and nurses powerful new capabilities to analyze complex medical data with a speed and accuracy that was previously impossible.
Think of AI as a brilliant assistant. It can sift through mountains of data, spot nearly invisible patterns in medical scans, and even help predict which patients are at higher risk for certain conditions. It's no surprise that the global AI in healthcare market, valued at $16.61 billion in 2024, is expected to skyrocket. The goal here isn't to replace doctors but to enhance their expertise.
The Shift from Theory to Practice
For a long time, the idea of AI in medicine was just that—an idea. Now, we’re seeing real-world applications pop up everywhere, delivering measurable improvements in patient care and operational efficiency. These aren't just science projects; they are tools built to help clinicians, reduce administrative headaches, and speed up critical research.
Let's break down where AI is already making a difference:
- Smarter Diagnostics: AI algorithms are proving incredibly good at analyzing MRIs, X-rays, and CT scans. They can flag subtle anomalies for a radiologist to review, acting as a second set of highly trained eyes.
- Personalized Treatment: By looking at a patient's unique genetic makeup, lifestyle, and medical history, AI can help map out truly customized treatment plans. This is a big step away from the one-size-fits-all model.
- Operational Efficiency: AI is a workhorse for the routine stuff. It can manage appointment scheduling, automate billing codes, and organize patient records, freeing up staff to focus on what matters most: the patients. The rise of AI Automation as a Service is a game-changer for streamlining these tasks.
The core of this movement is the jump from potential to practice. It’s all about using intelligent tools to empower human experts so they can deliver better, faster, and more efficient care.
Figuring out where to start can be daunting. Many healthcare leaders kick off their journey with AI strategy consulting to pinpoint the best opportunities within their own hospitals or clinics. For deeper dives and ongoing discussions on this topic, check out the resources on Ekipa AI blog for insights. Once you understand the practical applications, you can start building a clear plan for how this technology can serve your patients and your organization.
AI is Giving Clinicians a Second Set of Eyes in Medical Imaging
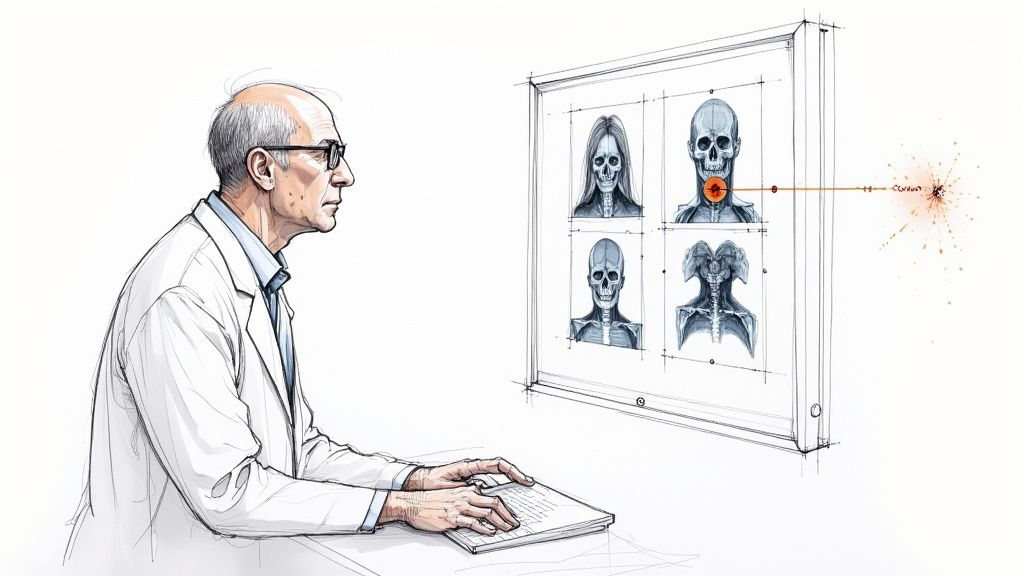
Imagine a radiologist working alongside a tireless partner, one that can spot patterns completely invisible to the human eye. That’s exactly what AI is bringing to medical imaging. We're seeing a fundamental shift in this field as machine learning models, trained on millions of scans, start to amplify the skills of clinicians.
