AI Medical Diagnosis Explained for Healthcare Leaders
Explore how AI medical diagnosis is transforming patient care. This guide explains key technologies, real-world applications, and strategic implementation.
At its core, AI medical diagnosis is about using sophisticated algorithms to make sense of complex medical data. It’s a tool that helps clinicians catch diseases earlier and with much higher precision.
Think of it as a second set of eyes—a digital partner that can see patterns in scans, patient records, and lab results that are often invisible to a human observer. This partnership between human expertise and machine intelligence is already changing the game for patient care.
The New Partner in Clinical Decision Making
Picture a world where a doctor's expertise is backed by a system that has analyzed millions of medical cases. That's the real value of AI medical diagnosis. It’s not about replacing doctors; it’s about giving them superpowers. The technology acts like a tireless assistant, digging through mountains of data to surface critical insights.
This frees up clinicians to focus on the uniquely human side of medicine: empathy, complex problem-solving, and building patient relationships. While the AI crunches the numbers, doctors and nurses can spend more time understanding the results in the context of a person's life. Visionaries like Dr. Daniel Kraft, a leading physician scientist and healthcare futurist, have been championing this kind of collaborative future for years.
Enhancing Diagnostic Capabilities
The magic of AI in a clinical setting is its ability to pull together information from all sorts of places at once. We're talking medical images, genomic data, lab reports—you name it.
Here’s a practical look at how it elevates a clinician's work:
- Spotting the Unseen: AI can pick up on faint abnormalities in MRIs or CT scans that might hint at an early-stage disease.
- Connecting the Dots: It pulls together a patient’s history, lab work, and clinical notes to build a complete picture of their health.
- Looking Ahead: By analyzing population-level data, AI can even help predict a patient's risk for certain conditions long before symptoms show up.
This added firepower leads directly to better outcomes. In fact, recent studies have shown some AI diagnostic models solve difficult medical cases correctly up to 85% of the time. That's a massive step forward. Getting a diagnosis faster and with more confidence can mean fewer unnecessary tests and a quicker path to the right treatment.
The goal is to build a seamless partnership where AI offers data-backed suggestions, and the clinician uses their experience and judgment to make the final decision. It’s the perfect blend of machine precision and human wisdom.
Bringing these systems into a hospital or clinic isn't something you can do overnight; it demands a clear, well-thought-out plan. This is where building a solid AI strategy becomes crucial. By focusing on high-level AI Solutions, healthcare organizations can give their teams the tools they need to make a real difference in patient care, from the ground up. With this foundation in place, we can now explore the specific technologies that make it all possible.
Understanding The Core Diagnostic Technologies
So, how does an AI actually learn to spot a disease? It’s not magic. It’s a combination of powerful technologies trained on staggering amounts of medical data. The engine behind AI medical diagnosis is built on a few key concepts that, once you get them, show how machines can reach such incredible precision.
Think of these technologies as different specialists on a medical team. Just like a hospital needs a general practitioner, a radiologist, and a medical scribe, an effective AI diagnostic system needs Machine Learning, Deep Learning, and Natural Language Processing to do its job well.
The infographic below shows the main methods currently in play, highlighting how widely each is being adopted and where the growth is happening.
