Artificial Intelligence in Medical Imaging: A Practical Guide
Discover how artificial intelligence in medical imaging is transforming diagnostics with key applications, benefits, and strategies to implement successfully.
Picture this: a radiologist, tasked with interpreting hundreds of complex scans in a single day. Each scan holds a story, and a tiny, overlooked detail could completely alter a patient's life. This is the reality where artificial intelligence in medical imaging is making a real difference—not as a replacement for human experts, but as a highly perceptive co-pilot. AI gives clinicians the ability to see more, see it faster, and with greater precision in everything from X-rays to CTs and MRIs.
How AI Is Reshaping Medical Imaging
At its core, artificial intelligence in medical imaging acts as a second set of incredibly sharp eyes for healthcare professionals. It uses powerful algorithms to sift through the visual data in medical scans, hunting for patterns and anomalies that are often too subtle or time-consuming for the human eye to catch on its own. The goal isn't to take over, but to enhance a clinician's judgment with massive computational power.
It's almost like giving a radiologist a set of digital super-senses. These AI algorithms are trained on immense, diverse libraries of medical images, learning to tell the difference between healthy anatomy and the earliest signs of disease with impressive accuracy. Once trained, they can automatically flag suspicious areas, measure structures with perfect consistency, and even help prioritize the most urgent cases. The result is a diagnostic workflow that's both more efficient and more precise.
A Partnership Between Human and Machine
The true power here comes from the synergy between human experience and machine precision. A seasoned clinician brings years of training, a deep understanding of the patient's unique context, and the kind of nuanced reasoning that only comes from experience. The AI brings tireless, objective pattern recognition and quantitative analysis to the table.
This collaboration directly addresses some of the biggest hurdles in modern healthcare:
- Tackling Massive Workloads: The sheer volume of imaging studies is overwhelming. AI helps manage this load, reducing the risk of burnout and ensuring every scan gets the attention it deserves in a timely manner.
- Boosting Diagnostic Consistency: By offering an objective analysis, AI helps standardize interpretations, reducing variability between different clinicians or even different hospitals.
