AI in Medical Diagnosis and Patient Care
Explore how AI in medical diagnosis is transforming patient care. Learn about real-world AI applications, benefits, and challenges in modern healthcare.
Picture this: a radiologist has a second set of eyes that can scan thousands of medical images in a few seconds, flagging subtle patterns the human eye might otherwise miss. This isn't science fiction; it's the reality of AI in medical diagnosis today.
The point isn't to replace physicians. It's about giving them powerful tools that can process incredibly complex data—from MRIs and CT scans to genomic sequences and patient histories—with a speed and precision that’s simply beyond human capability.
The New Co-Pilot in the Exam Room
At its core, artificial intelligence in healthcare creates a powerful partnership between a doctor's intuition and a machine's analytical might. This collaboration is already leading to earlier disease detection, more personalized treatment plans, and, most importantly, better outcomes for patients. Healthcare organizations are actively bringing in comprehensive AI Solutions to stay on the leading edge of medical innovation.
This guide will break down how AI is becoming an indispensable ally for clinicians. We’ll look at the specific technologies driving this shift and see some real-world use cases. To appreciate this leap, it helps to look back at the broader integration of computers in healthcare, which really set the stage for these advanced diagnostic tools.
Key Technologies Transforming Diagnosis
AI in diagnostics isn't a single "thing." It's a combination of several key technologies working together to turn raw data into something a clinician can actually use. Grasping these core components is the first step to seeing just how big of an impact AI is having.
To give you a clearer picture, this table summarizes the main technologies and what they do in a diagnostic setting.
Key AI Technologies in Medical Diagnosis
| AI Technology | Primary Function in Diagnosis | Common Application |
|---|---|---|
| Machine Learning (ML) | Learns from vast datasets to identify patterns and predict outcomes. | Analyzing patient records to predict disease risk or treatment response. |
| Deep Learning | Uses complex neural networks to interpret unstructured data, like images. | Identifying cancerous nodules in CT scans or detecting diabetic retinopathy from images. |
| Natural Language Processing (NLP) | Understands and extracts information from human language. | Sifting through clinical notes and medical literature to find relevant information. |
As you can see, each piece of the puzzle plays a specific role.
Machine Learning (ML) is the engine behind it all. It allows a system to learn from massive amounts of data without being explicitly programmed for every scenario. In a hospital, an ML model could analyze millions of patient files to pinpoint subtle risk factors for a disease that no single doctor could ever spot on their own.
Deep Learning, a more advanced form of ML, uses intricate "neural networks" that are loosely modeled on the human brain. This makes it incredibly good at making sense of messy, unstructured data. Think about interpreting a medical image—that's where deep learning truly shines.
Then there's Natural Language Processing (NLP). This is what gives AI the ability to read and understand human language. An NLP algorithm can comb through thousands of pages of a patient's clinical notes or the latest research papers, pulling out the most relevant details in a fraction of the time it would take a person.
AI’s ability to blend both breadth and depth of medical expertise is a game-changer. It can demonstrate clinical reasoning that, in many aspects, exceeds that of any single physician by analyzing patterns across millions of cases simultaneously.
The real magic happens when these technologies are integrated into the daily workflow of a clinic or hospital. As we'll explore, these foundational concepts are already being applied to solve real-world diagnostic challenges, making healthcare more effective and efficient for everyone.
How AI Learns to See What Doctors See
So, how does an algorithm learn to spot a tumor on a lung scan or flag the very first signs of diabetic retinopathy in an eye exam? It's not magic—it's a highly sophisticated training process that mirrors how human experts build their skills, just on a massive scale. At its core, AI learns by sifting through enormous datasets of medical information, gradually developing an "intuition" to recognize what seasoned doctors see.
The entire process starts with Machine Learning (ML). You can think of an ML model as an incredibly diligent medical student. It's handed a digital library containing millions of labeled medical images—some showing healthy tissue, others pointing out specific abnormalities. By studying example after example, it begins to pick up on the subtle textures, shapes, and patterns tied to certain conditions.
