Best AI Medical Scribe: 5 Top Solutions for 2026
Best AI Medical Scribe: Compare top tools, features, and pricing to pick the right solution for your practice in 2026.

Physician burnout is a critical issue, with administrative tasks and clinical documentation consuming hours that could be spent on direct patient care. While traditional human scribes offered a solution, scaling them is often costly and logistically complex. A new generation of AI is now transforming this landscape. The best AI medical scribe platforms promise to eliminate the documentation burden by ambiently capturing patient conversations and converting them into structured, accurate clinical notes, often directly within the Electronic Health Record (EHR).
This technological shift not only saves clinicians up to two hours per day but also enhances note quality and allows for more focused patient interaction. To fully grasp their capabilities, understanding the foundational technology is key; a comprehensive guide to audio transcription offers a great overview of the core principles involved. However, with dozens of specialized tools flooding the market, how do you choose the right one for your specific clinical environment? This guide is designed to cut through the noise and provide clear, actionable insights.
We will break down the top AI medical scribe solutions, analyzing their accuracy, EHR integration capabilities, security protocols, and overall suitability for different settings, from solo practices and telehealth providers to large hospital systems. For each platform, you'll find a detailed review, screenshots, and direct links to help your evaluation. Selecting the right AI tools is a strategic decision that impacts both operational efficiency and the quality of care. This resource provides the clarity needed to navigate your options and find the perfect fit for your organization's needs, a crucial step in building a robust AI strategy consulting framework.
1. Nuance Dragon Ambient eXperience (DAX) Copilot
Nuance DAX Copilot represents the enterprise-grade pinnacle of ambient clinical intelligence, making it a leading contender for the title of best AI medical scribe, especially for large, established healthcare organizations. Acquired by Microsoft, Nuance has leveraged its deep history in clinical documentation and voice recognition to build a powerful, secure, and deeply integrated solution. Its core function is to listen to the natural conversation between a clinician and patient, then automatically draft comprehensive clinical notes directly within the electronic health record (EHR).
What sets DAX Copilot apart is its mature ecosystem and deep-seated EHR integrations. It’s not a standalone app but a workflow-embedded tool designed for systems like Epic and MEDITECH Expanse. This integration minimizes friction, allowing physicians to review and sign off on AI-generated notes without ever leaving their primary work environment. This deep embedding is a critical differentiator for hospitals focused on maximizing physician adoption and minimizing workflow disruption.
Key Features & Differentiators
Ambient AI Capture: The system passively captures multi-speaker conversations in exam rooms or via telehealth, distinguishing between the clinician, patient, and other speakers to create accurate, structured SOAP notes.
Deep EHR Integration: Its primary strength lies in seamless workflows within major EHRs, reducing the need for context switching and copy-pasting.
Enterprise-Grade Security: Built on Microsoft Azure, it boasts a strong security and compliance posture, including a HITRUST certification, which is a crucial requirement for large health systems handling sensitive patient data.
Proven Scalability: It has been deployed across major U.S. health systems, demonstrating its ability to handle high volumes and complex organizational needs.
| Feature | Nuance DAX Copilot Offering |
|---|---|
| Primary Use Case | Large hospitals and multi-site health systems |
| Integration Level | Deep, native embedding in Epic, Cerner, MEDITECH |
| Onboarding | Sales-led, enterprise implementation process |
| Pricing Model | Premium, per-provider licensing (requires custom quote) |
Pros:
Proven scalability and reliability in large-scale deployments.
Robust security and compliance backed by Microsoft's infrastructure.
Mature, deep integrations with leading EHR vendors.
Cons:
Premium pricing makes it less accessible for smaller clinics.
Lacks a self-service or instant-onboarding option for individual practitioners.
2. Abridge
Abridge has rapidly emerged as a powerful AI medical scribe, focusing on creating structured, billable clinical notes from ambient conversations with auditable evidence. It is engineered for health systems that prioritize not just note generation but also data integrity and deep workflow integration, particularly within the Epic ecosystem. Abridge listens to the patient-clinician dialogue and generates a real-time summary, highlighting key medical details and ensuring every part of the note can be traced back to the original conversation.
What truly differentiates Abridge is its "Linked Evidence" feature. This allows clinicians to click on any part of the generated note and instantly hear the corresponding segment of the conversation, providing an unparalleled level of transparency and trust. This focus on auditable, billable documentation makes it a compelling choice for large organizations aiming to streamline revenue cycle management while simultaneously reducing physician burnout. Its tight integration with Epic's mobile (Haiku) and desktop (Hyperspace) applications ensures a seamless experience within the existing clinical workflow.
Key Features & Differentiators
Linked Evidence: Every sentence in the generated note is linked to the specific moment in the audio conversation, enabling instant verification and building clinical trust.
Deep Epic Integration: Offers a fluid user experience within Epic Haiku and Hyperspace, allowing clinicians to manage notes without switching applications.
Actionable Outputs: The platform can identify and suggest potential orders and next steps directly from the conversation, accelerating point-of-care decision-making.
Enterprise Governance: Designed with health systems in mind, offering the security, scalability, and administrative controls necessary for large-scale deployment.
| Feature | Abridge Offering |
|---|---|
| Primary Use Case | Health systems and large clinics, especially those using Epic |
| Integration Level | Deep, native embedding in Epic Haiku/Hyperspace |
| Onboarding | Sales-led, enterprise implementation process |
| Pricing Model | Per-provider, per-month enterprise licensing (requires custom quote) |
Pros:
Groundbreaking "Linked Evidence" feature provides exceptional note transparency.
