AI Use In Medical Field : A Practical Explainer
Explore the real-world AI use in medical field. This guide explains how AI improves diagnostics, streamlines operations, and shapes the future of patient care.
Artificial intelligence is no longer a futuristic concept in medicine—it's here, and it's already a fundamental part of how healthcare professionals deliver better patient care and run their operations. The practical use of AI in the medical field has moved far beyond theory, from sharpening diagnostic accuracy to creating personalized treatment plans and untangling complex administrative workflows. Think of it as a powerful assistant, one that enhances human expertise with insights pulled from massive amounts of data.
How AI Is Reshaping Modern Medicine
AI's role in healthcare has graduated from the experimental stage to become a key part of daily operations in many health systems. This isn't just a minor update; it represents a major shift in how patient care is delivered, managed, and fine-tuned for the best possible results.
The pace of adoption is staggering. Right now, a remarkable 80% of hospitals are already using some form of AI to improve patient outcomes and make their internal processes more efficient. This rapid uptake is driving incredible market growth, with projections showing the global AI in healthcare market exploding from $11 billion in 2021 to an estimated $431.05 billion by 2032.
A New Era of Patient Care
Let's be clear: the goal of AI in medicine is to augment, not replace, human expertise. It gives doctors, nurses, and administrators tools that can sift through enormous datasets, spot patterns invisible to the naked eye, and forecast outcomes with a speed that humans simply can't match.
Imagine giving a seasoned physician a team of tireless digital researchers. This team can instantly scan every relevant medical journal, patient chart, and diagnostic image to provide a complete picture. This synergy between human intuition and machine intelligence leads directly to more confident decisions and, ultimately, better patient care.
Before we dive deeper, it's helpful to see where AI is making its mark. The table below outlines the key areas being impacted right now.
Key Areas of AI Impact in the Medical Field
Area of Application Core AI Function Primary Benefit to Healthcare
Clinical Diagnostics
Analyzes medical images (X-rays, MRIs, etc.) to detect subtle anomalies.
Earlier and more accurate disease detection.
Personalized Treatment
Assesses genetic data and patient history to suggest tailored therapies.
More effective treatment plans, especially in oncology.
Operational Efficiency
Automates routine tasks like scheduling, billing, and resource planning.
Frees up clinical staff to focus on direct patient care.
As the table shows, AI's influence is broad, touching everything from the exam room to the back office. It is making a tangible difference across the board.
This shift isn't just about plugging in new software. It's about fundamentally rethinking how healthcare systems work. Success hinges on having a clear vision and a solid strategy to guide the way.
For healthcare organizations, understanding these applications is the first step. Building a more intelligent and responsive system of care requires a clear roadmap, and as we explore specific AI solutions for the healthcare industry, it's obvious that a well-thought-out plan is the foundation for getting it right.
AI's Role in Sharpening Diagnostic Accuracy
One of the most immediate and powerful applications of AI in healthcare is its ability to boost diagnostic precision. In a clinical setting, AI isn't here to replace doctors. Instead, it acts as an incredibly sharp-eyed partner, capable of seeing patterns that might slip past even the most experienced human eye.
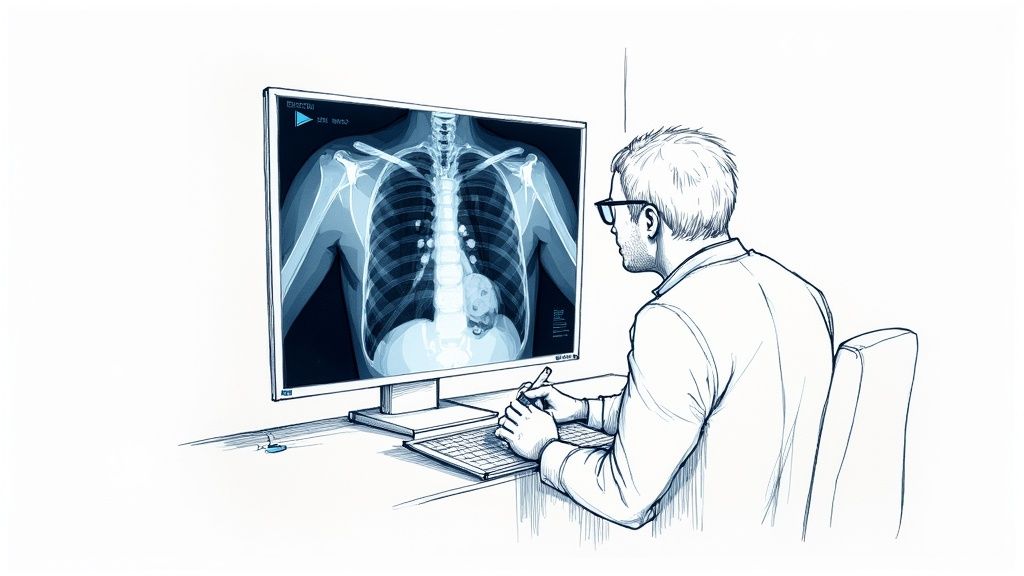
This collaboration is especially mature in medical imaging. Radiologists spend their days poring over complex scans where a tiny, almost invisible shadow could be the first sign of a serious disease. AI algorithms, having been trained on millions of similar images, can analyze MRIs, CT scans, and X-rays in mere seconds, highlighting areas of concern for a specialist to review.