This isn't a one-and-done deal. The more data the model processes, the better its pattern recognition gets, much like a resident physician who gets sharper with every case file they review. This foundational skill is the engine behind everything from predicting patient outcomes to making clinical workflows more efficient through workflow automation.
Going Deeper with Neural Networks
For trickier diagnostic challenges, we need a more powerful approach called Deep Learning. This method uses complex structures known as neural networks, which are loosely modeled after the interconnected neurons in our own brains. This design allows the AI to "see" and understand images with a much greater level of nuance.
Instead of just spotting basic patterns, a deep learning model can process layers of information within a single image. It might identify the main anomaly, evaluate the tissue around it, and even check that visual data against information pulled from the patient's electronic health record. This multi-layered analysis is what allows AI to reach, and sometimes exceed, specialist-level accuracy in many imaging tasks.
The infographic below shows just how dominant this application is.
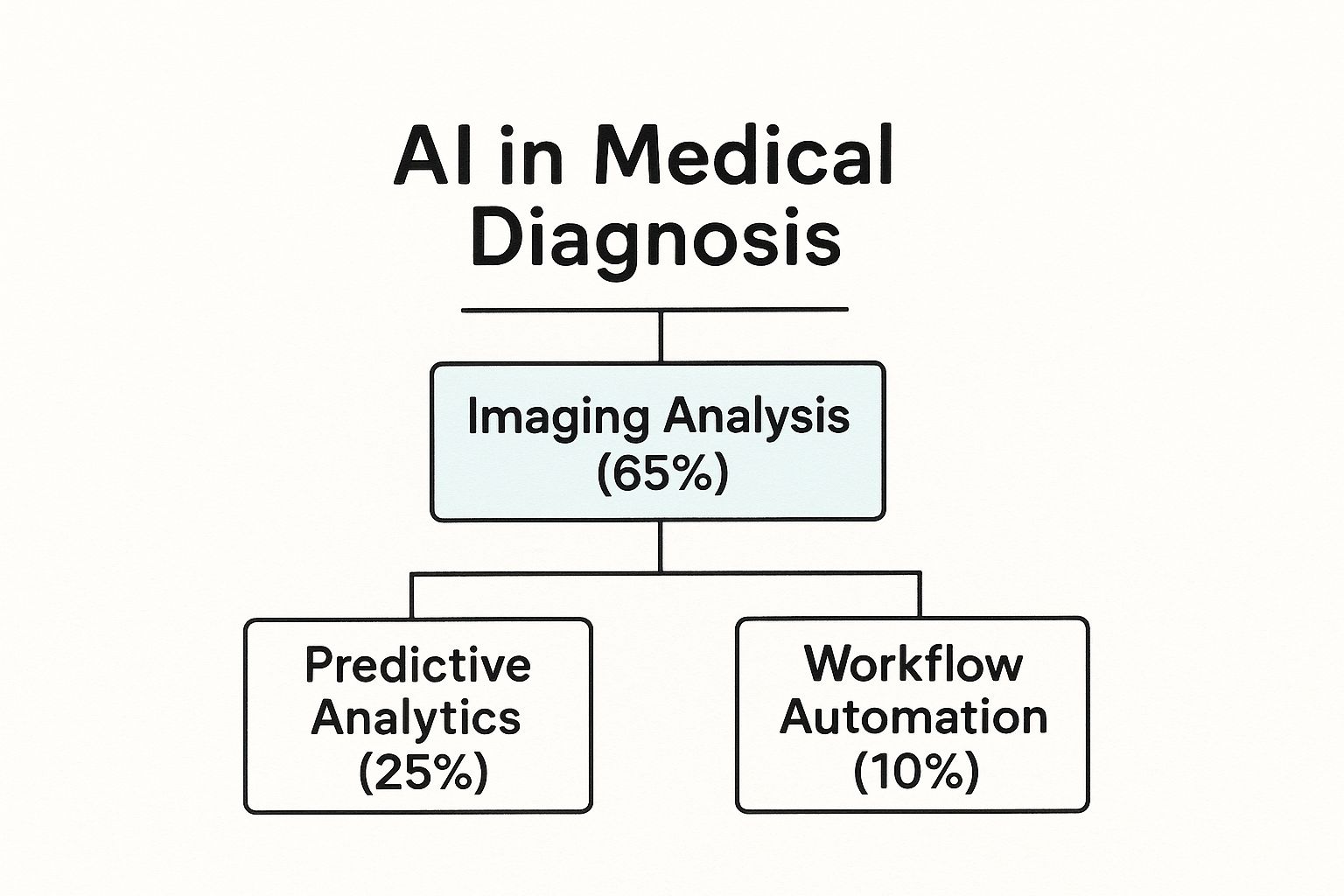
As you can see, most of the focus in diagnostic AI right now is on making sense of visual medical data, which is exactly where deep learning truly shines.
