Your Guide to the AI Medical Revolution
Discover how AI medical systems are reshaping healthcare. Our guide explains AI's role in diagnostics, treatment, and the future of patient care.
Imagine having a medical assistant who has not only read every published medical study but has also analyzed millions of patient scans and can recall every single detail instantly. That's the essence of AI medical technology. It's not science fiction anymore; it’s the reality unfolding in clinics and hospitals around the globe, using intelligent algorithms to enhance human expertise and make healthcare smarter and more personal.
What Is The AI Medical Revolution
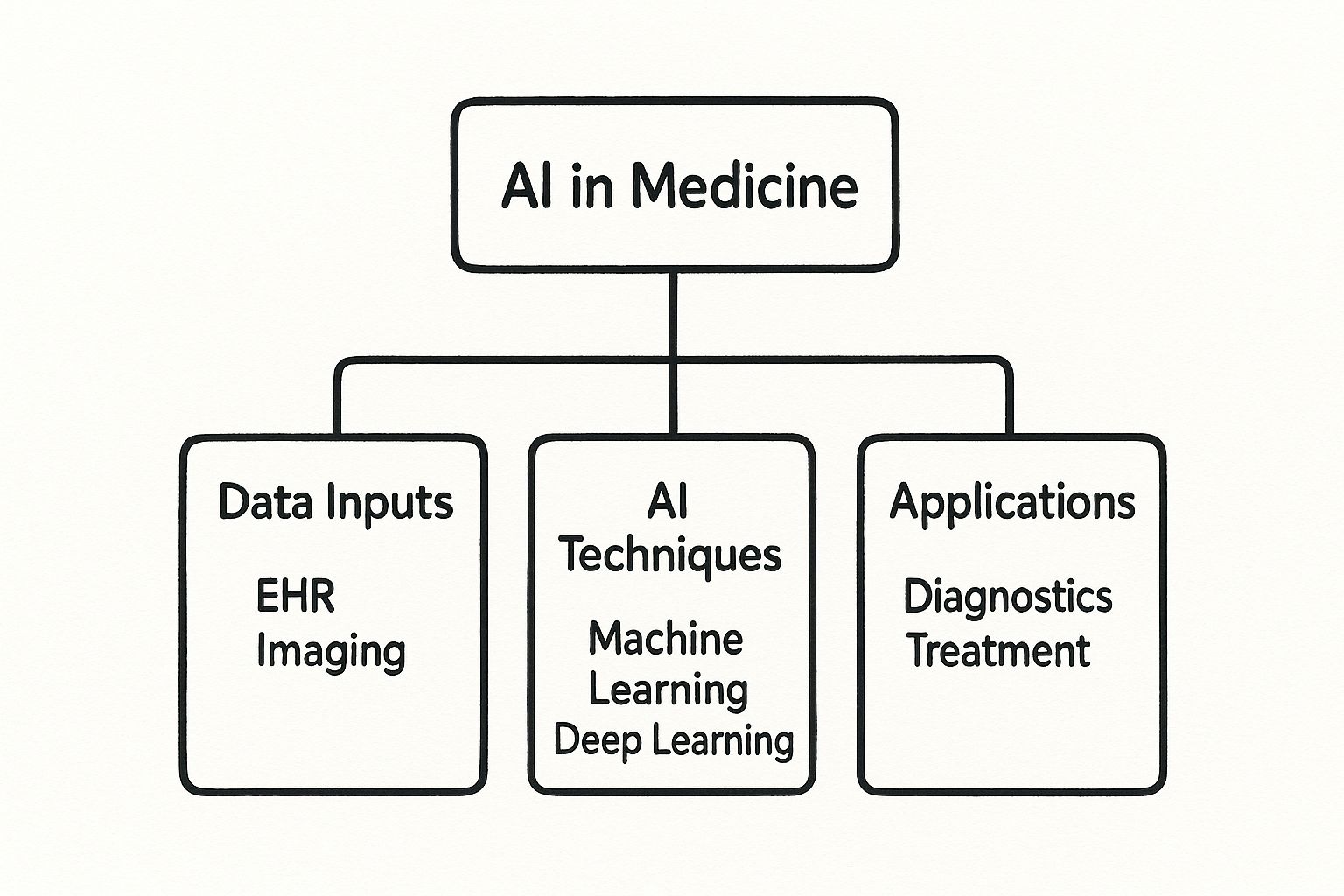
At its core, "AI medical" simply means applying artificial intelligence and machine learning to make sense of complex medical data. Think of AI as a powerful analytical engine. It tirelessly sifts through mountains of information—from electronic health records (EHRs) and diagnostic images to genomic sequences and clinical trial results—searching for patterns and insights that are often invisible to the human eye.