These systems tear through complex images from X-rays, CT scans, and MRIs with incredible speed and precision. They’re built to flag subtle signs of conditions like cancer, diabetic retinopathy, and neurological disorders—often far earlier than humanly possible. The growth here is staggering, with 80% of hospitals now utilizing AI in some form to improve care and streamline operations.
This isn't about replacing doctors. It's about empowering them with better tools. Think of AI as an expert second opinion, flagging potential issues for review, which in turn reduces diagnostic errors and gets answers to patients faster.
Boosting Both Accuracy and Speed
One of the biggest wins with AI in imaging is its sheer capacity to process massive amounts of data without getting tired. A human radiologist might expertly review dozens of complex scans in a day, but an AI can analyze thousands in that same period without its accuracy ever wavering.
For example, an AI model can be trained to pinpoint tiny cancerous nodules on a lung scan that might otherwise be overlooked in a routine check. In ophthalmology, algorithms can spot the earliest signs of diabetic retinopathy from retinal photos, enabling intervention long before a patient’s vision is at risk.
The real magic of AI in diagnostics is how it enhances human expertise. By taking on the high-volume, repetitive pattern-recognition work, it frees up clinicians to focus on the most complex cases, connect with patients, and map out treatment plans.
This partnership between human and machine is rapidly setting a new standard of care, leading to diagnoses that are both faster and more reliable.
How This Is Already Affecting Patient Outcomes
This isn't just theory; AI-powered diagnostics are actively saving lives today. Take oncology, where AI tools help clinicians map out tumors for radiation therapy with pinpoint precision, which is critical for minimizing damage to surrounding healthy tissue.
The impact is clear across a range of specialties:
- Stroke Detection: AI algorithms can analyze a brain scan in just minutes to find signs of a stroke, helping doctors deliver time-critical treatments much more quickly.
- Cardiology: Certain models can evaluate cardiac MRIs to predict a patient's risk of heart failure, giving cardiologists the data they need to build proactive treatment plans.
- Dermatology: AI-powered smartphone apps can analyze photos of skin lesions to estimate the likelihood of malignancy, encouraging people to see a doctor sooner.
These examples show that the use of AI in the medical field has moved far beyond the conceptual stage. In fact, entire platforms are being designed to make this process seamless. For instance, our team developed a platform specifically for managing, annotating, and analyzing medical images to accelerate diagnostic workflows. If you're curious about how Ekipa's Diagnoo platform helps healthcare professionals, you can read our guide on Diagnoo.
This deep integration of technology is making diagnostics more accurate, accessible, and ultimately, more affordable.
Accelerating Drug Discovery and Research
It’s not just inside the clinic where AI is making its mark. The ai usage in medical field is fundamentally rewriting the playbook for pharmaceutical research and development. Traditionally, getting a new drug from a lab to the pharmacy shelf is a marathon—a journey that can take more than a decade and cost billions, with countless dead ends along the way.
AI is stepping in as a super-powered research assistant, crunching massive amounts of biological data at a speed and scale no human team could ever match. Instead of scientists manually sifting through thousands of chemical compounds, AI models can scan genomic and proteomic libraries to flag the most promising candidates in a tiny fraction of the time. This frees up researchers to focus on molecules that actually have a shot, cutting down on early-stage failures and speeding up the whole pipeline.
Pinpointing Promising Drug Candidates
At its heart, drug discovery is a complex matching game: you need to find the perfect molecule that interacts with a specific biological target to combat a disease. AI is a natural fit for this, finding subtle patterns in colossal datasets that would otherwise go unnoticed.
Machine learning algorithms can predict how a potential drug might bind to a protein, forecast its likely effectiveness, and even flag potential side effects—all before a single vial is prepared in the lab.
This kind of predictive insight is a massive leap forward. In cancer therapy, for example, AI can dive into "deep-level information in genomics" to uncover new drug targets or even help design treatments tailored to a patient’s specific tumor profile. It’s a huge part of the shift toward true precision medicine.