Strong Epic workflow integration creates a seamless user experience.
Rapidly growing adoption across major U.S. health systems demonstrates its effectiveness.
Cons:
Pricing is not publicly available and requires an enterprise sales process.
Primarily oriented toward health systems, making it less accessible for solo practitioners.
3. Suki
Suki emerges as a versatile and powerful AI assistant that extends beyond simple documentation, making it another top choice for the best AI medical scribe. Positioned for both individual physicians and large health systems, Suki offers a compelling blend of ambient note generation, direct dictation, and integrated coding assistance. Its core value is reducing administrative burden not just by listening to patient encounters but also by helping clinicians efficiently manage related tasks like finding information or completing orders with voice commands.
What truly differentiates Suki is its bidirectional EHR integration and its focus on coding. Unlike many tools that just push notes into the EHR, Suki can pull patient data and interact with the record more dynamically. The inclusion of ICD-10 and HCC coding assistance directly within the workflow provides a significant ROI for organizations focused on revenue cycle accuracy. This combination of clinical documentation and administrative support makes it a highly practical tool for busy practices looking to streamline multiple facets of the patient encounter.
Key Features & Differentiators
Ambient and Dictation Modes: Offers the flexibility to passively listen to a conversation or to actively dictate notes and commands, suiting different clinical scenarios and physician preferences.
Integrated Coding Assistance: Provides real-time suggestions for ICD-10 and HCC codes based on the clinical note, helping to improve billing accuracy and close care gaps.
Bidirectional EHR Integrations: Connects deeply with major EHRs like Epic, Oracle Health, and athenahealth, allowing for both pushing notes and pulling relevant patient data via voice.
Cross-Platform Availability: Accessible via dedicated iOS and Android apps as well as on desktop, providing flexibility for clinicians whether they are in the clinic, hospital, or on the go.
| Feature | Suki Offering |
|---|---|
| Primary Use Case | Clinics and health systems needing documentation and coding support |
| Integration Level | Bidirectional with Epic, Oracle Health, athenahealth, MEDITECH |
| Onboarding | Sales-led demonstration and guided implementation process |
| Pricing Model | Per-provider, subscription-based (requires a custom quote) |
Pros:
Strong bidirectional EHR connectivity enhances workflow efficiency.
Built-in coding assistance provides a direct impact on revenue cycle management.
Offers 24/7 support and is available on mobile and desktop platforms.
Cons:
Pricing is not publicly available and generally requires a sales-led process.
May be more feature-rich than what a solo practitioner requires.
4. Augmedix
Augmedix provides a hybrid model that makes it a compelling and flexible contender for the best AI medical scribe, catering to diverse clinical needs and budgets. The platform uniquely offers a spectrum of services, from a fully automated ambient AI solution, Augmedix Go, to traditional human-in-the-loop scribe services. This allows healthcare organizations to choose the level of automation and human oversight that best fits their specific workflows, from fast-paced primary care to complex specialty consultations.
What sets Augmedix apart is its tiered product strategy. Clinicians can start with the self-service mobile app for instant, AI-generated note drafts, or they can opt for a managed service where a real-time scribe assists with documentation. This product range makes it an excellent choice for organizations seeking to pilot AI documentation with a lower barrier to entry while retaining the option to scale to a more comprehensive, human-supported service for providers who require a higher level of accuracy and support.
Key Features & Differentiators
Hybrid Service Model: Offers both a pure AI ambient listening app (Augmedix Go) and human-assisted remote scribing, providing a unique "best of both worlds" approach.
Mobile-First Accessibility: The Augmedix Go app is designed for clinician-controlled recording and review directly from a smartphone, offering high flexibility and ease of use.
Established Vendor: Augmedix is a publicly-traded company with a long history in the medical scribe industry, providing established trust and deep experience in clinical environments.
Scalable Implementations: The platform is designed to support everyone from individual practitioners to large-scale hospital and health system deployments.
| Feature | Augmedix Offering |
|---|---|
| Primary Use Case | Clinics and hospitals wanting a flexible AI scribe solution |
| Integration Level | EHR integration supported; varies by service tier |
| Onboarding | Sales-led process for both automated and managed services |
| Pricing Model | Custom quotes based on service level and provider volume |
Pros:
Flexible product range covers fully automated AI to human-assisted services.
Established company with a strong track record and public references.
Mobile app offers a convenient and user-friendly experience for clinicians.
Cons:
Pricing is not publicly available and requires a sales consultation.
The fully automated app may have limited availability for new customers or smaller practices.
5. DeepScribe
DeepScribe positions itself as a strong ambient AI medical scribe with a notable emphasis on specialty-specific workflows, particularly in complex fields like oncology. It goes beyond simple transcription by aiming to understand the context and nuances of patient encounters. The platform is designed to listen to the natural conversation between a clinician and patient, then intelligently generate structured clinical notes, pre-charting information, and even suggest billing codes.