Understanding the Doctor's Notes
Images are only one part of the puzzle. A goldmine of diagnostic information is often locked away in unstructured text—think clinical notes, research articles, and years of patient histories. This is where Natural Language Processing (NLP) steps in. NLP acts as a smart translator, giving AI the ability to read, understand, and pull key insights out of human language.
An NLP algorithm can scan a patient's entire medical record from the last decade in seconds, piecing together symptom timelines or identifying potential drug interactions that a person might easily miss. This ability turns messy, text-based data into structured, usable information for a far more complete diagnostic picture. Seeing how AI for medical imaging and diagnostics is implemented gives a clearer view of its practical power.
When you combine the visual analysis from deep learning with the contextual understanding from NLP, AI systems can build a holistic view of a patient’s health that’s far richer than what any single data source could offer on its own.
Together, these technologies—Machine Learning, Deep Learning, and NLP—are the essential building blocks of diagnostic AI. They work in concert to create tools that can see, learn, and reason, ultimately amplifying the skills of human clinicians and giving them a powerful partner in patient care.
Real-World Wins AI Is Delivering Today
Theory is one thing, but the real test of AI in medical diagnosis is what it can do in a busy clinic. The good news is that AI is already delivering some incredible wins, fundamentally changing how we approach patient care by making diagnostics faster, more accurate, and far more efficient. These aren't just ideas on a whiteboard; they are active, real-world applications saving lives right now.
This isn't a niche trend anymore. We're seeing a massive shift, with roughly 80% of hospitals already using AI to improve how they care for patients and manage their operations. The results speak for themselves, especially in areas like cancer diagnostics, where AI tools have hit a remarkable 93% match rate when identifying malignancies. That's a huge step forward for early detection.
Radiology Reimagined
If you want to see where AI has made its biggest splash, look no further than radiology. Radiologists have the monumental task of poring over thousands of images, a process that requires intense focus and can be incredibly draining. AI algorithms essentially act as a highly-trained partner, spotting subtle patterns a human might miss after a long shift.
- Mammography: AI can detect the faintest hints of early-stage breast cancer, often flagging suspicious areas before they’re obvious to the human eye.
- Lung Scans: When looking at CT scans, AI is fantastic at finding tiny pulmonary nodules that could be the first sign of lung cancer, giving patients a crucial head start on treatment.
- Brain Scans: On an MRI, an AI can help spot signs of a stroke or tumor, allowing medical teams to prioritize the most critical cases and act faster.
This doesn't just boost accuracy; it dramatically cuts down the workload, letting radiologists focus their skills on the most challenging interpretations.
The goal isn't to replace the radiologist but to empower them. AI takes on the high-volume, repetitive work, freeing up human experts to do what they do best: solve complex medical puzzles and collaborate on patient care.
Pathology and Cardiology Enhanced
AI’s impact goes well beyond just imaging. In pathology, it’s completely changing how tissue samples are analyzed. What used to be a purely manual process of a pathologist scanning slides under a microscope can now be accelerated. An AI can pre-scan these slides, highlight suspicious areas, and even count different cell types, which shaves a huge amount of time off the diagnostic process.
Cardiology is seeing a similar leap, particularly in predicting problems before they happen. By analyzing electrocardiogram (ECG) data, AI models can pick up on subtle electrical patterns that signal a high risk of a future heart attack. This allows cardiologists to shift from reacting to a crisis to proactively treating patients to prevent one.