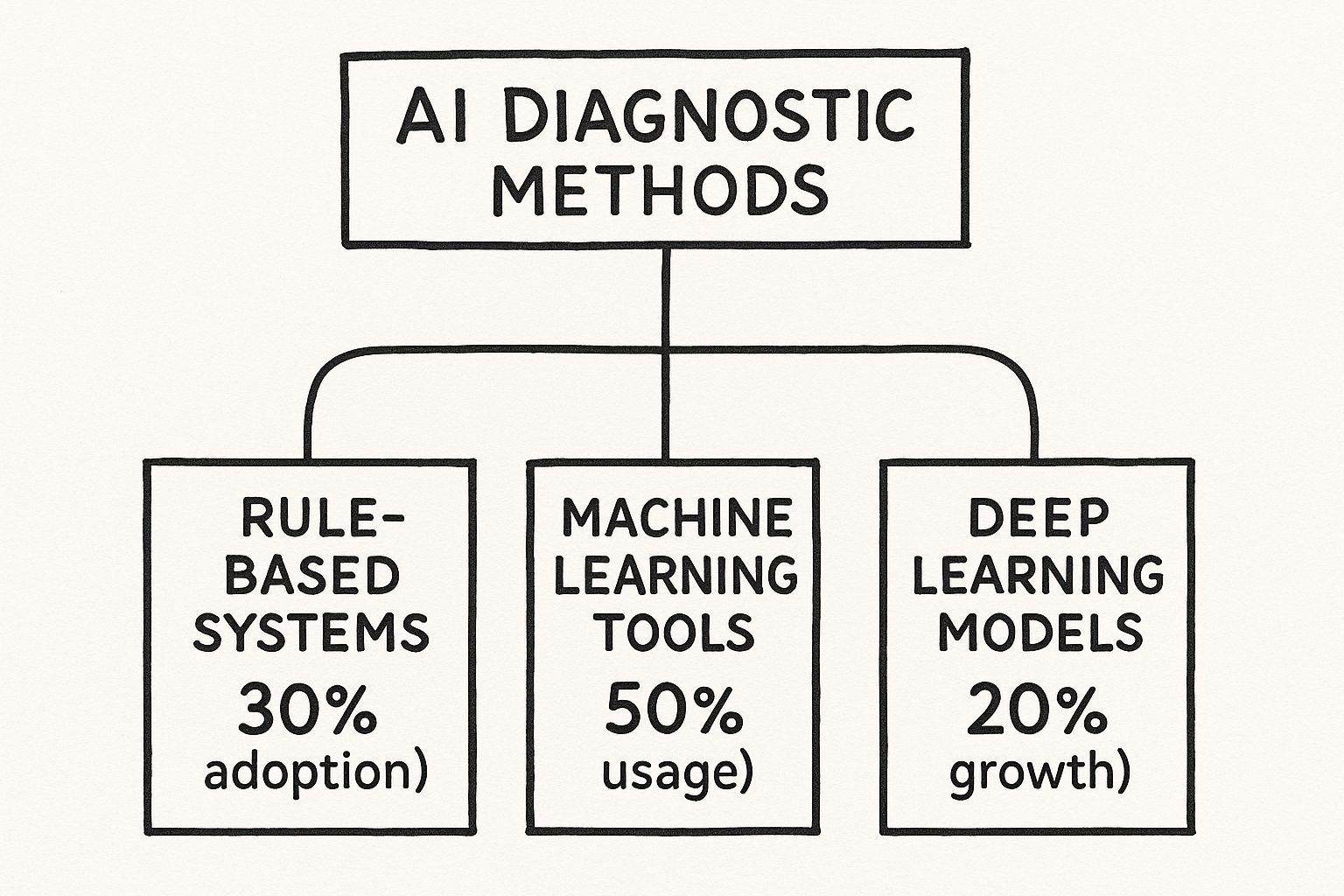
As you can see, older rule-based systems still have their uses, but Machine Learning tools are by far the most common. At the same time, Deep Learning models are gaining ground fast as the technology gets better and more accessible.
To really get a feel for how these pieces fit together, let's look at the "big three" that form the foundation of modern medical AI.
Comparing Key AI Technologies in Medical Diagnosis
Each of these core technologies plays a distinct but complementary role. The table below breaks down their primary functions, where you're most likely to see them in action, and the kind of data they're built to handle.
| Technology | Primary Function | Example Application | Data Type Processed |
|---|---|---|---|
| Machine Learning (ML) | Pattern recognition and prediction from structured data. | Predicting patient risk for conditions like heart disease from electronic health records (EHRs). | Structured data (e.g., lab results, patient vitals, spreadsheets). |
| Deep Learning (DL) | Identifying complex, hierarchical patterns in large, unstructured datasets. | Analyzing medical images like MRIs or X-rays to detect tumors or anomalies. | Unstructured data (e.g., medical images, genomic sequences). |
| Natural Language Processing (NLP) | Understanding and extracting information from human language. | Pulling key symptoms and patient history from a clinician's free-text notes. | Text-based data (e.g., doctor's notes, research papers, patient reports). |
This comparison shows how each technology is specialized for a different kind of diagnostic challenge, from making predictions based on numbers to finding clues hidden in images or text.