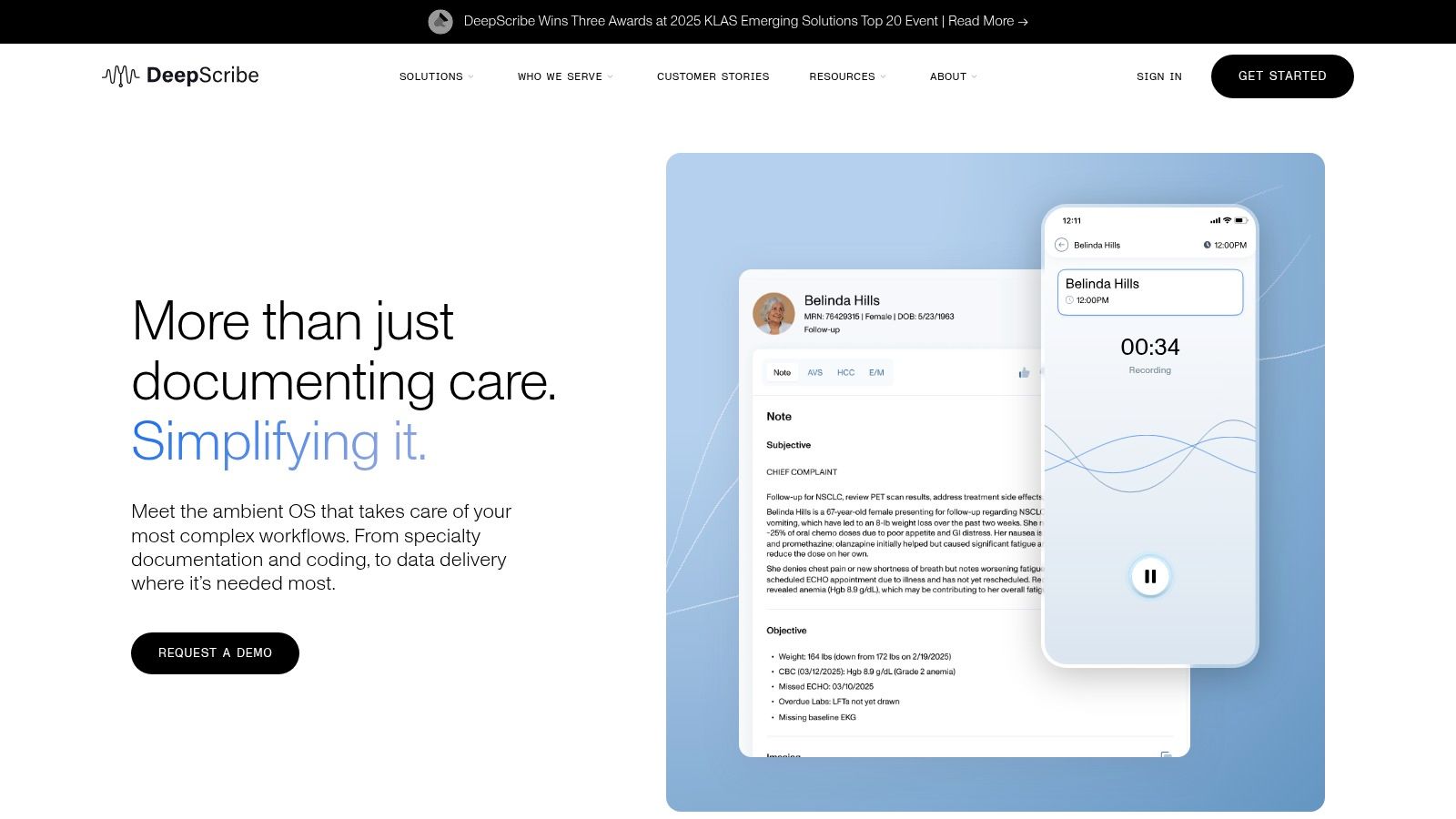
What differentiates DeepScribe is its focus on deep clinical understanding and customization. Its "Customization Studio" allows practices to tailor the AI's output to their specific documentation styles and templates, a crucial feature for specialties with unique noting requirements. Furthermore, by integrating AI-powered coding and pre-charting, DeepScribe aims to streamline more of the administrative workflow, not just the note-taking portion. This dual focus on specialty depth and workflow automation makes it a compelling option for outpatient clinics seeking a comprehensive solution. The platform's ability to extract structured data from conversations is a prime example of an advanced AI-powered data extraction engine in action, as detailed in Ekipa AI's product overview.
Key Features & Differentiators
Specialty-Specific AI: The platform is trained on data from over 25 specialties, allowing for more accurate and context-aware documentation in fields like cardiology, orthopedics, and oncology.
Customization Studio: Enables providers to fine-tune the AI's note-generation style, ensuring documentation aligns with their personal or practice-wide preferences.
Telemedicine and Mobile Support: Offers flexibility with dedicated iOS and Android apps, seamlessly supporting both in-person and virtual patient encounters.
AI Coding Intelligence: Suggests relevant ICD-10 and CPT codes based on the encounter, helping to streamline the billing process and improve revenue cycle management.
| Feature | DeepScribe Offering |
|---|---|
| Primary Use Case | Specialty clinics, outpatient groups, and telemedicine providers |
| Integration Level | API-based integrations with 100+ EHRs including athenahealth and eClinicalWorks |
| Onboarding | Sales-led demonstration and implementation process |
| Pricing Model | Custom, per-provider subscription (requires quote) |
Pros:
Strong focus on specialty-specific documentation and customization.
Supports both mobile and telehealth workflows effectively.
Includes value-add features like AI-powered billing code suggestions.
Cons:
Pricing is not transparent and requires engaging with the sales team.
The onboarding process is not self-service, making it less suitable for individual users seeking immediate setup.
6. Ambience Healthcare (AutoScribe)
Ambience Healthcare positions its AutoScribe platform as more than just an AI scribe; it’s a comprehensive clinical documentation and revenue integrity tool. This makes it a compelling candidate for the best AI medical scribe for health systems focused on demonstrating a clear financial return on investment. The platform not only captures the patient encounter ambiently but also actively assists clinicians with real-time coding and compliance guidance, directly linking documentation quality to financial outcomes.
