10 AI in Medical Field Examples You Should Know
Discover the top 10 AI in medical field examples strategies and tips. Complete guide with actionable insights.
The application of artificial intelligence in the medical field is no longer a futuristic concept; it's a present-day reality transforming patient outcomes, operational efficiency, and research capabilities. This article moves beyond theoretical discussions to provide a curated, actionable collection of real-world ai in medical field examples. For business leaders, CTOs, and AI strategists, understanding these applications is crucial for identifying strategic opportunities and avoiding costly missteps in implementation.
This is not a list of generic success stories. Instead, we offer a strategic breakdown of 10 impactful use cases across diagnostics, clinical care, research, and patient engagement. Each example is analyzed through a business lens, detailing not just what the AI does, but how it achieves results. We'll explore the specific data inputs required, key implementation considerations, and the measurable KPIs you should track to gauge success. To truly understand the advancements, it's beneficial to explore how professionals can leverage AI for academic research, which often pioneers these clinical applications.
Readers will gain a comprehensive understanding of how to translate these real-world use cases into a viable roadmap for their own organizations. From enhancing diagnostic accuracy with AI-powered image analysis to optimizing hospital workflows through predictive analytics, this guide provides the tactical insights needed to develop a robust AI strategy consulting framework. You will leave with a clear picture of what’s possible, what it takes to get there, and how to measure the return on your technology investment.
1. Medical Image Analysis and Diagnostics
Medical image analysis is one of the most impactful and mature ai in medical field examples. This application uses sophisticated deep learning algorithms, particularly Convolutional Neural Networks (CNNs), to analyze medical scans like X-rays, CT scans, and MRIs. These AI models are trained on vast, labeled datasets to identify patterns indicative of diseases such as cancerous tumors, neurological disorders, or diabetic retinopathy, often with a speed and accuracy that surpasses human capability.

The primary goal is to augment the radiologist's workflow, not replace it. By highlighting potential areas of concern, the AI acts as a second set of eyes, reducing diagnostic errors and significantly cutting down the time required to read a scan. For healthcare providers, this translates into higher patient throughput, earlier disease detection, and improved treatment outcomes. Industry leaders like Google Health and Siemens Healthineers have developed FDA-approved algorithms that demonstrate this potential in real-world clinical settings. For a deeper dive into how these systems are built, explore specialized platforms for Medical Image Analysis and Diagnostics.
Strategic Implementation and KPIs
Why Use It: Implement this AI application to increase diagnostic accuracy, reduce radiologist burnout by automating repetitive tasks, and enable earlier, more effective patient interventions. It's ideal for high-volume imaging departments looking to optimize resource allocation and improve clinical quality.
Actionable Tips:
Start Small: Begin with an AI model focused on a single, high-prevalence pathology before expanding to multi-disease detection systems.
Ensure Data Diversity: Your training data must reflect the demographic diversity of your patient population to avoid algorithmic bias and ensure equitable performance.
Human-in-the-Loop: Always maintain a human-in-the-loop validation process. A radiologist must confirm AI-driven findings to ensure quality assurance and accountability.
Key Performance Indicators (KPIs):
Diagnostic Accuracy: Measure the model's sensitivity, specificity, and Area Under the Curve (AUC) score.
Turnaround Time (TAT): Track the average time from scan acquisition to final report delivery.
Radiologist Productivity: Monitor the number of scans interpreted per radiologist per day.
2. Drug Discovery and Development
Accelerating the pharmaceutical pipeline is a monumental challenge, making AI's role in this area one of the most transformative ai in medical field examples. This application leverages machine learning and deep learning to analyze complex biological data, predict molecular interactions, and identify promising drug candidates at unprecedented speeds. AI models can screen billions of compounds virtually (in silico), predicting their efficacy, toxicity, and binding affinity to specific protein targets, drastically reducing the time and cost associated with traditional R&D.
The goal is to compress the drug development timeline, which traditionally takes over a decade and costs billions. By identifying viable candidates faster and predicting failures earlier, AI minimizes resource-intensive lab experiments. Companies like Insilico Medicine and Exscientia have pioneered this space, using generative AI to design novel molecules from scratch and even advancing AI-designed drugs into human clinical trials. Similarly, DeepMind's AlphaFold has revolutionized biology by accurately predicting protein structures, a crucial step in understanding disease mechanisms and designing targeted therapies.
