Medical Diagnosis Artificial Intelligence: A New Era
Explore how medical diagnosis artificial intelligence is transforming patient care, with real-world applications, tech trends, and practical integration tips.
For decades, clinicians have peered at grainy medical scans, searching for the subtle clues that could change a patient's life. This critical work is now getting a powerful new ally: medical diagnosis artificial intelligence. This isn't some far-off concept anymore; it's a real-world partner, working alongside doctors today.
Imagine an expert assistant that can analyze thousands of data points in seconds, spotting patterns the human eye might miss after a long shift. That's the essence of what this technology brings to the table.
The New Reality of AI in Medical Diagnosis
This guide is designed to cut through the noise and show you how AI genuinely enhances a doctor's expertise, paving the way for faster, more precise diagnoses. We'll unpack the core technologies like machine learning and computer vision, highlight its impact in specialties like radiology and oncology, and lay out a clear roadmap for putting these tools to work.

Why AI in Diagnostics Is Gaining Momentum
The move toward artificial intelligence in healthcare isn't just a tech trend—it’s a direct response to some of the biggest challenges in modern medicine. Providers are under constant pressure to deliver accurate diagnoses quickly, all while navigating a flood of patient data and often working with limited resources.
This is where AI algorithms shine. They are built to process enormous datasets from medical imaging, genomics, and electronic health records without getting tired. In oncology, for instance, AI models can analyze pathology slides to flag cancerous cells with incredible precision, helping doctors confirm findings and decide on treatment plans much faster. It's a practical solution for managing overwhelming amounts of complex information.
The market growth tells the same story. The global AI market in medical diagnostics is on track to jump from USD 1.94 billion in 2025 to over USD 10.28 billion by 2034. That surge is being fueled by advanced algorithms that are proven to improve clinical outcomes.
Expanding the Scope of AI in Healthcare
The impact of AI is reaching far beyond the hospital's diagnostic labs. As we get more comfortable with these AI tools for business, we're seeing them pop up in other areas of care, like the exciting developments in AI-driven diagnostics in the future of physical therapy, where intelligent systems are starting to personalize rehabilitation programs.
Ultimately, the goal is to build a more efficient, patient-focused healthcare system. By handing off routine analytical tasks to AI, medical professionals get more time to focus on what they do best: patient interaction and complex clinical reasoning. This shift doesn't just improve diagnostic accuracy; it enhances the entire patient experience.
AI's true power in diagnostics lies in its ability to augment human expertise, not replace it. By acting as a tireless analytical partner, it enhances a clinician's ability to see more, understand deeper, and act faster.
This guide will give you a clear understanding of the technologies at play and a strategic path for bringing them into your organization. To see how these tools are already being applied across the sector, you can explore our overview of AI applications in the healthcare industry.
How AI Technologies Decode Medical Data
To really get what’s happening with AI in medical diagnosis, you have to look past the hype and see the actual tools doing the work. These aren't far-off concepts; they're practical technologies that handle medical information in very specific, very powerful ways.
It helps to think of them as a team of digital specialists, each with a unique skill set contributing to the final diagnosis.
This collaboration between different AI capabilities is what transforms raw, messy data into insights that can save lives. Our work is grounded in using these technologies to build diagnostic tools that healthcare providers can actually trust and rely on.
Machine Learning: The Pattern Recognizer
At the core of almost all diagnostic AI is Machine Learning (ML). Picture a medical resident who has reviewed millions of patient cases, not just the thousands they might see in a career. That’s what ML algorithms do. They are trained on huge datasets—medical records, lab results, clinical outcomes—to learn the incredibly subtle patterns tied to different diseases.
Instead of a developer writing hard-coded rules, the ML model figures out the patterns on its own. It uncovers complex connections between symptoms and diseases that even an experienced clinician might miss, making it a powerful ally for predicting patient risk or catching the earliest signs of trouble in structured data.
Computer Vision: The Digital Eye
While machine learning is a wizard with numbers and tables, Computer Vision gives AI the power to "see." It acts like a digital microscope on steroids, allowing computers to analyze medical images with a level of precision that’s hard to fathom. It learns by studying millions of images—X-rays, CT scans, MRIs, and pathology slides—until it knows what a healthy organ looks like versus one with an anomaly.
For a radiologist, this is like having a second set of tireless eyes. The AI can:
- Flag Suspicious Areas: Automatically highlight potential tumors or fractures on a scan, ensuring they don't get missed.
- Quantify Findings: Measure the size and density of a nodule with perfect consistency, every single time.