AI doesn't just find needles in haystacks; it analyzes the entire haystack to predict where the needles are most likely to be. This predictive capability turns a process of chance into one of calculated strategy, saving invaluable time and resources.
By digging into these real-world use cases, you can see how AI is no longer a small, incremental tool but a foundational part of modern medical innovation.
Redesigning Clinical Trials for Better Outcomes
Finding a promising drug candidate is just the first step. The clinical trial phase is notoriously slow, incredibly expensive, and often struggles with one of its biggest hurdles: finding the right patients. AI brings a powerful set of tools to the table that can streamline this critical stage and boost the odds of success.
For starters, AI models can comb through millions of electronic health records to find the ideal patient group for a specific trial. This ensures the people selected are genuinely the best fit for the drug being tested, which not only speeds up recruitment but also improves the quality of the data collected.
AI's contribution doesn't stop there. It helps across the board:
- Optimizing Trial Design: Algorithms can run simulations of a trial using different setups, helping researchers design studies that can deliver clear results with fewer participants.
- Monitoring and Adherence: AI-powered apps and wearables can track whether patients are sticking to the trial protocol in real time, sending alerts that help keep the study on course.
- Predicting Outcomes: By analyzing early data as it comes in, AI can help predict which patient groups are responding best, allowing for adaptive trial designs that can pivot to focus on what’s working.
Getting this right requires a solid game plan, which is why many organizations start with a Custom AI Strategy report to map out their R&D objectives from the beginning.
The collective impact of AI on drug discovery is enormous. It's shortening timelines, cutting costs, and improving the probability of success. Ultimately, AI is helping get new, life-saving medicines to patients faster than ever before—a critical advantage when facing some of the world's toughest health challenges. Seeing the whole journey laid out in an AI Product Development Workflow shows just how structured this process has become.
Enhancing Clinic Operations and Patient Care
AI's role in healthcare isn't just confined to the high-tech worlds of diagnostics and drug discovery. It’s also making a massive difference on the ground, changing how clinics manage their day-to-day work and interact with patients. These AI-powered tools have moved from being a futuristic concept to a practical reality, tackling some of the most persistent administrative and patient-facing challenges. Partnering with a custom healthcare software development firm can accelerate this transformation.
This couldn't come at a better time. Physician burnout is a serious issue, and a huge part of it stems from the mountain of administrative work, like constantly updating electronic health records. By automating the repetitive, time-draining tasks, AI gives doctors, nurses, and staff their time back, letting them focus on what they do best: caring for patients.
Automating the Administrative Burden
Picture a clinic where the calendar seems to manage itself—scheduling appointments, handling billing, and sending patient follow-ups without constant human intervention. That's exactly what AI-driven systems are starting to deliver. They can intelligently predict patient no-shows, optimize the schedule to cut down on wait times, and automate routine communications like appointment reminders or post-visit care instructions.
This isn't just a minor convenience; it fundamentally lightens the load on administrative teams. Clinics using these tools can often see more patients without overwhelming their staff, all while lowering operational costs and cutting down on simple human errors in billing and record-keeping. AI-powered transcription is a perfect example. A doctor can simply speak their notes, and the system instantly converts that audio into structured text within the patient's EHR, saving critical minutes after every single visit.
Improving the Patient Journey
A great patient experience doesn’t start when the doctor walks in the room. It begins the moment a person decides they need care and continues long after they've left the clinic. AI is becoming a key player in making that entire journey smoother and more personal.
It touches several key points along the way:
- Intelligent Triage: AI-powered symptom checkers can help patients get a better sense of their condition's urgency. Based on their inputs, the tool can guide them to the right care setting—be it a telehealth appointment, an urgent care visit, or the emergency room.
- Personalized Communication: Instead of generic pamphlets, AI can send health information, medication reminders, and follow-up plans tailored to the individual. This personal touch helps patients stick to their treatment plans and stay engaged in their own health.
- Efficient Scheduling: Forget phone tag and endless email chains. Patients can now interact with AI assistants to book appointments whenever it's convenient for them, quickly finding a slot that works without the hassle.
By taking over routine interactions and adding a layer of personalization, AI helps build a stronger, more trusting relationship between the patient and the clinic. When patients feel supported and informed every step of the way, they're not only more satisfied—they often see better health outcomes.