Strategic Implementation and KPIs
Why Use It: Implement this AI application to dramatically reduce R&D costs and timelines, increase the success rate of drug candidates, and gain a competitive edge by focusing on unmet medical needs. It is essential for pharmaceutical companies and biotech startups aiming to innovate faster and bring life-saving therapies to market more efficiently.
Actionable Tips:
Combine AI and Chemistry: Integrate AI models with traditional computational chemistry methods to enhance prediction accuracy and leverage established scientific principles.
Validate Experimentally: Always use AI-driven predictions as a starting point. Subsequent experimental validation in the lab is crucial for confirming a compound's viability.
Focus on Unmet Needs: Direct your AI discovery efforts toward diseases with limited treatment options to maximize impact and secure a stronger market position.
Key Performance Indicators (KPIs):
Time-to-Candidate: Measure the average time from project initiation to the identification of a preclinical drug candidate.
Hit Rate: Track the percentage of screened compounds that meet the predefined criteria for a successful "hit."
R&D Cost Reduction: Calculate the cost savings achieved per development phase compared to traditional non-AI benchmarks.
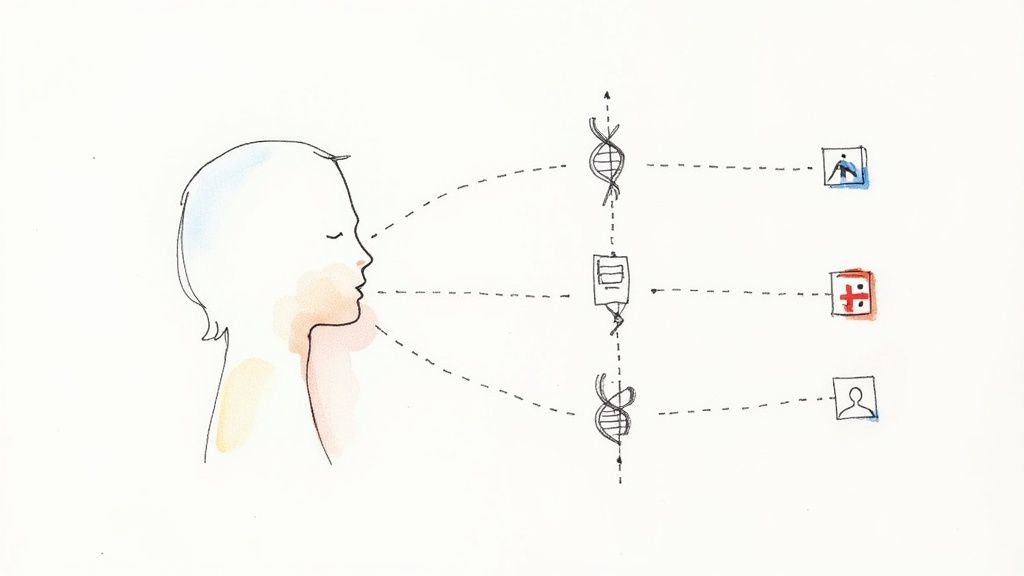
3. Personalized Treatment Recommendations
Personalized treatment recommendation is a transformative application and one of the most promising ai in medical field examples. This approach leverages advanced machine learning models to sift through vast datasets, including a patient's genetic profile, medical history, lifestyle factors, and clinical trial outcomes. The AI identifies subtle patterns to predict which therapies will be most effective for an individual, moving healthcare from a one-size-fits-all model to true precision medicine.
The core objective is to tailor medical interventions to the unique characteristics of each patient, maximizing efficacy while minimizing adverse effects. This is particularly impactful in complex fields like oncology, where companies such as Tempus and Foundation Medicine use AI to analyze tumor genomics and suggest targeted therapies. By matching treatments to specific molecular signatures, these platforms provide oncologists with data-driven insights, leading to more effective, personalized care plans and better patient outcomes. Building such a system requires deep expertise in both AI and custom healthcare software development.
