AI and Medical Diagnosis Transforming Healthcare
Explore how AI and medical diagnosis are revolutionizing healthcare. This guide explains AI's role in boosting accuracy, speed, and patient outcomes.
When a doctor looks at a medical scan, they see a complex image. An artificial intelligence model, on the other hand, sees millions of data points, searching for subtle patterns that might be invisible to the human eye. This is the new reality of AI and medical diagnosis—a powerful partnership that is already reshaping healthcare.
AI isn't here to replace clinicians. Instead, think of it as a superhuman assistant, augmenting a doctor’s own skills to deliver faster, more accurate diagnoses.
The New Reality of AI in Medical Diagnosis
AI in healthcare isn't some far-off concept anymore; it's being put to work in real clinics and hospitals, saving lives today. The technology fundamentally changes how medical professionals tackle diagnostics, adding a new layer of data-driven insight to their years of experience. It’s like giving a seasoned detective a team of tireless analysts who can sift through mountains of evidence in seconds.
This teamwork lets doctors focus their expertise on the nuanced, complex decisions and direct patient care, while the AI handles the heavy lifting of data analysis.
A Rapidly Accelerating Transformation
The move to bring AI into clinical settings is happening fast. By 2025, artificial intelligence has become a cornerstone in medical diagnosis across the globe, with an estimated 80% of hospitals using AI technologies to improve how they care for patients and run their operations. This isn't just a few experimental projects anymore; it's becoming routine.
In fact, almost half (46%) of healthcare organizations in the U.S. are already exploring generative AI models. It’s clear this integration is well underway. The momentum is fueled by tangible benefits for both patients and providers. To get a better sense of this specific sector, you can explore the challenges and opportunities within the AI in healthcare industry.
Core Benefits Reshaping Patient Outcomes
To put it simply, AI is having a huge impact. Let's look at the key benefits in a quick summary.
| Area of Impact | Description | Example Application |
|---|---|---|
| Accuracy | AI algorithms spot patterns in medical data with incredible precision. | Detecting early-stage cancer or diabetic retinopathy from scans. |
| Speed | Automation of analysis cuts down diagnostic wait times dramatically. | Rapidly analyzing lab results or medical images to get answers to patients faster. |
| Prediction | Models can identify high-risk patients before symptoms are obvious. | Analyzing patient records to predict the likelihood of sepsis or heart failure. |
These core benefits show just how much value AI brings to the table, making diagnostics more precise, efficient, and proactive.
Beyond just analyzing images, other forms of artificial intelligence are making a difference, too. For instance, medical voice recognition software is changing how doctors handle patient records and cut down on administrative work, which frees up even more of their time for what matters most: caring for patients.
How AI Learns to See What Doctors See
So, how can a machine look at an MRI and spot a tumor with the same—or sometimes even better—accuracy than a radiologist with years of experience? The secret is in how it's taught. At its heart, AI learns a lot like we do: through repetition and pattern recognition, just at a scale no human brain could ever manage. This whole process runs on technologies like machine learning and its more advanced cousin, deep learning.
Think about teaching a child to identify a cat. You'd show them picture after picture, pointing out the pointy ears, the whiskers, the tail. Eventually, their brain builds a reliable model of what a "cat" is. AI models go through a similar training process, but it’s far more intense.