This isn't about replacing doctors. It's about empowering them. It’s like giving a skilled physician a team of super-powered researchers who can process data at breathtaking speed. The ultimate goal is to support clinical decisions, smooth out workflows, and, most importantly, improve patient outcomes.
Core Technologies Driving The Change
This shift is powered by a few key technologies, but two stand out as the real workhorses: machine learning and natural language processing.
To get a clearer picture, let's look at the foundational tools making all of this possible. The table below breaks down the key AI technologies, what they do, and how they're being used in medicine right now.
Core AI Technologies in Modern Medicine
| AI Technology | Primary Function | Medical Application Example |
|---|---|---|
| Machine Learning (ML) | Learns patterns from vast datasets to make predictions or classifications. | Training an algorithm on thousands of X-rays to spot the subtle, early signs of a tumor. |
| Natural Language Processing (NLP) | Enables computers to understand, interpret, and generate human language. | Analyzing unstructured text in doctor's notes or patient feedback to identify trends in symptoms or treatment responses. |
| Computer Vision | Allows AI to "see" and interpret visual information from images and videos. | Assisting radiologists by automatically detecting anomalies in MRI scans or CT images. |
| Robotics | Integrates AI with physical machines to perform tasks with precision. | Powering surgical robots that assist surgeons in performing minimally invasive procedures with greater accuracy. |
Each of these technologies plays a distinct but often overlapping role, working together to turn raw data into actionable medical insights. From reading a scan to guiding a surgical tool, AI is becoming a fundamental part of the modern medical toolkit.
Let's break down the two most dominant technologies:
- Machine Learning (ML): This is the engine that actually learns from the data. You can train an ML model on thousands of patient records to predict who is most at risk for developing a certain disease.
- Natural Language Processing (NLP): This is all about teaching computers to understand our language. NLP is what allows a system to read a doctor's handwritten notes, pull out the important information from a patient's email, or even scan through dense research papers to find relevant studies.
This infographic does a great job of showing how these different inputs are processed by AI to create real-world applications.
As you can see, it’s a clear path from raw data to a tangible medical solution, with AI algorithms sitting right at the center of that transformation.
The real power of AI medical systems lies in their ability to synthesize diverse information sources, creating a more complete picture of a patient's health than any single test or observation ever could.
The market's explosive growth tells the rest of the story. The global AI healthcare market jumped from $1.1 billion in 2016 to $22.4 billion by 2023—that's an incredible increase of about 1,779%. And it’s not slowing down. Projections show the market is on track to hit $188 billion by 2030.
This massive investment is a clear sign that AI-driven healthcare solutions are no longer just a niche idea; they're quickly becoming a core part of modern medicine.
How AI Is Improving Diagnostics and Treatment
Let's move beyond the theory and step into the clinic, where the real impact of AI medical tools comes into sharp focus. This isn't science fiction; these technologies are actively reshaping patient care today. They act as a powerful partner to medical professionals, helping them uncover insights previously buried in mountains of complex health data. From spotting diseases earlier to designing treatments for a single patient, AI is becoming a vital part of modern medicine.