- Catching Disease Earlier: Often, these algorithms can spot minuscule changes that signal the very beginning of a disease, which can dramatically improve patient outcomes.
The diagram below gives you a clear picture of this partnership in action, showing how a radiologist might work with a scan that has AI-powered highlights.
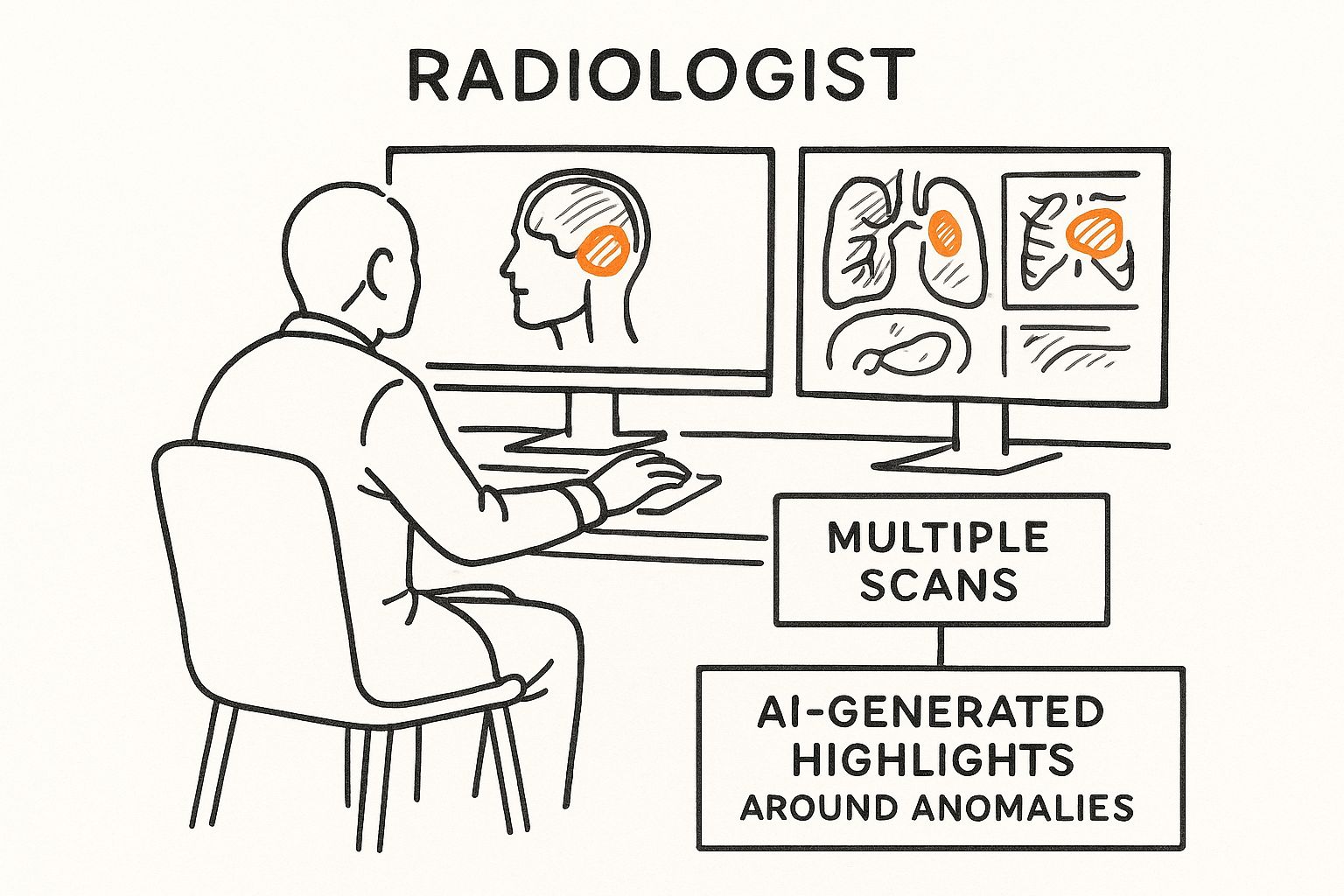
As you can see, the AI acts as a smart filter, guiding the radiologist's attention straight to the areas that matter most, making their entire process smoother and more focused.
More Than Just Pixel Analysis
But the influence of AI doesn't stop at the image itself. It's also improving the entire operational workflow that surrounds medical imaging. For instance, AI is making huge strides in managing the mountains of related patient data and clinical reports through advanced and accurate AI document processing. This creates a much more connected and intelligent process, from the moment a patient is scanned to the final report. Our work in the healthcare sector is centered on building these kinds of cohesive, intelligent systems.
By speeding up analysis and sharpening diagnostic accuracy, AI is fundamentally making healthcare smarter and more effective for everyone involved. This guide will take you through the key technologies, real-world applications, and strategic thinking behind this powerful alliance.
Understanding The Core AI Technologies
You don’t need a degree in computer science to grasp the basics of how AI works in medical imaging. Think of it this way: how would you teach a computer to recognize a cat? You wouldn't try to program a long list of rules like "has pointy ears" or "has a long tail." Instead, you'd simply show it thousands of pictures of cats until it started to figure out the patterns on its own.
That’s the core idea behind Machine Learning (ML). It’s a field of AI where systems learn directly from data instead of being explicitly told what to do. This approach is the bedrock for nearly all modern AI, and understanding the fundamentals of Machine Learning is the first step to seeing its power in a clinical setting.

Deep Learning: The Brain of The Operation
Deep Learning (DL) takes this concept a step further. It's a more advanced type of machine learning that uses something called a "neural network," which is loosely modeled on the web of neurons in our own brains. These networks have multiple layers, which allows them to learn incredibly subtle and complex patterns from enormous datasets—far more than any human ever could.