What truly differentiates AutoScribe is its embedded focus on the revenue cycle. While drafting notes, the system provides real-time E/M and ICD-10/CPT suggestions based on the conversation and documented findings. This feature helps ensure that the final note accurately supports the level of service billed, reducing under-coding and audit risks. For large organizations, its suite of analytics and governance tools provides critical oversight into documentation trends and their impact on revenue integrity, making it one of the more unique AI solutions in the scribe market.
Key Features & Differentiators
Embedded Coding Guidance: Provides real-time suggestions for E/M levels and relevant ICD-10/CPT codes during the documentation process, aiming to improve billing accuracy.
Revenue Integrity Analytics: Offers dashboards and governance tools for health system leaders to monitor documentation quality and its direct impact on financial performance.
Ambient Note Creation: Captures the natural clinician-patient conversation to automatically generate structured clinical notes, reducing administrative burden.
Proven Enterprise Outcomes: The company highlights case studies and external validation to demonstrate tangible ROI and improvements in clinician burnout for large-scale deployments.
| Feature | Ambience Healthcare (AutoScribe) Offering |
|---|---|
| Primary Use Case | Health systems and large practices focused on revenue cycle optimization |
| Integration Level | Integrates with major EHRs, though not always as deeply native as some competitors |
| Onboarding | Enterprise-focused, sales-led implementation process |
| Pricing Model | Custom, per-provider licensing (requires quote) |
Pros:
Strong, unique focus on connecting documentation to financial ROI.
Provides real-time coding prompts to improve billing accuracy and compliance.
Backed by published case studies demonstrating successful enterprise outcomes.
Cons:
Primarily oriented toward large health systems, making it less accessible for small clinics.
Pricing is not transparent and requires a direct sales engagement.
7. Nabla Copilot
Nabla Copilot offers a compelling, lightweight alternative in the ambient scribe market, making it one of the best AI medical scribe options for individual clinicians and small practices prioritizing speed and privacy. It is designed for practitioners who want to get started immediately without lengthy sales cycles or complex implementations. Its core value proposition is its browser-based simplicity and a strong emphasis on client-side data handling, appealing to users wary of their data being stored on vendor servers.
What makes Nabla stand out is its instant accessibility and EHR-agnostic design. A physician can sign up and start using the tool within minutes directly from a web browser, capturing patient encounters and receiving draft clinical notes almost immediately. This frictionless onboarding is a significant advantage for those who want to test the waters of AI scribing without committing to an enterprise-level contract. This approach is ideal for tech-savvy clinicians in private practice, telehealth providers, or those in settings where IT resources are limited.
Key Features & Differentiators
Browser-Based Capture: Allows for easy access and use on any computer with a web browser, eliminating the need for special hardware or software installations.
Rapid Self-Onboarding: Clinicians can sign up and begin using the service almost instantly, often with a free trial, providing immediate time-to-value.
Strong Privacy Stance: The platform emphasizes that user data is not persistently stored on its servers, addressing a key concern for many healthcare professionals.
EHR-Agnostic Workflow: Functions as a standalone tool, allowing notes to be easily copied and pasted into any EHR system, offering maximum flexibility. You can learn more about how Nabla Copilot and other AI tools for business are transforming professional workflows.
| Feature | Nabla Copilot Offering |
|---|---|
| Primary Use Case | Individual clinicians, small practices, and telehealth providers |
| Integration Level | Standalone, copy-paste functionality for any EHR |
| Onboarding | Self-service, instant sign-up with free trial |
| Pricing Model | Monthly subscription tiers, publicly listed |
Pros:
Extremely fast and easy to get started with its self-serve model.
Competitive and transparent monthly pricing is ideal for smaller budgets.
Strong privacy focus provides peace of mind for security-conscious users.
Cons:
Lacks the deep, embedded EHR integrations required by large hospital systems.
Public pricing may vary and should be verified directly for the most current rates.
8. 3M Health Information Systems (M*Modal Fluency / Ambient Clinical Documentation)
3M Health Information Systems provides a comprehensive suite of clinical documentation tools, including the M*Modal Fluency portfolio, which has evolved to offer ambient scribe capabilities. As a long-standing vendor in healthcare IT, 3M targets large, complex health systems that require robust, scalable solutions from an established partner. Its offerings are designed to streamline documentation workflows across diverse clinical environments.
The primary differentiator for 3M is its massive installed base and extensive EHR compatibility, supporting over 250 different systems with its Fluency Direct speech recognition engine. This makes it a strong contender for the best AI medical scribe in multi-system environments where a single, unified solution is needed. Leveraging partnerships with AWS, 3M integrates advanced AI services like Comprehend Medical to power its ambient documentation, ensuring a technologically current and scalable platform. This is a great example of custom healthcare software development meeting enterprise-scale needs.
Key Features & Differentiators
Broad EHR Compatibility: Its core strength is the ability to integrate with over 250 EHRs, providing flexibility for organizations with a mix of legacy and modern systems.
Ambient Documentation: The platform offers ambient listening and virtual assistant features to automate the creation of clinical notes from natural patient conversations.
Cloud-Powered AI: Utilizes AWS services like Transcribe Medical and Comprehend Medical to enhance the accuracy and scalability of its AI-driven documentation.
