Transforming Medicine with AI and Machine Learning in Healthcare
Explore how AI and machine learning in healthcare are boosting patient care, diagnostics, and operational efficiency. Discover real-world impacts today.
AI and machine learning in healthcare aren't science fiction anymore. They've become practical, powerful tools that are actively changing how we deliver patient care. Think of them as incredibly smart assistants for doctors and nurses, capable of sifting through massive amounts of complex data to improve diagnoses, personalize treatments, and make hospitals run more efficiently. This isn't some far-off future; it's a new standard of care that's taking shape right now.
The New Standard of Care in Modern Medicine

Bringing AI and machine learning in healthcare into the clinic represents a real shift in how medicine works. It's not about replacing clinicians. Instead, this technology enhances the skills of doctors and nurses, acting like a highly specialized clinical assistant. It's brilliant at processing huge datasets—from medical images and lab results to patient histories—on a scale no human could ever manage.
This capability frees up medical professionals to focus on what they do best: applying critical thinking, connecting with patients, and delivering compassionate care. It creates a powerful partnership between human experience and machine intelligence, which is exactly what we need to tackle today's biggest healthcare challenges.
Augmenting Human Expertise
The challenges we face in global healthcare are massive. Around 4.5 billion people can't get the essential health services they need, and we're facing a projected shortage of 11 million health workers by 2030. Technology has to be part of the solution. AI-powered tools are uniquely suited to help bridge this gap by making healthcare more efficient, affordable, and effective for everyone. You can find more insights on how AI is transforming global health.
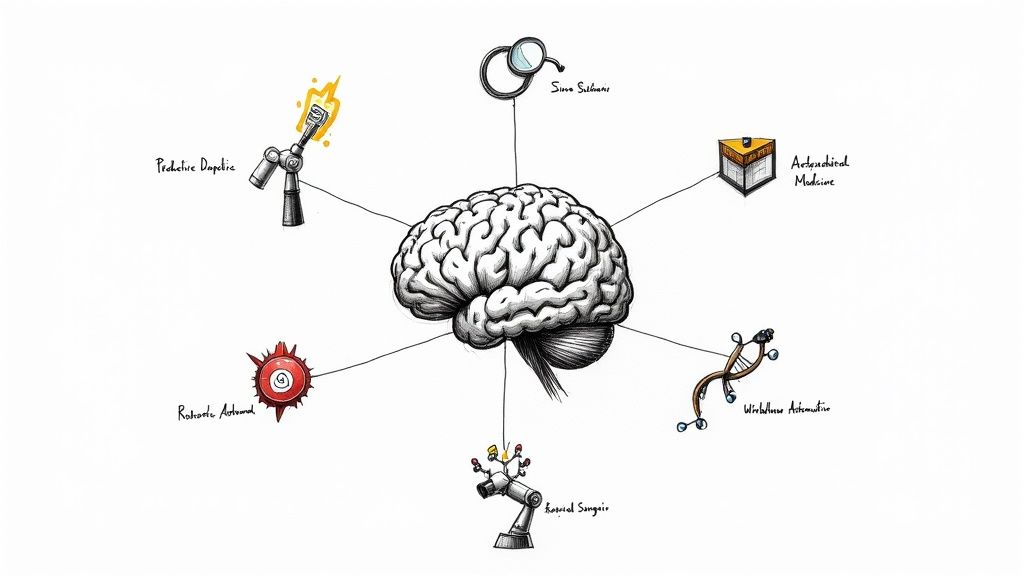
This whole movement is about building systems that are more proactive and efficient. In this guide, we'll dive into three key areas where these tools are making a huge difference:
- Smarter Diagnostics: AI algorithms can spot subtle patterns in X-rays, MRIs, and other medical data that the human eye might miss, leading to earlier, more accurate diagnoses for diseases like cancer.
