Artificial Intelligence in Healthcare: A Complete Modern Guide
Discover how artificial intelligence in healthcare is transforming patient care, diagnostics, and treatment options. Learn more now!
Artificial intelligence in healthcare isn't some far-off dream anymore—it's here, right now, making medicine smarter, faster, and more personal. At its core, it's about using sophisticated software and algorithms to mimic human thinking when analysing complex medical data. This technology is already hard at work behind the scenes, doing everything from spotting diseases early to making hospitals run more smoothly.
How AI Is Reshaping Modern Medicine

Bringing artificial intelligence into healthcare is a huge leap from traditional methods, shifting us towards a much more efficient, data-driven system. These intelligent tools are moving out of the lab and onto the front lines of clinical practice, touching nearly every part of a patient's journey and hospital operations. This isn't just about playing with new gadgets; it's a fundamental change in how medical professionals handle diagnostics, treatment, and day-to-day efficiency.
For healthcare leaders, making this switch needs a clear, thought-out plan. The sheer amount of medical data we have—from patient records to genomic sequencing—is a massive opportunity. AI is brilliant at sifting through these enormous datasets to spot subtle patterns and connections that a person could easily miss.
The Strategic Imperative for AI Adoption
For any healthcare organisation that wants to stay competitive and give patients the best possible care, adopting AI has become a strategic must-do. The global AI in healthcare market was valued at $16.61 billion in 2024 and is expected to skyrocket, which shows just how quickly the industry is getting on board. This growth is being driven by real, tangible benefits that solve some of the sector's oldest problems.
Here are a few key areas where AI is already making a difference:
- Accelerating Medical Research: AI algorithms can tear through decades of clinical trial data and scientific papers in minutes, massively speeding up the discovery of new drugs and treatments. To get a sense of how AI can help at the very start of innovation, you can explore how to use AI for academic research.
- Enhancing Diagnostic Accuracy: Whether it's reading X-rays and scans or spotting the earliest signs of conditions like sepsis, AI tools give clinicians a second pair of expert eyes, helping to reduce the risk of human error.
- Personalising Patient Treatment: By analysing a patient's genetics, lifestyle, and medical history, AI can help build truly personalised treatment plans. It’s a move away from the old one-size-fits-all model.
Implementing AI successfully is less about the technology itself and more about the strategy behind it. It requires a deep understanding of clinical needs, data infrastructure, and workflow integration to ensure the tools genuinely support clinicians and improve patient outcomes.
Navigating this complex but rewarding journey starts with a solid foundation. This is where thoughtful AI strategy consulting becomes the critical first step for any healthcare institution. As we delve deeper into specific applications, it becomes clear that a well-crafted plan is the key to unlocking the full potential of this technology.
Understanding the Core AI Technologies in Healthcare
To really get what AI is doing in healthcare, we need to pop the bonnet and look at the engines driving the change. These aren't just vague, far-off ideas; they're specific tools already solving real clinical and operational problems. Think of them as the different specialists in a hospital, each with a unique skillset that contributes to looking after a patient.
The most fundamental of these is Machine Learning (ML). Picture a medical student who can sift through millions of patient charts in a matter of seconds. They're not just memorising the information but learning to spot the subtle patterns that come before a diagnosis. That's ML in a nutshell. It trains algorithms on huge datasets—like medical images, lab results, and patient records—to make predictions without being explicitly programmed for every single possibility. This is what allows AI to forecast disease outbreaks or flag patients at higher risk for certain conditions.
Making Sense of Unstructured Medical Data
While ML is great with neat, organised data, a huge chunk of valuable medical information is locked away in messy formats like doctors' notes, research papers, and patient emails. This is where Natural Language Processing (NLP) steps in. Simply put, NLP gives machines the power to read, understand, and interpret human language.
Think of it as a super-efficient consultant who can instantly read a decade's worth of jargon-filled clinical notes and pull together a complete patient history. NLP algorithms can extract crucial information—symptoms, diagnoses, medications—from plain text and turn it into structured data that ML models can then analyse. This is vital for everything from improving clinical documentation to creating smart symptom checkers that point patients towards the right care.
Giving AI the Power of Sight
The third key technology is Computer Vision, which lets AI systems interpret visual information. In a hospital, this technology is like a radiologist with bionic eyes, able to spot minuscule anomalies in medical scans that a human might overlook.
Computer vision algorithms are trained on thousands of labelled images (like X-rays, MRIs, and CT scans) to recognise specific markers linked to diseases. For instance, they can identify potential cancerous cells on a biopsy slide or detect the early signs of diabetic retinopathy from a retinal scan. These powerful tools are some of the most practical AI tools for business in a clinical environment today.