Machine Learning: The Digital Medical Student
At its heart, Machine Learning (ML) works like a medical student poring over thousands of case files. The student learns to recognize patterns by being shown countless examples—patient symptoms, lab results, and their final diagnoses.
In the same way, an ML algorithm is fed massive datasets of labeled medical information. It might sift through thousands of patient records to learn the statistical connections between specific biomarkers and a certain disease. After enough training, it gets really good at predicting outcomes when it sees new, unfamiliar data. This makes ML perfect for jobs like identifying patients at high risk for diabetes based on their health records.
Deep Learning: The Expert Radiologist’s Brain
If Machine Learning is the diligent student, then Deep Learning (DL) is the seasoned radiologist with decades of experience under their belt. Deep Learning is a more advanced part of ML that uses intricate structures called neural networks, which are loosely inspired by the human brain.
These networks have many layers, which lets them learn from data in a much more subtle and intuitive way. A deep learning model can look at a chest X-ray and pick up on tiny, complex patterns—like the faint shadow of an early-stage tumor—that a less experienced human eye might easily miss.
This is because DL models don't just follow rules; they learn to recognize features and hierarchies within the data itself. This ability to "see" complexity makes them incredibly powerful for image analysis in fields like radiology and pathology. For example, our own Diagnoo, a tool for medical image annotation, is built on these principles to help create the high-quality datasets needed to train such models.
Natural Language Processing: The Master Transcriber
Finally, we have Natural Language Processing (NLP), which acts as the brilliant medical transcriber on the team. A huge amount of critical diagnostic information is locked away in unstructured text—doctors’ notes, patient histories, and clinical trial reports.
NLP gives AI the ability to read, understand, and interpret human language. An NLP algorithm can scan a doctor's notes and pull out key diagnostic clues, like reported symptoms or family medical history. This technology is essential for building a complete picture of a patient's health by making sense of the narrative part of medical records. It bridges the gap between raw text and actionable data, ensuring no crucial detail gets lost in translation.
AI's Breakthrough Role in Cancer Detection
Nowhere does the potential of AI medical diagnosis feel more real than in oncology. This is where complex data and life-or-death decisions meet, creating the perfect environment for AI to show what it’s truly capable of. In cancer care, algorithms are more than just data processors; they become a critical partner in the fight against one of humanity's most persistent diseases.
It all starts with training. AI models are fed enormous visual libraries containing thousands upon thousands of mammograms, CT scans, and pathology slides. Each image has been carefully labeled by expert oncologists, teaching the AI to spot the subtle textures, shapes, and patterns that hint at malignancy—often long before they’re obvious to the human eye.
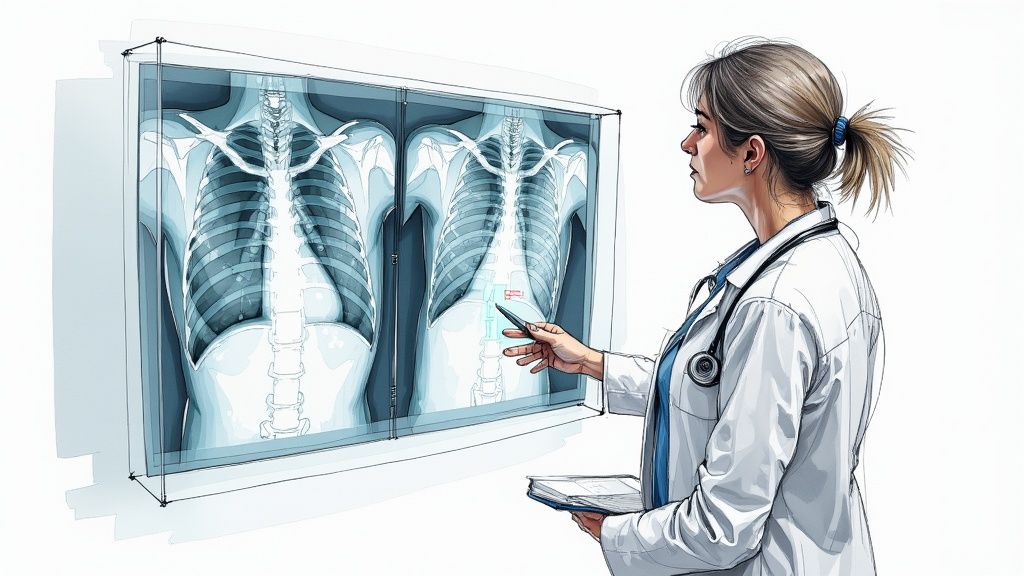
A Vigilant Second Opinion for Radiologists
Think of this AI as a tireless second pair of eyes. A radiologist’s job is incredibly demanding, requiring intense concentration to find tiny abnormalities across hundreds of images a day. An AI assistant can pre-screen these scans, flagging suspicious areas that deserve a closer look.