- Personalized Medicine: By analyzing a person's genetic makeup and other unique factors, machine learning can help design treatment plans that are tailor-made for the individual, often leading to better results with fewer side effects.
- Operational Excellence: From automating tedious paperwork to optimizing hospital bed schedules, AI is cleaning up the backend processes that keep healthcare facilities running, so clinicians can spend more time with patients.
Understanding this shift isn't optional anymore. It's essential for everyone in the healthcare world—from hospital CEOs and frontline doctors to the patients themselves.
Adopting this new standard requires a clear plan and a smart approach. When integrated properly, AI Solutions can cut down on diagnostic errors, speed up medical research, and bring quality care to more people. This guide will give you a complete picture of how these technologies work, where they're being used today, the benefits they offer, and the practical steps to get them implemented successfully.
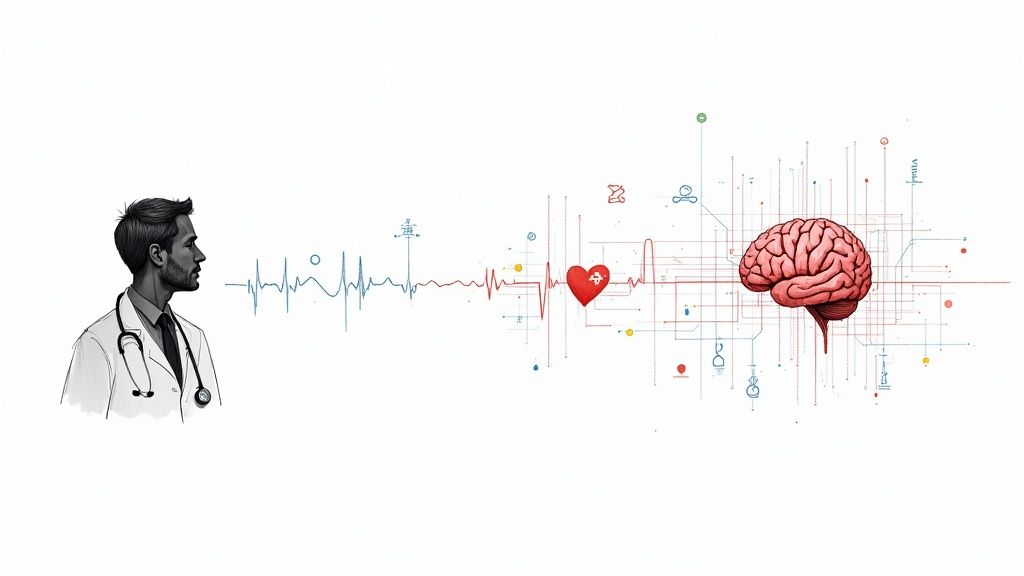
How AI Learns to Think Like a Clinician
To really get a handle on AI and machine learning in healthcare, it helps to stop thinking of it as a magic box. Instead, picture it as a system that learns, almost exactly like a medical resident on their journey to becoming an expert.
At a high level, AI is just the big idea of making machines smart. Machine learning is how we actually do it—we train algorithms on mountains of data, letting them get better and better on their own without someone having to code every single rule.
This whole process looks a lot like a clinician's training. A new resident starts with textbooks and protocols, which is a very structured, rule-based way to learn. AI models start in a similar way, through a process called supervised learning. We feed an algorithm thousands of medical images, each one meticulously labeled "cancerous" or "benign." By poring over these examples, the AI learns to connect specific visual patterns to the correct diagnosis, just as a resident memorizes diagnostic criteria.
From Textbooks to Intuition
Once a resident has the basics down, they start building real clinical intuition. How? By seeing patterns across thousands of actual patient cases. This is where unsupervised learning enters the picture for AI.
With this method, we give the algorithm a huge dataset with no labels at all—just raw patient records or jumbled genetic sequences. Its job is to find hidden structures and connections all by itself. It might uncover a brand-new patient subgroup that responds uniquely to a drug or spot a subtle link between a lifestyle habit and a disease that human analysts completely missed. This is how AI graduates from simply knowing the textbook to generating genuinely new insights.