Going back to our cat example, a deep learning model doesn’t just see a generic "cat." Its layers learn to identify specific features like whisker texture, eye shape, and fur patterns, building a much richer understanding. This is precisely why it’s so powerful for analyzing medical scans, which are dense with intricate details. The market for this technology has grown dramatically, starting from around USD 14.16 billion and is expected to climb to USD 21.78 billion. Currently, lung-related imaging leads the pack with a 22% market share, but oncology applications are catching up fast, with a projected growth rate of over 30% CAGR.
Convolutional Neural Networks: The AI’s Eyes
Within the world of deep learning, there's a special type of network that is an absolute natural at image analysis: the Convolutional Neural Network (CNN). You can think of a CNN as the AI's visual cortex. It processes images much like our own eyes do, starting by identifying small, simple features like edges and textures.
Then, it combines those simple features to recognize larger, more complex objects, like organs, blood vessels, or tumors. This makes CNNs the true workhorses of AI in medical imaging. They excel at understanding the spatial relationships in an image—the very same skill a radiologist relies on when interpreting a scan.
To give you a better sense of how these different technologies fit together, here's a quick breakdown of the key techniques and what they do.
Table: Key AI Techniques and Their Roles in Medical Imaging
| AI Technique | Primary Function in Medical Imaging | Example Application |
|---|---|---|
| Machine Learning (ML) | Broad framework for learning from data to make predictions or decisions. | A model that predicts a patient's risk of disease based on their clinical data and basic image features. |
| Deep Learning (DL) | Uses multi-layered neural networks to find complex, non-obvious patterns in large datasets. | An algorithm that identifies diabetic retinopathy from retinal fundus images by analyzing subtle vascular changes. |
| Convolutional Neural Networks (CNNs) | A specialized type of DL designed specifically to process and analyze visual data like scans and X-rays. | A system that detects and localizes potential cancerous nodules on a CT scan of the lungs. |
This table shows how each technology builds on the last, from the broad principles of ML to the highly specialized capabilities of CNNs, which are essential for practical clinical use.
The Three Core Tasks of AI in Imaging
At the end of the day, these sophisticated technologies are trained to perform three essential tasks that give clinicians new superpowers.
Image Classification: This is the most straightforward task. It answers a simple "what is this?" question. For instance, it can look at a skin lesion and classify it as likely benign or malignant.
Object Detection: Taking it a step further, object detection answers "where is it?" It draws a box around a specific area of interest, like highlighting the exact location of a tiny nodule on a chest X-ray that might otherwise be missed.
Image Segmentation: This is the most granular and precise function. It answers the question, "what are its exact boundaries?" The AI carefully outlines the precise shape of a tumor or organ, pixel by pixel. This level of detail is critical for planning surgery or accurately measuring tumor volume to see if a treatment is working.
By mastering these three tasks—classification, detection, and segmentation—AI models can automate tedious measurements, flag suspicious findings, and provide quantitative data that was previously difficult to obtain.
These core technologies are the engines driving the powerful AI tools that are already making a difference in healthcare. Now that we understand how they work, let's look at how they are being applied in the real world to improve patient care.
AI in Action: Real-World Diagnostic Applications
Now that we have a handle on the technology, let's see where the rubber meets the road. The real story of artificial intelligence in medical imaging isn't in the code; it's in the clinic, where these tools are already changing how doctors diagnose complex diseases.
This isn't some far-off future. It's happening right now. The U.S. Food and Drug Administration (FDA) has already cleared hundreds of AI-powered medical imaging tools, a massive jump from just a few years ago. That rapid approval shows a growing confidence in the technology. In fact, about two-thirds of U.S. radiology departments are already using some form of AI, primarily for critical conditions like stroke, breast cancer, and detecting lung nodules.
A New Ally in Oncology
When it comes to cancer, catching it early can make all the difference. AI is quickly becoming a crucial partner for oncologists, helping them spot subtle signs of malignancy that the human eye might miss.
Take mammography, for example. An AI model trained on millions of past scans can flag tiny calcifications or distortions in breast tissue—often the earliest signs of cancer. It works like a tireless second set of eyes, reducing the risk of an oversight and letting radiologists zero in on the most suspicious cases. This is exactly the kind of challenge we built our AI-powered diagnostic tool, Diagnoo, to solve. You can learn more about how it helps with the early detection of breast cancer https://www.ekipa.ai/products/diagnoo.