Strategic Implementation and KPIs
Why Use It: Implement this technology to enhance treatment efficacy, reduce the costs associated with ineffective trial-and-error therapies, and accelerate the adoption of precision medicine. It is crucial for specialty clinics, oncology centers, and research hospitals aiming to deliver cutting-edge, patient-centric care.
Actionable Tips:
Integrate Diverse Data: Combine genomic data from sequencing with clinical data from Electronic Health Records (EHRs) to create a comprehensive patient profile.
Prioritize Explainability: Use explainable AI (XAI) models to show clinicians the "why" behind a recommendation, fostering trust and encouraging adoption.
Involve Multidisciplinary Teams: Establish review boards, such as tumor boards, where clinicians can validate and discuss AI-generated recommendations in a collaborative setting.
Key Performance Indicators (KPIs):
Treatment Efficacy Rate: Measure the percentage of patients showing a positive response to AI-recommended therapies.
Time to Optimal Treatment: Track the average time from diagnosis to the start of the most effective treatment plan.
Adverse Event Reduction: Monitor the decrease in side effects or negative reactions compared to standard treatment protocols.
4. Virtual Health Assistants and Chatbots
Virtual Health Assistants represent one of the most patient-facing ai in medical field examples, shifting how individuals access initial care and manage their health. These AI-powered conversational agents use advanced Natural Language Processing (NLP) to understand patient inquiries, assess symptoms, provide reliable health information, and even offer medication reminders. They serve as a scalable first point of contact, improving access to care while reducing the burden on human clinicians.
These systems are designed to handle a high volume of routine queries, freeing up medical professionals to focus on more complex cases. Leading platforms like Ada Health and Babylon Health provide sophisticated symptom checkers, while specialized bots like Woebot offer crucial mental health support. By integrating these tools, healthcare organizations can offer 24/7 assistance, enhance patient engagement, and streamline the triage process, guiding users to the appropriate level of care. You can explore building similar solutions with a specialized Clinic AI Assistant.
Strategic Implementation and KPIs
Why Use It: Implement this technology to improve patient access and engagement, reduce administrative overhead, and provide continuous support for chronic disease management. It is ideal for healthcare systems aiming to lower call center volumes, improve patient satisfaction, and offer accessible mental health resources.
Actionable Tips:
Prioritize a Clear Escalation Path: Always ensure the chatbot can seamlessly transfer a patient to a human provider, especially when serious symptoms are detected.
Communicate AI Limitations: Be transparent with users. Include clear disclaimers that the assistant does not provide a formal diagnosis and is for informational purposes only.
Ensure Data Compliance: Strictly adhere to HIPAA and GDPR regulations for handling sensitive patient data to build trust and avoid legal penalties.
Key Performance Indicators (KPIs):
Patient Engagement Rate: Measure the number of active users and the frequency of interactions per user.
Symptom Checker Accuracy: Track the percentage of times the AI's triage recommendation aligns with a clinician's final assessment.
Reduction in Call Center Volume: Monitor the decrease in routine calls handled by human agents after chatbot implementation.
5. Predictive Analytics for Disease Prevention
Predictive analytics is a transformative entry among ai in medical field examples, shifting the focus from reactive treatment to proactive prevention. This application leverages machine learning models to analyze vast datasets, including electronic health records (EHRs), genomic data, biomarkers, and lifestyle factors. By identifying subtle patterns and correlations, these AI systems can forecast an individual's risk of developing chronic conditions like heart disease, diabetes, or sepsis long before symptoms appear.
The core objective is to empower clinicians with foresight, enabling them to intervene early with personalized prevention plans. For example, identifying a patient at high risk for a cardiovascular event can trigger targeted lifestyle recommendations, medication adjustments, and more frequent monitoring. Organizations like Optum and Google DeepMind have demonstrated success in predicting patient deterioration and cardiovascular risk, respectively. This proactive approach helps healthcare systems improve population health outcomes, reduce hospitalization rates, and lower long-term care costs. For a closer look at how these systems are architected, explore our guide on the AI Product Development Workflow.