- Detect Microscopic Details: Spot cancerous cells on a pathology slide that are nearly invisible to the human eye.
This is a game-changer for speeding up and improving the accuracy of any diagnosis that hinges on visual information.
Computer Vision doesn’t just see images; it interprets them. By learning from millions of examples, it can identify subtle visual cues that signal disease, often before they become obvious to human observers.
Natural Language Processing: The Data Interpreter
So much of a patient's story is buried in unstructured text—doctors' notes, discharge summaries, and clinical trial reports. This is where Natural Language Processing (NLP) steps in. Think of NLP as a tireless researcher who can read and understand human language at an impossible scale.
In a matter of seconds, an NLP model can sift through millions of clinical documents to connect a patient's reported symptoms to potential diagnoses or find ideal candidates for a new clinical trial. This ability to convert unstructured text into organized, useful data is foundational for modern medical AI. By automating this traditionally manual task, tools like our AI-powered data extraction engine unlock critical insights that were previously hidden in plain sight.
By weaving these three technologies together, we get a system that can see, read, and reason with medical data. It’s this powerful combination that allows AI to effectively support clinicians, speed up the diagnostic process, and ultimately drive better patient outcomes.
How AI Is Really Being Used in Patient Care Today
The true power of AI in medical diagnosis isn't just a concept in a research paper; it's happening right now in clinics and hospitals. It's not about replacing doctors. Instead, think of it as a powerful new tool in their toolkit, helping them see more, work faster, and ultimately improve patient outcomes.
These AI systems are designed to handle the heavy lifting of data analysis and pattern recognition. This frees up clinicians to focus on the uniquely human side of medicine: navigating complex decisions, communicating with patients, and applying their years of experience. Let's look at where this is making a real difference.
A Second Pair of Eyes for Medical Imaging
Radiology is probably the most talked-about area for AI, and for good reason. Radiologists are tasked with finding tiny, often subtle, abnormalities in a sea of visual data. It's a high-stakes, high-volume job. AI-powered computer vision acts like a tireless assistant, meticulously scanning every pixel to flag areas that need a closer look.
Here are a few concrete examples:
- Catching Cancer Sooner: In lung cancer screenings, AI algorithms can pinpoint suspicious nodules on CT scans that might otherwise be missed, leading to earlier diagnosis and treatment.
- Speeding Up Stroke Response: When a stroke is suspected, time is everything. AI can analyze brain scans in seconds to spot signs of a blockage or bleed, helping neurologists make life-saving decisions much faster.
- Improving Mammogram Accuracy: AI models, trained on millions of mammograms, are becoming incredibly skilled at identifying concerning areas, helping to catch breast cancer at its earliest, most treatable stages.
This isn't just about small improvements. The impact is significant, enhancing both the speed and accuracy of how we interpret medical images. The evidence is mounting that AI models have demonstrated the ability to detect diseases far earlier than was previously possible.
AI in radiology is about augmenting human perception. It gives clinicians a way to see more clearly and consistently within complex medical images, turning a flood of visual data into clear, actionable insights.
Finding Clues in Pathology and Cardiology
The impact of AI extends well beyond just radiology. Take pathology, for example. Grading tumors from tissue samples is a critical step in determining a patient's prognosis, but it can be subjective. AI brings a new level of objectivity by analyzing cellular structures on digital slides, helping pathologists grade tumors with a consistency that's hard to achieve manually. The result is more reliable prognoses and more personalized treatment plans.
Cardiology is another field seeing major gains. AI algorithms can analyze ECG readings to predict serious cardiac events like atrial fibrillation or even sudden cardiac arrest, sometimes days before they happen. This predictive capability shifts the entire paradigm from reacting to a crisis to proactively preventing one.
Here's a quick look at how these applications stack up across different specialties.
AI Diagnostic Applications Across Medical Specialties
AI is not a one-size-fits-all solution. Its application is tailored to solve specific, high-value problems within each medical field, using the technology best suited for the task.
| Medical Specialty | Primary Application | Problem Solved | Key AI Technology |
|---|---|---|---|
| Radiology | Nodule & lesion detection | Reduces missed findings and diagnostic time | Computer Vision |
| Pathology | Cancer cell grading & quantification | Improves consistency and objectivity of tumor grading | Computer Vision, Pattern Recognition |
| Cardiology | Arrhythmia detection & risk prediction | Enables early warning for life-threatening events | Machine Learning (on ECG/EHR data) |
| Dermatology | Malignant lesion identification | Assists in early screening for skin cancers | Computer Vision |
| Oncology | Treatment response prediction | Helps tailor therapies to individual patients | Machine Learning (on genomic & clinical data) |
| Neurology | Early Alzheimer's & stroke detection | Identifies subtle biomarkers in brain scans | Computer Vision, NLP (on patient notes) |
As you can see, the common thread is using AI to process vast amounts of data—whether images, signals, or records—to find patterns that inform clinical decisions and lead to better patient care.