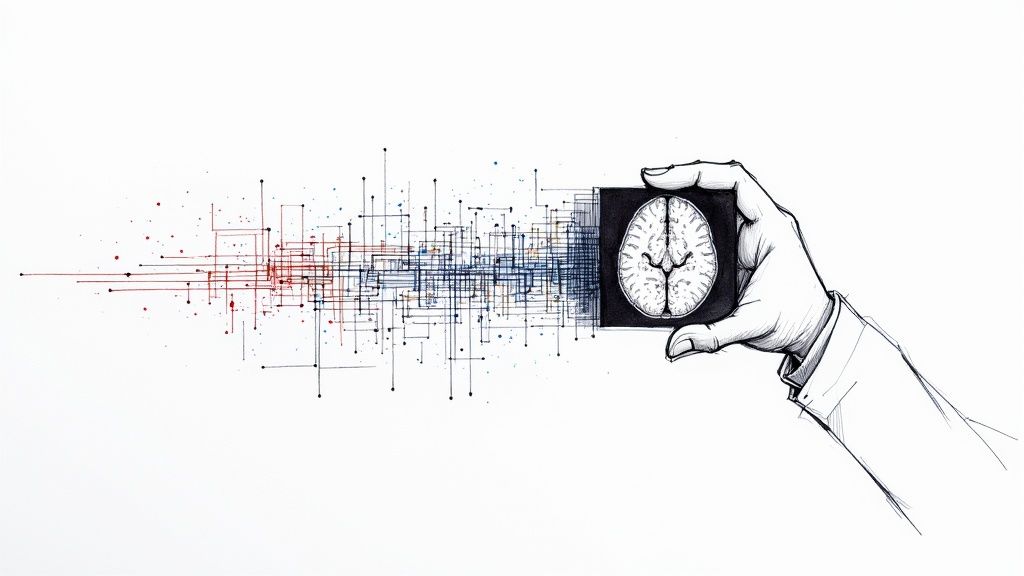
Perhaps the most mature and impactful application is in medical imaging. Think of an AI as a radiologist’s second set of eyes—but eyes that never get tired and have been trained on millions of scans. These algorithms can analyze MRIs, CT scans, and X-rays with stunning precision, flagging subtle patterns that might signal the early stages of diseases like cancer or Alzheimer's. This is where lives are saved, as early detection is almost always the key to a better outcome.
Seeing the Unseen in Medical Scans
In a practical sense, an AI system might highlight a suspicious lesion on a mammogram or a tiny nodule in a lung CT scan that a human observer, on a busy day, could easily miss. The AI doesn't make the final call. Instead, it directs the expert’s attention to areas that need a closer look, creating a seamless human-machine collaboration.
For example, researchers at Penn Medicine developed an AI tool that can detect cancer cells that are difficult, or even impossible, for the human eye to see. By sifting through huge amounts of imaging data in a fraction of the time, it adds a layer of precision that can completely change a patient's prognosis. For situations like these, it's worth exploring advanced diagnostic platforms. You might be interested in our guide on AI-powered diagnostic tools like Diagnoo, which shows how this technology is being used right now.
One of AI's greatest strengths in diagnostics is its ability to do the heavy lifting that researchers once had to do manually—pulling together and making sense of complicated datasets without the risk of human error.
This boost in diagnostic power isn't just about getting it right; it's also about speed. By automating the initial review of scans, AI frees up radiologists to concentrate on the most complex cases. This helps reduce backlogs and gets patients their results—and a treatment plan—much faster.
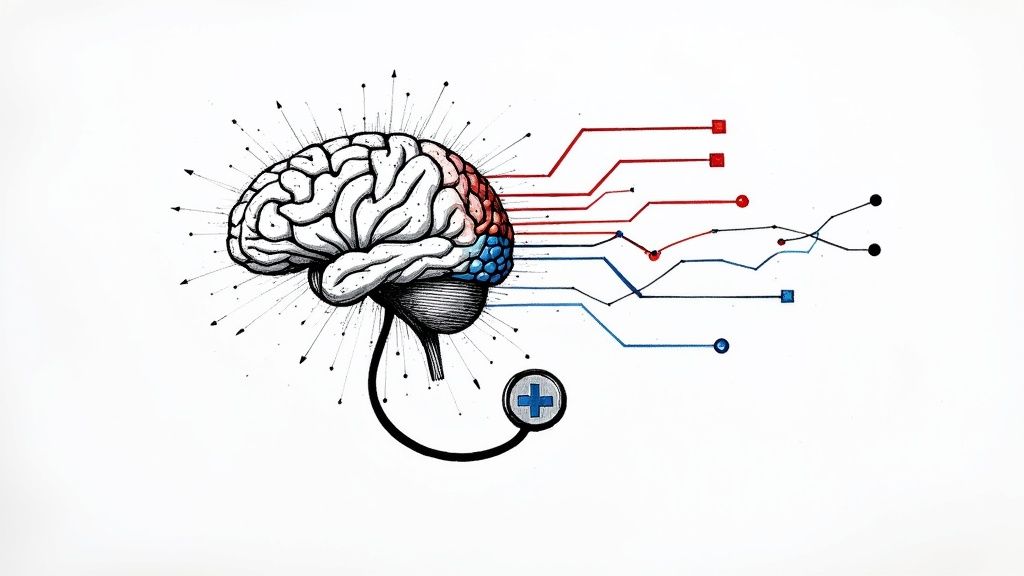
Personalizing Treatment Down to the DNA
Beyond spotting disease, AI medical systems are at the forefront of personalized medicine. We're moving away from the old one-size-fits-all approach. Now, AI can analyze an individual's unique genetic makeup, lifestyle, and medical history to predict which therapies will work best for them. This is making a huge difference in fields like oncology.