Strategic Implementation and KPIs
Why Use It: Implement predictive analytics to transition your healthcare model from reactive to preventive. It is ideal for large health systems, accountable care organizations (ACOs), and insurers aiming to manage population health risks, reduce costs associated with chronic diseases, and improve patient quality of life.
Actionable Tips:
Validate Models Rigorously: Ensure predictive models are validated across diverse patient populations to prevent algorithmic bias and confirm their accuracy for your specific demographics.
Integrate with Clinical Workflows: Embed risk scores and alerts directly into the EHR system to provide clinicians with actionable insights at the point of care without disrupting their workflow.
Prioritize Patient Communication: Develop clear protocols for communicating risk predictions to patients. Frame the conversation around shared decision-making and empowering them with preventive strategies.
Key Performance Indicators (KPIs):
Model Predictive Accuracy: Measure the model's AUC (Area Under the Curve), precision, and recall for specific disease predictions.
Reduction in Disease Incidence: Track the rate of new diagnoses for targeted conditions (e.g., Type 2 diabetes) within the high-risk patient cohort.
Healthcare Cost Avoidance: Calculate the estimated savings from prevented hospital admissions, emergency visits, and chronic disease treatments.
6. Pathology and Histopathology Image Analysis
Digital pathology represents another frontier where AI is making a significant impact, making it a crucial component in any list of ai in medical field examples. This application uses deep learning algorithms to analyze whole-slide images (WSIs) of tissue samples, identifying cellular and morphological patterns that are invisible to the human eye. The AI can detect and classify cancerous cells, grade tumors, and quantify biomarkers with exceptional precision, assisting pathologists in making more accurate and consistent diagnoses.
AI models are trained on vast digital archives of annotated pathology slides to recognize subtle features indicative of disease. The technology's primary role is to augment the pathologist's expertise by automating time-consuming tasks like cell counting and highlighting suspicious regions for review. This not only increases diagnostic speed but also enhances objectivity by providing quantitative data to support qualitative assessments. Companies like PathAI and Proscia are at the forefront, developing platforms that integrate seamlessly into existing laboratory workflows, ultimately leading to better-informed treatment decisions and improved patient prognoses. For those looking to build similar sophisticated AI tools for business, understanding the underlying data and workflow is key.
Strategic Implementation and KPIs
Why Use It: Implement AI in pathology to improve diagnostic consistency, accelerate slide review times, and unlock new prognostic insights from tissue samples. It is particularly valuable for high-volume labs and research institutions aiming to standardize analysis and support precision medicine initiatives.
Actionable Tips:
Standardize Pre-Analytics: Ensure consistent tissue staining and digital scanning protocols across all samples. High-quality, standardized data is the foundation of an effective AI pathology model.
Integrate with LIS: Plan for seamless integration with your existing Laboratory Information System (LIS) to streamline workflows from slide scanning to final report generation.
Phased Rollout: Begin by using AI as a quality assurance tool or for second opinions on challenging cases before deploying it for primary diagnostic screening.
Key Performance Indicators (KPIs):
Diagnostic Concordance: Measure the agreement rate between AI-assisted diagnoses and the consensus diagnosis of expert pathologists.
Slide Review Time: Track the average time a pathologist spends per case with and without AI assistance.
Biomarker Quantification Accuracy: Evaluate the AI's precision in quantifying markers (e.g., Ki-67, PD-L1) compared to manual methods.
7. Clinical Decision Support Systems
AI-enhanced Clinical Decision Support Systems (CDSS) are a critical example of ai in medical field examples integrated directly into the clinical workflow. These systems act as an intelligent co-pilot for physicians, analyzing vast amounts of patient data from Electronic Health Records (EHRs) alongside the latest medical literature and clinical guidelines. The goal is to provide real-time, evidence-based recommendations at the point of care, suggesting potential diagnoses, optimizing treatment plans, and flagging dangerous drug-drug interactions.