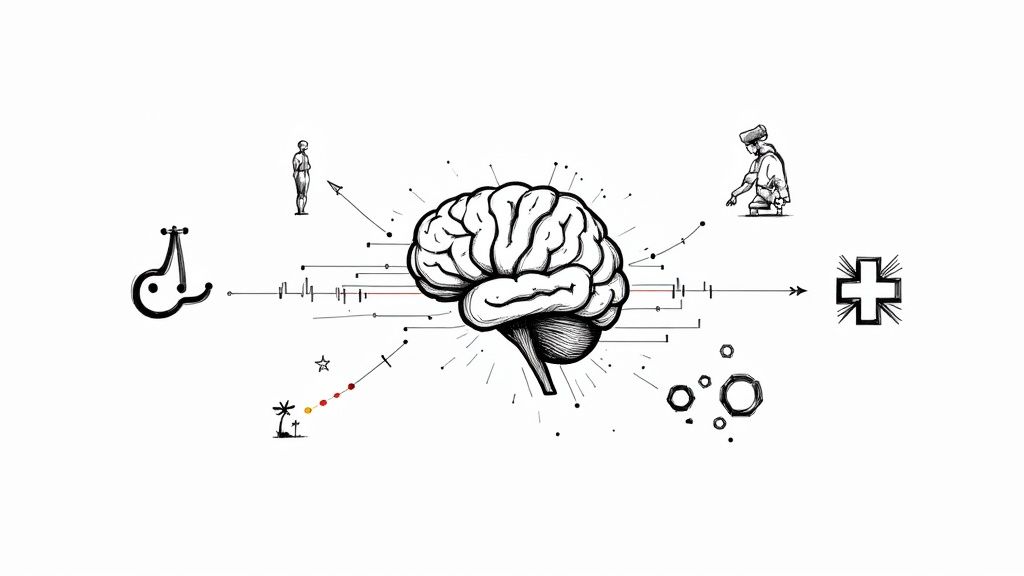
The infographic below really brings this learning process to life, showing how these different AI methods build on each other to create a system with sharp, clinician-like analytical skills.
As you can see, the combination of structured "textbook" learning and intuitive pattern-finding is what creates such a powerful analytical engine.
The Power of Deep Learning
The most sophisticated version of this is deep learning. It's a type of machine learning that mimics the structure of the human brain's neural networks.
Deep learning models are incredible at processing messy, complex information, like the subtle tone shifts in a patient's voice or the microscopic details in a high-resolution MRI. Researchers at Penn Medicine actually built a tool using this approach that can spot cancer cells totally invisible to the human eye.
These systems are trained on datasets so massive they can pick out patterns with a precision that goes beyond human ability. This is the technology behind the most advanced diagnostic tools, outbreak prediction models, and personalized treatment plans. For instance, a purpose-built tool like a clinic AI assistant can apply these same principles to streamline patient communication and administrative work, giving staff more time for hands-on care.
By weaving together supervised, unsupervised, and deep learning, AI and machine learning in healthcare builds a system that doesn't just know what's in the medical books. It can also find new patterns and continuously sharpen its "clinical judgment" with every new piece of data it sees. This makes it an amazing partner for medical professionals, helping them elevate their expertise and deliver better care.
Five Ways AI Is Reshaping Patient Outcomes
The real power of AI and machine learning in healthcare isn't just theory; it’s happening right now in clinics and hospitals. We're seeing these technologies deliver better, faster, and more accurate medical care every day. You can explore many real-world use cases to see this in action.
From spotting diseases years before symptoms show up to crafting treatments based on someone's unique DNA, AI is fundamentally changing what it means to be a patient. Here are five of the most significant ways this shift is taking place.