The shift from old-school methods to AI-supported workflows is striking. This table shows just how much changes when AI is brought into the picture, highlighting clear wins in efficiency, accuracy, and the patient experience.
Comparison of Traditional vs AI-Enhanced Healthcare Processes
Healthcare Process Traditional Approach AI-Enhanced Approach
Appointment Scheduling
Manual phone calls, long wait times, high potential for human error.
Automated booking via chatbot, optimized schedules, predictive no-show alerts.
Clinical Documentation
Manual data entry into EHRs, time-consuming for clinicians.
Voice-to-text transcription, automated data structuring, reduced administrative burden.
Patient Triage
Nurse-led phone triage, potential for inconsistent advice.
AI-powered symptom checker provides instant, standardized guidance.
Billing and Coding
Manual coding and claim submission, prone to errors and delays.
Automated code suggestions based on clinical notes, faster claim processing.
Bringing these systems on board really does transform a clinic's operational backbone. Virtual assistants built for healthcare are a great example of this in action. To see how this works in practice, you can learn more about how Ekipa's Clinic AI Assistant helps manage both patient interactions and administrative duties. Ultimately, this isn't just about plugging in new tech; it's a strategic decision to build a more efficient and patient-focused practice.
Navigating the Challenges and Ethical Questions
Bringing AI into medicine isn't just a technical challenge; it comes with serious responsibilities. While the potential benefits are enormous, we have to move forward carefully, balancing progress with critical issues like data privacy, regulatory hurdles, and the very real risk of algorithmic bias. Rushing ahead without a solid ethical framework can shatter patient trust and, frankly, create more problems than it solves.
One of the biggest conversations happening right now is about the "black box" problem. This is when an AI gives you a startlingly accurate prediction, but you have no idea how it got there. For a doctor who needs to explain a diagnosis or treatment plan to a patient, that lack of transparency is a non-starter. Trust in medicine relies on understanding the "why," and leaning on an unexplainable algorithm makes that nearly impossible.
This is why a strong governance framework is essential from day one. Responsible innovation has to be the guiding principle. As we've detailed in guides on the AI Product Development Workflow, this means building AI solutions that are not just powerful, but also safe, fair, and trustworthy for every single patient.
Upholding Data Privacy and Security
In healthcare, nothing is more sensitive than patient data. AI models need massive amounts of this data to learn, which puts an even brighter spotlight on the need for bulletproof security. This isn't just a good idea—it's a legal and ethical mandate.
Protecting this information is paramount. Anyone working with these systems needs a deep understanding of HIPAA compliant document management. Any AI tool that touches patient records must be designed with compliance baked in from the very beginning to shield that data from breaches or misuse.
Key Takeaway: The conversation around AI in medicine has to start with privacy. Earning and keeping patient trust means showing an absolute commitment to protecting their data, from the first line of code to the final clinical application.
Confronting Algorithmic Bias
An AI model is a mirror; it reflects the data it's trained on. If that data contains existing biases—and healthcare data often does, showing disparities in outcomes across different populations—the AI will learn and even amplify those same biases. The result? Algorithms that are less accurate for certain groups of people, leading to genuine inequities in care.
Think about a diagnostic tool trained mostly on data from a single demographic. It might completely miss the mark when used on someone from a different background. This is where a detailed AI requirements analysis becomes so critical. It forces you to think about data diversity and fairness right from the start. The only way to fight bias is to consciously build diverse datasets and constantly check your models to make sure they're working for everyone.
Balancing Innovation with Physician Adoption
Despite these hurdles, doctors are embracing AI faster than ever. A recent AMA report revealed that 66% of U.S. physicians are now using AI tools, a massive 78% increase from just the year before. This isn't just a trend; it's a fundamental shift. With 68% of physicians believing AI has a positive impact on patient care, it’s clear they see the potential. You can discover more insights about these AI adoption trends on intuitionlabs.ai.
But this momentum hinges on one thing: building tools that clinicians actually trust and can easily fit into their day-to-day work. The goal isn't to replace a doctor's judgment but to enhance it. This requires a true partnership between developers and medical professionals to make sure the technology solves real-world problems. It's often where having our expert team involved can bridge that crucial gap between what's technically possible and what's clinically useful.
