Artificial Intelligence AI in Healthcare: Transforming Patient Care
Discover how artificial intelligence AI in healthcare is revolutionizing patient care, diagnostics, and treatment. Learn more about its transformative impact.
Picture an incredibly sharp assistant for every single clinician, capable of sifting through millions of data points in a heartbeat to flag potential risks or suggest the best care pathways. That’s no longer a futuristic fantasy; it’s the practical reality of artificial intelligence (AI) in healthcare today. It's moving from abstract concept to a real tool that enhances, rather than replaces, human expertise.
How AI Is Redefining Healthcare
Artificial intelligence in healthcare isn't some far-off sci-fi idea anymore. It's a suite of practical tools already being put to work in the NHS and private clinics all over the UK.
Don't think of it as a robot doctor. A better way to see it is as an incredibly powerful collaborator. Its main job is to analyse huge volumes of complex medical data—from patient records and imaging scans to genetic information—far faster and often with a different kind of precision than a human can manage alone.
This ability is unlocking major improvements in both patient outcomes and the day-to-day running of healthcare facilities. For clinicians, it means having data-driven support to make more confident decisions. It frees them from tedious data analysis, letting them focus on what truly matters: caring for their patients. For administrators, AI offers a way to get the most out of limited resources, smooth out processes, and bring down costs.
The Growing Importance in the UK Market
The move towards AI in UK healthcare is more than just a passing trend—it's a massive shift, both clinically and economically. The UK's AI in healthcare market was valued at around USD 1.33 billion in 2023 and is projected to hit nearly USD 12.5 billion by 2030.
This explosive growth is being fuelled by the widespread adoption of AI software, which accounted for over half of the market's revenue in 2023. Significant government investment in digital health is also playing a huge role.
A great, practical example of this is the rise of advanced medical speech recognition. These tools are helping to automate clinical documentation, a change that dramatically cuts down the admin burden on medical staff. It’s a perfect illustration of how focused AI applications are solving genuine, everyday problems in the field.
Core Areas of AI Application
To really grasp how AI is making a difference, it helps to see where it's being applied. The following table breaks down some of the most impactful areas.
Key Areas of AI Impact in Healthcare
Domain Primary AI Function Example Application
Diagnostics
Image & Pattern Recognition
Analysing X-rays or MRI scans to detect subtle signs of disease like cancer or diabetic retinopathy, often earlier than the human eye.
Personalised Medicine
Predictive Analytics
Tailoring treatment plans (e.g., for cancer) based on a patient's unique genetic profile and lifestyle data.
Operational Workflow
Automation & Optimisation
Automating appointment scheduling, managing hospital bed allocation, and predicting patient flow to reduce waiting times.
Drug Discovery
Data Analysis & Simulation
Speeding up the development of new medicines by analysing vast biological datasets to identify promising compounds.
Understanding these key areas is the first step for any leader looking to build a successful adoption plan. But going from a broad concept to a practical application requires a clear, well-thought-out strategy. This is where getting expert guidance on your AI approach can make all the difference, ensuring you focus on areas that will deliver real, meaningful results.
How AI is Changing Clinical Practice
Talk of artificial intelligence in healthcare can often feel a bit abstract. But for clinicians on the ground here in the UK, AI is quickly becoming a concrete and powerful tool. It’s not about replacing human judgement; it’s about augmenting it with insights drawn from vast amounts of data, helping doctors and nurses diagnose faster, predict risks earlier, and design more effective treatments.
This isn’t some far-off future, either. The shift is already well underway. Back in 2021, around 25% of UK clinicians reported they were already using AI tools in their daily work. Look at the Calderdale and Huddersfield NHS Foundation Trust, for example. Since 2021, they’ve been using predictive analytics to forecast adult ICU occupancy with up to 90% confidence. This is where the real value starts to emerge—when theory becomes practice.
A Second Pair of Eyes for Medical Imaging and Diagnostics
One of the most mature and impactful uses of AI is in medical imaging. Radiologists and pathologists spend their careers training their eyes to spot the tiniest, almost invisible, abnormalities in scans like X-rays, MRIs, and CTs. AI algorithms, especially those built on deep learning, can be trained on millions of these images to do the same thing, but with incredible speed and consistency.
