A Practical Guide to AI Deployment in Healthcare
Discover our practical guide to AI deployment in healthcare. Get a proven framework for strategy, implementation, and scaling success in clinical settings.
Bringing AI into a healthcare setting isn't some far-off idea anymore. It's happening now, and it’s essential for better patient outcomes and more efficient operations. This guide is designed to give you a real-world, practical framework for getting AI off the ground—from the initial "are we ready?" conversations to making sure your clinical teams actually embrace and use the new tools.
Getting Started with AI in Healthcare
Lots of hospitals see the promise of AI, but there's often a huge gap between that potential and putting it into practice. We're here to bridge that gap. Successfully implementing AI isn't just a tech project; it’s a fundamental change in how you operate, make clinical decisions, and care for patients. Whether you're a large hospital system or a small, independent clinic, this guide lays out a clear path to take the mystery out of the process and kick off a successful AI initiative with powerful AI solutions.
Where We Stand Today
AI adoption is definitely not a one-size-fits-all story in healthcare. The data shows a big difference depending on the size and network of a facility.
For example, by 2025, it's projected that large hospitals (over 400 beds) will see AI usage skyrocket to 90–96%. But for smaller hospitals with fewer than 100 beds, that number is much lower, sitting around 53–59%.
We see the same pattern with hospital networks. Large, multi-hospital systems are expected to reach adoption rates between 81–86%, while independent hospitals are trailing at just 31–37%.
This tells us that resources and scale are big factors, but it also creates a great opportunity for smaller organizations to learn from the experiences of the early adopters. No matter your size, those first few steps are everything, as we explored in our AI adoption guide. This visual breaks down the foundational process.
As you can see, it all starts with assessing your organization's readiness, picking a high-impact use case, and then figuring out the complex regulatory landscape.
A Step-by-Step Deployment Strategy
A successful AI rollout is a journey, not a sprint. It's an iterative process that requires a structured approach with clear, achievable goals.
The most effective strategy isn't a massive, system-wide overhaul. Instead, start with a well-defined pilot project that solves a specific, high-value problem.
This could be anything from automating tedious administrative work to helping radiologists improve diagnostic accuracy for a specific cancer. This phased approach lets you learn, adapt, and build confidence within your institution before you even think about scaling up. To get it right, you have to stay focused on the unique challenges and opportunities within the AI in healthcare industry.
Building a Foundation for AI Success
Before a single line of code is written, the fate of any healthcare AI project is often decided. It all comes down to strategic alignment and getting brutally honest about your organization's current capabilities. This foundational phase is about asking the tough questions and laying the groundwork for a project that delivers real value, not just a flashy new tool.
It all starts with a readiness assessment.
I’ve seen it happen too many times: organizations jump straight into development, only to discover their data is a mess, their staff isn't prepared for the change, or they chose the wrong problem to solve. Getting guidance from an expert in AI strategy consulting can help you avoid these classic missteps by defining clear objectives and KPIs that actually matter to your bottom line. Think of it as creating a solid roadmap before you even start the engine.
Evaluating Your Organizational Readiness
A real assessment goes way beyond your tech stack. It's a holistic look at your people, processes, and data. You need to take a hard look at your data infrastructure—is it accessible? Is it clean? Is it secure enough for this kind of work?
You also have to be realistic about your team's technical skills. Do you have the data science and engineering talent in-house, or will you need to upskill your teams or find a partner for custom healthcare software development?
The goal isn't to have a perfect score in every category. It's to identify your strengths and weaknesses so you can build a realistic deployment plan. An honest self-assessment is the first step toward a successful outcome.
This process is really a deep-dive AI requirements analysis to figure out what you truly need to succeed. Only then can you build a targeted plan to bridge the gaps and make sure your organization is actually prepared for the changes coming its way.
Choosing the Right First Project
Once you have a clear picture of your readiness, the next crucial move is picking the right use case. It's easy to get distracted by the latest AI trend, but the real wins come from solving a genuine clinical or operational problem that's already causing friction.
Start by mapping out your existing workflows to find the bottlenecks. Where are clinicians burning out on administrative tasks? Which diagnostic processes are prone to errors? Looking at real-world use cases can be incredibly helpful here, showing you how other organizations have successfully applied AI tools for business.