Think of it as a seasoned detective working alongside a forensics expert who can analyze evidence at a microscopic level. The detective—the radiologist—still makes the final judgment, but the AI expert provides critical, data-driven clues that could easily be missed. This dynamic drastically cuts down on human error and gets patients their diagnoses faster.
A Second Pair of Eyes in Medical Imaging
The impact AI is having on the analysis of medical scans is profound. These systems go far beyond flagging obvious problems; they're trained to identify subtle textures and patterns that point to disease in its earliest stages.
- Oncology: In cancer detection, AI tools can spot potentially malignant nodules on lung scans or pinpoint microcalcifications in mammograms that signal early-stage breast cancer. That kind of early warning can be the difference between a treatable condition and a late-stage diagnosis.
- Neurology: For neurologists, AI helps detect the faintest signs of a stroke or the subtle brain atrophy linked to Alzheimer's disease on an MRI, often well before clear symptoms appear.
- Cardiology: In cardiology, algorithms can analyze cardiac MRIs to assess heart function and identify damage from a heart attack with incredible precision, guiding cardiologists toward the most effective treatment plans.
This technology isn't just a concept anymore; it's gaining real traction. A 2025 survey showed that 66% of physicians are actively using health-AI tools, a huge jump from just 38% in 2023. That rapid adoption signals a growing trust in AI's ability to genuinely help with patient care.
From Population Health to Personalized Medicine
Beyond just reading scans, another major use of AI in the medical field is driving the move toward personalized medicine. For decades, treatments were developed for the "average" patient. AI lets clinicians break free from this one-size-fits-all model by digging into a patient's unique biological data.
By crunching massive datasets of genomic information, lifestyle factors, and medical histories, AI can predict how a specific person might respond to a certain therapy. This is a game-changer in oncology, where an AI model can analyze a tumor's genetic signature to recommend the most potent chemotherapy drug, cutting out much of the painful trial-and-error process.
AI transforms patient data from a static record into a predictive blueprint. It helps answer the most important question: "What is the best possible treatment for this specific patient?"
This level of personalization was computationally impossible not long ago. Now, it's becoming a reality, allowing for treatment plans that are finely tuned to an individual's unique situation.
The New Generation of AI Diagnostic Tools
These capabilities are also showing up directly at the point of care through a new generation of AI-powered diagnostic tools. These systems are designed to help clinicians make faster, more informed decisions on the spot. Some tools, for instance, can analyze a patient's stated symptoms and medical history to suggest a list of potential diagnoses, ranked by probability.
These are far more than glorified symptom checkers; they are sophisticated analytical engines. An AI tool might analyze subtle changes in a person's voice to detect early signs of Parkinson's disease or use a smartphone camera image to identify potentially malignant skin lesions with high accuracy.
Our own Diagnoo tool helps medical teams classify patient issues to accelerate triage and care delivery, which is a perfect example of this in action. These tools don't just add efficiency—they empower clinicians, shorten diagnostic timelines, and bring expert-level analysis to more healthcare settings than ever before. You can learn more about it here: https://www.ekipa.ai/products/diagnoo.
Streamlining Hospital Operations With AI

While the clinical breakthroughs in AI tend to capture the spotlight, a hospital’s ability to run smoothly behind the scenes is just as crucial for great patient care. The administrative side of healthcare is often a maze of manual processes, endless paperwork, and complex logistics—and this is exactly where the use of AI in the medical field is making a huge difference.