The Power of Data in Machine Learning
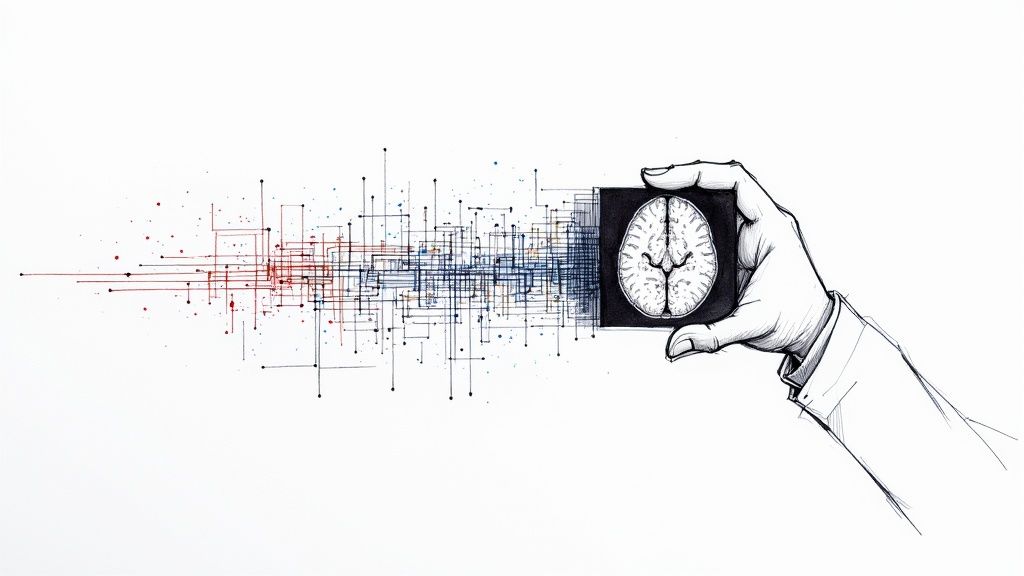
Machine learning is the real engine behind AI and medical diagnosis. The basic idea is to feed an algorithm a massive amount of medical data—images, lab results, patient charts, you name it. For something like diagnostic imaging, this means training an AI on hundreds of thousands of scans.
- Labeled Data: Each image in the training set is carefully "labeled" by human experts. For instance, radiologists will meticulously outline areas that show tumors, fractures, or other abnormalities.
- Pattern Recognition: The algorithm sifts through all these labeled examples to find the subtle patterns in pixels, textures, and shapes that consistently point to a specific diagnosis.
- Model Building: Based on what it learns, it builds a predictive model. When it sees a new, unlabeled scan, the AI uses this model to flag potential problems with a specific level of confidence.
AI can process irrationally large amounts of data to identify patterns, make predictions, and perform analyses that researchers would otherwise need to conduct manually. This ability to see the connections in vast datasets is what gives it a unique diagnostic edge.
This is how raw data gets turned into insights that can save lives, a principle that applies to all effective AI tools for business.
Deep Learning and the "Neural Network"
Deep learning takes this a step further. It's a more sophisticated type of machine learning that uses artificial neural networks, which are designed to loosely mimic the structure of the human brain. These networks have multiple layers of "neurons," and each layer gets progressively smarter.
Let's say it's analyzing a chest X-ray. The first layer might just learn to spot basic edges and shapes. The next layer could combine those to recognize the outline of a lung or a rib. Go a few layers deeper, and it starts learning to identify incredibly complex features, like the distinct texture of a malignant nodule.
This layered approach is what allows the AI to pick up on intricate patterns that are often invisible to the naked eye. That’s a game-changer for early disease detection, where the signs can be incredibly subtle. The entire process has to be built on a solid foundation, which is why a structured AI Product Development Workflow is so critical for creating reliable diagnostic tools.
The Critical Role of High-Quality Data
You’ve heard the saying "garbage in, garbage out," and it's never been more true than with AI. The quality of the training data is everything. If an AI is trained on a dataset that isn't diverse enough or is full of labeling errors, it will learn those same biases and make flawed diagnoses. Data curation isn't just a step; it's one of the most important parts of the entire process.
Beyond just the images, these AI models also need to understand medical context. This means knowing how conditions are classified using systems like the International Classification of Diseases. For example, by understanding the framework behind things like ICD-10 codes for ADHD, an AI can better interpret complex patient histories and symptoms.
Ultimately, this is how an algorithm develops the "sight" to help doctors, turning abstract data points into clear, actionable clinical intelligence.