Enterprise-Class Support: As a major player in the industry, 3M provides extensive implementation, training, and support services tailored for large healthcare organizations.
| Feature | 3M HIS (M*Modal) Offering |
|---|---|
| Primary Use Case | Large health systems and hospitals with diverse EHR environments |
| Integration Level | Broad compatibility with 250+ EHRs via cloud speech platform |
| Onboarding | Enterprise-level, sales-led implementation and deployment |
| Pricing Model | Per-provider, quote-based enterprise licensing |
Pros:
Exceptional EHR compatibility simplifies deployment in multi-system health networks.
Backed by a large, established vendor with significant enterprise support capabilities.
Leverages powerful cloud AI services for performance and scale.
Cons:
Procurement and deployment processes are designed for enterprise workflows, not individual clinics.
Product information can be suite-oriented, making it hard to evaluate the standalone scribe offering.
9. Freed AI (getfreed.ai)
Freed AI is designed for individual clinicians and small-to-mid-size practices that need a simple, self-serve ambient scribe without the enterprise-level complexity or cost. It carves out its niche by offering a straightforward, transparently priced solution that users can try and adopt within minutes. Its core value is providing a fast, accessible, and effective tool that generates SOAP notes from patient conversations, positioning itself as a strong candidate for the best AI medical scribe for those prioritizing ease of use and speed.
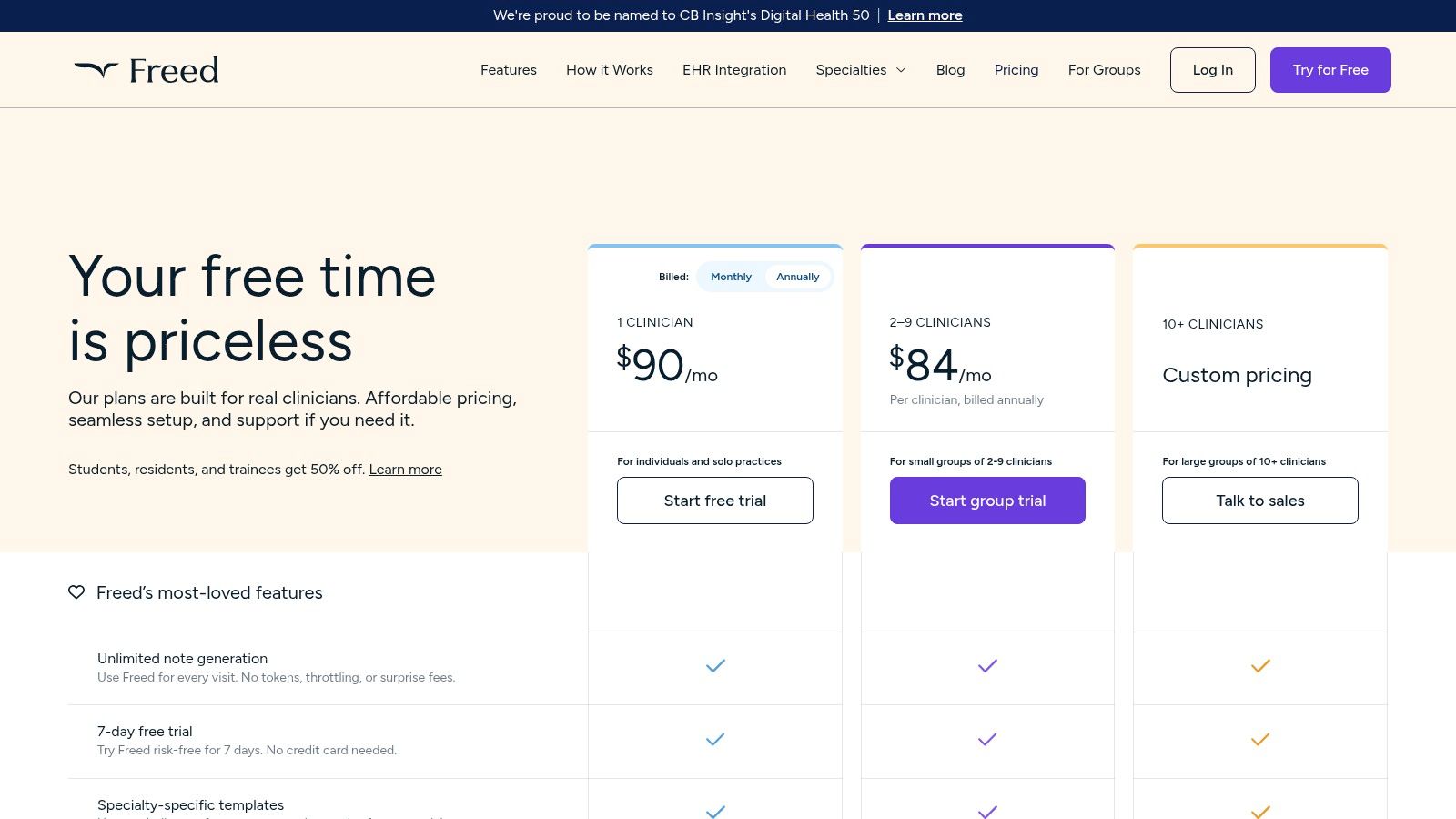
What differentiates Freed is its user-first, self-service model. Unlike enterprise systems requiring lengthy sales cycles, Freed offers a 7-day free trial and public pricing tiers, empowering physicians to test the platform on their own terms. This approach drastically lowers the barrier to entry, making it an ideal choice for smaller clinics or solo practitioners looking to reduce their documentation burden immediately. The platform's focus on essential features, like specialty-specific templates and simple EHR data transfer, makes it a practical, no-frills solution.
Key Features & Differentiators
Self-Service Onboarding: Users can sign up for a free trial and begin using the service instantly, a major advantage over platforms requiring a sales consultation and formal implementation.