Think of AI as a digital operations manager. It steps in to automate the repetitive, time-draining tasks that contribute to staff burnout and create frustrating delays across the entire system. This isn’t about replacing people; it’s about empowering skilled professionals to spend less time on clerical work and more time with their patients.
Tasks like medical coding, insurance billing, and patient scheduling are perfect for this. They follow specific rules but have a high degree of complexity, making them ideal for intelligent automation. When an AI takes over, accuracy goes up, and the team is freed from the daily grind of administrative work.
Predictive Analytics for Resource Management
One of the most powerful applications of AI in hospital logistics is predictive analytics. Hospitals are constantly in flux, with patient demand swinging dramatically and unexpectedly. By digging into historical data, AI models can forecast future needs with impressive accuracy, shifting the hospital from reactive crisis management to proactive, strategic planning.
This has a direct and immediate impact on several key operational areas:
- Emergency Room Wait Times: AI can analyze patient admission trends, public health data, and even seasonal factors to predict when the ER will get slammed. This gives administrators a heads-up to adjust staffing, ensuring the department is ready for a surge and patients aren't left waiting.
- Bed Availability: By predicting patient discharge times and lengths of stay, AI algorithms can create a live, dynamic map of available beds. This is a game-changer for managing patient flow, preventing bottlenecks in the ER, and getting patients into the right rooms without long waits.
- Staffing Optimization: AI can generate optimal staff schedules that account for predicted patient volume, staff availability, and even individual shift preferences. This helps guarantee proper coverage and fights back against the chronic understaffing that leads to burnout—a major problem in healthcare.
These applications show how AI Automation as a Service can help build a more resilient and responsive healthcare system from the inside out.
Automating the Administrative Burden
Beyond just planning resources, AI is also chipping away at the mountains of paperwork that bog everything down. The prior authorization process, for example, is a notorious source of frustration for providers and patients alike, often delaying necessary treatments for days or weeks.
An AI system built for prior authorizations can scan a patient's record, cross-reference it with an insurer's criteria, and automatically submit the required forms. A task that used to involve a week of phone calls and faxes can now be handled in minutes.
This kind of automation creates a positive ripple effect. It speeds up the revenue cycle because claims are coded correctly and submitted on time, which means fewer denials and faster reimbursements. By developing these smart workflows, hospitals can dramatically improve their financial stability while getting patients the care they need much faster. These systems are fantastic examples of powerful internal tooling that boosts both efficiency and patient satisfaction.
Putting these tools to work effectively usually starts with solid AI strategy consulting to pinpoint the areas where automation will deliver the biggest wins. By tackling these core operational headaches, healthcare organizations can build a more efficient, cost-effective, and patient-focused environment. The end goal is simple: let technology handle the logistics so people can focus on healing.
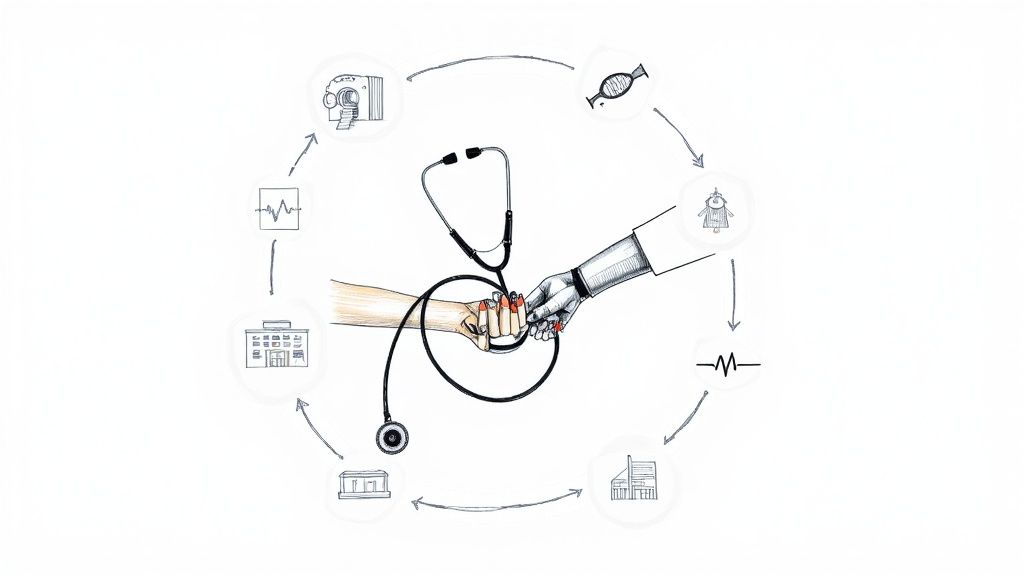
Navigating The Challenges of Medical AI
While the promise of AI in medicine is enormous, putting it into practice is a lot more complicated than just installing new software. Successfully weaving AI into the fabric of healthcare means navigating a minefield of significant hurdles. Getting it right demands a thoughtful, deliberate strategy that balances cutting-edge innovation with deep-seated responsibility.