1. Predictive Diagnostics and Early Detection
One of AI's biggest strengths is its ability to see what the human eye might miss. It can analyze medical images—like X-rays, CT scans, and MRIs—with an almost superhuman level of detail.
Think about it: an AI model, trained on millions of past scans, can pick up on subtle patterns that signal the earliest signs of diseases like cancer. It might flag a tiny, suspicious cluster of cells on a mammogram that would otherwise go unnoticed, leading to life-saving early intervention. This moves healthcare from being reactive to proactive, catching problems before they become crises.
2. Personalized Treatment Plans
The days of "one-size-fits-all" medicine are numbered. AI is pushing us into an era of truly personalized care, where doctors can design therapies based on a patient's specific genetic makeup, lifestyle, and history.
By sifting through massive genomic datasets, machine learning can predict how someone might respond to a particular drug. This helps an oncologist choose the most effective chemotherapy with the fewest side effects, making cancer treatment a much more targeted process.
This level of customization ensures patients get the best possible care from day one, cutting out the painful trial-and-error process that can waste precious time. A targeted approach means better outcomes and a higher quality of life.
3. Accelerated Drug Discovery and Research
Developing new medicines is a notoriously slow and expensive journey. It can take over a decade and cost billions to get a single drug from the lab to the pharmacy. AI is hitting the fast-forward button on this entire process.
Machine learning algorithms can simulate how molecules interact, predict which new compounds are most likely to work, and identify promising drug candidates in a tiny fraction of the usual time. They can also analyze clinical trial data to pinpoint the ideal patient groups for new treatments. This means life-saving therapies can reach the people who need them much, much faster. Exploring AI in the healthcare industry reveals just how deep this impact goes.
4. Intelligent Workflow Automation
Burnout among clinicians is a serious problem, and a lot of it comes from the mountain of administrative work. AI is offering some much-needed relief by automating the repetitive tasks that don't involve direct patient care.
In fact, the shift is already well underway. It's estimated that by 2025, around 80% of U.S. hospitals will be using AI to improve both patient care and their own operations. This includes tools that listen to and transcribe doctor-patient conversations into medical notes, giving clinicians back hours of their day.
Intelligent automation systems also tackle other critical jobs:
- Patient Scheduling: Optimizing calendars to cut down on wait times and help clinics see more patients.
- Medical Billing: Catching errors to reduce claim denials and improve the hospital’s financial stability.
- Inventory Management: Predicting when supplies will run low to make sure critical equipment is always on hand.
By offloading these tasks, AI lets doctors and nurses get back to what they do best: focusing on their patients.
5. Robotic-Assisted Surgery
In the operating room, AI is the surgeon's ultimate co-pilot. By pairing robotics with intelligent software, surgeons can perform incredibly complex procedures with more precision and through smaller incisions than ever before.
During an operation, AI algorithms can provide real-time feedback, highlighting critical nerves or blood vessels to avoid. This blend of human expertise and machine accuracy leads to huge benefits for the patient:
- Less blood loss during surgery.
- Reduced pain and scarring afterward.
- A much faster recovery time.
This combination of skill and technology is setting a new standard for surgical excellence, making difficult operations safer and more effective.
The Measurable Benefits of Integrating AI Systems
When we talk about AI and machine learning in healthcare, we're not just discussing futuristic concepts. We're talking about real, tangible results that are changing how healthcare is delivered today. The reason investment in this technology is exploding—projected to fly past $120 billion by 2028—is simple: it works. It adds real value across the board, from the operating room to the back office.
These benefits really boil down to three core areas: improving patient outcomes, making daily operations run smoother, and bringing down the staggering costs of care. This isn't just about adopting new tech for its own sake. It’s a direct response to the immense pressures on the industry. A recent survey of healthcare leaders found that 86% are already using AI to handle growing patient numbers, cut down on wait times, and support overworked staff. If you're interested, there's more data on these AI in healthcare statistics.