This same idea is being applied across different types of cancer:
- Lung Cancer: AI analyzes CT scans to find and measure pulmonary nodules with incredible precision, tracking their growth over time to better gauge risk.
- Prostate Cancer: By reviewing MRI scans, AI can outline the prostate gland and highlight suspicious areas, helping to guide more accurate biopsies.
This isn't just about finding cancer; it's about finding it sooner, opening up more effective treatment options.
Sharpening Insights in Neurology
The brain is a universe of complexity, and interpreting neurological scans takes years of specialized training. AI is giving neurologists powerful new tools to measure brain health and spot signs of disease earlier than ever before.
In neurology, AI's strength is its ability to see what we can't—to detect and quantify tiny changes in brain volume or structure over time that are almost impossible for a person to track consistently.
For instance, when a patient is being evaluated for Alzheimer's disease, an AI can analyze a series of MRI scans to precisely measure the rate of shrinkage in the hippocampus, a key indicator of the disease. This gives doctors objective data to back up their diagnosis. In stroke care, speed is everything. AI algorithms can instantly analyze CT scans to find brain bleeds or blockages, empowering emergency teams to make critical treatment decisions just minutes after a patient arrives.
Enhancing Precision in Cardiology
Heart disease is still a major global health issue, and imaging is at the core of how we diagnose and manage it. AI is helping to make cardiac imaging analysis faster and much more reliable. A great example is in the analysis of echocardiograms—ultrasound videos of the beating heart.
Traditionally, measuring heart function, like the ejection fraction, required a cardiologist to manually trace the heart's chambers on a screen. This is slow and can vary from one doctor to another. AI automates it completely. An algorithm can watch the video, outline the chambers, and calculate the ejection fraction in seconds, delivering the same, consistent result every single time. This kind of workflow automation frees up cardiologists from tedious tasks so they can spend more valuable time with their patients.
Why Bother with AI? The Strategic Payoffs
Bringing artificial intelligence into medical imaging isn't just about getting a new piece of tech. When you look at AI as a strategic asset—not just another tool—you start to see its real power to elevate clinical quality, speed up operations, and improve patient care.
These benefits fall into three main buckets, each creating serious value for any healthcare organization. It’s all about making the entire system smarter, more responsive, and more reliable. Let's break down what this actually looks like for diagnostics, daily workflows, and patient health.
Sharpening Diagnostic Accuracy
The most immediate win is a big one: better diagnostic accuracy. Think of an AI model as a tireless second reader, scanning every image for patterns so subtle or faint that even a seasoned expert might miss them on a busy day. This alone helps chip away at diagnostic errors, a persistent problem in any high-volume imaging department.
AI flags potential issues, drawing a clinician's eye straight to areas needing a closer look. It’s this blend of human expertise and machine perception that leads to earlier, more dependable diagnoses. In fields like oncology or neurology, catching something early can change everything for a patient. It's the difference between reacting to a problem and getting ahead of it.
Making the Day-to-Day Run Smoother
Beyond just finding things on a scan, AI has a knack for streamlining the work itself. By handling the repetitive, time-consuming tasks, it injects a massive dose of efficiency into the system. This is where workflow automation really shines.
Picture this: an AI system automatically sorts incoming scans, bumping urgent cases to the top of the list for immediate review. Or imagine algorithms that can measure a tumor's volume or a heart's ejection fraction in seconds—a task that would otherwise eat up a specialist's valuable time. This isn't science fiction; these are practical uses of AI Automation as a Service happening right now.
By automating these steps, hospitals can fine-tune their internal tooling and let their top clinicians do what they do best. Instead of getting bogged down with manual measurements, they can focus on complex cases, consult with colleagues, and spend more face-to-face time with patients.
Driving Better Patient Outcomes
At the end of the day, it's all about helping patients. And that's where better accuracy and efficiency truly pay off. A faster, more precise diagnosis means treatment can start sooner, often when it stands the best chance of working.