Transparent Pricing: Clear, publicly listed pricing tiers allow for easy cost-benefit analysis without needing a custom quote, which is rare in the clinical documentation space.
EHR Push (Beta): While not a deep native integration, its browser-based extension allows for one-click copy-pasting of notes into web-based EHRs, streamlining the workflow.
Security & Compliance: The platform is HIPAA-compliant and SOC 2 certified, with clear options for users to manage and delete their data, addressing key security concerns for smaller practices.
| Feature | Freed AI Offering |
|---|---|
| Primary Use Case | Solo practitioners, small to mid-size private clinics |
| Integration Level | Browser-based extension for pushing notes into web EHRs |
| Onboarding | Self-service with a 7-day free trial |
| Pricing Model | Transparent monthly/annual subscriptions with public tiers |
Pros:
Extremely fast and simple self-onboarding process.
Clear, public pricing makes it accessible for small budgets.
Ideal for individual providers and smaller clinical groups.
Cons:
Integrations are lighter compared to deeply embedded enterprise tools.
Advanced enterprise features and customizations require contacting sales.
10. Tali AI
Tali AI carves out a unique space in the AI medical scribe market by prioritizing transparency, accessibility, and self-service. It's an excellent choice for individual practitioners, small clinics, and teams who want to test the waters with a free trial before committing to a paid plan. Unlike enterprise-first solutions, Tali's public pricing and straightforward onboarding process lower the barrier to entry, making it one of the more approachable options available.
What distinguishes Tali AI is its balance between powerful features and user-friendly access. The platform doesn't just offer an AI scribe; it also includes direct-to-EHR dictation, customizable templates, and even a knowledge base assistant. This combination of tools makes it a versatile digital assistant rather than just a simple transcription service. Its appeal lies in this flexibility, catering to clinicians who value the ability to sign up and start immediately without a lengthy sales process. This type of solution is a great example of how AI can improve internal tooling for professional teams.
Key Features & Differentiators
Public Pricing & Free Trial: Offers a 14-day free trial of its Pro plan and transparent pricing tiers, allowing users to evaluate the platform thoroughly before purchase.
Versatile Toolset: Combines an ambient AI scribe with direct dictation into EHR fields and an AI-powered knowledge base assistant for quick clinical lookups.
Multilingual Support: Includes multilingual note translation capabilities, adding significant value for clinicians serving diverse patient populations.
Self-Serve Onboarding: Designed for quick adoption by individuals and small groups who can sign up and integrate the tool into their workflow with minimal friction.
| Feature | Tali AI Offering |
|---|---|
| Primary Use Case | Solo practitioners, small to mid-sized clinics, and pilot programs |
| Integration Level | Chrome extension for web-based EHRs; direct dictation |
| Onboarding | Self-service sign-up with a free trial; sales for enterprise |
| Pricing Model | Publicly listed monthly/annual subscription tiers |
Pros:
Transparent pricing and a free trial make it easy to get started.
Excellent fit for solo clinicians and smaller practices.
A bundled toolset offers more than just scribing.
Cons:
Advanced EHR integrations can be less seamless than deeply embedded enterprise tools.
Large-scale or complex hospital deployments still require a sales-led process.
11. Notable (Ambient Scribe agent)
Notable’s Ambient Scribe stands out by positioning its AI medical scribe not as a standalone product, but as a key "agent" within a much broader healthcare automation platform. This approach is designed for health systems that want to solve clinical documentation burnout while simultaneously automating adjacent administrative tasks like revenue cycle management, prior authorizations, and patient outreach. It treats the clinical note as the starting point for a cascade of automated workflows.
The core differentiator is its extensible, platform-based model. While the Ambient Scribe agent captures the patient-clinician conversation in real-time to generate notes, other agents in Notable's library can be configured to use that data to trigger downstream actions. For example, once a diagnosis is documented, an agent could automatically check for required authorizations or schedule a follow-up appointment. This makes Notable an ideal choice for organizations pursuing end-to-end automation rather than just a point solution for documentation, often as part of an AI Automation as a Service strategy.
Key Features & Differentiators
Ambient Scribe Agent: Captures encounter conversations to generate accurate, real-time clinical documentation.
Workflow Automation Library: An extensive collection of pre-built "agents" that can automate tasks across the revenue cycle, patient engagement, and population health.
Extensible Platform: Allows health systems to configure and deploy automations tailored to their specific operational workflows and goals.
Enterprise Governance & Analytics: Provides robust tools for managing automations at scale, with analytics to track performance and ROI.
| Feature | Notable Offering |
|---|---|
| Primary Use Case | Health systems seeking platform-level automation beyond clinical notes |
| Integration Level | Deep, workflow-level integration with EHRs and other administrative systems |
| Onboarding | Enterprise, sales-led implementation and workflow configuration |
| Pricing Model | Custom, bundled pricing based on the scope of automation agents deployed |
Pros:
Holistic platform approach connects scribing with revenue-cycle and administrative automations.
Extensible and configurable to match unique organizational workflows.
Strong focus on enterprise-grade analytics and governance.
Cons:
Enterprise focus and sales-led process make it inaccessible for smaller practices.
Pricing is bundled and not transparent, requiring a custom quote based on scope.
12. G2 (Medical Transcription / AI Scribe listings)
G2 serves a unique role in this list, acting not as an AI medical scribe itself, but as a crucial aggregator and review platform for them. For healthcare leaders overwhelmed by options, G2 provides a crowdsourced reality check, offering peer-driven insights into how different AI scribe tools perform in the wild. It’s an essential first stop for creating a shortlist and comparing vendors based on user satisfaction, feature sets, and market presence.