Enhancing Patient Outcomes
Let's start with what matters most: patient health. AI's ability to analyze medical data at a speed and scale no human can match is a game-changer for diagnostics. In fields like radiology, for example, algorithms trained on millions of images can spot the faint, early signs of disease that might otherwise go unnoticed. This means catching problems sooner and starting treatment when it's most effective.
It's also about making medicine more personal. Machine learning can look at a patient's unique genetic makeup, lifestyle, and medical history to predict how they'll respond to different drugs. This helps doctors move away from a one-size-fits-all approach and choose the best therapy right from the start, which often means fewer side effects and a better chance of recovery. It’s a fundamental shift from just reacting to sickness to proactively managing health.
Boosting Operational Efficiency
Anyone who's worked in a hospital knows they are incredibly complex environments. AI brings a much-needed dose of efficiency by automating the mountain of routine administrative tasks that bog clinicians down. A great example of this is Intelligent Document Processing (IDP), which automates the handling of patient records, claims, and referrals.
By automating repetitive workflows, AI liberates clinicians from administrative burdens, allowing them to dedicate more time and energy to direct patient care. This not only improves the quality of care but also helps combat staff burnout.
AI also smooths out the bumps in hospital logistics. It can predict patient admission spikes, create smarter operating room schedules, and make sure staff and equipment are where they need to be, when they need to be there. This kind of intelligent workflow automation means less time spent waiting and a better experience for everyone involved.
Lowering Healthcare Costs
When you improve patient outcomes and make operations more efficient, the cost savings naturally follow. Predictive analytics is a huge part of this. By identifying patients at a high risk of being readmitted or developing complications after surgery, providers can step in with preventative care. This proactive approach helps avoid expensive emergency treatments later on.
AI also helps on the research front by making the drug discovery process faster and less expensive. It can even optimize hospital supply chains to reduce waste. Every dollar saved on an unnecessary procedure or a streamlined process is a dollar that can be reinvested into patient care. Our own AI strategy consulting is focused on helping organizations find exactly these kinds of high-impact opportunities.