To give you a clearer picture, here's a breakdown of how these technologies work in practice.
Key AI Technologies in Healthcare and Their Functions
| AI Technology | Core Function | Healthcare Application Example |
|---|---|---|
| Machine Learning (ML) | Learns patterns from data to make predictions or decisions. | A model that analyses patient data to predict the likelihood of hospital readmission. |
| Natural Language Processing (NLP) | Understands and interprets human language from text or speech. | An algorithm that scans doctors' notes to identify unreported adverse drug reactions. |
| Computer Vision | Interprets and analyses visual information from images and videos. | Software that detects signs of cancerous growths in mammograms or CT scans. |
As you can see, each technology plays a distinct but complementary role.
The infographic below shows how these different threads of data can come together.
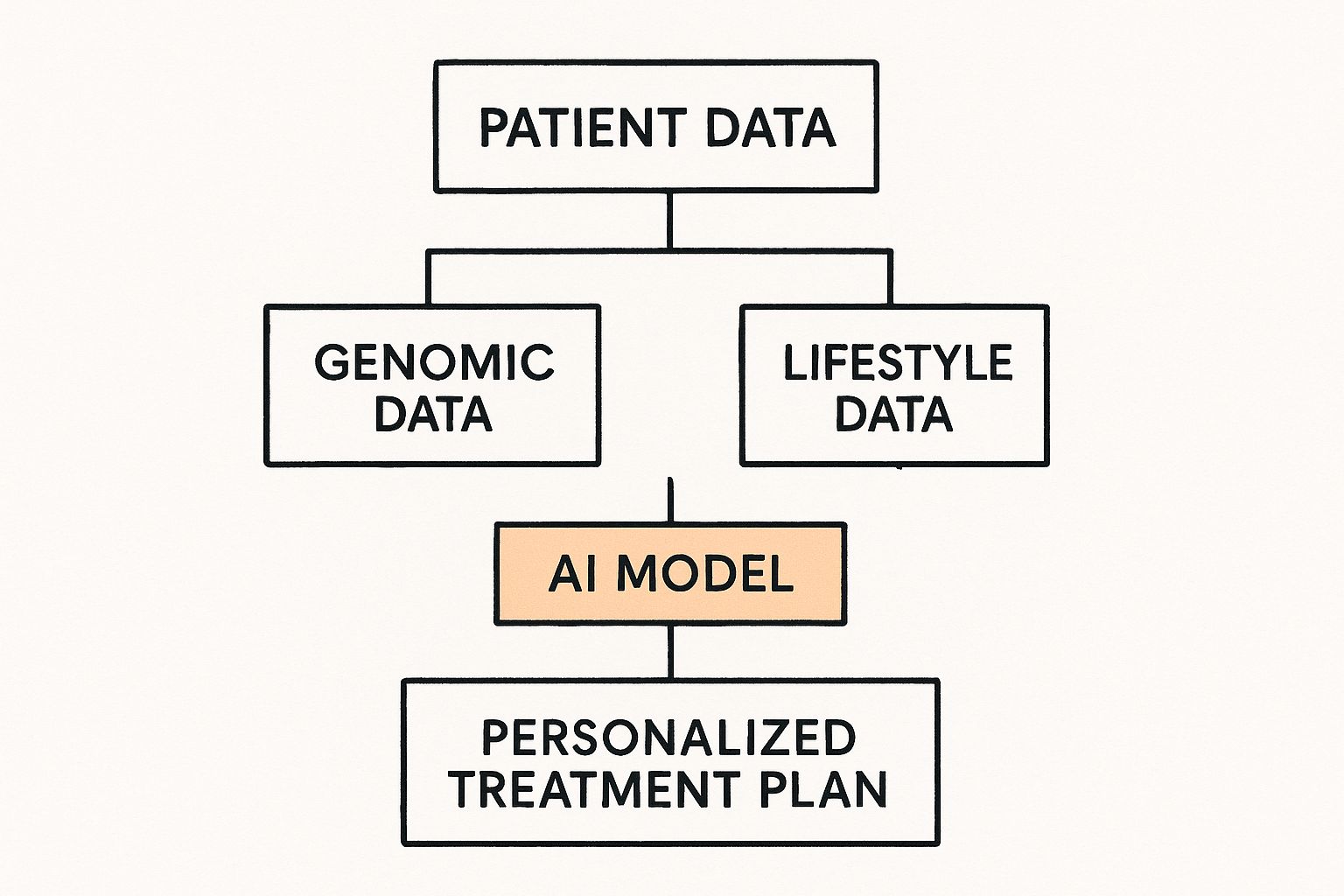
When AI models synthesise diverse inputs like genomic information and lifestyle data, they can generate truly personalised treatment plans.