Transforming Medical Imaging with AI Analysis
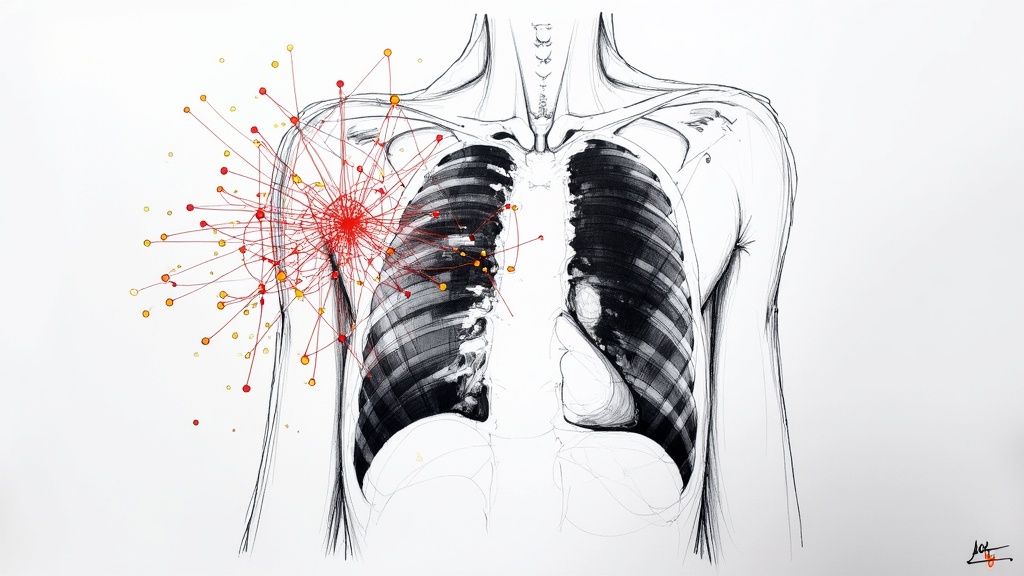
If there's one area where you can see the immediate, powerful impact of AI and medical diagnosis, it's in medical imaging. For specialists in fields like radiology, pathology, and dermatology, AI algorithms are quickly becoming an essential part of the toolkit. They analyze complex visual data with a level of speed and precision that perfectly complements human expertise.
Think about a radiologist who has to review hundreds of mammograms every single day. An AI can act as a tireless second set of eyes, flagging subtle or hard-to-spot areas of concern. This isn't about replacing the expert; it's about giving them a powerful tool to catch potential diseases earlier and more consistently.
A New Standard in Diagnostic Precision
The real magic of AI here is its ability to learn from enormous datasets. After being trained on thousands upon thousands of images, these models learn to spot the incredibly subtle patterns that often signal the presence of a disease.
For example, an AI trained on retinal scans can pick up on the earliest signs of diabetic retinopathy—a major cause of blindness—sometimes well before a human would notice or a patient experiences any symptoms. In dermatology, an AI can look at a picture of a skin lesion and assess its likelihood of being malignant, all by comparing it against a massive database of confirmed cases. This gives dermatologists a data-backed risk score, helping them decide which patients need a biopsy most urgently.
By taking over the more routine parts of image analysis, AI frees up highly trained specialists to focus their energy on the most complex and ambiguous cases. This directly improves both their workflow and patient outcomes.
Speed and Accuracy A Powerful Combination
But it's not just about being more accurate. The sheer speed at which AI can process these images is a complete game-changer, especially for healthcare systems struggling with heavy caseloads and long patient wait times.
Recent studies have validated this powerful one-two punch of speed and accuracy. Artificial intelligence has proven it can dramatically lighten the workload in diagnostic medicine. One major review of AI's diagnostic impact, which looked at over 2,500 articles, found AI can slash diagnostic time by 90% or more while also improving accuracy. Because radiology is already so digitized, it's a natural fit for AI, with some systems even capable of performing independent diagnoses.
The infographic below puts this advantage into clear perspective.