The whole challenge really boils down to three core pillars: data integrity, regulatory compliance, and ethical responsibility.
These aren't just boxes to check; they're the very foundation of safe, effective, and trustworthy medical AI. If any one of these pillars crumbles, the entire initiative can fail, leading to bad patient outcomes, legal headaches, or a complete loss of public trust. This is exactly why a meticulously planned approach, often starting with a Custom AI Strategy report, is so critical to map out a responsible path forward.
The Bedrock of AI: Data Integrity and Quality
High-quality, unbiased data is the lifeblood of any medical AI. An algorithm is only as smart as the data it learns from, and in healthcare, the stakes couldn't be higher. If a model is trained on incomplete, inaccurate, or skewed information, its recommendations will be unreliable at best and dangerously wrong at worst.
Think about an AI tool designed to spot skin cancer. If it’s mostly trained on images from a single skin tone, it develops a massive blind spot. The tool becomes far less effective for anyone outside that specific demographic, creating a serious health equity issue. Making sure your data is diverse, complete, and clean isn't just a best practice—it's the non-negotiable first step. This crucial phase of data preparation is a core part of any thorough AI requirements analysis.
Beyond quality, security is everything. Healthcare data is incredibly sensitive and is protected by strict regulations like the Health Insurance Portability and Accountability Act (HIPAA). Any AI system that touches this information must comply with these rules, period. This means robust data anonymization, ironclad storage security, and tightly controlled access to keep patient privacy locked down.
Navigating the Regulatory Maze
The rulebook for medical AI is being written as we go, with technology often moving faster than legislation. Agencies like the U.S. Food and Drug Administration (FDA) are stepping up, creating new frameworks to review AI-powered medical devices and confirm they are both safe and effective for real-world clinical use.
The landscape is changing fast. The number of FDA-cleared AI/ML devices is on track to nearly double between 2022 and 2025. These tools are now being used in radiology, cardiology, neurology, and dozens of other specialties, with radiology currently leading the pack. You can dive deeper into these regulatory trends and see what they mean for the future of AI medical devices. Gaining clearance isn't easy; it's a demanding process that requires extensive clinical validation and crystal-clear documentation.
For any hospital or health system, this means one thing: regulatory approval can't be an afterthought. It has to be baked into the design of any AI solution from day one, whether you build it yourself or buy it from a vendor.
Addressing the Ethical Minefield
Perhaps the trickiest part of this whole equation is the ethics. This goes way beyond data privacy and touches on fundamental questions of fairness, transparency, and who's ultimately accountable when things go wrong. Algorithmic bias is a huge concern here, as AI systems can accidentally reinforce or even worsen existing health disparities if they aren't built and monitored with extreme care.
Here are some of the tough ethical questions every organization has to answer:
- Transparency: Can a doctor—or a patient—understand why the AI made a certain recommendation? "Black box" algorithms, where the logic is hidden, just don't work in a field where clinicians need to trust the reasoning behind a decision.
- Accountability: If an AI model contributes to a misdiagnosis, who is responsible? The software developer? The hospital? The doctor who followed the AI's advice? You have to draw these lines clearly before the technology is deployed.
- Equity: Does the AI perform equally well for everyone, regardless of their race, gender, or socioeconomic background? You have to test for this relentlessly to avoid causing unintended harm to already vulnerable groups.
To help visualize these obstacles, here's a look at the common hurdles organizations face and how to think about overcoming them.
Key Implementation Challenges for AI in Healthcare
Challenge Area Specific Issue Strategic Mitigation Approach
Data Governance
Poor quality, siloed, or non-standardized patient data.
Establish a central data governance framework. Invest in data cleansing, standardization, and interoperability tools.
Technical Infrastructure
Lack of sufficient computing power or secure cloud infrastructure.