Together, these three pillars—Machine Learning, Natural Language Processing, and Computer Vision—form the foundation of modern medical AI. They're the building blocks for the incredible applications we're about to explore, from smarter diagnostics to more efficient hospitals.
Better Diagnosis, Smarter Treatments: AI on the Front Line

If you want to see where AI truly makes a difference in healthcare, look no further than how we diagnose illness and treat patients. AI algorithms are becoming a powerful second pair of eyes for clinicians, helping them spot diseases earlier and create much more effective treatment plans. This is especially clear in medical imaging, where AI is bringing a new level of precision to radiology and pathology.
Imagine an AI model that has studied millions of mammograms. It learns to recognise the faintest, almost invisible patterns that could signal early-stage cancer and flags them for a radiologist to examine. This isn’t about replacing the human expert; it's about giving them a superpower—a tool that can sift through visual information on a scale no person ever could. The result is earlier, more reliable diagnoses.
Sharpening Diagnostic Accuracy
AI’s ability to untangle complex data is shifting diagnostics from a reactive to a proactive discipline. By spotting tiny anomalies in scans, tissue samples, and other medical data, these systems give clinicians a crucial head start, allowing them to step in before a condition worsens.
Radiology is a perfect example of this in action. AI tools have shown they can significantly cut down on errors, reducing false positives by up to 5.7% and false negatives by 9.4% in breast cancer screening. But technology alone isn't a magic wand. Despite these advancements, nearly 976,000 scans in England recently missed the NHS target for reporting by over a month. That’s a 28% jump from the previous year, highlighting that deep-seated operational hurdles still need to be cleared.
The Dawn of Personalised Medicine
Beyond diagnostics, AI is the engine powering personalised medicine, especially in genomics. Every patient's unique genetic code is a massive dataset filled with clues about their health. AI can analyse this genetic information alongside lifestyle habits and medical history to predict how someone will react to different treatments.
This paves the way for truly customised therapies. Instead of using a one-size-fits-all approach, doctors can choose medications and doses tailored to an individual patient, boosting effectiveness while minimising side effects.
By pulling together genomic, clinical, and lifestyle data, AI shifts treatment from educated guesswork to fine-tuned precision. It’s about giving the right patient the right treatment at exactly the right time.
This level of detail also helps streamline the mountain of paperwork and communication that bogs down clinical practice. Tools like the Clinic AI Assistant are already helping teams manage patient information more efficiently, freeing them up to focus on care.
Predicting Patient Futures with Analytics
Another game-changing application is predictive analytics. By poring over historical data, AI models can forecast a patient's risk of developing a disease or how their condition might progress. For instance, an algorithm could monitor a patient's vitals and lab results in real-time to predict the onset of sepsis hours before obvious symptoms appear, triggering an immediate life-saving response.
These predictive models aren’t just theory; they’re built on the analysis of thousands of patient cases. Some of the most valuable applications include:
- Spotting At-Risk Patients: AI can scan electronic health records to flag individuals with a high chance of developing chronic illnesses like diabetes or heart disease, prompting preventative care.
- Predicting Treatment Response: Models can forecast how a patient with a specific cancer might respond to a particular chemotherapy drug, helping oncologists make better-informed choices from the start.
- Forecasting Hospital Readmissions: By analysing a patient's data at discharge, AI can identify who is most likely to be readmitted, allowing hospitals to provide better follow-up care and support.
Making Hospitals More Efficient with AI
When we talk about artificial intelligence in healthcare, it’s easy to get caught up in the exciting stuff like diagnostics and treatments. But honestly, some of the most profound changes AI is making are behind the scenes, tackling the operational chaos that dogs so many hospitals. This is where AI helps with the administrative grind—the endless paperwork and logistical puzzles that lead to staff burnout and inefficiency.
Think about it from a practical standpoint. AI Automation as a Service can take on crucial but frustrating tasks that have always been done by hand. A classic example is patient scheduling. On the surface, it seems simple, but it’s actually a complex juggle of doctor availability, room bookings, and patient needs. AI can look at all these moving parts at once and create a schedule that just works, cutting down wait times and stopping those bottlenecks that everyone hates.