This isn’t about replacing the expert; it's about augmenting their ability. The system is built to reduce the chances of a false negative, where the very first signs of cancer might be overlooked. By pointing out potential trouble spots, the AI helps direct the radiologist's attention where it's needed most, which improves both diagnostic accuracy and speed. It's a perfect blend of human expertise and machine precision. Our expertise in healthcare software development is centered on creating these exact kinds of collaborative tools.
This human-AI partnership isn't just about finding cancer; it’s about finding it sooner. Early detection is one of the biggest factors in successful treatment, making this technology a monumental step forward for oncology.
The results speak for themselves. Some AI diagnostic tools have reached a match rate of up to 93% in identifying cancer cases. This level of accuracy is becoming essential as clinics and labs face a growing number of patients. By bringing AI into the workflow, labs can track samples more efficiently and deliver results faster, building a more responsive healthcare system. You can read more about how AI is revolutionizing diagnostics on scispot.com.
From Faster Biopsies to Personalized Medicine
This collaboration has a direct impact on the patient experience. When AI helps a radiologist prioritize suspicious findings, biopsies can be scheduled faster. For someone waiting anxiously for answers, shrinking the timeline from weeks to days can make an enormous emotional difference and get treatment started much earlier.
But it doesn't stop at diagnosis. AI’s analytical power is also opening the door to highly personalized treatment plans. By analyzing the specific genomic and cellular details of a tumor from a pathology slide, AI can help oncologists predict which treatments are most likely to work for that individual.
This shifts cancer care away from a one-size-fits-all model and toward true precision medicine. AI doesn’t just help find cancer; it helps us fight it smarter, improving patient outcomes and demonstrating the incredible potential of well-designed AI Solutions.
A Look at AI's Impact Across Different Medical Fields
While cancer detection often gets the most headlines, the real story of AI medical diagnosis is its incredible range. The same smart technology that spots tumors on a CT scan is now being adapted for all sorts of medical specialties, changing how doctors find and treat a huge variety of conditions. AI is quickly becoming a go-to tool for providers everywhere.
This isn't just about a single new gadget; it's a fundamental shift in how medicine is practiced. We're seeing powerful AI Solutions pop up on multiple fronts, creating a healthcare system that's more about preventing problems than just reacting to them.
A New Era for Cardiology and Heart Health
In a field like cardiology, where every second counts, AI is a game-changer. Models are being trained to read electrocardiograms (ECGs) in a flash, catching tiny flutters and dips that might signal a future heart attack. Think of it as a digital specialist who can screen a patient's heart rhythm and flag a risk long before it becomes an emergency.
This is pushing cardiology from a reactive practice to a proactive one. Instead of waiting for a heart attack to happen, AI helps doctors pinpoint high-risk individuals and step in early. These are some of the most powerful real-world use cases for diagnostic AI right now.
The results speak for themselves. AI models can now rule out a heart attack twice as fast as a human doctor, and they do it with an astonishing 99.6% accuracy. This kind of speed doesn't just save precious time; it also eases the strain on busy emergency rooms, letting staff concentrate on patients who need them most. You can explore more AI healthcare statistics like this on dialoghealth.com.
Detecting Neurological Disorders Sooner
Neurology is another field being completely transformed. Conditions like Alzheimer's and Parkinson's disease are notoriously tricky because they creep up over many years, with early signs that are easy to brush off. AI is perfectly built to catch these faint, early warnings.
For instance, AI tools can now listen to how a person talks—noting subtle changes in their vocabulary, sentence construction, or even how often they hesitate—to spot the first signs of cognitive decline.