Specialized Fields Seeing Big Gains
AI's diagnostic muscle is also making waves in more specialized fields. Take ophthalmology, where an AI can now diagnose diabetic retinopathy—a primary cause of blindness—from a simple retinal photo. This can be done in a primary care office, making screening far more accessible and getting high-risk patients to a specialist sooner. In the same way, AI is helping dermatologists analyze skin lesions for signs of melanoma with more consistency.
A perfect example of this in action is the emergence of smart clinical assistants. An innovative tool like the Clinic AI Assistant helps manage patient records, flags potential issues that need a closer look, and handles administrative tasks. This gives doctors and nurses more time to focus on what truly matters—the patient in front of them. It's this practical integration of sophisticated AI that is pushing medicine into its next chapter.
The Measurable Impact on Patients and Providers
Moving AI into medical diagnosis isn't just a theoretical upgrade; it delivers tangible, real-world benefits for both patients and the people caring for them. The true impact is seen in better accuracy, huge gains in efficiency, and ultimately, improved health outcomes that also bolster a hospital's bottom line.
The numbers really speak for themselves. When AI systems are brought in to help crack complex diagnostic puzzles, the results can be stunning. For example, one recent study found that a sophisticated AI correctly diagnosed up to 85% of challenging cases from the New England Journal of Medicine. That's a rate over four times higher than what experienced physicians achieved on the same problems. It’s a powerful demonstration of how AI can sift through massive amounts of data to spot patterns the human eye might miss.
This isn't just an interesting academic finding. That kind of precision directly leads to catching diseases earlier and more accurately, which is the absolute foundation of effective treatment.
Boosting Diagnostic Accuracy and Speed
One of the biggest wins for AI in medical diagnosis is how it sharpens a clinician's accuracy. Picture it as getting a world-class second opinion in seconds, one that's been trained on millions of previous cases. This is a game-changer in fields like radiology and pathology, where the workload is crushing and the potential for human error from sheer fatigue is always a risk.
AI algorithms can scan medical images with a level of consistency that's hard to match, flagging tiny anomalies that might otherwise slip by. For patients, this translates into:
- Earlier detection of diseases like cancer, when the chances of successful treatment are highest.
- Fewer misdiagnoses, which helps avoid unnecessary, stressful procedures or critical delays in care.
- Quicker results, which can significantly reduce the anxiety that comes with waiting for answers.
This isn't just about better patient care; it also makes a provider's entire workflow smarter. By taking on the heavy lifting of initial, high-volume analysis, AI frees up specialists to pour their expertise into the most complex cases, spend more time with patients, and develop better treatment strategies.
Driving Operational Efficiency and Reducing Costs
Beyond the clinical improvements, AI brings serious operational advantages to the table. Automating routine diagnostic work allows healthcare facilities to handle a higher volume of cases with the same team, or even a smaller one. This is a direct answer to the pressing problems of staff shortages and burnout that plague the industry.
A key advantage is AI's ability to tackle diagnostic challenges more cost-effectively. Studies have shown that AI can often arrive at the right diagnosis with lower overall testing costs than traditional physician-led workups, cutting down on waste and putting resources where they're needed most.
These efficiencies add up to significant cost savings. By catching diseases in their early stages, AI helps drive down the enormous long-term treatment costs that come with advanced illness. At the same time, by making diagnostic workflows more efficient, it reduces the time and labor spent on each case, which allows for higher patient throughput and smarter resource management. This creates a powerful return on investment, making healthcare not just better, but more sustainable. Improving how healthcare professionals connect and collaborate, supported by tools like an HCP Engagement Co-pilot, can further streamline communication and operations within the hospital.
Navigating the Roadblocks to AI Adoption
For all the promise AI in medical diagnosis holds, the road to actually getting it into hospitals and clinics is far from smooth. We’re not just plugging in a new piece of software; we're weaving a powerful new technology into the fabric of one of the most complex, regulated, and human-centric fields there is. To successfully deploy any AI Solutions, we have to tackle these hurdles head-on.