An algorithm can, for instance, dig through the genomic data from a tumor and cross-reference it with massive databases of treatment outcomes. This helps an oncologist choose a targeted therapy that’s most likely to work for that patient's specific cancer subtype. It cuts down on the painful and emotionally draining trial-and-error process.
- Predicting Treatment Effects: AI can mine deep genomic data to predict how a tumor will react to certain drugs.
- Optimizing Doses: In radiation therapy, AI helps design plans that hit the tumor hard while sparing as much healthy tissue as possible.
- On-the-Fly Adjustments: An AI can monitor how a patient is responding to treatment in real-time and suggest changes to the plan as needed.
Accelerating the Path to New Cures
AI’s influence doesn't stop at the bedside; it reaches all the way back to the lab. Drug discovery is a notoriously slow and expensive journey, often taking more than a decade and costing billions. AI is rewriting that script by dramatically speeding up the early phases of research.
By simulating how different molecules might interact inside the human body, AI can identify promising drug candidates in months instead of years. This incredible screening power allows pharmaceutical companies to focus their time and money on the compounds most likely to succeed, ultimately bringing new life-saving drugs to market much sooner.
You can see this momentum in the market figures. In 2024, the global AI healthcare market was valued at around $29 billion. It’s projected to explode to over $504 billion by 2032. That growth, a compound annual rate of over 44%, shows just how quickly AI is being woven into the fabric of diagnostics, drug discovery, and patient care. You can find more details in this market forecast on Fortune Business Insights. From the lab bench to the hospital bed, AI is fundamentally improving how we find, fight, and cure disease.
The True Benefits of Integrating AI in Healthcare
While the technology behind AI medical systems is fascinating, its real worth is measured in the tangible improvements it brings to hospitals, clinics, and, most importantly, patient lives. These aren't futuristic ideas; they're practical advantages being realized today.
The benefits spread throughout the entire healthcare system, strengthening three pillars that matter most: making care more precise, making operations more efficient, and delivering better health outcomes for everyone.
Perhaps the most obvious gain is a sharp reduction in human error. Even the most dedicated doctors and nurses are human, and fatigue during a long shift can lead to an oversight. Think of AI as a tireless, vigilant assistant.
Whether it's analyzing a complex MRI or checking a patient's chart for potential drug interactions, an AI provides a critical second look. This extra layer of precision helps catch mistakes before they cause harm, making patient care fundamentally safer.
Elevating Clinical Precision and Accuracy
AI's power to sift through enormous datasets makes it an incredible analytical partner for clinicians. In radiology, for instance, an AI can flag a tiny, ambiguous spot on a lung X-ray that might be an early-stage tumor.
The system isn't replacing the radiologist; it's augmenting their expertise. It draws their attention to areas that warrant a closer look, ensuring nothing gets missed. This teamwork leads to a more consistent and reliable diagnostic process, smoothing out the natural variations that can occur between different doctors and upholding a higher standard of care.
By standardizing the initial review of complex data, AI helps establish a baseline of accuracy. This frees up medical experts to focus their brainpower on the most subtle and challenging aspects of a case.
The bottom line? Diagnoses are not only faster but also more dependable. This newfound precision is the bedrock for building more effective, personalized treatment plans.
Streamlining Workflows and Boosting Efficiency
Beyond the exam room, AI medical solutions are overhauling the administrative side of healthcare. A huge chunk of any clinician's day is eaten up by paperwork, data entry, and other repetitive chores. They’re necessary evils that pull time away from patients.
AI-driven automation can handle these routine duties with incredible speed and accuracy. It can transcribe a doctor’s spoken notes, manage complex appointment schedules, and process billing codes, letting medical staff get back to what they were trained to do: care for people. This boost in efficiency brings several key advantages:
- Reduced Administrative Burden: Doctors and nurses spend less time on clerical tasks and more time building relationships with patients, which improves care and helps combat professional burnout.