This technology can pick up on tiny linguistic shifts that even a spouse or close friend might miss, providing a simple, non-invasive way to screen for diseases like Alzheimer's. One such tool, CognoSpeak, has shown a 90% success rate in flagging the disease just from speech analysis.
It's a similar story with stroke diagnosis. AI software has proven to be twice as accurate as clinicians when analyzing brain scans to identify a stroke. In a situation where every minute is critical, that level of precision is everything. Getting the diagnosis right, and right away, means the correct treatment can start immediately, which can drastically improve a patient's chances of recovery. This is a perfect example of how specialized AI in the healthcare industry is making a real difference.
From the heart to the brain, the applications for AI medical diagnosis are expanding by the day. And with each new use case, the core benefit remains the same: giving clinicians better information so they can provide faster, more accurate, and more personalized care to every single patient.
Navigating the Hurdles: Implementation Challenges and Ethics

Bringing AI medical diagnosis tools into a clinical setting isn't like installing a new piece of software. It’s a fundamental operational shift, one that brings its own set of very real challenges and tough ethical questions. For any healthcare leader, staring these hurdles down is the first step toward actually overcoming them.
A successful rollout depends on a clear-eyed plan that accounts for both the complex technology and the people who will use it. From integrating with decades-old systems to ensuring the AI is fair for every patient, each step is a puzzle to solve. This is where guidance from an expert AI strategy consulting team can turn potential roadblocks into a clear path forward.
The Technical Hurdles of Integration
Right out of the gate, you’ll likely face technical integration issues. Many hospitals and clinics are built on legacy IT systems that simply weren't designed for the massive, high-velocity datasets that power modern AI. Making a sophisticated new AI platform talk to an older Electronic Health Record (EHR) system without a hitch can be a monumental task.
Then there's the data itself. An AI model is only as smart as the data it learns from. If your historical patient records are a mess—riddled with inconsistencies, missing fields, or poor labeling—the AI’s diagnostic accuracy will be compromised. This reality often forces a significant, upfront effort to clean and standardize data, a crucial first step in any AI Product Development Workflow.
Algorithmic Bias and the "Black Box" Problem
Beyond the wires and servers lie deep ethical considerations. Algorithmic bias is one of the most serious. If an AI is trained primarily on data from one demographic, its performance can drop significantly when diagnosing patients from underrepresented groups. Fighting this bias isn't just an ethical nice-to-have; it's a clinical necessity for equitable care.
Another major challenge is what’s known as the "black box" problem. Some of the most powerful AI models, especially in deep learning, can provide an answer without showing their work. They can't explain the logic behind their conclusions. For a clinician who is professionally and legally on the hook for every diagnosis, this lack of transparency is a massive barrier to trust.
Building that trust requires a real commitment to explainable AI (XAI). This means choosing or developing models that can articulate why they arrived at a particular diagnostic suggestion. It's the key to getting clinicians on board and satisfying regulators.
Tackling these issues isn't about buying a single product. It’s about building a comprehensive strategy that includes upgrading infrastructure, creating strong data governance policies, and selecting AI tools for business that are built on fairness and transparency.
Data Privacy and Regulatory Compliance
Finally, every AI tool in healthcare must operate within a maze of strict regulations. Protecting patient privacy under laws like HIPAA is absolutely non-negotiable. Any AI medical diagnosis platform must have ironclad security protocols to protect sensitive health information.
This means ensuring data is encrypted at every stage, access is locked down, and the entire system is compliant with all relevant healthcare laws. A Custom AI Strategy report is invaluable for mapping these compliance needs from the very beginning, making sure innovation doesn't compromise patient trust or legal standing.
The challenges are significant, but with the right expertise from our expert team, they are entirely surmountable.
Building Your AI Implementation Roadmap
So, you see the potential of AI medical diagnosis. But how do you get from a great idea to a tool your clinicians actually use? The answer is a clear, actionable plan—a roadmap that guides your organization from initial concept to full-scale adoption, as we explored in our AI adoption guide.
The trick is to avoid boiling the ocean. Don't try to solve everything at once. Instead, start small by identifying a single, high-impact problem. Maybe your radiology department is drowning in a backlog of scans, or perhaps you could triage patient messages far more efficiently. A successful pilot project in one of these areas is the best way to prove the value and build momentum for bigger things.