The money pouring into this space shows just how high the stakes are. The AI in healthcare market was valued at $6.7 billion in 2020, jumped to $22.4 billion in 2023, and is expected to skyrocket to $208.2 billion by 2030. That kind of explosive growth tells you the pressure is on to solve these adoption problems, and fast. You can discover more insights about AI in healthcare trends to see the full picture.

Upholding Patient Data Privacy
Patient data is the fuel for any diagnostic AI, but it's also profoundly personal and protected. The first and arguably most important roadblock is data privacy. Healthcare systems have to thread a very fine needle, navigating a labyrinth of regulations like HIPAA to keep patient information locked down while still making it usable for training AI models.
This goes way beyond standard cybersecurity. We’re talking about sophisticated data anonymization techniques and building secure protocols that allow for data sharing without risking a breach. One mistake can shatter patient trust and bring on massive legal and financial penalties, which is why solid data governance has to be the top priority.
The Challenge of Algorithmic Bias
An AI algorithm is a reflection of the data it learns from. If that data isn't a fair and balanced representation of the real world, the AI will inherit its blind spots, creating biased and unreliable tools. This isn't just a technical problem; it's a massive ethical and clinical one.
An AI model trained mostly on data from one demographic might stumble when trying to diagnose conditions in another. This can easily reinforce or even amplify existing health disparities, completely undercutting the goal of making care more equitable for everyone.
Fighting this means making a serious commitment to gathering diverse, high-quality datasets. This often pushes different institutions to collaborate and pool their data to build something more representative. Dealing with bias isn't a simple fix; it’s a foundational requirement for any AI you hope to trust. Every part of the AI Product Development Workflow must have checkpoints for finding and rooting out bias.
Overcoming Technical Integration Hurdles
Let’s be honest: many hospitals and clinics are running on older IT systems that were never built to talk to a modern AI platform. This creates a huge technical barrier. Getting new AI tools to work means either overhauling these legacy systems or building complex "bridges" to connect them—both of which can be incredibly expensive and disruptive.
For AI to be useful, data has to flow effortlessly between electronic health records (EHRs), imaging archives (like PACS), and the AI models themselves. If that connection isn't seamless, the AI becomes an isolated tool that nobody can fit into their daily workflow. Many organizations find they need to bring in experts in healthcare software development to make these connections actually work.
Navigating the Regulatory Landscape
Finally, you can't just launch a diagnostic AI tool. It has to pass muster with strict regulatory bodies like the FDA. Getting that approval is a long, demanding journey where you have to prove, through extensive clinical validation, that your tool is safe, accurate, and truly effective.
The world of regulatory compliance for medical devices is notoriously complex and always changing. Staying on the right side of the rules requires deep expertise and obsessive documentation from the first line of code to the final rollout. For any organization serious about using these tools, understanding and planning for these regulatory demands isn't optional—it's absolutely essential.
What's Next for Diagnostic AI
Looking down the road, the relationship between doctors and AI in medical diagnosis is poised to become much more seamless and collaborative. The future isn't about AI taking over; it's about amplifying a clinician's own expertise with smarter tools that work alongside them. This next generation of innovation is all about building a richer, clearer picture of a patient's health.
One of the biggest leaps forward is the move toward multimodal AI. Think about an AI that doesn't just analyze a CT scan on its own. Instead, it pulls together insights from medical images, genetic markers, recent lab results, and even the doctor's handwritten notes. This creates a truly holistic view, connecting subtle clues that a human might miss and providing an analysis that mirrors the real complexity of a patient's condition.
The Push for Explainable and Trustworthy AI
Another crucial area of development is Explainable AI (XAI). For a long time, one of the biggest roadblocks to widespread adoption has been the "black box" problem—the AI gives an answer, but nobody can see how it got there. XAI is designed to crack open that box and show the reasoning behind its conclusions. This kind of transparency is absolutely essential for building trust and giving doctors the confidence to lean on AI-driven insights.
The goal is a human-centric model where technology acts as a trusted advisor, not the final word. Getting there requires a thoughtful game plan. For any organization looking to pioneer this future, creating a Custom AI Strategy report is the non-negotiable first step. It’s all about meshing what the technology can do with what clinicians actually need, a point we explored in our AI adoption guide.