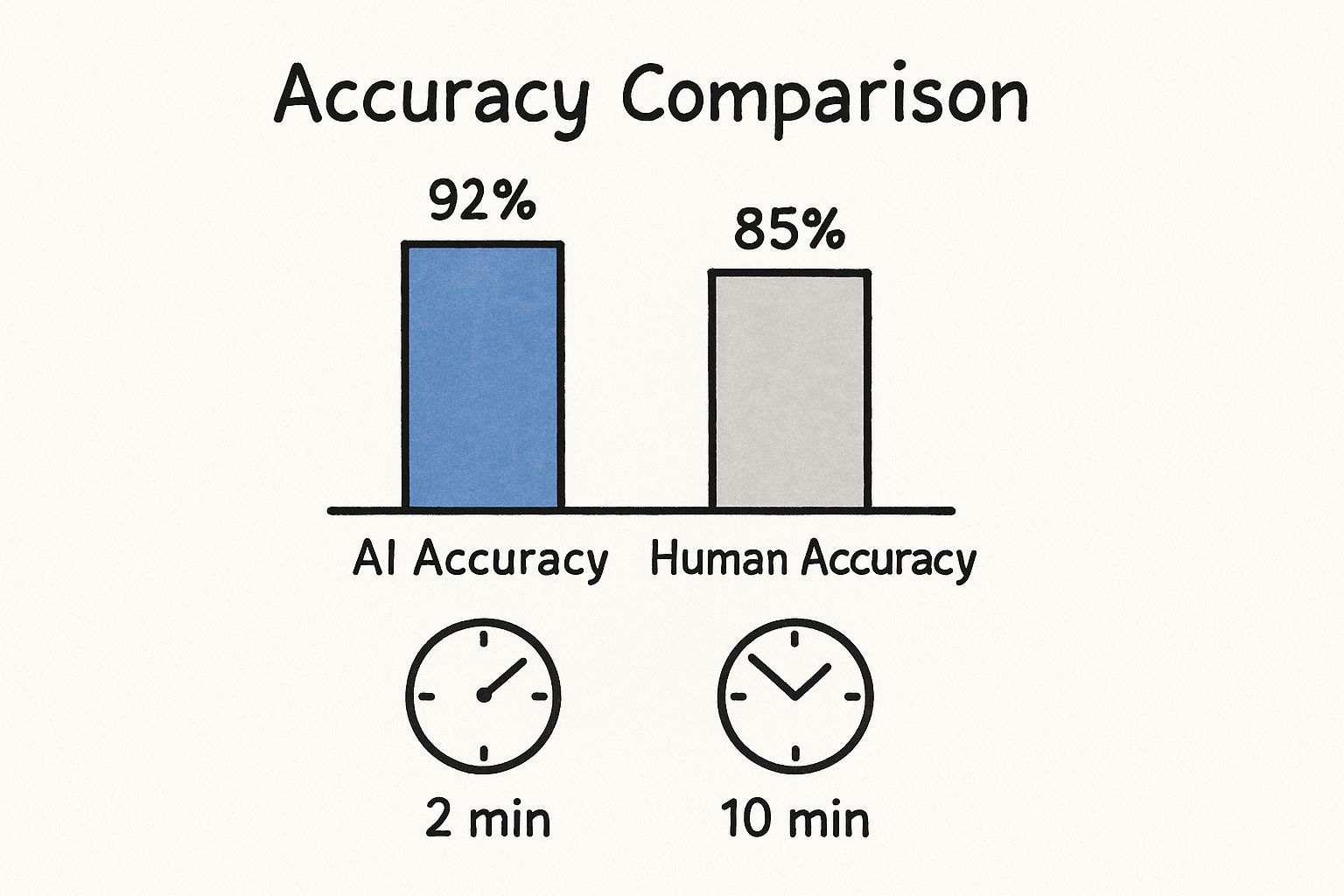
As you can see, AI-assisted analysis not only boosts the accuracy rate but gets the job done in a small fraction of the time. For patients, that means getting crucial answers faster.
To really appreciate the difference, let's look at a side-by-side comparison.
Comparing Diagnostic Imaging Approaches
| Feature | Traditional Human Analysis | AI-Assisted Analysis |
|---|---|---|
| Speed | Can take several minutes to hours per scan, depending on complexity. | Analysis is often completed in seconds or a few minutes. |
| Accuracy | Dependent on individual expertise, workload, and fatigue. | Consistently high, with the ability to detect subtle patterns humans might miss. |
| Workload | Can lead to burnout due to high volume and repetitive tasks. | Reduces manual review time, freeing up specialists for critical cases. |
| Consistency | Varies between individual practitioners and even for the same person over a day. | Delivers objective and standardized results every time. |
This table makes it clear how AI isn't just an incremental improvement—it represents a fundamental shift in how diagnostic imaging is performed.
Real-World Use Cases in Action
These aren't just concepts being tested in a lab; they are practical tools being put to work in clinics and hospitals today. The ability to analyze medical images quickly and reliably stands out as one of the most compelling real-world use cases for AI in the entire healthcare field.
Here are a few concrete examples of how it's being used right now:
- Oncology: AI tools are highlighting potential tumors in CT scans and MRIs, which helps oncologists stage cancer more precisely and build more effective treatment strategies.
- Pathology: Digital pathology is being completely transformed by AI. It can analyze tissue samples at a microscopic level to find cancer cells with incredible speed, easing the manual burden on pathologists. A great example of a tool in this space is our Diagnoo platform, an AI Medical Imaging Assistant.
- Cardiology: AI algorithms can analyze cardiac MRIs to precisely measure blood flow and heart muscle function, giving cardiologists hard data to diagnose heart conditions.