- Faster Turnaround Times: Automating data processing means lab results are analyzed and reports are generated much quicker. For patients, this means less time spent anxiously waiting.
- Cost Savings: Efficiency directly translates to lower operational costs from manual labor and administrative slip-ups, making the entire healthcare system more financially sustainable.
Achieving Better Patient Outcomes
This is where it all comes together. Greater precision and streamlined workflows have one ultimate goal: better health for patients. When a diagnosis is more accurate and delivered sooner, treatment can start earlier, which is often when it's most effective.
This proactive approach is fast becoming the new standard. In fact, by 2025, artificial intelligence is expected to be nearly everywhere, with forecasts showing that 90% of hospitals worldwide will use AI for early diagnosis and remote patient monitoring.
The economic impact is also huge, with projections pointing to $150 billion in reduced U.S. healthcare costs by 2026. You can explore more in these insights on AI healthcare statistics.
Ultimately, bringing AI into medicine creates a powerful positive cycle. More precise diagnostics lead to more effective treatments. More efficient operations give clinicians the time and energy to provide empathetic, high-quality care. It’s a win-win that builds a healthier, more resilient system for everyone.
Navigating the Risks and Ethical Questions
Whenever we bring new technology into medicine, we have to take an honest, clear-eyed look at the challenges. The potential for AI medical tools is incredible, there's no doubt about it. But putting them into practice introduces a whole new set of ethical and practical hurdles that healthcare leaders need to get ahead of. The only way to move forward responsibly is to understand these risks from the start and build a foundation of trust and transparency.
The most obvious concern for everyone—patients and providers alike—is data security. AI systems, especially machine learning models, need a massive amount of patient data to learn their jobs. This places an enormous responsibility on organizations to guard that information against breaches and misuse. Patient confidentiality has to be non-negotiable.
The Challenge of Algorithmic Bias
One of the most serious ethical landmines in AI medical technology is algorithmic bias. Here’s the simple truth: an AI model is only as good as the data it’s trained on. If that training data comes mostly from one demographic group, the algorithm will inevitably be less accurate for everyone else. This can take existing health disparities and make them even worse.
Think about it this way: an AI tool trained mostly on data from male patients might struggle to spot the signs of heart disease in women, whose symptoms often present differently. The AI isn't being malicious; it's just reflecting the historical biases already present in medical research and data collection. To fix this, we have to make a conscious, deliberate effort to build and test algorithms with diverse, representative datasets that actually look like the real-world patient population.
The core ethical mandate is simple: ensure that AI medical tools close, rather than widen, the gaps in healthcare equity. This means putting fairness and inclusivity at the heart of every stage of AI development and deployment.
Getting this right involves a few critical steps:
- Auditing Datasets: Proactively digging into training data to find demographic gaps or imbalances before they cause problems.
- Diverse Testing: Rigorously testing AI models across different ethnic, gender, and age groups before they ever touch a real patient.
- Continuous Monitoring: Putting systems in place to watch how the AI performs in the real world so you can catch and correct any emerging biases quickly.
This isn't just a box-ticking exercise. It's essential for building tools that actually help all patients equally.
Unpacking the Black Box Problem
Another major hurdle is what we call the "black box" problem, which is especially common with advanced deep learning models. This is when an algorithm gives you a startlingly accurate prediction, but you have no idea how it got there. For a doctor, that lack of transparency can be a huge barrier to trust.
If an AI flags a scan as potentially cancerous, a clinician needs to know why. Was it a specific cluster of cells? A subtle shift in tissue density? Without that reasoning, it’s incredibly difficult to confidently use the AI's insight to make a final diagnosis or recommend a treatment. The trust between the clinician, the AI, and the patient hangs on this very explainability.
Key AI Risks and How to Mitigate Them
To bring AI medical technology into a healthcare setting responsibly, organizations have to develop clear strategies to manage these complex issues. The table below breaks down the biggest risks and offers some practical ways to address them head-on.