Think of it as giving the clinician a second set of highly trained eyes that never get tired. An AI can flag a suspicious area on a mammogram that points to early-stage breast cancer or identify subtle signs of diabetic retinopathy from an eye scan. This allows for much earlier intervention. The radiologist isn't sidelined; they’re empowered.
By automatically prioritising scans that show potential issues, AI helps clinicians focus their limited time and expertise where it's needed most. This can reduce backlogs and, just as importantly, shorten that anxious wait for a patient's results.
This partnership between human expertise and machine precision is exactly what modern healthcare technology is all about: building tools that support, not supplant, the people on the front line.
Moving from Reactive to Proactive Care with Predictive Analytics
Another game-changing area for AI is using predictive analytics to get ahead of problems. Hospitals are swimming in data—vital signs, lab results, patient histories, you name it. It's far too much for any human to process in real-time. AI models, however, can sift through this data constantly, looking for patterns that signal a patient is at high risk of developing a critical condition, often long before obvious symptoms appear.
A perfect example is the fight against sepsis, a life-threatening condition where every hour counts. By monitoring subtle changes in a patient's data stream, an AI system can alert a nurse or doctor to a high sepsis risk, giving them a head start of several hours. This kind of early warning system can have a dramatic impact on patient outcomes and mortality rates.
These predictive tools are being rolled out in all sorts of scenarios:
- Forecasting Patient Admissions: Helping hospitals manage bed capacity and staffing rotas more efficiently.
- Identifying Readmission Risks: Flagging patients who are likely to return shortly after discharge so extra support can be put in place.
- Predicting Disease Outbreaks: Analysing public health data to anticipate things like seasonal flu spikes.
Speeding Up Drug Discovery and Delivering Personalised Medicine
Getting a new drug to market is an incredibly long and eye-wateringly expensive process. It can take over a decade and cost billions. AI is stepping in to radically shorten this timeline. By crunching complex biological data, algorithms can identify promising drug candidates and predict their likely effectiveness and side effects, all before they even hit a lab bench.
But AI isn't just about creating new drugs; it's about making medicine more personal. We're moving into an era of precision medicine, where treatment is tailored to an individual’s unique genetic makeup, lifestyle, and environment. AI systems can analyse a patient’s genomic data alongside their clinical history to recommend the most effective cancer therapy or calculate the perfect dose of a specific medication.
This data-first approach helps ensure patients get the treatment most likely to work for them from the outset, cutting down on trial-and-error and improving their chances of a better outcome. To see how these tools are being applied today, take a look at these real-world use cases.
Streamlining Operations with AI Automation
While clinical breakthroughs tend to capture the public's imagination, some of the most profound impacts of artificial intelligence in healthcare are happening behind the scenes. Look beyond the diagnosis, and you'll find AI quietly untangling the immense operational complexities of modern hospitals and clinics. It’s tackling the unseen administrative burdens that eat up time and resources—precious assets that should be dedicated to patient care.
At its core, this is about reducing the daily friction that slows everything down. Think of all the administrative work that bogs down highly-trained staff: medical coding, billing, scheduling, and inventory management. These jobs are essential, of course, but they're also repetitive and data-intensive. This makes them perfectly suited for automation. A smart approach to workflow automation can break these administrative logjams, freeing up professionals to work at the top of their game.
The image below gives a sense of how an AI-powered workflow can be mapped out to automate these kinds of complex, multi-step processes.
It’s a clear visualisation of the journey from manual, error-prone tasks to an intelligent, automated system that runs with far greater efficiency and consistency.
Optimising Hospital Management with Intelligent Systems
Good hospital management is all about foresight and smart resource allocation. This is precisely where AI comes in, turning historical and real-time data into genuinely useful predictive insights. For example, intelligent systems can analyse admission patterns, public health trends, and even seasonal spikes in illness to forecast patient flow with surprising accuracy. This allows administrators to get ahead of the curve, managing bed availability, optimising staff rotas, and preventing A&E departments from becoming overwhelmed.
It's a similar story in supply chain management. Instead of relying on manual stock takes, AI algorithms can predict the demand for everything from surgical gloves to crucial medicines. This automates the reordering process, helping to prevent both costly stockouts and wasteful over-ordering. The end goal is a seamless operational flow where the right resources are always in the right place at the right time.