Making the Entire Clinic Run Smarter
Beyond diagnosing disease, AI is also smoothing out the day-to-day operations of healthcare. For instance, voice recognition technology is making a huge difference in reducing the administrative burden on doctors. Resources on AI voice recognition in healthcare show how these tools can listen to a patient visit and automatically generate structured clinical notes.
This is a game-changer, freeing up hours that were once spent on paperwork.
Similar AI tools are being used to manage patient records, predict ER wait times, and optimize surgical schedules. These applications might not sound as dramatic as finding a tumor, but they are essential for building a more efficient and responsive health system. By automating the routine, we give clinicians back their most precious asset: more time to focus on their patients.
Your Roadmap for Integrating AI Diagnostics
Bringing AI into your diagnostic workflow isn't like buying a new piece of lab equipment. It’s a major strategic shift that demands a clear, well-thought-out plan. And that plan doesn't start with algorithms or software—it starts with data.
Before you do anything else, you have to get your data house in order. High-quality, diverse, and properly anonymized datasets are the fuel for any successful AI initiative. Without a clean, robust data pipeline, even the most sophisticated AI will produce unreliable, or even dangerous, results. It’s the non-negotiable first step.
The goal here is to build a brand-new capability, one that marries the deep expertise of your clinicians with the analytical power of modern AI. To get there, you need a structured approach, beginning with a sharp focus on the specific clinical problems you want to solve. This keeps your efforts grounded in creating real, measurable value right from the start.
Navigating the Regulatory and Ethical Maze
Once you have a handle on your data, you’ll run straight into the next major hurdle: the tangled web of regulations and ethics. In healthcare, this isn't just red tape; it's a critical part of building trust with both your clinicians and your patients.
You absolutely have to get these things right:
- Regulatory Approvals: You’ll be dealing with bodies like the FDA, which has already given the green light to over 400 AI-based medical devices and algorithms. You must understand the specific clinical validation and clearance pathways for the type of AI tool you’re considering.
- Data Privacy and Security: HIPAA compliance is the bare minimum. You need ironclad protocols for anonymizing patient data and keeping it secure at every stage, from training the AI model to its daily use in the clinic.
- Ethical Oversight: Algorithmic bias is a massive ethical landmine. If your AI is trained on data that doesn't reflect your actual patient population, it can easily perpetuate—or worsen—existing health disparities. An ethical review process isn't optional; it's essential for ensuring fairness.
The market is exploding, which adds a sense of urgency. With massive growth projected, North America is currently leading the pack, thanks to strong R&D funding and mature regulatory frameworks. You can get a deeper sense of these market dynamics from this comprehensive AI diagnostics market report.
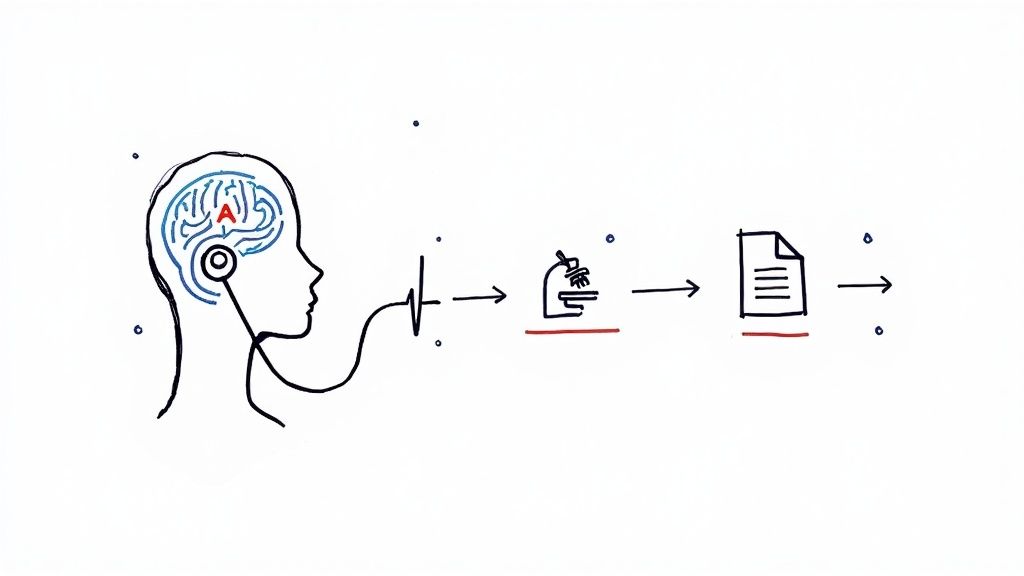
This diagram breaks down the typical flow of an AI-assisted diagnosis, from the moment data is fed into the system to the final clinical review.