For instance, a quick AI analysis of a CT scan can help a stroke team make critical, life-saving decisions minutes earlier. In the same way, detecting a tiny cancerous nodule early opens the door to less invasive treatments and a much better long-term outlook for the patient.
This direct line from a technology investment to a person's health is the ultimate ROI. It proves that AI isn't just a cost—it's a strategic investment in the very mission of healthcare.
By embracing robust AI Solutions, organizations are doing more than just a tech upgrade. They're fundamentally improving their ability to deliver care that's high-quality, efficient, and effective. A thoughtful AI strategy consulting approach is the key to making sure these benefits touch every part of the clinical workflow.
Implementing Your AI Medical Imaging Strategy
Moving from theory to practice with AI in medical imaging isn't about just flipping a switch on new software. It's a thoughtful, step-by-step journey that carefully weaves technology into your clinical workflows and organizational goals.
The first, and most important, step is to get specific. A vague goal like "improve diagnostics" won't get you far. A much better target is something like, "reduce the average turnaround time for stroke protocol CT scans by 30%." Picking the right problem to solve is the single most critical decision you'll make. Focus on a high-impact, clearly defined challenge where AI can deliver obvious, measurable value.
Building The Technical Foundation
Once you know what you want to achieve, it's time to lay the groundwork. This is where a lot of great ideas can fall apart if you're not careful. An AI model is only as smart as the data it learns from, which makes data quality and accessibility your absolute top priorities. You need data that is clean, diverse, and properly anonymized—this is non-negotiable for both model accuracy and patient privacy.
The next piece of the puzzle is seamless integration. If an AI tool can't talk to your existing Picture Archiving and Communication System (PACS) or Electronic Health Record (EHR), it’s going to cause more headaches than it solves. The whole point is to make the AI feel like a natural part of the radiologist's world, not some clunky, bolted-on accessory.
Navigating Regulatory And Human Factors
Bringing AI into a clinical setting is about more than just tech; you have to navigate a maze of regulations and, just as importantly, people. Any AI tool used for diagnosis has to meet strict standards, like getting FDA clearance and being fully HIPAA compliant to protect patient data.
Success isn't just about having the best algorithm. It hinges on building trust and making sure the technology fits into the human-centric art of medicine.
At the same time, you can't overlook the human element. Clinicians need solid training, not just on which buttons to click, but on the tool's strengths and, crucially, its limitations. Getting radiologists, IT specialists, and data scientists working together closely is the secret sauce for a smooth rollout and for making the system better over time. Our team offers hands-on implementation support designed to manage these complex interactions and clear the technical hurdles, guiding you from a great idea to a successful clinical tool.
A Global Perspective on AI Adoption
The push for AI in medical imaging is happening everywhere, though some regions are moving faster than others. The North American market was valued at USD 223.8 million and is expected to explode to nearly USD 2.8 billion, growing at a compound annual rate of over 28%. Asia Pacific is actually the fastest-growing region, thanks to increasing healthcare demands and huge leaps in technology.
Globally, hospitals are leading the charge. This shows a major institutional belief in AI's ability to help manage the ever-growing number of diagnostic scans. This trend is well-documented in market analyses from sources like Precedence Research.
A successful implementation brings all these threads together: clear goals, a solid technical base, regulatory diligence, and a collaborative team. To make sure you get it right, a custom AI strategy can provide the detailed, personalized plan you need to turn your vision into a clinical reality.
Where Is AI in Medical Imaging Headed Next?
What we've seen so far with artificial intelligence in medical imaging is really just scratching the surface. The next wave isn't just about spotting anomalies better or faster; it's about looking into the future—predicting outcomes and personalizing care in ways we've only dreamed of. This isn't a story about replacing doctors, but about giving them a crystal ball.
Beyond Diagnosis: The Power of Prediction
One of the most exciting frontiers is predictive analytics. Imagine an AI that doesn’t just identify a tumor on a scan. Instead, it analyzes the tumor's unique characteristics and forecasts its likely growth rate or even predicts how it will respond to specific treatments.