Your Roadmap to AI Implementation
Bringing AI into your practice is a strategic journey, not a quick fix. For healthcare leaders, a clear roadmap is what separates a successful initiative from a stalled one. The whole process really begins with a simple question: what are the most pressing, high-impact problems in your clinic that AI could realistically solve?
Forget about chasing flashy technology for a moment. Instead, focus on tangible needs. This could be anything from cutting down patient wait times to accelerating the analysis of routine scans or creating custom internal tooling. A thorough AI requirements analysis is the critical first step, making sure any solution you pursue is directly tied to a measurable clinical or operational goal.
Building Your Foundation
Before you can even think about implementing sophisticated algorithms, you need a solid data infrastructure. AI models are only as good as the data they’re trained on, so getting your data house in order—organizing it, cleaning it, and securing it—is an absolute must.
From there, start with small, manageable pilot projects. These initial efforts are perfect for proving the concept, working out the kinks, and getting buy-in from your team. A successful pilot can build the momentum you need for larger-scale adoption. To make sure your approach aligns with your clinic's specific goals, many leaders find it helpful to develop a Custom AI Strategy report, which lays out a clear path forward.
A responsible AI governance plan is also non-negotiable. It helps ensure your systems are not just effective but also ethical. The workflow below outlines three critical pillars for maintaining that all-important patient trust.
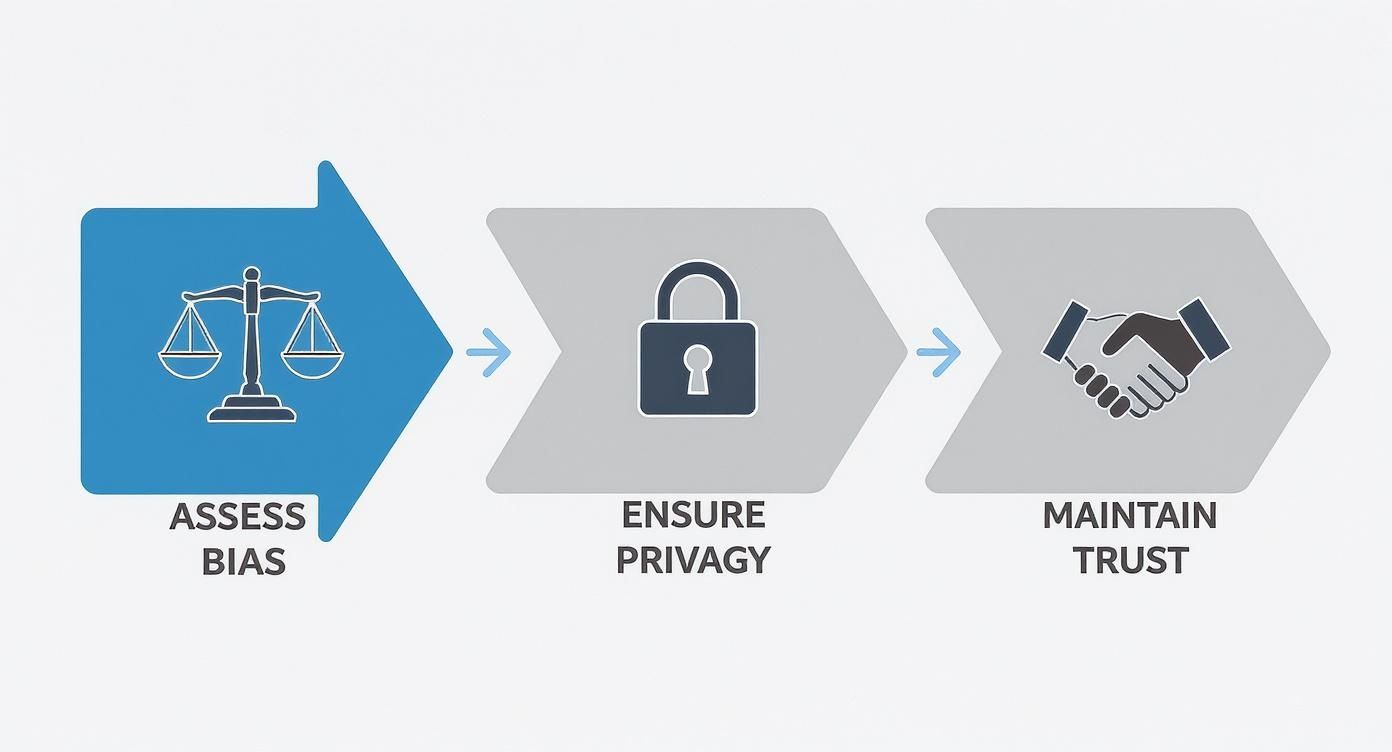
This process isn't a one-time checklist. Assessing for bias, ensuring data privacy, and maintaining trust are continuous, interwoven activities that have to be part of your daily operations.