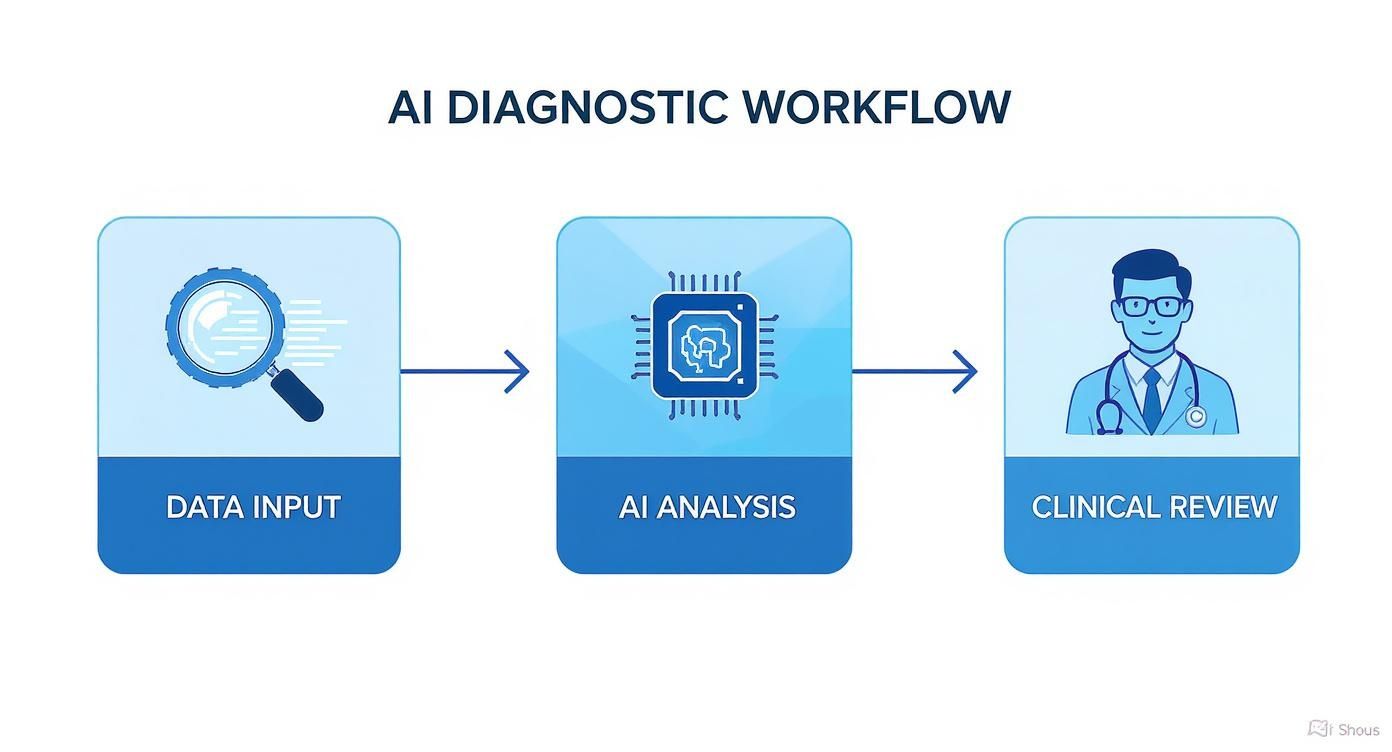
What's really important to notice is the "human-in-the-loop" design. The AI isn't making the final call; it's a powerful assistant that provides insights to the clinician, who remains in control of the diagnosis.
Building a Bulletproof Business Case
To get any project off the ground, you need buy-in from both clinical staff and the C-suite. That means building a business case that clearly spells out the return on investment (ROI).