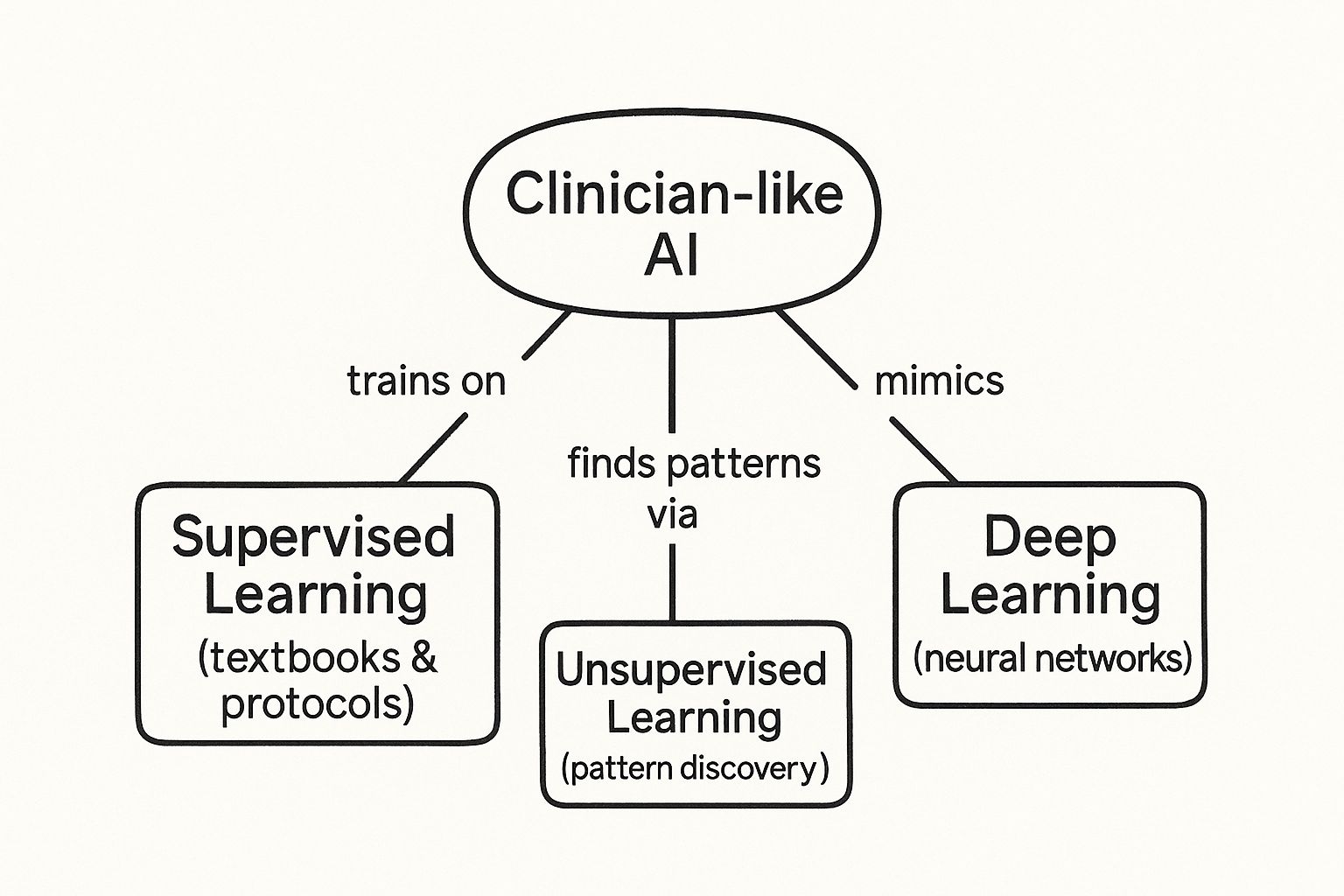
To pull this all together, here’s a quick summary of the key benefits AI and machine learning bring to the table.
Key Benefits of AI and Machine Learning in Healthcare
This table provides a snapshot of the primary advantages gained by weaving AI technologies into the fabric of both clinical and administrative healthcare functions.
Benefit Area Description Example Application
Improved Patient Outcomes
Enhanced diagnostic accuracy, personalized treatment plans, and proactive health monitoring lead to better patient results.
AI algorithms detecting early-stage cancer in mammograms with higher accuracy than human review.
Enhanced Operational Efficiency
Automation of repetitive administrative tasks frees up staff time, streamlines workflows, and optimizes resource allocation.
AI-powered scheduling systems that reduce patient wait times and optimize operating room usage.
Reduced Healthcare Costs
Predictive analytics can prevent costly complications, reduce hospital readmissions, and streamline the drug discovery process.
Machine learning models identifying at-risk patients for post-operative complications, enabling preventative care.
Accelerated Medical Research
AI can analyze vast datasets to identify patterns and insights, dramatically speeding up clinical trials and drug development.
AI platforms analyzing genomic data to identify potential new drug targets in a fraction of the traditional time.
From faster diagnoses to more efficient hospitals, the impact is clear. Each of these benefits reinforces the others, creating a powerful cycle of improvement that is reshaping what's possible in medicine.
Navigating the Challenges of AI Implementation

As promising as it is, bringing AI and machine learning in healthcare to life isn't as simple as flipping a switch. You can’t just plug it in and expect magic. Anyone who has been through this process knows that a clear-eyed view of the hurdles is non-negotiable. Getting AI working effectively in a real clinical setting means tackling everything from patient data privacy to the sticker shock of new systems.
Organizations that get ahead of these challenges are the ones that succeed. It takes a solid, proactive strategy to weave AI into the healthcare fabric ethically and effectively—one that actually delivers on the hype without creating new problems.