What makes G2 invaluable is its ability to surface both established leaders and emerging innovators in the clinical documentation space. It allows buyers to filter and compare solutions side-by-side, reading candid reviews from verified users in similar roles. This peer feedback provides a layer of validation that vendor marketing materials cannot, helping decision-makers identify potential red flags or hidden strengths before committing to a demo. Effectively using G2 can significantly streamline the initial research phase of selecting the best AI medical scribe.
Key Features & Differentiators
Crowdsourced User Reviews: Offers access to authentic feedback, satisfaction ratings, and detailed commentary from real-world clinical and administrative users.
Grid Comparison Reports: Features dynamic comparison grids that allow buyers to visually stack vendors against one another based on satisfaction, features, and market presence.
Vendor Profiles & Demos: Centralizes vendor information and provides direct links to schedule demos or start trials, simplifying the next steps in the procurement process.
Niche Tool Discovery: Excellent for identifying newer or specialty-specific tools that might not appear in traditional analyst reports but are highly rated by their user base.
| Feature | G2 Offering |
|---|---|
| Primary Use Case | Vendor discovery, comparison, and initial shortlisting |
| Integration Level | N/A (Links out to individual vendor platforms) |
| Onboarding | Free to browse, with optional user account creation |
| Pricing Model | Free for buyers; vendors pay for enhanced profiles |
Pros:
Provides unbiased, peer-driven feedback to validate vendor claims.
Free and easily accessible resource for market research.
Helps surface new and innovative AI scribe solutions.
Cons:
Requires careful filtering as "Medical Transcription" can include non-AI services.
Pricing and specific implementation details often require leaving G2 to engage with vendors directly.
Top 12 AI Medical Scribes — Feature Comparison
| Vendor | Core capabilities | Deployment & EHR integration | Target customers & value proposition | Pricing & onboarding | Key differentiator |
|---|---|---|---|---|---|
| Nuance Dragon Ambient eXperience (DAX) Copilot | Ambient multi‑speaker capture; generative clinical note drafts | Deep Epic & MEDITECH Expanse integrations; Azure/HITRUST; Microsoft channel distribution | Large health systems needing mature, EHR‑embedded ambient scribe | Premium, sales‑led onboarding | Enterprise‑grade EHR integrations and Microsoft compliance/distribution |
| Abridge | Context‑aware notes with “Linked Evidence”; actionable orders at point of care | Deep Epic (Haiku/Hyperspace) integration; enterprise deployments | Systems requiring auditable, billable documentation and governance | Sales‑led pricing; enterprise onboarding | Auditable provenance for billable clinical notes |
| Suki | Ambient documentation, voice commands, coding assistance (ICD‑10/HCC) | Bidirectional EHR integrations (Epic, Oracle, athena, MEDITECH); iOS/Android/web | Enterprises needing coding support plus robust EHR connectivity | Sales‑led pricing; demo/quote required | Built‑in coding assistance and 24/7 support |
| Augmedix | Automated draft notes + human‑in‑the‑loop scribe options; mobile app | Hospital and health‑system implementations; clinician review workflows | Organizations wanting flexible accuracy/budget tradeoffs (auto → human) | Sales‑led pricing; enterprise availability | Mix of automated scribe and managed human scribe services |
| DeepScribe | Specialty‑aware documentation; AI pre‑charting and coding intelligence | Multiple EHR integrations; telemedicine and mobile support | Specialty clinicians (e.g., oncology) and telehealth teams | Sales‑led pricing; contact sales for enterprise tiers | Specialty customization studio and strong telehealth workflows |
| Ambience Healthcare (AutoScribe) | Ambient notes + real‑time coding prompts; revenue integrity tools | Enterprise deployments with health‑system analytics | Health systems focused on documentation quality tied to financial ROI | Sales‑led pricing; enterprise engagement | Emphasis on documentation → financial outcomes and ROI case studies |
| Nabla Copilot | Browser‑based capture; fast self‑serve draft notes; client‑side privacy | EHR‑agnostic workflows; quick self‑onboarding; MFA/security controls | Clinicians wanting rapid, privacy‑focused self‑serve solution | Competitive monthly tiers; try‑for‑free/self‑serve | Privacy‑first claims and rapid time‑to‑value for individuals |
| 3M (M*Modal Fluency / Ambient Clinical Documentation) | Cloud speech recognition and ambient documentation | Broad EHR compatibility (250+ systems); AWS collaborations; enterprise support | Large organizations needing long‑standing documentation vendors | Sales‑led, suite‑oriented procurement | Large installed base and broad EHR coverage |
| Freed AI (getfreed.ai) | Unlimited notes (paid tiers); specialty templates; EHR push (beta) | Self‑serve setup for small/mid clinics; SOC2/HIPAA claims | Solo clinicians and small groups seeking transparent pricing | Public pricing pages; 7‑day free trial | Clear public pricing and fast self‑onboarding |
| Tali AI | AI scribe, dictation into EHR fields; multilingual notes | EHR text‑field dictation; templates; knowledge base features | Individuals and multi‑provider clinics needing self‑serve plans | Published plans; 14‑day Pro trial | Publicly listed plans and unlimited scribes on Pro tier |
| Notable (Ambient Scribe agent) | Real‑time ambient scribe agent plus workflow automation agents | Extensible platform with enterprise security and analytics | Organizations seeking platform automation beyond documentation (RCM, authorizations) | Sales‑led, bundled/agent pricing | Platform‑level automation library that extends beyond notes |
| G2 (Medical Transcription / AI Scribe listings) | Crowdsourced reviews, vendor comparisons, category reports | Marketplace with vendor profiles and links to demos/signups | Buyers shortlisting vendors and seeking peer feedback | Free to browse; vendor pricing off‑site | Peer reviews and comparative insights to inform shortlists |
Making the Right Choice: How to Select and Implement Your AI Medical Scribe
The journey to find the best AI medical scribe is not about chasing the newest technology; it's about finding the right technological partner for your clinical practice. As we've explored, the landscape is diverse. Tools like Nuance DAX Copilot and 3M M*Modal offer enterprise-grade solutions with deep EHR integration, making them ideal for large hospital systems. In contrast, platforms like Abridge and Suki balance robust features with user-centric design, fitting well within mid-sized practices and specialty clinics focused on improving clinician experience.