While AI models show great promise, their performance still requires human oversight. A recent meta-analysis of 83 studies found that generative AI achieved an overall diagnostic accuracy of 52.1%. While comparable to non-expert physicians, this was significantly lower than the accuracy of expert physicians.
This statistic really drives home why the collaborative model is so important. You can read the full research about these findings to get a deeper understanding of why the human-AI partnership is here to stay. Bringing these advanced tools into a clinical setting is complex, and it often takes guidance from our expert team to navigate the implementation and ensure the technology truly empowers clinical judgment.
FAQs About the Future of Diagnostic AI
How will AI change a doctor's daily job?
AI is set to take over much of the grunt work—the routine data sifting and administrative burdens. This will free up doctors to focus on what they do best: tackling complex cases, connecting with patients, and crafting nuanced treatment plans. It will simply become another piece of their internal tooling, as fundamental as the stethoscope.
Will patients interact directly with diagnostic AI?
Yes, that’s already starting to happen. We'll see more patient-facing AI tools for business for things like symptom checking, booking appointments, or helping manage chronic diseases. But when it comes to an official diagnosis and treatment plan, a human doctor will always be the one making the final call.
What is the single biggest trend to watch in diagnostic AI?
Without a doubt, it’s the shift from reactive to proactive care. Instead of just diagnosing diseases that are already present, the next wave of AI will focus on identifying patients at high risk of developing a condition before symptoms even appear. This opens the door for early interventions that could prevent illnesses from ever taking hold.
Common Questions We Hear
As we wrap up this deep dive into AI's role in medical diagnosis, let's tackle some of the most common questions people ask. These answers should clear up any lingering confusion and put AI’s place in healthcare into perspective.
Is AI Going to Replace Doctors and Radiologists?
Not at all. The goal isn't replacement; it's collaboration.
Think of diagnostic AI as an incredibly sharp co-pilot for a physician. It can sift through mountains of data and spot subtle patterns far faster than any human ever could. This frees up doctors and radiologists to do what they do best: focus on nuanced cases, connect with patients, and craft comprehensive treatment plans.
The future is a partnership where a clinician’s irreplaceable expertise is amplified by intelligent technology. The result? Faster, more accurate care for everyone.
What Are the Biggest Risks We Should Worry About?
Like any powerful tool, AI comes with its own set of challenges. The main concerns really boil down to three things: algorithmic bias, data privacy, and the "black box" problem.
- Algorithmic Bias: If an AI model is trained on data that doesn't represent diverse patient populations, it can become less accurate for underrepresented groups. This is a serious issue that could accidentally widen existing health disparities.
- Data Privacy: We're talking about incredibly sensitive patient information here. Protecting it from breaches requires iron-clad security measures and a constant focus on data governance.
- The 'Black Box' Problem: Sometimes, even the creators of a complex AI can't fully explain how it reached a specific conclusion. For a doctor to trust an AI's recommendation, they need to understand its reasoning.
The good news is that the industry is actively working on these problems. The solutions lie in building more diverse training datasets, implementing robust cybersecurity, and pushing for "explainable AI" (XAI) that can actually show its work.
How Can a Hospital Get Started with Diagnostic AI?
The key is to think big but start small. Jumping into a massive, hospital-wide AI overhaul is a recipe for disaster.
Instead, a much smarter approach is to pick one specific, high-impact problem to solve first. Maybe it's reducing the backlog for radiology readings or improving the accuracy of initial cancer screenings. Find a pain point where AI can deliver a clear win.
From there, run a pilot project. Test the technology in a controlled setting, measure its real-world performance, and—most importantly—get feedback from the clinical staff who will actually use it. This proves the concept and helps build buy-in.
Working with specialists who offer AI strategy consulting can be a game-changer here. They can help you build a practical roadmap that ensures the technology integrates smoothly with your existing workflows and delivers real value.
Ready to see how AI can elevate your organization's diagnostic capabilities? At Ekipa, we specialize in turning AI opportunities into scalable impact. Discover our AI Solutions and meet our expert team today.