These systems are not just theoretical; they are actively deployed in hospitals worldwide. For instance, many EHRs, like those from Epic Systems, feature integrated sepsis alert systems that continuously monitor patient vitals and lab results to predict the onset of sepsis, a life-threatening condition. Similarly, IBM Watson for Clinical Trial Matching helps oncologists find suitable clinical trials for their patients by analyzing patient data against complex trial eligibility criteria. The core value lies in augmenting human expertise, ensuring patient safety, and promoting adherence to best practices.
Strategic Implementation and KPIs
Why Use It: Implement an AI-powered CDSS to standardize care quality, reduce medical errors, and improve patient outcomes. It is particularly valuable in high-stress, complex environments like emergency departments or intensive care units where timely, data-driven decisions are paramount. This application helps organizations manage risk and ensure care aligns with the latest evidence.
Actionable Tips:
Minimize Alert Fatigue: Design alerts to be highly specific and clinically relevant. Overloading clinicians with low-priority notifications can lead to them being ignored.
Ensure Transparency: Make the system's recommendations explainable. Clinicians are more likely to trust and adopt a tool if they understand the reasoning behind its suggestions.
Integrate Seamlessly: Embed the CDSS directly within existing EHR workflows to avoid disrupting established processes and requiring clinicians to switch between applications.
Key Performance Indicators (KPIs):
Adverse Event Rate: Track the reduction in preventable medical errors, such as adverse drug events.
Adherence to Guidelines: Measure the percentage of cases where care aligns with evidence-based clinical protocols.
Clinician Adoption Rate: Monitor the frequency and consistency with which physicians use and follow the system's recommendations.
8. Medical Imaging Registration and Segmentation
Beyond initial diagnostics, AI offers profound value in the precise manipulation of medical images through registration and segmentation. This application uses advanced deep learning models to automatically align multiple images from different scans or time points (registration) and to delineate specific anatomical structures like organs, tissues, or tumors (segmentation). This automation is a critical step in modern medical workflows, enabling complex procedures like 3D reconstructions for surgical planning, targeted radiation therapy, and longitudinal monitoring of disease progression.
The goal is to eliminate the time-consuming and often variable manual work of clinicians tracing structures on scans. By providing consistent, rapid, and accurate segmentations, these ai in medical field examples create a foundation for quantitative analysis and personalized treatment. Major industry platforms like NVIDIA's Clara and Siemens' syngo.AI platform offer powerful tools that are integrated directly into clinical systems, demonstrating the technology's maturity. Building such systems often requires a robust AI Product Development Workflow to ensure clinical accuracy and seamless integration.
Strategic Implementation and KPIs
Why Use It: Implement this AI to significantly accelerate pre-operative planning, improve the precision of radiation oncology, and provide objective, quantitative data for tracking treatment response. It is invaluable for oncology, cardiology, and neurology departments that rely on precise anatomical measurements.
Actionable Tips:
Validate Against Gold Standards: Regularly benchmark the AI model's output against manual segmentations performed by expert clinicians to ensure continued accuracy and reliability.
Account for Anatomical Variation: Train models on diverse datasets that include a wide range of anatomical variations and pathologies to build robust and generalizable systems.
Maintain Physician Oversight: Always implement a final review step where a clinician can validate or adjust the AI-generated segmentation before it is used for clinical decision-making.
Key Performance Indicators (KPIs):
Segmentation Accuracy: Measure performance using metrics like the Dice Similarity Coefficient (DSC) and Intersection over Union (IoU).
Processing Time: Track the time taken from image upload to the delivery of the final segmented model.
Manual Adjustment Rate: Monitor the percentage of AI-generated segmentations that require manual correction by a clinician.
9. Hospital Operations and Workflow Optimization
Efficiently managing a hospital is a monumental task, making workflow optimization one of the most practical ai in medical field examples. This application uses predictive analytics and machine learning to streamline everything from patient flow and bed management to operating room scheduling and staff allocation. By analyzing historical data on admissions, discharges, and departmental bottlenecks, AI models can forecast demand and suggest real-time adjustments.
The goal is to create a "smart hospital" that anticipates needs before they become critical. This proactive approach reduces patient wait times, minimizes overcrowding in emergency departments, and ensures resources like surgical suites are used to their full capacity. Optimizing these processes is paramount, and it often involves leveraging HIPAA-ready data analysis tools that scale for healthcare outcomes to ensure both efficiency and compliance. Leaders like Qventus and GE Healthcare have demonstrated significant reductions in patient length of stay and improved operational margins by implementing these systems. For a deeper look at the underlying technology, explore an AI-powered data extraction engine.