Conduct a thorough tech audit. Plan for scalable cloud or on-premise solutions that meet HIPAA security standards.
Regulatory & Compliance
Navigating the complex and evolving FDA and HIPAA requirements.
Build a cross-functional team including legal and compliance experts from the start. Design for compliance, not after the fact.
Clinical Workflow Integration
AI tools that don't fit naturally into how clinicians already work.
Involve clinicians heavily in the design and testing phases. Focus on user-centric design that augments, not disrupts, workflows.
Ethical & Bias Concerns
Algorithms trained on non-diverse data, leading to biased outcomes.
Mandate the use of diverse and representative training datasets. Implement continuous auditing for bias post-deployment.
Organizational Change
Resistance from staff, lack of AI literacy, and fear of job displacement.
Develop a comprehensive change management and training program. Emphasize AI as a tool to support clinicians, not replace them.
Navigating these challenges isn't just about having the right tech. It’s about building a culture of responsible innovation. It underscores why working with our expert team, a group that deeply understands these nuances, is so important for building AI systems that are not only powerful but also fundamentally trustworthy.
Your Roadmap to a Successful AI Rollout
Moving from theory to practice is where the rubber meets the road with AI in the medical field. A great integration isn't just about plugging in new tech; it's about following a clear, step-by-step playbook that breaks a massive initiative down into manageable wins. Without a solid plan, even the most promising AI projects can fizzle out.
The journey doesn't start with software. It starts with a problem. The smartest AI integrations I've seen always begin by identifying a specific, high-impact issue that needs solving. This focus ensures your efforts are aimed squarely at what matters most: improving patient care or making operations run smoother.
Step 1: Pinpoint a Specific Problem
Instead of asking, "Where can we use AI?" try asking, "What's our biggest bottleneck right now?" Maybe it's the agonizing wait times for radiology reports, the chaotic patient flow in the ER, or the soul-crushing paperwork for prior authorizations that delays treatment.
When you nail down a precise challenge, you automatically create clear metrics for success. This laser-focused approach is far more effective than a vague, organization-wide push for "AI adoption," which usually just burns through resources with little to show for it.
Step 2: Run an AI Readiness Check
Once you know the problem you want to tackle, you have to take an honest look in the mirror. It's time to assess your organization's readiness by diving deep into your data, infrastructure, and the skills your team currently has. Think of it as checking your foundation before you start building.
This assessment will expose any critical gaps—in data quality, tech infrastructure, or staff expertise—before they have a chance to derail the entire project.
You’ll want to ask a few key questions:
- Data: Is your patient data clean, organized, and easy to get to? Or is it trapped in a dozen different systems that don't talk to each other?
- Infrastructure: Do you have the computing muscle and secure cloud setup needed to run sophisticated AI models?
- People: Does your team have the know-how to manage and make sense of AI tools, or will you need to bring in training or outside help?
Step 3: Launch a Small-Scale Pilot Program
With a clear problem and a solid grasp of your capabilities, it's time to dip a toe in the water. A small, controlled pilot program is the perfect way to prove an AI solution's worth without committing to a massive, system-wide overhaul right out of the gate.
This is where you build momentum. Pick a single department or one specific workflow to test your chosen AI tool. The goal is to gather hard data that shows its impact—whether that's faster diagnoses, fewer administrative mistakes, or happier patients. A successful pilot gives you the concrete evidence you need to get everyone, from leadership to clinicians, on board for a bigger rollout. This methodical process is a key part of our implementation support, designed to lower risk while boosting the odds of success.
As you move through these steps, you'll constantly be navigating the three core challenges of any healthcare AI project: data, compliance, and ethics.

This image really drives home the point that a successful journey requires you to keep your eye on technical readiness, regulatory rules, and ethical duties from day one.
Step 4: Scale Up and Integrate
Once your pilot has delivered the goods, you can start the process of scaling up. This final stage is all about weaving the AI tool more deeply into your existing clinical and operational workflows. It demands a thoughtful change management plan, thorough staff training, and continuous monitoring to make sure the technology keeps performing as it should.
Following this roadmap transforms the overwhelming task of AI integration into a strategic, step-by-step process. Each stage builds on the last, helping you create real, lasting value for your organization and your patients.
So, Where Do You Go From Here?