Automating the Administrative Burden
So much of a healthcare professional's day is eaten up by admin. This isn't just inefficient; it pulls them away from looking after patients. This is where custom internal tooling driven by AI can be a game-changer, potentially saving thousands of hours of repetitive work. These tools handle things like data entry, processing insurance claims, or medical coding with greater accuracy, freeing up skilled people to do what they were trained for.
This isn't just about efficiency for its own sake. It’s about morale and better care. When a nurse isn't drowning in forms, they have more time and energy for their patients. That directly translates to better health outcomes and a far better experience for everyone.
Predictive Power in Hospital Operations
Good workflow automation is more than just ticking off tasks. It's about looking ahead. AI models can crunch historical data on admissions, track local health trends, and even factor in things like public holidays to predict how busy a hospital will be. This foresight helps managers make smarter decisions.
- Optimise Staffing Levels: You can make sure you have enough clinicians on shift for a surge, but you're not overstaffed during quiet periods.
- Manage Bed Availability: By predicting when patients will be discharged and how many new ones are coming in, hospitals can manage bed capacity and avoid turning people away from A&E.
- Predict Supply Needs: AI can forecast the demand for everything from masks to critical medicines, making sure you never run out of essentials without wasting money on overstocking.
The growth here is huge. The UK's AI in healthcare market is expected to hit USD 12,493.8 million by 2030, with the NHS and other savvy providers leading the charge. You can dig deeper into the UK's AI healthcare market growth on Grandview Research and explore other real-world use cases.
By turning operational data into actionable foresight, AI allows hospitals to run less like frantic emergency rooms and more like well-organised, highly efficient systems.
Getting these benefits isn't automatic, though. It requires a solid plan. As we've discussed in our AI adoption guide, you need to start by figuring out where your biggest bottlenecks are and how a smart automation strategy can fix them. This is where a collaborative approach like AI co creation really shines, turning a promising technology into real-world results that build a stronger, more efficient healthcare system.
Navigating the Challenges of AI Adoption

Bringing artificial intelligence into healthcare is never as simple as just flicking a switch on new software. The path is littered with practical hurdles that have little to do with the technology itself and everything to do with data security, creaking infrastructure, and, crucially, human trust. To successfully integrate AI into a clinical setting, you have to face these barriers head-on with a clear, well-thought-out plan.
One of the first brick walls many organisations hit is trying to mesh sophisticated AI systems with their existing IT infrastructure. Plenty of hospitals still run on older, siloed systems that were never built for the sheer volume of data that modern machine learning demands. Getting these legacy platforms to communicate with new AI tools without grinding to a halt or opening up security holes is a massive technical and financial puzzle.
Building Trust and Overcoming Scepticism
Even if you solve the technical side, you’re left with a deeply human challenge: getting clinicians to trust the technology. Many AI models feel like a ‘black box’—they give you an answer, but the logic behind it is hidden. For a doctor or nurse whose decisions can mean life or death, that lack of transparency is a non-starter. Trust comes from systems that are not just accurate but also explainable.
This isn't a niche concern; it's widespread. A recent survey found that 73% of UK healthcare professionals have never used AI in their work. Their main worries? The fear of errors and a fundamental lack of confidence in the technology. This highlights that winning people over isn't just about better algorithms; it's about providing solid training and support to help professionals weave AI into their daily routines.
Addressing Data Privacy and Regulatory Hurdles
Then there's the maze of legal and regulatory standards. Healthcare data is some of the most sensitive information out there, guarded by strict rules. Any AI system you introduce must have data privacy and cybersecurity at its core to protect patients and stay on the right side of the law. This usually means putting robust legal compliance policies in place from day one.
Tackling these different obstacles calls for a structured approach. It really comes down to a few key actions:
- Start with a thorough technology audit to get an honest picture of your current system's limitations.
- Create a phased implementation plan, beginning with low-risk projects that can deliver clear wins.
- Build comprehensive training programmes to close the skills gap and build staff confidence.
- Set up clear governance frameworks for managing data and providing ethical oversight.
Successfully integrating AI is not a technology project; it is a change management initiative. It requires a strategic blueprint that addresses infrastructure, workflow integration, staff training, and ethical considerations in equal measure.
Finding your way through this complex process often requires expert guidance. A well-defined AI Product Development Workflow ensures each challenge is methodically handled from the very beginning. It's about turning potential roadblocks into a clear, secure, and ethical path forward.
What's Next for AI in Medicine?