A smart way to do this is by prioritizing potential projects with a clear framework. A Custom AI Strategy report can be indispensable for weighing each option systematically against key criteria:
Clinical Impact: Will this project directly improve patient outcomes or safety?
Return on Investment (ROI): Can you point to a clear financial benefit, like reduced costs or better efficiency?
Technical Feasibility: Do you actually have the data you need, and is the tech mature enough for the job?
Implementation Complexity: Is this a manageable pilot project, or is it a massive overhaul that introduces huge risk?
To make this more tangible, let's look at a prioritization matrix. This is a tool I often recommend to clients to move beyond gut feelings and make data-informed decisions about where to start their AI journey.
Use Case Prioritization Matrix
| Use Case Example | Clinical Impact (High/Medium/Low) | Financial ROI (High/Medium/Low) | Data Availability (Good/Fair/Poor) | Implementation Complexity (Low/Medium/High) | Priority Score |
|---|---|---|---|---|---|
| Predictive Sepsis Alerts | High | High | Good | Medium | High |
| Automated Patient Scheduling | Low | High | Good | Low | High |
| AI-Assisted Radiology Reading | High | Medium | Fair | High | Medium |
| NLP for Clinical Note Summary | Medium | Medium | Poor | High | Low |
As you can see, a project like automated patient scheduling using AI Automation as a Service might be an ideal starting point. It has a clear ROI, uses existing administrative data, and solves a common, nagging operational headache.
By selecting a high-impact but achievable first project, you build crucial momentum. A successful pilot acts as a powerful proof-of-concept, generating the buy-in and confidence you'll need to tackle more ambitious AI solutions down the road.
2. Nail Down Your Data Governance and Compliance Strategy
In healthcare, data is everything. It’s the raw material for innovation, but it also carries an immense weight of responsibility. When you bring AI into the picture, you're handling massive amounts of sensitive patient information, which makes data governance and regulatory compliance the absolute bedrock of your project. This isn't just about checking a box; it’s about building a foundation of trust with patients, clinicians, and regulators.
You have to bake privacy and security into your system from the very beginning, not try to bolt it on later. A proactive approach, often starting with a thorough AI requirements analysis, is the only way to effectively manage risk and create a sustainable framework for your AI work.
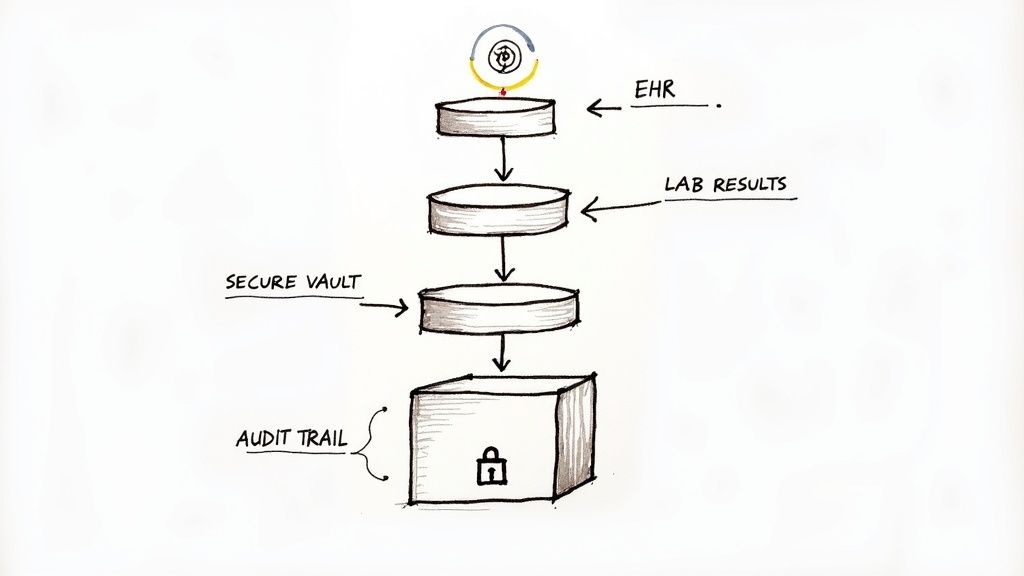
Ultimately, this process is about creating crystal-clear policies for how data is collected, stored, used, and audited across the entire AI lifecycle.