Protecting Patient Data and Ensuring Compliance
In medicine, nothing is more sacred than patient data. AI systems have to live within the strict confines of privacy laws like HIPAA, which dictate every aspect of handling protected health information (PHI). This isn't just about checking a legal box; it's about earning and keeping the trust of every single patient.
A big question is how we train these models without exposing sensitive information. One of the most practical answers emerging is federated learning. It's a clever approach where an AI model learns from data across multiple hospitals without that data ever leaving the premises. The model trains on each hospital's local, secure server, and only the anonymous learnings—not the patient files—are sent back to improve the main algorithm. This keeps privacy locked down while allowing for powerful, collaborative AI development.
Mitigating Algorithmic Bias
An AI is a reflection of the data it learns from. If that data is skewed, the AI will be, too. An algorithm trained on data from just one demographic might perform poorly for others, and that's a serious problem. It could easily make existing health disparities even worse.
The only way to combat this is with a deliberate focus on data diversity. This means actively building datasets that represent the true spectrum of patients—spanning different ages, ethnicities, genders, and backgrounds. But it doesn't stop there. We need constant vigilance through auditing and transparency. Algorithms must be tested regularly for fairness to ensure they work for everyone, and this is where expert AI strategy consulting can be invaluable.
Managing High Implementation Costs
Rolling out an AI system is a major financial undertaking. The price tag goes far beyond the software license. You have to account for:
- Infrastructure Upgrades: These complex algorithms need some serious computing power.
- System Integration: The new tools have to talk to your existing Electronic Health Record (EHR) systems, which is often easier said than done.
- Staff Training: Doctors, nurses, and admin staff all need to understand how to work with the new technology.
The initial investment can feel steep. But the real story is the long-term return on investment (ROI)—found in greater efficiency, fewer errors, and ultimately, better patient care.
The smartest way forward is often to start small. Pick one high-impact area, like automating a tedious administrative task, and run a pilot project. This lets you prove the value of AI on a smaller scale, making it much easier to get the buy-in needed for a wider rollout. It turns a massive, intimidating project into a series of smaller, achievable wins.
A Practical Roadmap for Bringing AI into Your Healthcare Practice
Putting AI and machine learning to work in a healthcare setting isn't just about plugging in new software. It’s a strategic move that needs a clear, practical plan. Think of this as your roadmap, guiding you from an initial idea to a real-world solution that actually makes a difference.
Start with a Single, High-Impact Problem
The first step, and honestly the most important, is to pick the right problem to solve. Instead of trying to overhaul everything at once, focus on a specific, measurable challenge.
What does that look like? Maybe it’s tackling the frustratingly high rate of patient no-shows. It could be about accelerating the time it takes to analyze diagnostic images or even just making the claims process less of a headache. The key is to narrow your focus. By zeroing in on one well-defined issue, you can show a clear win much faster.
Get the Right People and Your Data in Order
With a clear goal in mind, it's time to build your team. This isn't just a job for the IT department. You need a mix of experts at the table: clinicians who live the daily workflow, IT pros who understand your current systems, data scientists to work their magic, and leaders who can champion the project. This blend is what makes a solution both technically sound and genuinely useful in a clinical setting.
At the same time, you have to get your data house in order. An AI model is completely dependent on the data it learns from. That means taking a hard look at the quality, accessibility, and security of your data. Making sure it’s clean, standardized, and compliant with all privacy regulations isn't just a box to check—it's the foundation of the entire project.
Find the Right Partners and Prove the Concept
Choosing a technology partner is a make-or-break decision. You need someone who gets both AI and the unique, complex world of medicine. Look for a team with real, proven experience in healthcare who can help you navigate the technical and regulatory landscape. As you think about specific tools, looking at reviews of things like the best WordPress chatbot plugins for healthcare can give you a feel for what’s out there.