Automating the Administrative Burden
The administrative weight on healthcare is staggering. It's not uncommon for a clinician's day to be dominated by documentation rather than actual patient interaction. Here, automation offers immediate and very tangible relief.
- Medical Coding and Billing: AI algorithms can scan clinical notes and patient records to automatically suggest the correct billing codes. This doesn't just speed up the revenue cycle; it also helps cut down the nearly 80% error rate that can come with manual coding, leading to better accuracy and compliance.
- Clinical Documentation: Tools like advanced AI-driven medical transcription are changing the game. They can convert a doctor's spoken notes directly into structured text in the electronic health record. This slashes documentation time, freeing up clinicians to focus on their patients.
These tools aren't just time-savers. They reduce the cognitive load on healthcare professionals, which is a major factor in burnout, and let them redirect their expertise back to where it matters most. A tool like a clinic AI assistant can take on appointment scheduling and routine patient communications, offloading yet more of those day-to-day administrative tasks.
By handing over these high-volume, rules-based jobs to AI, healthcare organisations can realise significant cost savings, improve the quality of their data, and, most importantly, give their clinical teams back the one thing they can never make more of: time.
Navigating the Hurdles of AI Implementation
Bringing artificial intelligence into healthcare isn't like installing a new piece of software. It’s a fundamental shift in how we work, especially in a field as sensitive and tightly regulated as medicine. And while the upsides are enormous, the path to getting it right is strewn with challenges that need a solid, well-thought-out strategy.

It’s better to think of these hurdles not as roadblocks, but as critical checkpoints. Getting past each one properly is the only way to build an AI programme that’s both effective and sustainable. A proactive plan is simply non-negotiable for anyone serious about navigating these complexities from day one.
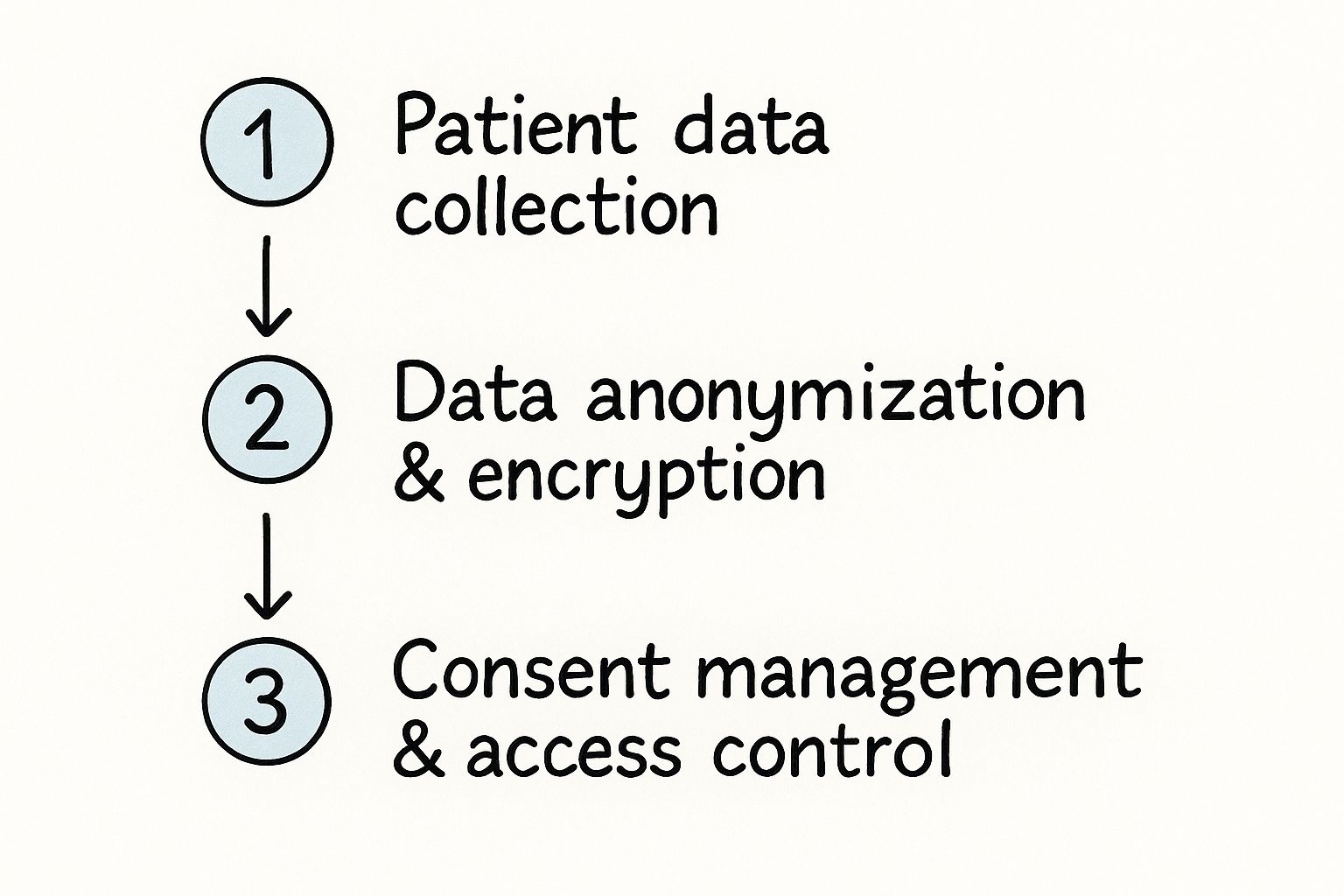
Data Privacy and Regulatory Compliance
At the heart of any healthcare AI is data—and lots of it. We're talking about vast quantities of highly sensitive patient information. Protecting that data isn't just a good idea; it's the most important ethical and legal duty you have. In the UK, that means grappling with the dual demands of GDPR and the NHS’s own stringent standards for how patient data is handled.
Staying compliant is a serious undertaking. It calls for robust data governance, top-tier cybersecurity, and transparent processes that keep patients firmly in control of their own information. Get this wrong, and you're not just facing hefty fines. You risk shattering the trust your patients have in you, which can be impossible to get back.