Your pitch has to go beyond the cool tech. It needs to connect directly to your organization's core goals. For clinicians, frame it around better patient outcomes. For administrators, focus on operational efficiency and cost savings.
A compelling business case for diagnostic AI focuses on tangible outcomes. It's not about the technology itself, but about what it enables: faster diagnoses, reduced clinician burnout, lower error rates, and a higher standard of patient care.
Pulling this together often requires a seasoned guide. Expert implementation support can help you pinpoint the highest-impact use cases and actually quantify their potential value, giving you the hard data needed to secure a budget for your pilot project.
Choosing the Right Partner and Technology
With a solid plan and executive backing, you’re ready to pick your tools and—just as critically—your partner. The market is flooded with AI solutions, but the right one for you is the one that slides into your existing clinical workflows without causing chaos. If a tool disrupts how your clinicians work, they won't use it. It's that simple.
This is where a service-oriented approach can be a game-changer. Look for a partner who will manage the entire rollout smoothly, from initial setup to the ongoing support and maintenance that will inevitably be required.
A good partner provides more than just software; they guide you through the thorny integration challenges. Following a structured roadmap is the key to ensuring your final solution is effective, compliant, and actually embraced by your clinical team. By taking these deliberate steps, you can confidently introduce the power of AI into your organization and truly begin to elevate the quality of patient care.
Measuring the Impact of Your AI Initiatives
Getting your first AI diagnostic tool up and running is a huge step, but it’s just the starting line. The real work begins now: figuring out if these systems are actually making a difference in your clinical practice. You have to look past the technical specs and accuracy claims. The crucial part is defining and tracking key performance indicators (KPIs) that show real-world use cases improvements for your operations and, most importantly, for your patients.
This isn't just about proving the tech works. It's about building a solid, data-driven argument for expanding its use and demonstrating that your investment is paying off where it matters most.
Defining Your Core Metrics for Success
To get a true picture of AI's impact, you need to look at it from a few different angles. Your metrics should cover clinical effectiveness, operational efficiency, and the experience of both patients and staff. If you only focus on how accurate the algorithm is, you're missing the whole story of how this technology affects your entire healthcare ecosystem.
Before you flip the switch, you need to establish a baseline. This gives you a clear "before and after" snapshot, which is exactly the kind of hard data you’ll need to justify more investment and get your clinical teams excited.
Here are a few things you should be tracking:
- Diagnostic Turnaround Time: How long does it take from the moment an image is captured to the final report being signed? Shaving time off this process can dramatically reduce patient anxiety and get treatment plans in motion faster.
- Clinician Workload and Burnout: You can use simple surveys or workload analysis to see if the AI is genuinely lightening the cognitive load on your radiologists and pathologists. A noticeable drop in burnout is a massive win.
- Report Consistency: Take a look at the variability in diagnostic reports across different clinicians. One of the quiet benefits of a good AI tool is that it helps standardize findings, leading to more consistent reports across the board.
True ROI in diagnostic AI isn't a single number. It’s a mix of clinical, operational, and financial wins. You see it not just in faster reports, but in fewer unnecessary procedures, better long-term patient outcomes, and a more sustainable workload for your expert staff.
From Pilot Project to Scaled Solution
Think of your first AI deployment as a focused experiment. It’s a pilot program, run in a controlled setting, designed to prove the concept, smooth out any workflow hitches, and collect the data you need to build a business case for a wider rollout. Start small. Pick a single sub-specialty in radiology or pathology where you can keep a close eye on the results.
Once that pilot starts showing clear, positive results, you can map out a phased plan to scale up. This approach keeps risks low and lets you apply the lessons you learned from the initial deployment. This is where your business case, now packed with real data from the pilot, becomes absolutely essential for getting the budget and buy-in you need to expand. As we’ve covered in our AI adoption guide, doing a thorough AI requirements analysis right from the start sets you up for this kind of measurable success.
The Human Side of Scaling AI
The tech is only half the equation. As you start to scale, managing the human side of the change is absolutely critical. Your clinicians need to trust the AI's outputs, and that trust is built on a foundation of transparency, solid training, and ongoing validation.
Your scaling plan has to include:
- Comprehensive Staff Training: Don't just show them how to use the software. You need to educate your staff on the basics of how the AI model works, what its limitations are, and how to correctly interpret its suggestions.
- Clear Governance and Oversight: You need a clear protocol for what happens when the AI and the clinician disagree. The "human-in-the-loop" model isn't just a suggestion; it should be a hard rule, with the clinician always having the final say.