This close collaboration between human experts and intelligent algorithms is actively setting a new benchmark for medical imaging, making diagnostics faster, more accurate, and ultimately more accessible for everyone.
Predicting Disease Before Symptoms Appear
What if a hospital could flag patients most at-risk for a crisis like sepsis or heart failure before they even feel sick? While AI is a game-changer in medical imaging, its real power lies in forecasting disease. This is a fundamental shift from reactive to proactive medicine, turning algorithms into a modern-day lookout, spotting trouble on the horizon long before it arrives.
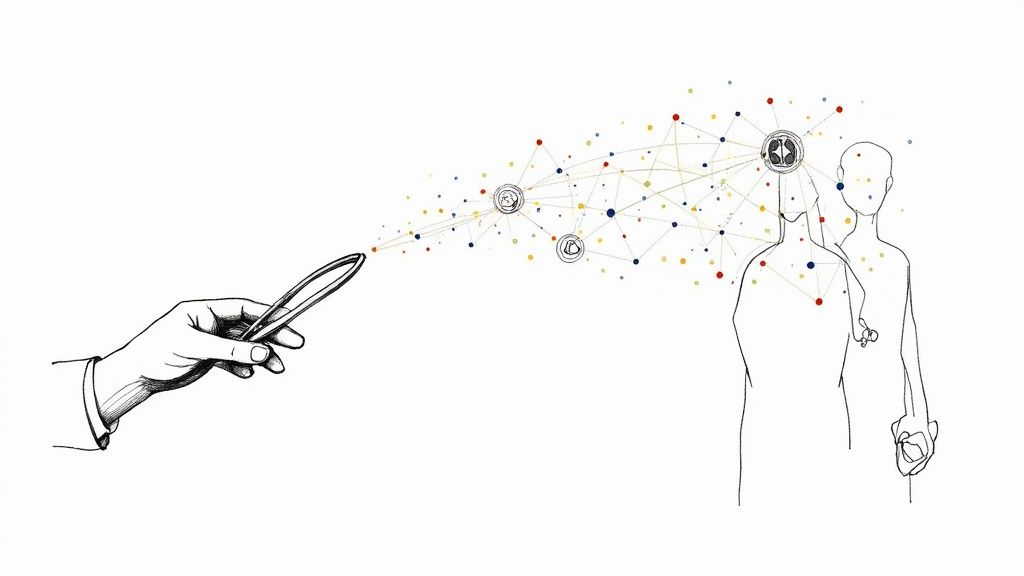
This isn't about looking at a single scan. Instead, AI models dive deep into a patient's entire history, sifting through electronic health records (EHRs), genetic markers, lab results, and even lifestyle details from past visits. By connecting millions of data points that might seem unrelated, these systems uncover the subtle, complex patterns that signal a higher risk for a specific illness.
This is a core objective of modern healthcare software development—building systems designed to keep people healthier for longer by intervening much earlier.
How AI Models Forecast Health Risks
At its heart, predictive analytics in medicine is about calculating probability. An AI can't see the future, but it can calculate the odds with stunning accuracy by learning from the past.
- Learning from History: The AI is first trained on massive, anonymized health records from millions of patients. It learns which combinations of symptoms, lab values, and genetic factors have historically led to a specific disease.
- Monitoring in Real-Time: In a hospital, these models can watch incoming patient data as it happens. For instance, an AI might analyze vital signs from ICU monitors, searching for tiny changes that, when combined, strongly point to the onset of sepsis.
- Creating Personal Risk Scores: Based on this ongoing analysis, the system generates a personalized risk score for each patient. This gives clinicians a clear, data-backed way to prioritize their attention and focus on those who need proactive care the most.
This data-driven foresight allows healthcare providers to move from just treating sickness to actively preserving wellness. It’s about stopping a health crisis before it ever begins—a change that requires both advanced technology and a clear vision.
Pinpointing the most impactful predictive opportunities within a health system is where expert AI strategy consulting becomes invaluable.
The Impact of Early Intervention
The benefits here are enormous. When a high-risk patient is flagged early, clinicians can take preventative steps that are often simpler, less invasive, and far more effective than treating a disease in its advanced stages.