Assembling the Right Team
An AI project isn't just an IT initiative; it's a clinical one. Success hinges on putting together a multidisciplinary team that can see the project from every angle.
- Clinical Champions: You need doctors, nurses, and technicians on board from day one. These are the people who live the workflows every day, and they’re the only ones who can tell you if a tool is genuinely useful or just a flashy distraction.
- Technical Experts: This is where your data scientists and engineers come in. They’ll handle the heavy lifting of managing data, building the models, and making sure the tech actually works.
- Administrative Leadership: Without buy-in from the top, even the best ideas can stall. You need leaders who can secure the budget and champion the project throughout the organization.
When these three groups work together, you build solutions that are not only technically impressive but also clinically sound and seamlessly integrated into how your teams already work. This could even lead to developing custom internal tooling that perfectly fits your needs.
Data Readiness and Partner Selection
Once you have a target and a team, your focus has to shift to the raw materials: data and technology. The old saying "garbage in, garbage out" has never been more true than with AI. Your model's performance is entirely dependent on the quality of the data it learns from, which means you need to invest time upfront making sure your data is clean, organized, and accessible.
Finally, you need to decide if you're building this alone or bringing in a partner. Choosing the right technology partner can make all the difference. Look for someone who doesn't just understand the tech but also gets the unique pressures and regulations of healthcare. From strategy to rollout, the right partner acts as an extension of your team. You can see how we approach this with our AI Product Development Workflow.
Ultimately, unlocking AI's potential isn't about a single giant leap. It's about a well-planned journey built on small wins, a great team, and the right partners to guide you.
Frequently Asked Questions about AI in Medical Diagnosis
As we explore bringing AI into the world of medical diagnosis, it’s only natural to have questions. This isn't just about new software; it's about changing how we approach patient care. Let's tackle some of the most common questions that come up when healthcare leaders start thinking about adopting AI.
Is AI going to replace doctors?
In a word, no. The goal here is augmentation, not replacement. Think of AI as an incredibly sophisticated assistant. It can sift through mountains of data—like thousands of medical images or complex genomic sequences—and spot patterns that might be invisible to the human eye. Ultimately, the final diagnosis and the patient care plan are still firmly in the hands of the clinician. They take the insights from the AI and combine them with their own expertise, experience, and, most importantly, the human context of the patient sitting in front of them.
Just how accurate is AI at diagnosing diseases?
This is a great question, and the answer is: it depends entirely on the specific job it's designed for and the quality of data it learned from. For certain tasks, like analyzing X-rays or mammograms, top-tier AI models have shown they can perform on par with, and sometimes even better than, human specialists. But these are highly specialized tools, not general-purpose diagnosticians. Every AI diagnostic tool goes through intense clinical testing and regulatory approval to prove it’s safe, reliable, and does what it claims to do. For more answers to common AI questions, you can find a lot of great information in BuddyPro.ai's FAQ section.
What's the first step for a hospital wanting to implement AI?
Jumping in without a plan is a recipe for frustration. The journey always starts with a clear, focused strategy. A phased approach almost always works best.
- Find a Real Problem: Don't start with the technology; start with a pain point. Is it long turnaround times for pathology reports? A bottleneck in radiology? Pinpoint a specific, high-impact issue that AI could realistically help solve, perhaps through workflow automation.
- Check Your Data: AI models are only as good as the data they're trained on. Take a hard look at your data infrastructure. Do you have the clean, well-organized data needed to make an AI tool effective?
- Assemble Your Crew: You need a mix of people at the table. Get clinicians, IT specialists, and data scientists talking to each other. A great way to begin is with a small, focused pilot project to test the waters and prove the value before you consider a wider rollout.
Who regulates these AI diagnostic tools?
AI diagnostic tools are considered medical devices, so they fall under the same strict oversight as a new scanner or surgical instrument. In the United States, that means the FDA. Before any AI tool can be used on patients, its developers have to go through a rigorous approval process. This involves submitting extensive evidence from clinical trials to prove the tool is both safe and effective. This regulatory framework is crucial for building trust with both medical providers and the patients they serve.
Ready to turn these insights into action? The Ekipa our expert team can help you build a clear, effective strategy to integrate AI into your clinical workflows. Get started with your custom AI roadmap today.