It’s this complex regulatory maze that leads so many healthcare organisations to seek out expert support. Having tailored implementation support can provide a clear roadmap for building systems that are not only powerful but also tick every single compliance box. Find out more at: https://www.ekipa.ai/implementation-support
Technical Hurdles and System Integration
Let's be realistic: many healthcare providers, including a significant number of NHS Trusts, are running on older, legacy IT systems. These systems have been workhorses for years, but they were never built to talk to modern AI platforms. Trying to integrate new AI tools into this old infrastructure is often the biggest technical headache of all.
This integration gap throws up a few common problems:
- Data Silos: Patient records get stuck in different, disconnected systems. This makes it a nightmare to pull together the unified, clean datasets that AI models need to learn from.
- Interoperability Issues: Getting new and old systems to communicate effectively can feel like trying to mix oil and water, often demanding expensive, custom-built solutions.
- Scalability Concerns: Legacy setups can buckle under the strain of processing the sheer volume of data that advanced AI applications require.
Clearing these technical barriers isn't just about buying new tech. It requires a meticulous approach to integration, testing, and deployment to make sure new tools actually help, rather than hinder, daily operations.
Ethical Considerations and Algorithmic Bias
An AI model is only ever as good, or as fair, as the data it’s trained on. If the historical data fed into an algorithm contains existing societal biases—whether related to ethnicity, gender, or postcode—the AI will learn and amplify them. This is a serious problem, as it can lead to the AI producing less accurate diagnoses or treatment plans for certain groups of people.
Mitigating algorithmic bias isn't a technical problem to be solved; it's an ethical imperative. It demands a conscious, ongoing effort to build diverse datasets, constantly check algorithms for fairness, and always, always keep a human in the loop for critical clinical decisions.
This commitment to fairness is vital for building trust. With more than half of NHS Trusts now bringing AI into their workflows, the focus on ethical use and maintaining public confidence has never been more critical for long-term success.
The Human Element: Fostering Trust and Buy-In
Finally, we arrive at what might be the biggest challenge of all: people. Clinicians are, quite rightly, cautious about any new technology that affects patient care. For AI to really take hold, it has to be seen as a trusted co-pilot, not a replacement for their hard-won expertise.