Think about it: a model might predict a high risk of pancreatic cancer by spotting subtle patterns scattered across years of a patient's health records—patterns a human doctor could easily miss. That prediction could trigger a recommendation for targeted screening, potentially catching the cancer at a highly treatable Stage 1 instead of a near-fatal Stage 4.
The performance of these tools is already impressive. In cardiology, AI has been shown to rule out heart attacks at double the speed of human clinicians with 99.6% accuracy. In oncology, AI models are now predicting cancer patient survival with roughly 80% accuracy, helping to fine-tune personalized treatment plans. You can explore more of these groundbreaking AI healthcare statistics to see the full picture.
This proactive approach is what makes predictive analytics so compelling. It gives doctors the gift of time—time to intervene, to treat, and to completely change a patient's health trajectory. To work, however, these powerful tools must be rolled out thoughtfully, following a structured AI Product Development Workflow that ensures they fit safely and seamlessly into clinical practice. It’s not just about better diagnostics; it’s about fundamentally changing patient outcomes for the better.
Navigating the Hurdles of AI in Healthcare
While the potential of using AI for medical diagnosis is massive, actually bringing these tools into a hospital or clinic is anything but a simple plug-and-play affair. It’s a journey filled with technical roadblocks, ethical minefields, and strict regulatory hurdles. Having a smart algorithm is one thing; making it work safely and effectively in the real world of patient care is another challenge entirely.
The path to getting it right is complex. Organizations have to think about everything from data privacy and HIPAA compliance to the very real danger of algorithmic bias. To succeed, you need a careful, strategic approach that puts patient safety and clinician trust front and center.
Technical and Integration Challenges
One of the first walls you’ll hit is technical. Many healthcare systems are running on older IT infrastructure and electronic health record (EHR) systems that simply weren't built for the massive datasets AI requires. Trying to connect a modern AI platform to these legacy systems can be a painful—and expensive—process.
This isn’t just about flipping a switch. It takes serious work to get data flowing securely and smoothly between the old and the new. Without a solid plan for interoperability, even the most powerful AI tool will be stuck in a silo, unable to provide any real value.
Data Privacy and Regulatory Compliance
In healthcare, patient data is intensely personal and legally protected. Regulations like the Health Insurance Portability and Accountability Act (HIPAA) in the U.S. set an incredibly high standard for privacy. Any AI solution that touches patient information must be fully compliant, meaning all data has to be properly anonymized and locked down.
The real trick is training sophisticated AI models without ever compromising patient confidentiality. This demands bulletproof security and a deep understanding of the law, making compliance the bedrock of any healthcare AI project.
This is where specialized tools come into play. For instance, our VeriFAI platform helps businesses ensure AI compliance by validating that a model is fair and performs according to regulatory standards—something that's absolutely critical in a high-stakes field like medicine.
The Risk of Algorithmic Bias
An AI model is a product of its education. If you train it on data that isn’t diverse or representative of all the patients it will see, the algorithm can inherit and even amplify hidden biases. Think about it: a model trained mostly on data from one demographic might misdiagnose conditions in another, making existing health disparities even worse.
Fighting this bias requires a proactive approach:
- Curate Diverse Datasets: You have to go out of your way to source and include data from a wide spectrum of patient populations.
- Audit, Audit, Audit: Continuously test the AI to see if it's producing biased results or performing unfairly for certain groups.
- Demand Transparency: Whenever possible, use AI models that aren't a complete "black box," so doctors can understand why the tool is making a specific recommendation.
Building Trust Through Clinical Validation
Last but certainly not least is the human factor. Doctors and nurses won’t use a tool they don’t trust. This trust isn’t built on marketing promises; it's earned through hard evidence.
Every new AI diagnostic tool has to go through rigorous clinical validation. Its performance must be tested in real clinical settings and measured against the current gold standard of care. This is the only way to prove that an AI is not just accurate but also safe and genuinely helpful. Success here comes from having a clear plan from day one, which is why a thoughtful strategy is so crucial for navigating these challenges and turning an innovative idea into a trusted clinical tool.
The Future of Diagnostics and Your Role In It
We’re really just at the starting line when it comes to AI and medical diagnosis, but the finish line is coming into view: a future where healthcare is more predictive, precise, and deeply personalized. We've seen how AI is already making its mark—redefining medical imaging, flagging diseases before symptoms ever show up, and giving clinicians a powerful co-pilot to translate overwhelming data into life-saving insights.
The goal was never to replace human expertise. It’s about creating a powerful partnership between a skilled clinician and a smart algorithm.