If you think AI in healthcare is impressive now, just wait. What we're seeing today—smarter diagnostics, more efficient hospitals—is really just the opening act. The real story is shifting from simply treating sickness to proactively keeping people well.
The next big leap is all about preventative medicine. Think about AI that doesn't just flag a potential disease but helps stop it from ever developing. By crunching vast datasets of population health records, genetic markers, and even environmental influences, these systems can spot at-risk groups or individuals years before they feel a single symptom. This allows public health bodies to launch targeted interventions that get ahead of illness.
Generative AI and the Need for Strong Ethics
Generative AI is pouring fuel on this fire. In the world of drug discovery, for example, these models can dream up entirely new molecules and forecast how they'll work, potentially slashing the years and billions it takes to develop new medicines. In training, it can create incredibly realistic virtual patients, giving junior doctors and surgeons a safe space to hone their skills on complex procedures. To get a handle on these powerful tools, organisations need a solid plan, which is where something like a Custom AI Strategy report becomes invaluable.
The future of healthcare won't be built by technology in a vacuum. It will be forged by a genuine partnership—a kind of AI co creation—that brings technologists, clinicians, patients, and ethicists to the same table, making sure innovation always serves people first.
Of course, with great power comes great responsibility. As these AI capabilities grow, our ethical guidelines have to keep pace. Making sure we use artificial intelligence in healthcare responsibly means we need to face some tough questions:
- Algorithmic Fairness: How do we ensure our AI models don't perpetuate existing biases? We need to constantly check and correct them to avoid creating or worsening health inequalities.
- Data Governance: We need crystal-clear rules for protecting patient privacy while still enabling the research that drives progress. It's a delicate balance.
- Equitable Access: The incredible benefits of medical AI can't just be for the wealthy or those in top-tier health systems. They have to be available to everyone.
Getting this right isn't just about having good ideas; it requires a clear vision and a steady hand to guide the way. The goal is to build systems that are not only powerful but also fair, transparent, and trustworthy. To figure out how your organisation can navigate this new terrain and stay ahead, it's worth speaking with our expert team.
Frequently Asked Questions
As we explore the role of artificial intelligence in healthcare, a few key questions always come up. Let's tackle them head-on to get a clearer picture of what this shift really means for medicine.
What Are the Biggest Benefits of Using AI in Healthcare?
The two biggest wins are speed and precision. In fields like radiology and pathology, AI algorithms can spot subtle patterns in images that might escape the human eye, leading to much more accurate diagnoses. It’s also making truly personalised medicine possible by sifting through vast amounts of patient data—from genetics to lifestyle—to predict which treatments will work best for a specific individual.
Beyond the clinic, AI is a game-changer for hospital operations. By automating workflows with smart workflow automation and building custom internal tooling, it frees up staff from administrative headaches, optimises how hospital resources are used, and ultimately brings down costs. All this adds up to better outcomes for patients, less stress for clinicians, and a more efficient healthcare system.
Is AI Going to Replace Doctors and Nurses?
Not at all. The aim isn't to replace healthcare professionals, but to empower them. Think of AI as an incredibly capable assistant or a co-pilot, handling the repetitive, data-intensive tasks that consume so much of a clinician's day.
This frees up doctors and nurses to focus on what they do best: critical thinking, managing complex patient cases, and providing compassionate, face-to-face care. These are skills that technology can't replicate. AI provides insights and flags potential concerns, strengthening a clinician's judgement rather than overriding it. This kind of partnership is at the heart of effective AI co creation.
Think of AI as an incredibly skilled assistant. It can analyse millions of data points to provide a recommendation, but the final, nuanced decision will always rest with the experienced healthcare professional.
What Are the Main Risks of Using AI in Healthcare?
The biggest hurdles revolve around data, bias, and trust. Protecting patient data is non-negotiable, so any AI system has to be built with rock-solid security and privacy measures from the very beginning.
Another major worry is algorithmic bias. If an AI model is trained on data that doesn't accurately represent diverse populations, it can perpetuate and even worsen existing health inequalities. Then there’s the ‘black box’ problem—if doctors can't understand why an AI made a certain recommendation, they won't trust it.
Getting this right means putting strong governance in place, constantly checking the models for fairness and accuracy, and training staff properly. Having a roadmap, like a Custom AI Strategy report, is crucial for navigating these complexities. To learn more about how to get started, you can chat with our expert team.
Ready to discover how AI can transform your organisation? Ekipa AI delivers tailored AI strategies and end-to-end execution to turn your ideas into scalable impact. Explore our services today, and meet the team that can make it happen.