Build a Rock-Solid Governance Framework
Think of your governance framework as the rulebook for how your organization handles data. It needs to clearly define roles, responsibilities, and procedures to ensure every piece of information is managed securely and ethically. This is a team sport, requiring tight collaboration between your clinical, legal, and administrative teams—it can't just be an IT project.
Your framework must spell out a few key things:
Data Ownership: Who is ultimately on the hook for the quality and integrity of specific datasets? Is it a department head? A specific clinician?
Access Controls: How do you manage permissions? The goal is to ensure only authorized people can view or modify sensitive health information.
Data Lineage: Can you trace a single data point from its origin all the way to its use in an AI model? This transparency is non-negotiable for audits and for figuring out what went wrong when a model gives a strange result.
This structure provides the crucial checks and balances you need to maintain control over your most valuable—and sensitive—asset.
Get HIPAA and GDPR Compliance Right
If you're operating in healthcare, you live and breathe regulations like HIPAA in the U.S. and GDPR in Europe. These aren't just suggestions; they are mandatory. They’re designed to protect patient privacy, not to stifle innovation, so integrating them into your AI deployment from the start is the only path forward. For a deeper dive, there are excellent resources covering the specific HIPAA Security Rule requirements.
Here's the key takeaway: Compliance is a continuous effort. It applies to initial data collection, but also to how the AI model operates and generates insights every single day. A "compliant-by-design" mindset is the only safe way to operate.
This means putting a few key practices into action:
Data Anonymization: Use proven techniques like de-identification to strip out personally identifiable information (PII) before any data touches a model for training.
Secure Infrastructure: Your entire tech stack—whether on-premise or in the cloud—must meet strict security standards. No exceptions.
Regular Audits: Don't just set it and forget it. You need to run periodic risk assessments and audits to find and fix potential vulnerabilities in your data processes.
Get Your Data Ready for AI
Here’s a hard truth: the quality of your AI is a direct reflection of the quality of your data. Before you can even think about training a model, the raw data from your Electronic Health Records (EHRs), lab systems, and imaging archives has to be meticulously prepared. From my experience, this is often the most grueling and time-consuming part of any AI project.
This prep work boils down to a few critical activities. First is data cleaning. This is the unglamorous but vital job of finding and fixing errors, inconsistencies, and missing values. Bad data in means bad predictions out.
Next comes data labeling. This is where you bring in the experts—usually clinicians—to annotate the data and give it context for the AI. For an AI that reads chest X-rays, for instance, you'd have radiologists label images to identify specific conditions.
Finally, you have data integration. This involves pulling together information from all those siloed systems into a single, structured format that an AI model can actually work with. It ensures the model gets a complete, accurate picture to learn from. Once you have these foundational data practices locked in, you can build your AI solutions on a solid, compliant base and move forward with real confidence.
You’ve done the hard work of wrangling the data and validating your model. Now comes the real test: turning that algorithm into a tool that doctors, nurses, and other clinicians will actually use and trust. This is where the rubber meets the road, moving from the controlled environment of a data lab to the unpredictable reality of patient care.
The goal isn't just to plug in a new piece of technology. It's to seamlessly weave AI-driven insights into the fabric of daily clinical practice, making it an invisible but indispensable part of the workflow.
This is about delivering the right information to the right person at precisely the right moment, all without adding to the immense cognitive load clinicians already carry.
The Big Question: Build or Buy?
One of the first forks in the road is deciding whether to build a custom solution in-house or license a pre-built, third-party model. There’s no universal right answer here—the decision hinges entirely on your organization’s unique needs, available talent, and long-term strategy.
Building from the ground up gives you ultimate control. You can tailor the tool to your specific clinical pathways and integrate it deeply with your unique systems. This is often the best path for solving a novel or highly specialized problem where an off-the-shelf solution simply doesn't exist.
On the flip side, buying a licensed tool can get you to the starting line much faster. These solutions often come with regulatory clearance (like FDA approval) and have been validated on broad patient populations. This route lowers the development risk and can be less costly upfront, but it comes at the cost of customization. You might find yourself wrestling with a tool that doesn’t quite fit your EHR or workflow.
My Two Cents: I've seen both approaches succeed and fail. The key is to match the approach to the problem. For a highly specific workflow unique to your institution, build it. For a common, well-defined task like analyzing mammograms, a validated, licensed tool is often the smarter, faster choice.