Building that trust comes down to transparency, education, and genuine collaboration. Doctors and nurses need to understand how an AI tool arrives at its conclusions. They need to be involved in its development and validation, and they need to see concrete proof that it helps them do their jobs better.
Without buy-in from the people on the front lines, even the most brilliant AI initiative will never move beyond a pilot project and become a true standard of care.
Building Your Healthcare AI Strategy
Embarking on an artificial intelligence initiative in healthcare starts with a clear plan, not a shiny new piece of technology. So many organisations fall into the trap of buying exciting new AI tools for business before they’ve even figured out what problem they’re trying to solve. This is a recipe for expensive pilot projects that fizzle out, delivering no real value.
The secret is to flip the script. Instead of asking, "What can we do with AI?", leaders need to ask, "What are our biggest clinical or operational headaches, and could AI be the answer?". This simple shift in thinking is what separates a flashy experiment from a genuine improvement in patient care.
Identifying High-Impact Use Cases
Your first move is to pinpoint the most promising opportunities. This isn’t a job for the IT department alone; it needs clinical staff, IT experts, and administrative leaders all in the same room. The goal is to find the areas where AI can make the biggest difference, whether that's boosting diagnostic accuracy, slashing administrative waste, or simply making the patient journey smoother.
It's about taking a hard look at your current processes to find the real bottlenecks.
- Clinical Opportunities: Could an AI model help your radiologists spot the most urgent scans in a massive queue? Can predictive analytics flag patients who are at a high risk of being readmitted? These are concrete problems with measurable results.
- Operational Opportunities: Think about where your team's time is being drained by repetitive, soul-destroying tasks. Medical billing and appointment scheduling are classic examples, perfectly suited for workflow automation. In other cases, building custom internal tooling can solve those unique logistical puzzles that off-the-shelf software just can't handle.
Working with an experienced partner through an AI co creation process can seriously speed this up, helping you uncover the real-world use cases that will deliver the most value for your organisation.
Assembling the Right Team and Securing Sponsorship
An AI project is far more than just an IT initiative. It’s a major organisational shift, and it needs backing from the top. Getting strong executive sponsorship from day one is non-negotiable. You need a senior leader who can act as a champion—someone to clear roadblocks, secure the budget, and keep everyone focused on the bigger picture.
Just as critical is putting together a cross-functional team. This can't just be data scientists and engineers. You need clinicians who live and breathe the daily workflow, administrators who hold the purse strings, and compliance officers who can navigate the maze of regulations. This mix of expertise ensures that what you build is not only technically clever but also clinically useful and operationally sound.
A classic mistake is to build an AI solution in a silo. If you don't get constant feedback from the frontline staff who will actually use the tool, you risk creating something that is brilliant on paper but completely impractical in a busy clinic.
A Phased Approach from Pilot to Scale
Trying to roll out a massive, organisation-wide AI system in one go is almost guaranteed to fail. A much smarter strategy is to start small, prove the value, and build momentum. Kick things off with a tightly-defined pilot project that has one clear, measurable goal.
This initial pilot does a few crucial things: it shows what the technology can do, helps you spot unexpected challenges early on, and builds trust among stakeholders. A successful pilot usually follows a clear AI Product Development Workflow, moving step-by-step from an idea to a working solution. Once that pilot has proven its worth, then you can start thinking about scaling up.
The following roadmap breaks down this journey into manageable stages.
AI Implementation Roadmap: A Phased Approach
Phase Key Activities Primary Goal
1. Discovery & Strategy
Identify pain points, define business case, secure executive sponsorship, assemble a cross-functional team.
Align AI initiatives with strategic organisational goals and identify high-impact pilot projects.
2. Pilot & Validation
Develop a minimum viable product (MVP), collect initial data, test in a controlled environment, gather user feedback.
Prove the concept's value on a small scale and demonstrate tangible ROI to build support.
3. Refinement & Integration
Enhance the model based on feedback, ensure data security, integrate with existing systems (EHR, etc.), train end-users.
Prepare the solution for a broader rollout by ensuring it's robust, secure, and user-friendly.