Once your team, data, and partners are ready, it's time to launch a pilot project. A pilot is your real-world test. It lets you try out the solution on a smaller scale, measure its actual impact, and get crucial buy-in from the people who will use it every day. A successful pilot gives you the hard evidence you need to make the case for a wider rollout.
If you’re wondering where to start, our team can help you with a Custom AI Strategy report to find the best opportunities for your organization.
We've built a structured AI Product Development Workflow specifically to guide organizations like yours through every stage—from the initial idea to full-scale implementation support. Adopting AI is a big step, but with a deliberate, phase-by-phase approach, you can translate powerful technology into real, measurable improvements for your patients and your practice.
Frequently Asked Questions
It's natural to have questions about how technologies like AI and machine learning will really affect healthcare. The potential is massive, but so are the concerns about safety, jobs, and privacy. Let's tackle some of the most common questions people ask.
Will AI Replace Doctors and Other Healthcare Professionals?
The short answer is no. The real goal is to augment human expertise, not replace it. Think of AI as an incredibly powerful assistant.
AI is fantastic at sifting through mountains of data and spotting patterns that would take a human days to find. This frees up doctors and nurses to do what they do best: apply critical thinking, connect with patients, and deliver compassionate, hands-on care. It's a partnership, not a replacement.
How Is Patient Data Kept Safe and Private When Using AI Systems?
This is non-negotiable. Protecting patient data is paramount, and any AI system used in healthcare must adhere to ironclad regulations like HIPAA.
Several layers of security are used to make this happen. Data is often anonymized, meaning all personal identifiers are stripped away. It's also encrypted and stored in secure environments with strict access controls. An even more advanced method is called federated learning, where the AI model learns from data across multiple hospitals without the sensitive information ever leaving the source. This is a game-changer for privacy.
What Is the Biggest Barrier to AI Adoption in Smaller Clinics or Hospitals?
For smaller practices, the biggest hurdles are usually the upfront cost and not having a team of tech experts on staff. Building or buying an AI system and getting it to talk to your existing electronic health records (EHRs) can be a significant investment.
The good news is that this is changing. The emergence of "AI Automation as a Service" and other cloud-based platforms is leveling the playing field. These models allow smaller organizations to tap into powerful AI capabilities without a massive initial outlay. A great way to start is by picking one specific problem to solve, like automating an internal tooling process. It’s a practical first step that delivers real value and builds momentum for bigger things. As we explored in our AI adoption guide, it all starts with a solid plan and the right partner.
How does AI handle the complexity and variability of human health?
AI models, particularly those using deep learning, are specifically designed to handle complex and variable data. They are trained on vast and diverse datasets that include a wide range of patient profiles, symptoms, and outcomes. This allows the AI to learn the subtle nuances and variations in human health that might be missed by traditional statistical methods. The system continuously learns and refines its understanding with new data, making it adaptable to the complexities of medicine.
What ethical considerations are most important for AI in healthcare?
Beyond data privacy, key ethical considerations include transparency, accountability, and fairness. It's crucial that AI systems are "explainable," meaning clinicians can understand how the AI reached a particular conclusion. Accountability is about defining who is responsible if an AI makes a mistake—the developer, the hospital, or the clinician? Finally, fairness means ensuring that AI tools do not perpetuate or worsen existing health disparities, which requires constant auditing for bias.
Can AI help with mental healthcare?
Absolutely. AI is already being used in mental health to analyze speech patterns, text messages, and even facial expressions to detect early signs of depression, anxiety, or other conditions. Chatbots can provide immediate, accessible support and cognitive behavioral therapy exercises. While not a replacement for human therapists, these AI tools for business and individuals offer valuable resources for mental wellness and can help bridge gaps in care.
Ready to see what AI can do for your healthcare operations? The expert team at Ekipa is here to help you build a clear, actionable strategy. Explore our AI Solutions or get to know our expert team to get started.