- Continuous Model Monitoring: AI models aren't "set it and forget it" tools. Their performance has to be constantly checked against new, real-world clinical data to make sure they stay accurate and unbiased over time.
Following this disciplined path ensures that as you expand your use of medical diagnosis artificial intelligence, you're not just adding new gadgets—you're fundamentally raising the standard of care. It's a journey that demands both technical know-how and strategic foresight, qualities that our expert team helps organizations navigate every day.
Let's Build Your AI Healthcare Strategy Together
Getting medical diagnosis artificial intelligence right is about more than just buying software; it’s about finding the right partner. As we've explored, AI can be an incredible asset, amplifying the skills of your clinical team and fundamentally improving patient care. But the road from a good idea to a fully validated and integrated clinical tool is complex. It demands a mix of deep industry experience, sharp technical skill, and a focused strategy.
Trying to go it alone is a tough ask. That’s where we come in. We act as that crucial partner, offering everything you need to make sure your AI projects deliver real-world value. Our work spans from high-level AI strategy consulting all the way to building custom internal tooling that fits perfectly into your existing clinical workflows. We get the nuances of healthcare and build solutions that clinicians actually want to use.
The most successful AI integrations are not just technology projects; they are strategic collaborations. A strong partnership ensures that the final solution is clinically relevant, operationally sound, and built for measurable, long-term impact.
The future of healthcare is taking shape right now, one intelligent solution at a time. We'd love to hear about the specific challenges your organization is facing. Connect with our expert team and let's talk about how we can build the next generation of AI-powered healthcare together, driving better outcomes for both your patients and your practice.
FAQ: Common Questions About AI in Medical Diagnosis
We hear a lot of the same questions from healthcare leaders exploring AI. Let's tackle the big ones.
Will AI Replace Doctors and Radiologists?
Not a chance. The consensus across the industry is that AI is here to augment human expertise, not replace it.
Think of it like having an incredibly sharp co-pilot. The AI can sift through massive amounts of data—far more than a human could in the same timeframe—and flag potential issues or patterns. This frees up clinicians to focus on what they do best: handling complex cases, building treatment plans, and connecting with patients.
It's a "human-in-the-loop" model. The AI makes recommendations, but the final, critical judgment call always belongs to the doctor.
What Are the Biggest Hurdles to Getting Started?
From what we've seen, three challenges pop up again and again: data quality, regulatory navigation, and workflow integration.
AI models are hungry for data, but they need it to be high-quality and diverse. Hospitals often have this data, but it's stuck in different systems and formats. Then there's the regulatory side; getting a tool cleared by bodies like the FDA is a serious, meticulous process.
Finally, you have to get the tool to actually work within your hospital's existing IT infrastructure. Dropping a new piece of software into a busy clinical workflow without causing major disruptions takes real expertise in areas like custom healthcare software development.
How Do You Keep AI Fair and Ethical?
This is probably the most important question of all, and it requires constant vigilance. It all starts with the data used to train the model. If you only train an AI on data from one demographic, it won't work well for others. You have to intentionally build datasets that reflect the true diversity of your patient population.
Once a model is built, it needs to be relentlessly tested for performance gaps across different groups of people. Ethically, the key is transparency. A doctor can't trust a "black box" recommendation. This is where explainable AI (XAI) comes in—building models that can show their work and explain why they reached a certain conclusion.
What's the First Step My Hospital Should Take?
Start with a problem, not a product. Don't go shopping for AI; instead, identify a specific, high-impact challenge you're facing. Maybe it's a long backlog for mammogram readings or a need to speed up sepsis detection.
Once you have a target, the next step is a thorough AI requirements analysis to see if your data is ready and to build a solid business case. Bringing in a partner for AI strategy consulting can help you create a practical roadmap for a small pilot project. The goal is to get a quick win that proves the value and builds momentum for a larger rollout.
Adopting medical diagnosis AI is a strategic journey, not a simple purchase. Starting with a clear problem and a solid plan ensures that your investment improves patient care and operational efficiency.
By asking these questions upfront, healthcare leaders can move forward with a clear-eyed strategy. The aim isn't just to adopt new technology, but to build a smarter system where human expertise and intelligent tools work hand-in-hand to save lives. Connect with our expert team to learn more.
Ready to transform your healthcare strategy with AI? At Ekipa AI, we help you move from idea to impact. Get your Custom AI Strategy report in 24 hours and start building the future of diagnostics today.