The journey into medical AI is no small undertaking, but it's a defining step toward a smarter, more efficient, and deeply patient-focused future. As we've seen, the path isn't always straight—it’s filled with complexities like data integrity and regulatory hurdles—but the destination is worth it. True success isn't about just buying a piece of software; it's about thoughtful, strategic implementation guided by people who’ve been there before.
Finding a team that speaks both the language of technology and the unique dialect of healthcare is absolutely essential. They can help you see around corners and avoid common pitfalls.
This all starts with a clear, well-thought-out plan. It begins with a solid foundation, which means a detailed AI requirements analysis to pinpoint where you'll get the most bang for your buck and to honestly assess if your organization is ready. From there, you need a structured AI Product Development Workflow to make sure new solutions are built and woven into your existing systems without causing chaos. As we explored in our AI adoption guide, a methodical approach breaks a massive initiative down into manageable, achievable steps.
Finding a Partner to Build the Future, Together
Navigating the intersection of healthcare and AI requires more than just technical chops. You need a partner who can translate the incredible potential of AI into real-world results that doctors, nurses, and patients can feel. This means everything from creating custom AI solutions from the ground up to providing ongoing AI strategy consulting as things change.
Whether you're looking to bring in powerful AI tools for business operations, build specialized internal tooling for your clinical teams, or require custom healthcare software development, the right guide ensures your investment actually pays off.
Building the future of medicine is about more than just technology. It requires a shared vision and a trusted partnership, combining deep healthcare knowledge with advanced AI capabilities to create solutions that genuinely improve lives.
At Ekipa AI, we're focused on turning big ideas into executed reality. We invite you to connect with our expert team to talk about how we can help you tackle these challenges and realize what's possible with AI. Let's build the future of healthcare, together.
Frequently Asked Questions (FAQ)
1. Will AI replace healthcare professionals like doctors and nurses?
No, the primary goal of AI in medicine is to augment, not replace, human expertise. AI can handle data-intensive and repetitive tasks, which frees up medical professionals to focus on critical thinking, patient interaction, and complex decision-making. AI acts as a powerful assistant, improving efficiency and accuracy.
2. What are the main benefits of using AI in the medical field?
The main benefits include:
- Improved Diagnostic Accuracy: AI algorithms can detect patterns in medical images and data that may be invisible to the human eye, leading to earlier and more precise diagnoses.
- Personalized Treatment Plans: AI can analyze a patient's genetic and clinical data to recommend tailored therapies, increasing treatment effectiveness.
- Operational Efficiency: AI automates administrative tasks like scheduling, billing, and resource management, reducing costs and freeing up staff to focus on patient care.
- Predictive Analytics: AI can forecast patient admissions and disease outbreaks, helping hospitals manage resources proactively.
3. What challenges need to be overcome for AI adoption in healthcare?
Key challenges include:
- Data Privacy and Security: Protecting sensitive patient data in compliance with regulations like HIPAA is paramount.
- Data Quality and Bias: AI models are only as good as the data they are trained on. Incomplete or biased data can lead to inaccurate and inequitable outcomes.
- Regulatory Compliance: AI-powered medical devices must meet strict regulatory standards from bodies like the FDA to ensure they are safe and effective.
- Integration with Existing Systems: New AI tools must be seamlessly integrated into complex clinical workflows without disrupting them.
4. How can a hospital start implementing AI?
A strategic approach is best:
- Identify a Specific Problem: Start with a clear, high-impact problem, such as reducing ER wait times or improving diagnostic speed.
- Assess Readiness: Evaluate your data quality, technical infrastructure, and team skills.
- Launch a Pilot Program: Test an AI solution on a small scale to prove its value and build support. A focused pilot is a key step, as we explored in our AI adoption guide.
- Scale and Integrate: After a successful pilot, gradually scale the solution across the organization with proper training and support.
5. What are some real-world use cases of AI in medicine today?
Some prominent real-world use cases include:
- Radiology: AI tools analyze X-rays, MRIs, and CT scans to detect signs of cancer, stroke, and other conditions.
- Oncology: AI helps identify the most effective cancer treatments based on a tumor's genetic makeup.
- Hospital Administration: AI-powered systems predict patient flow, optimize staff schedules, and automate billing processes.
- Drug Discovery: AI accelerates the process of discovering and developing new medications by analyzing complex biological data.
As the momentum behind AI Use In Medical Field continues to grow, healthcare leaders need the right strategy and partners to translate potential into real-world impact. Contact our AI strategy experts to know how to move forward confidently and turn innovation into meaningful patient outcomes.