This collaboration is what will finally shift medicine from a reactive, treatment-focused model to a truly proactive and preventive one.
Emerging Frontiers in Healthcare AI
This field is moving incredibly fast, with new ideas constantly changing what we thought was possible. Right now, two of the most exciting developments on the horizon are generative AI and federated learning. Each one tackles a huge challenge: data access and patient privacy.
Generative AI for Synthetic Data: One of the biggest roadblocks to training better diagnostic models is getting enough high-quality, diverse patient data. Generative AI offers a brilliant workaround by creating realistic, completely anonymous synthetic patient records. This means researchers can train and test their models without ever touching sensitive patient information, speeding up innovation while keeping ethics front and center.
Federated Learning for Privacy: This clever approach trains an AI model across multiple locations—say, a network of hospitals—without the patient data ever leaving its source. The model learns from the local data at each institution, and only the refined model updates, not the private information, are shared. It’s a game-changer for building powerful, globally-trained models while respecting strict privacy rules.
If there's one key takeaway, it's this: AI is a collaborative tool. It’s built to augment, not replace, human expertise. The future of medicine is this dynamic duo of brilliant clinicians and intelligent algorithms working side-by-side.
For healthcare leaders and innovators ready to get in on the ground floor, the moment is now. Moving forward means spotting the right opportunities and drawing up a clear plan for success, a process we break down in our AI adoption guide.
Whether your organization needs to streamline its operations with workflow automation or build custom internal tooling for specific challenges, the potential is enormous.
Getting started takes a clear vision and the right partner. To see how AI Solutions can fit your specific needs and to build a strategy that delivers real results, connect with our expert team. We’re here to help you navigate what’s next in diagnostics and turn that potential into real progress.
Frequently Asked Questions
As we dig into the world of AI and medical diagnosis, a lot of practical questions come to the surface. Let's tackle some of the most common ones to get a clearer picture of how this technology really works in healthcare.
Will AI Replace Doctors and Radiologists?
Not a chance. The overwhelming consensus is that AI is here to assist, not replace, medical professionals. Think of AI as an incredibly powerful assistant that's a master at spotting patterns in massive piles of data. It can flag potential issues in a scan or automate tedious tasks, but it lacks the critical thinking and empathy of a human doctor.
This dynamic frees up clinicians to concentrate on what they do best: handling complex patient cases, designing treatment plans, and focusing on the deeply human side of medicine. It’s a collaborative model—AI crunches the data, and doctors use their years of experience to make the final call.
How Accurate Is AI Compared to Human Doctors?
In certain, very specific tasks—like analyzing medical images—AI has demonstrated accuracy that's on par with, and sometimes even better than, human experts. But there's a huge caveat: an AI model is only as good as the data it's trained on.
If the training data is biased or incomplete, the results will be skewed. This is why rigorous, ongoing clinical validation and regulatory oversight are absolutely critical. We have to ensure these tools are safe, effective, and fair for everyone, which is a central part of any serious AI strategy consulting.
What Are the Biggest Barriers to Adopting AI in Hospitals?
The hurdles are significant. First, there's the technical headache of making new AI systems talk to ancient hospital IT infrastructure. Then you have the maze of regulatory and privacy rules like HIPAA. And, of course, the upfront cost can be substantial.
Beyond the tech and money, there's a cultural barrier. You have to build trust with the clinicians who will be using these tools every single day.
Overcoming these challenges isn't just about having great technology; it's about having a smart, structured plan. This is precisely why services like AI Automation as a Service exist—to offer a step-by-step, manageable path to getting it right.
How Can a Healthcare Organization Start Using AI?
The key is to start small and be strategic. Don't try to boil the ocean. Instead, pick one specific, high-impact problem to solve. Maybe it’s cutting down diagnostic wait times or making initial screenings more precise.
Run a pilot project to prove the concept and show stakeholders that it actually works. It's also crucial to bring your clinical and IT teams into the conversation from day one to make sure the new tool fits into how they already work. For those who aren't sure where to begin, a Custom AI Strategy report can build a clear roadmap, and this is the same structured approach we outline in our AI adoption guide.
Ready to see what AI can do for your organization's diagnostic power? At Ekipa AI, we help turn complex AI possibilities into real-world results. Explore our suite of powerful AI Solutions and let's start building your roadmap for a smarter future.