| Risk Category | Description of Challenge | Potential Mitigation Strategy |
|---|---|---|
| Data Privacy & Security | Protecting huge volumes of sensitive patient health information from unauthorized access or cyberattacks. | Implement robust data encryption, anonymization techniques, and strict access controls that comply with regulations like HIPAA. |
| Algorithmic Bias | AI models can perpetuate or even worsen existing health disparities if they are trained on non-diverse datasets. | Curate and audit all training data for diversity. Insist on rigorous testing across all demographic groups before any clinical deployment. |
| The "Black Box" Problem | A lack of transparency in how an AI model reaches its conclusions, making it difficult for clinicians to trust or verify its outputs. | Prioritize "explainable AI" (XAI) models that provide clear reasoning. Establish firm protocols for human oversight and final decision-making. |
| Accountability & Liability | Figuring out who is responsible when an AI-assisted diagnosis or treatment recommendation leads to a poor patient outcome. | Develop clear legal and ethical frameworks that define the roles and responsibilities of developers, institutions, and clinicians. |
Dealing with these issues isn't just a technical problem—it's a fundamental requirement for the ethical use of AI in medicine. Building strong governance, demanding transparency, and committing to fairness are the cornerstones of any successful and trustworthy AI medical strategy.
Your Roadmap for AI Medical Implementation
Getting AI medical solutions up and running is about much more than just buying new software. It requires a thoughtful, strategic plan. Think of this as a practical roadmap for healthcare leaders, designed to guide your organization from the first conversation all the way to a successful, scalable deployment. The key is to build momentum carefully, ensuring every step delivers real, measurable value.
The journey doesn't start with the technology; it starts with a problem. The most successful AI projects I've seen are the ones that zero in on a specific, high-impact challenge. It’s a common mistake to chase a shiny new tool. Instead, start by finding a genuine issue that AI is perfectly suited to solve.
Identify Your Starting Point
Before you jump into vendor demos, take a hard look at your current operations. Where are the real bottlenecks? Are your radiologists drowning in scans? Is the administrative team buried under a mountain of paperwork? Pinpointing these genuine pain points gives your AI strategy a clear direction and a strong sense of purpose from the outset.
Start by asking the right questions to uncover the best opportunities:
- Diagnostic Delays: Could AI help us review medical images faster and cut down the agonizing wait times for patients needing critical results?
- Administrative Overload: Can we use AI to automate routine tasks like billing, scheduling, or transcribing clinical notes, freeing up our staff to focus on patient care?
- Predictive Insights: Are we sitting on valuable data that could help us predict patient readmissions or flag individuals at high risk for certain conditions?
By focusing on one, well-defined problem, you create a clear finish line and make it much easier to measure success. A solid initial win does wonders for building confidence and getting key stakeholders on board for more ambitious projects down the road.
The goal of a first AI project should be to solve a real-world problem effectively. Choose a challenge where success is easily defined and the impact is clearly visible to both staff and patients.
Build a Solid Data Foundation
Let's be clear: AI runs on data. Without a high-quality, well-organized data infrastructure, even the most sophisticated algorithms are useless. This means making sure your electronic health records (EHRs), imaging archives, and other data sources are clean, accessible, and secure.
This groundwork is non-negotiable. You’ll need to break down data silos, standardize your formats, and put strong governance rules in place to protect patient privacy. This isn't just a technical hurdle; it’s a fundamental ethical and regulatory requirement.
Choose Partners and Launch a Pilot
Once your data house is in order, it's time to find the right technology and partners. You don't have to build everything from the ground up. Plenty of specialized vendors offer proven AI medical platforms designed to fit into existing workflows. My advice is to look for partners who genuinely understand the messy, complex reality of healthcare and can offer support long after the sale.
A pilot program is your best friend here. It’s the perfect way to test a solution in a controlled, real-world setting. Pick a specific department or clinical workflow to be your testing ground. This allows you to:
- Validate the Technology: Confirm the AI actually works as promised with your specific patient data and in your unique environment.
- Refine Workflows: Work out the kinks and smooth out any friction that arises when your team starts using the new tool in their day-to-day routines.
- Measure Impact: Gather the data you need to prove the improvements in efficiency, accuracy, or cost savings.
A successful pilot gives you the hard evidence required to make the case for a wider rollout. For organizations that need a guiding hand through this process, exploring expert implementation support can provide the structure and deep knowledge needed for a smooth transition. This methodical approach takes a lot of the risk out of the investment and paves the way for lasting success.
The Future of Medicine and What to Expect Next
Looking at the next decade, it’s clear that AI in medicine isn’t just a passing trend. We're seeing a fundamental shift away from a reactive, "treat-it-when-it's-broken" model of healthcare. Instead, we’re moving toward a system that’s proactive, predictive, and intensely personal.