For smaller, more agile settings, solutions such as Freed AI or Tali AI provide accessible, straightforward options that can deliver immediate value without a complex implementation cycle. The key takeaway is that there is no single "best" solution for everyone. Your unique clinical workflows, existing technology stack, patient volume, and budget are the critical factors that will guide your decision. The right tool for a high-volume telehealth provider will differ significantly from one needed in a hands-on specialty practice.
From Selection to Successful Implementation
Choosing a vendor is only the first step. The true measure of success lies in seamless adoption and tangible improvements in clinical efficiency and physician well-being. A successful rollout requires a deliberate strategy that goes beyond simply installing software.
Conduct a Pilot Program: Before committing to a full-scale deployment, identify a small, enthusiastic group of clinicians to pilot your top two or three choices. This provides invaluable real-world feedback on accuracy, workflow fit, and usability that you can't get from a sales demo. Collect both quantitative data (e.g., time saved per note) and qualitative feedback.
Prioritize Change Management: Technology is only effective if people use it. As we explored in our AI adoption guide, you must communicate the "why" behind the change, emphasizing the benefits of reduced administrative burden and more time for patient care. Provide comprehensive training, create champions within your teams, and establish a clear feedback loop for continuous improvement.
Define Clear Success Metrics: How will you know the investment is paying off? Establish key performance indicators (KPIs) before you begin. These might include reduced documentation time, improved note turnaround times, higher clinician satisfaction scores, or better coding accuracy.
Plan for Integration and Security: A thorough AI requirements analysis is crucial. Work closely with your IT department and the vendor to ensure the scribe integrates smoothly with your EHR and meets all HIPAA compliance and data security standards. This step is non-negotiable and foundational to a safe implementation.
Your Strategic Partner in AI Adoption
Navigating this complex landscape of vendors, pilots, and implementation strategies can be daunting. The selection and deployment process for crucial tools like an AI medical scribe is a significant undertaking. A misstep can lead to wasted resources, frustrated clinicians, and a failed project. This is where strategic guidance becomes indispensable.
Partnering with an expert can de-risk your investment and accelerate your path to value. At Ekipa AI, we specialize in helping organizations move from an initial idea to a fully integrated and adopted AI solution. Our AI strategy consulting services can help you build a Custom AI Strategy report that aligns the technology with your specific clinical and business goals. We guide you through the entire AI Product Development Workflow, ensuring your chosen scribe becomes a true asset, not another administrative hurdle. By leveraging our expertise, you can confidently select and implement the best AI medical scribe for your needs, freeing your clinicians to focus on what matters most: patient care. To see how we've helped others, explore our real-world use cases and connect with our expert team.
Frequently Asked Questions (FAQ)
What is an AI medical scribe?
An AI medical scribe is a software tool that uses artificial intelligence, primarily natural language processing (NLP) and speech recognition, to listen to conversations between clinicians and patients. It automatically transcribes, summarizes, and structures this conversation into a clinical note, which can then be reviewed by the clinician and entered into an Electronic Health Record (EHR).
How does an AI scribe improve a clinician's workflow?
The primary benefit is a significant reduction in administrative burden. By automating the note-taking process, AI scribes can save clinicians 1-2 hours of documentation time per day. This allows them to focus more on the patient during the visit, reduce after-hours charting (pajama time), and ultimately helps combat physician burnout.
Are AI medical scribes HIPAA compliant?
Reputable AI medical scribe vendors are designed to be HIPAA compliant. They use secure data encryption, follow strict access controls, and sign Business Associate Agreements (BAAs) with healthcare organizations. However, it is crucial for any practice to verify a vendor's compliance certifications (like SOC 2) and security protocols before implementation.
Do AI scribes work with any EHR system?
Compatibility varies. Some solutions, like Nuance DAX Copilot and Abridge, offer deep, native integrations with specific EHRs like Epic. Others, like 3M's offerings, boast broad compatibility with hundreds of systems. Lighter, self-service tools like Nabla and Freed often work on a copy-paste basis, making them EHR-agnostic but less integrated.
How accurate are AI medical scribes?
Accuracy has improved dramatically and is a key competitive differentiator. Most leading platforms achieve high levels of accuracy in transcribing and structuring notes. However, they are designed as clinical assistants, not replacements. The final note always requires review and sign-off by the licensed clinician to ensure 100% accuracy and clinical appropriateness.
Ready to transform your clinical documentation workflow but unsure where to start? Let Ekipa AI be your guide in navigating the complex AI vendor landscape. We help you select, pilot, and implement the perfect AI scribe solution tailored to your practice’s unique needs, ensuring a smooth transition and a powerful return on investment. Connect with our expert team today to learn more.