Strategic Implementation and KPIs
Why Use It: Implement this AI application to decrease operational costs, improve patient satisfaction through reduced wait times, and enhance staff productivity. It's ideal for healthcare systems struggling with capacity constraints, scheduling inefficiencies, or unpredictable patient surges.
Actionable Tips:
Pilot a Single Department: Start with a specific, high-impact area like the emergency department or a surgical unit to demonstrate value before a hospital-wide rollout.
Involve Clinical Staff: Engage nurses, doctors, and administrators in the planning process to ensure the AI solution addresses their real-world pain points and integrates smoothly into their routines.
Continuous Feedback Loop: Regularly monitor model performance and gather feedback from end-users to make iterative improvements and adjustments.
Key Performance Indicators (KPIs):
Patient Wait Times: Measure the average time from patient arrival to being seen in the emergency department or admitted.
Bed Occupancy Rate: Track the percentage of occupied beds versus total capacity to monitor utilization.
Operating Room (OR) Utilization: Analyze the percentage of time operating rooms are actively in use for surgical procedures.
10. Mental Health and Psychiatric Assessment
Mental health assessment is a profoundly impactful and growing area among ai in medical field examples. This application leverages AI, particularly Natural Language Processing (NLP) and machine learning, to analyze patient speech patterns, text-based communications, facial expressions, and other digital biomarkers. These AI systems can identify subtle cues and patterns associated with conditions like depression, anxiety, or psychosis, offering an objective layer of data to complement traditional clinical interviews.
The core objective is to provide clinicians with scalable, accessible tools for screening and monitoring mental health. By analyzing data from apps, wearables, or even telehealth sessions, AI can help detect early warning signs of a mental health crisis or track a patient's response to treatment over time. For providers, this leads to earlier interventions, personalized care plans, and improved management of mental health conditions, ultimately making care more proactive and accessible. Companies like Woebot and Mindstrong are pioneering these AI-driven approaches, demonstrating their potential to augment psychiatric care.
Strategic Implementation and KPIs
Why Use It: Implement this AI application to increase the accessibility of mental health screening, provide continuous monitoring for at-risk patients, and reduce the burden on overloaded mental health professionals. It is ideal for healthcare systems, insurers, and employers looking to offer scalable mental health support and improve early detection rates.
Actionable Tips:
Prioritize Clinician Oversight: AI tools should always be used to support, not replace, a qualified mental health professional. Human oversight is critical for accurate diagnosis and compassionate care.
Establish Crisis Protocols: Ensure any AI tool has a clear, built-in protocol for escalating cases where acute risk (e.g., self-harm) is detected, connecting the user to immediate human support.
Ensure Data Privacy and Transparency: Be transparent with users about how their data is being collected and analyzed. Adhere to strict data privacy regulations like HIPAA to build trust and ensure ethical implementation.
Key Performance Indicators (KPIs):
Screening Accuracy: Measure the tool's sensitivity and specificity in identifying individuals at risk for specific mental health conditions compared to clinical diagnoses.
User Engagement Rates: Track metrics like daily active users, session length, and retention to gauge the tool's utility and user acceptance.
Time to Intervention: Monitor the average time it takes from an AI-detected risk flag to a clinician-led intervention.