This would be a complete game-changer. Doctors could get ahead of a disease, choosing the most effective therapy from day one instead of relying on trial and error. These are the kinds of powerful, forward-thinking real-world use cases that are on the horizon.
Opening the "Black Box" to Build Trust
As AI models get smarter, they also get more complicated. A doctor can't rely on a recommendation without understanding the 'why' behind it. This is where Explainable AI (XAI) becomes absolutely essential.
XAI techniques are designed to peel back the layers of an algorithm's decision-making process. So, instead of simply circling a suspicious spot on an MRI, an XAI system might show the radiologist the specific pixels that triggered the alert or pull up similar-looking cases from its database. This kind of transparency is the bedrock of clinical trust and a central part of our AI Product Development Workflow.
Ushering in an Era of Truly Personal Medicine
Ultimately, all of this is leading us toward highly personalized medicine. The next generation of AI will be able to detect unique "imaging biomarkers"—subtle patterns in a scan, invisible to the human eye, that are specific to an individual patient’s biology.
These biomarkers will act as a roadmap, guiding doctors to create treatment plans tailored to one person, not just a general diagnosis. We're moving from one-size-fits-all protocols to bespoke strategies, a shift powered by advanced healthcare software development.
The future is a partnership between brilliant medical professionals and intelligent systems. It’s not just about writing better code; it's about having a clear vision for how to integrate this technology thoughtfully. To find out how you can be part of this evolution, connect with our expert team and let's explore what’s possible.
FAQs: Your AI in Medical Imaging Questions Answered
As AI continues to make its way into clinical practice, it’s only natural to have questions. Let's tackle some of the most common ones that come up when discussing artificial intelligence in medical imaging.
Is AI going to replace radiologists?
Not at all. The prevailing view among experts is that AI is here to augment human radiologists, not make them obsolete. Think of it as an incredibly skilled assistant. AI is fantastic at sifting through massive volumes of images to spot patterns or handle tedious, repetitive measurements. This frees up radiologists to do what they do best: apply critical thinking to complex cases, consult with other specialists, and focus on patient care. The end result is a more efficient, effective radiologist.
What are the biggest roadblocks to AI adoption in medical imaging?
Bringing AI into a real-world clinical setting isn't a simple plug-and-play process. The hurdles usually fall into four main categories:
- Data, Data, Data: AI models get smart by learning from vast amounts of high-quality, diverse, and carefully labeled data. Getting access to this data while protecting patient privacy is a major logistical challenge.
- Seamless Integration: New AI tools for business have to talk to the systems you already have, like your Picture Archiving and Communication System (PACS) and Electronic Health Records (EHRs). Without seamless integration, you just create more workflow headaches.
- The Regulatory Maze: Before any AI tool can be used on patients, it needs a green light from regulatory bodies like the FDA. This is a thorough and essential process to guarantee the tool is both safe and effective.
- Building Clinical Trust: You can have the best tool in the world, but if clinicians don't trust it, they won't use it. Building that confidence requires transparent, explainable AI and solid training, which is a key part of what we cover in our AI adoption guide.
How is patient privacy protected when using AI?
This is non-negotiable. Protecting patient data is the top priority and is legally mandated by regulations like HIPAA. The primary method used is data anonymization, where all personal information is completely scrubbed from medical images and records before they're used to train an AI model.
A more advanced and secure technique gaining traction is federated learning. It allows an AI model to learn from data across multiple hospitals without any of that sensitive data ever leaving its original, secure location. This "train-at-the-source" approach ensures the highest level of security and compliance. Responsible AI strategy consulting always builds these privacy-preserving measures into the very foundation of a project, proving that innovation and confidentiality can, and must, coexist.
At Ekipa AI, we guide organizations from the initial idea to real-world, scalable impact. Our work is driven by our passion for solving complex problems with cutting-edge technology. Get to know the people behind the innovation by meeting our expert team. If you're ready to see what AI can do for your practice, get your Custom AI Strategy report today.