One of the most mind-bending developments on the horizon is the use of generative AI to create synthetic patient data. Think about that for a second. We can now generate massive, realistic (but completely anonymous) datasets to train and test new algorithms. This approach slashes research timelines without ever touching real patient information, neatly sidestepping huge privacy hurdles.
The Rise of Continuous Health Monitoring
Your health is no longer just what happens inside a clinic. Wearable tech—smartwatches, biosensors, continuous glucose monitors—is turning our bodies into real-time data streams. AI is the key to making sense of it all.
Imagine an AI constantly analyzing your sleep quality, activity levels, and heart rate variability. It could spot subtle patterns that might signal a developing health issue weeks or even months before you’d ever feel a symptom. This creates an entirely new kind of conversation between you and your doctor, one focused on prevention and personalized advice.
Predicting and Managing Public Health Crises
On a much larger scale, AI is shaping up to be a game-changer for global public health. By crunching numbers on everything from anonymized health records to travel routes and climate data, AI models can forecast disease outbreaks with startling accuracy.
This gives public health organizations a massive advantage. Suddenly, they can:
- Get ahead of a crisis by strategically allocating vaccines, medications, and hospital beds.
- Launch awareness campaigns in the exact areas where they’ll have the most impact.
- Simulate different response strategies to see what works best before committing resources.
The real goal here isn't to replace doctors and nurses with algorithms. It’s to give them superpowers—to augment their expertise so they can deliver care with more precision, foresight, and personalization than ever before.
Forward-thinking initiatives like the ones seen in Canadian Digital Health Innovation highlight just how much global energy is pouring into this field. With smart planning and a strong ethical compass, AI is set to help build a healthier future for all of us.
Frequently Asked Questions About AI in Medicine
It’s completely understandable to have questions as AI tools start to show up in clinics and hospitals. Whether you're a patient or a healthcare provider, the topic brings a mix of curiosity and concern.
Let's cut through the hype and get straight to some of the most common questions people have about AI's real-world role in medicine.
How Is Patient Data Kept Private?
This is, without a doubt, one of the most important questions out there. Protecting patient data isn't just a goal; it's a legal and ethical mandate. Hospitals and their tech partners use a combination of powerful security layers, all designed to comply with strict regulations like HIPAA.
Here’s a look at the core defenses:
- Data Anonymization: Before any data is used to train an AI model, all personal identifiers—your name, address, social security number—are completely stripped away. The data becomes anonymous, making it impossible to trace back to an individual.
- Robust Encryption: All information, whether it’s sitting on a server or being sent between systems, is encrypted. Think of it as a digital lockbox that turns sensitive data into unreadable code for anyone who doesn't have the key.
- Strict Access Controls: Not just anyone can get into these systems. Access is tightly controlled, requiring multiple layers of authentication so only authorized personnel can view sensitive information.
These measures work together to ensure AI can learn from health data to improve care for everyone, but individual privacy is never put at risk.
The core principle is simple: use the data to learn, but always protect the person behind the data.
Will AI Replace Doctors and Nurses?
In a word, no. The aim of AI medical technology is to assist, not replace. It's best to think of AI as an incredibly capable partner that supercharges the abilities of human clinicians.
AI is a powerhouse when it comes to sifting through mountains of data with speed and accuracy—like analyzing thousands of medical scans to spot subtle patterns or flagging potential risks in patient records. What it can't do is replicate the empathy, intuition, and nuanced critical thinking that are the heart and soul of medicine.
The roles of doctors and nurses will certainly change. AI will take over many of the repetitive, data-heavy tasks, freeing up medical professionals to spend more time where it matters most: with their patients, building trust, and navigating the complex, human side of healing.
What Is a Good First Step for a Small Clinic?
Jumping into AI doesn't have to mean a massive, bank-breaking project, especially for smaller practices. The smartest way to start is to pick one specific, high-impact problem and find a targeted AI solution to solve it.
Take a look at your daily operations. Where are your biggest headaches? Is it the endless administrative work like scheduling and billing? Maybe it's keeping up with patient communication. There are plenty of affordable, ready-to-use AI tools that can automate these exact tasks and deliver real value right away.
By starting with a focused, manageable project, a small clinic can see a clear return on investment, help staff get comfortable with the new technology, and learn the ropes before ever thinking about a larger-scale overhaul.
At Ekipa AI, we specialize in helping organizations of all sizes identify and execute high-impact AI opportunities. Discover your tailored AI strategy in just 24 hours. Learn more at Ekipa.ai.