AI in Healthcare: 10 Use-Case Comparison
| Application | Implementation complexity | Resource requirements | Expected outcomes | Ideal use cases | Key advantages |
|---|---|---|---|---|---|
| Medical Image Analysis and Diagnostics | High — deep CNNs, PACS integration, regulatory hurdles | Large labeled imaging datasets, GPUs, radiologist oversight | Improved diagnostic accuracy and faster reads; scalable screening | Radiology screening, emergency triage, oncology imaging | Higher detection rates, reduced radiologist workload, consistent performance |
| Drug Discovery and Development | Very high — molecular models, simulation, wet‑lab linkage | HPC/cluster compute, proprietary molecular data, chemistry expertise | Faster candidate identification; reduced time and R&D cost | Lead discovery, protein folding, ADMET prediction, trial simulation | Accelerates R&D, finds novel candidates, cost and time savings |
| Personalized Treatment Recommendations | High — genomic integration, explainability, clinical validation | Genomic + clinical datasets, EHR integration, specialist input | Better treatment efficacy, fewer adverse events, tailored plans | Oncology, rare diseases, pharmacogenomics, precision medicine | Tailored therapy selection, improved outcomes, optimized adherence |
| Virtual Health Assistants and Chatbots | Moderate — NLP, user flows, optional EHR hooks | Conversational datasets, moderate compute, privacy/compliance controls | Increased access, instant responses, reduced admin burden | Symptom triage, medication reminders, basic mental health support | 24/7 availability, scalable patient engagement, cost‑effective support |
| Predictive Analytics for Disease Prevention | High — longitudinal models, SDOH and biomarker fusion | Large longitudinal datasets, analytics platforms, data governance | Early risk identification, reduced incidence and long‑term costs | Population health, primary care prevention, chronic disease screening | Enables early interventions, targets high‑risk groups, cost reduction |
| Pathology and Histopathology Image Analysis | High — whole slide analysis, standardization, validation | Digitized slides, high compute, staining and QC procedures | Very high diagnostic accuracy, faster pathology reporting | Cancer diagnosis, tumor grading, surgical pathology | Quantitative metrics, reduced variability, scalable high‑volume analysis |
| Clinical Decision Support Systems | Moderate–High — guideline encoding, EHR real‑time integration | Clinical data, knowledge bases, real‑time compute and UX design | Improved decision quality, fewer medication errors, guideline adherence | Point‑of‑care recommendations, drug interaction checks, sepsis alerts | Evidence‑based suggestions, error reduction, supports clinician decisions |
| Medical Imaging Registration and Segmentation | High — deformable registration, multi‑modal fusion | Annotated imaging datasets, GPUs, validation cohorts | Rapid accurate segmentation, improved surgical and RT planning | Surgical planning, radiation therapy targeting, longitudinal tracking | Saves manual effort, precise targeting, enables 3D reconstruction |
| Hospital Operations and Workflow Optimization | Moderate — forecasting models, system integration, change mgmt | Operational and scheduling data, analytics platform, stakeholder buy‑in | Reduced wait times, better resource utilization, lower costs | Bed/OR scheduling, staffing optimization, ED flow management | Operational efficiency, improved utilization, increased patient satisfaction |
| Mental Health and Psychiatric Assessment | Moderate–High — multimodal signals, ethical safeguards | Behavioral and speech datasets, NLP/vision tools, clinician oversight | Earlier detection, objective monitoring, improved access to screening | Screening, monitoring treatment response, crisis risk detection | Scalable screening, objective biomarkers, expands access to care |
Final Thoughts
The journey through these diverse ai in medical field examples reveals a clear and transformative narrative: artificial intelligence is no longer a futuristic concept but a present-day catalyst for a more precise, efficient, and personalized era of healthcare. From accelerating drug discovery and refining diagnostic accuracy in medical imaging to optimizing hospital workflows and providing personalized treatment recommendations, AI is fundamentally reshaping every facet of the medical landscape.
What we've seen across these applications is not just technological prowess but a strategic shift in how healthcare challenges are approached. The examples demonstrate a move from reactive, one-size-fits-all models to proactive, data-driven systems that can predict, personalize, and streamline care at an unprecedented scale.
Key Strategic Takeaways for Healthcare Leaders
As you consider integrating AI into your operations, several core themes from our analysis should guide your strategy:
Data is the Bedrock: The success of every example, from predictive analytics to pathology image analysis, hinges on high-quality, well-structured, and relevant data. A robust data governance and acquisition strategy is the non-negotiable first step.
Integration Over Isolation: The most impactful AI solutions are not standalone novelties. They are deeply integrated into existing clinical workflows, augmenting the capabilities of healthcare professionals without causing disruption. Think of AI as an intelligent layer within your current systems, not a replacement for them. This approach to building better internal tooling is critical for adoption.