Partnering for Success
Strategic adoption is the key to unlocking AI's full potential. The good news is, you don't have to navigate this complex field alone. Partnering with experts who understand both the technology and the unique demands of the healthcare landscape can make all the difference.
The right partnership transforms a complex technical challenge into a structured, manageable process. It ensures that your AI initiatives are not just technologically sound but also clinically relevant and seamlessly integrated into existing workflows.
A well-defined implementation plan is everything. As we've detailed in our guide on the AI Product Development Workflow, a structured approach ensures each stage, from planning to deployment, is handled with precision. By following a clear roadmap and leaning on expert guidance, you can confidently integrate AI in a way that truly benefits your patients and staff. To navigate your AI journey with confidence, consult with our expert team.
Your Questions, Answered
Diving into AI for healthcare naturally brings up a lot of questions. Let's tackle some of the most common ones I hear from leaders in the field to clear things up.
What Are the Primary Benefits of Using AI in Medicine?
The biggest wins are in four key areas. First, we're seeing a huge leap in diagnostic accuracy, especially with medical imaging where AI can spot patterns the human eye might miss. Second is the move toward truly personalized treatment plans based on a patient's unique data.
Third, AI is dramatically speeding up drug discovery and research, a process that used to take decades. And finally, there's a major boost in operational efficiency within hospitals. Think of it as reducing administrative drag so clinicians can spend more time on what matters: patient care.
We dive deeper into this topic in our blog post on the role of AI in drug development.
Will AI Replace Doctors and Medical Professionals?
Let's be clear: No. The goal of AI is to augment human expertise, not replace it. Think of AI as the most powerful assistant a doctor could ever have. It can sift through mountains of data in seconds, but it can't replicate the critical thinking, empathy, or complex ethical judgment of a trained professional.
The future isn't about machines taking over; it's a collaborative model where AI handles the heavy lifting on data, freeing up clinicians to provide better, more human-centric care.
What Are the Biggest Hurdles to AI Adoption in Healthcare?
Getting AI into a clinical setting isn't without its challenges. The biggest hurdles are often centered on data privacy and security—meeting strict HIPAA compliance is non-negotiable. We also have to tackle potential algorithmic bias to ensure AI tools provide equitable care for all patient populations.
Beyond that, you have the practical issues: navigating the complex regulatory maze for new medical devices, integrating with clunky legacy IT systems, and, frankly, earning the trust of the medical staff who will use these tools every day. As we explored in our AI adoption guide, you need a solid plan to overcome these obstacles.
How Can a Clinic Get Started with AI?
Don't try to boil the ocean. The best way to start is small and focused. Pinpoint a specific, high-impact problem you're facing right now. Maybe it's the backlog in analyzing medical images or the constant headache of patient scheduling.
Once you have your target, take a hard look at your data infrastructure and run a small pilot project to prove the concept works and delivers real value. Partnering with an expert in AI strategy consulting can help you build a practical roadmap and choose the right AI tools for business for your specific needs.
If you want to learn more about how AI can fit into your practice, feel free to connect with our expert team.
Ready to see how AI can give your organization a real advantage? At Ekipa AI, we help turn healthcare challenges into growth opportunities. Book a call with us today and let's start the conversation.