4. Scale & Optimisation
Deploy the solution across targeted departments, monitor performance against KPIs, continuously improve the model.
Achieve widespread adoption and maximise the operational and clinical benefits across the organisation.
Before you even think about scaling, you absolutely must define your Key Performance Indicators (KPIs). How will you know if you've succeeded? It could be anything from shorter patient waiting times and better diagnostic accuracy to a specific financial return on your investment. Having clear KPIs ensures every AI project stays grounded in reality, turning exciting potential into results you can actually measure.
Your Partner in Healthcare Innovation
We’ve journeyed through the incredible ways artificial intelligence is already reshaping healthcare, from spotting diseases earlier to making hospitals run more smoothly. But knowing what AI can do is one thing; making it happen is another entirely. Getting this right isn't just a technical challenge—it’s a strategic one that needs a clear vision and the right people on your side.
The path forward starts with a solid plan, one that's built with your specific goals in mind. This is where AI co creation comes into play, ensuring that every step you take is designed to deliver real, measurable results. You might begin with AI strategy consulting to map out the possibilities or dive straight into a Custom AI Strategy report to create a detailed blueprint.
Once that roadmap is in place, you can bring it to life by automating critical processes through services like AI Automation as a Service. The key is finding a partner who gets the nuances of healthcare. It's about building solutions that don't just work on a spreadsheet but earn the trust of the clinicians and patients who depend on them every day.
If you’re ready to explore how this can work for your organisation, the next step is to talk to the people who can guide you. We invite you to meet our expert team and see how we can help.
Answering Your Questions About AI in Healthcare
It's natural to have questions when exploring something as significant as artificial intelligence in medicine. Let's tackle some of the most common ones I hear from healthcare leaders.
Will AI Replace Doctors and Nurses?
This is probably the number one concern, and the answer is a clear no. The real aim is to augment, not replace, our brilliant clinicians.
Think of AI as the most capable assistant you've ever had. It's fantastic at sifting through mountains of data, analysing scans, or handling the drudgery of scheduling. This frees up doctors and nurses to spend more time on the things that truly require a human touch: navigating complex diagnoses, talking with patients, and delivering empathetic care.
What’s the Biggest Barrier to AI in UK Healthcare?
From what I've seen, one of the toughest nuts to crack is getting modern AI tools to play nicely with older hospital IT systems. Many healthcare organisations are running on legacy infrastructure that simply wasn't built for this kind of integration, a challenge we've looked at in our AI adoption guide.
Getting past this hurdle takes serious planning and a willingness to invest in modern healthcare software development. Alongside the tech challenge, we also have to be incredibly careful with data privacy. Complying with regulations like GDPR isn't just a tick-box exercise; it's fundamental when you're dealing with sensitive patient information.
How Can a Small Clinic Start Using AI?
You don't need a multi-million-pound budget to get started. For smaller clinics, the key is to think smart and start small. Focus on a single, specific problem that's causing you headaches right now.
A perfect example is bringing in AI-powered software for administrative tasks. Think automated appointment scheduling or intelligent patient reminders. The return on investment is almost immediate because you're freeing up valuable staff time. The best way forward is always to start with a clear, high-impact project, something we champion in our approach to AI co-creation.
How Do You Ensure AI Models Are Safe and Fair?
This is a huge responsibility and something that needs constant attention. It's not a one-and-done job. It all starts with the data we use to train the models; it must be diverse and truly representative of the patient population to avoid baking in biases from the start.
But here’s the most important part: AI in healthcare never flies solo. It always operates with a ‘human-in-the-loop’. A clinical expert is always there to review and validate the AI’s findings before any decision is made. This provides that critical final check and ensures a human is always accountable.
Building this continuous validation is a cornerstone of any responsible AI Product Development Workflow.
By talking through these common questions, I hope it’s clearer that AI, when implemented thoughtfully, can be a powerful partner in improving healthcare. The key is to build a solid plan with people who know the ropes. If you'd like to see who can help guide your own journey, I invite you to meet our expert team.
Ready to see what AI could do for your healthcare organisation? At Ekipa AI, we specialise in turning complex challenges into real-world, impactful solutions. Your journey can start today with a Custom AI Strategy report designed specifically for you.