Focus on Actionable Insights: AI's value isn't in generating complex algorithms; it's in delivering clear, actionable insights that lead to better decisions. Whether for a clinician choosing a treatment path or an administrator optimizing bed allocation, the output must be intuitive and directly support a specific action or decision. As we explored in our guide to real-world use cases, the best applications solve tangible problems.
Your Actionable Next Steps
The potential is immense, but realizing it requires a deliberate and strategic approach. Here’s how you can move from understanding these examples to implementing your own solutions:
Identify High-Impact Use Cases: Start by mapping your organization's biggest challenges and pain points. Where do inefficiencies, high costs, or diagnostic delays exist? Use the examples in this article as a blueprint to pinpoint where AI can deliver the most significant ROI.
Conduct a Data and Infrastructure Audit: Assess your current data assets and technological infrastructure. An initial AI requirements analysis is crucial to understand what is feasible today and what groundwork is needed for more ambitious projects tomorrow.
Develop a Pilot Program: Select one well-defined problem and launch a focused pilot project. This allows you to test hypotheses, measure KPIs, and demonstrate value to stakeholders before committing to a large-scale rollout. This iterative process is central to a successful AI Product Development Workflow.
Engage an Expert Partner: Navigating the complexities of AI implementation, from regulatory compliance to technical integration, requires specialized expertise. Partnering with a team that offers expert AI strategy consulting can de-risk your investment and significantly accelerate your timeline.
The proliferation of ai in medical field examples signifies a monumental opportunity to enhance patient outcomes, empower clinicians, and build more resilient healthcare systems. By moving from observation to action and adopting a strategic mindset, your organization can harness this transformative power to lead the future of medicine. For deeper insights and personalized guidance, feel free to connect with our expert team.
Ready to translate these examples into a competitive advantage for your organization? The team at Ekipa AI specializes in developing custom AI solutions that solve real-world healthcare challenges. Let us help you build a strategic AI roadmap that drives tangible results and positions you at the forefront of medical innovation. Our services range from a Custom AI Strategy report to hands-on AI Automation as a Service.
Frequently Asked Questions (FAQ)
1. What are the most common examples of AI in the medical field?
The most common and impactful examples include Medical Image Analysis (e.g., detecting tumors in X-rays and MRIs), Drug Discovery (accelerating research and development), Personalized Treatment Recommendations (tailoring therapies based on patient data), Predictive Analytics (forecasting disease outbreaks or patient risk), and Virtual Health Assistants (providing 24/7 patient support).
2. How is AI changing diagnostics in healthcare?
AI is revolutionizing diagnostics by enabling faster, more accurate, and more consistent analysis of medical data. For instance, AI algorithms can analyze medical images to identify signs of disease that might be missed by the human eye, review pathology slides to grade tumors, and detect patterns in electronic health records to predict the likelihood of a condition before symptoms are severe.
3. Can AI replace doctors or radiologists?
The current and foreseeable role of AI in medicine is to augment, not replace, human clinicians. AI excels at analyzing vast amounts of data and identifying patterns, acting as a powerful decision-support tool. It can automate repetitive tasks, reduce diagnostic errors, and provide data-driven insights. However, the final diagnosis, treatment planning, and patient care still require the critical thinking, empathy, and holistic judgment of a human doctor.
4. What are the main challenges of implementing AI in healthcare?
Key challenges include ensuring data privacy and security (HIPAA compliance), overcoming issues of data quality and bias, integrating AI systems with existing hospital IT infrastructure (like EHRs), navigating complex regulatory approvals (e.g., FDA), and managing the "black box" problem by ensuring AI recommendations are explainable and transparent to clinicians. Building trust among both providers and patients is also a critical hurdle.
5. How can a healthcare organization start using AI?
A strategic approach is best. Start by identifying a specific, high-impact problem within your organization, such as long diagnostic wait times or high readmission rates. Begin with a small pilot project to test an AI solution and measure its impact. Engaging with an expert partner for an AI Strategy consulting tool can help you build a realistic roadmap, ensure you have the necessary data and infrastructure, and navigate implementation complexities.