Piloting Your AI in the Real World
Whether you build or buy, a clinical pilot program isn't optional—it's essential. This is your chance to pressure-test the AI's accuracy, safety, and utility in a controlled clinical setting before you even think about a full-scale rollout. A well-run pilot is your best insurance policy against deploying a technically brilliant tool that falls flat in practice.
A successful pilot needs a solid game plan:
Define "Success" Upfront: What are you trying to achieve? Be specific. Are you aiming to reduce diagnostic errors by 10%? Cut down patient wait times? Boost clinician satisfaction scores? These Key Performance Indicators (KPIs) are your North Star.
Find Your Champion: You need a respected clinician—a doctor or nurse—who genuinely believes in the project. Their feedback and advocacy will be critical for convincing skeptical colleagues.
Start Small: Don't go big bang. Begin with a small, motivated group of users. This creates a safe space to gather honest feedback, iron out the kinks, and polish the user interface without disrupting an entire department.
Track Everything: Collect data relentlessly. Monitor the model's performance, how users interact with the tool, and, most importantly, the clinical outcomes. This data is the evidence you'll need to make the case for a broader deployment.
The pilot is where you prove the AI’s value not just to the C-suite, but to the frontline staff whose adoption will make or break the entire project.
The EHR Integration Challenge
Here’s a hard truth: if your AI tool forces a clinician to open another window or log into a separate system, it's probably dead on arrival. They live and breathe inside the Electronic Health Record (EHR). The only way to succeed is to embed your AI’s insights directly into their existing environment.
This is often the biggest technical mountain to climb, requiring close collaboration between your clinical teams, IT department, and potentially your EHR vendor. The user interface has to be dead simple, translating complex AI outputs into clear, actionable information.
For example, an AI that predicts sepsis risk shouldn't present a confusing dashboard of statistical probabilities. It should trigger a simple, unambiguous alert directly within the patient's chart. Following a structured process, like our AI Product Development Workflow, ensures these crucial integration details aren't overlooked.
By focusing obsessively on a seamless user experience, you stop talking about AI as a disruptive technology and start treating it as a trusted co-pilot that enhances, rather than complicates, the practice of medicine.
Getting Your AI into the Hands of Clinicians
An incredible AI tool is utterly useless if clinicians don't trust it. This is where the real work begins—the human side of technology deployment. Frankly, it's often the trickiest part of getting AI off the ground in any healthcare setting. Success isn't measured by algorithmic precision alone; it’s about earning the confidence of the people on the front lines.
This is all about change management. I'm going to walk you through how to get buy-in from everyone involved: the physicians, nurses, IT staff, and administrators. A powerful algorithm is just the starting point. Driving real adoption requires a thoughtful, human-centered game plan.
It's All About Change Management
Real adoption doesn’t start on launch day. It starts months earlier with honest conversations and a clear picture of how this new tool will genuinely make a clinician's life easier or improve patient care—not just add another blinking box to their already overloaded screens.
Your strategy needs to cover a few critical bases:
Nail Down the "Why": You have to clearly articulate the specific problem this AI solves and what the real-world benefits are. Forget the tech jargon. Frame it in terms of clinical outcomes, saved time, and operational wins.
Communicate Early and Often: Get everyone in the loop from the very beginning. Regular, transparent updates stop the rumor mill cold and build a sense of shared ownership. People support what they help create.
Find Your Champions: Identify a few respected physicians and nurses who are genuinely excited about the project. Their peer-to-peer influence is infinitely more powerful than any top-down memo from administration.
A smart communication plan can turn a team of skeptics into curious supporters. As you work to drive adoption, looking into different AI-powered software development strategies can also help you build tools that users actually want to use from the start.
The biggest mistake I see is treating training like a one-and-done event. Effective training is an ongoing process. You need to support users with easy-to-access resources and continuous learning opportunities as they go from novice to expert.
From a Successful Pilot to Enterprise-Wide Rollout
Once your pilot program has proven its worth, it's time to think bigger. Scaling the initiative requires a solid governance framework to make sure the AI tool stays safe, effective, and reliable as more people start using it. A huge part of this is keeping a close eye on model performance.
AI models aren't "set it and forget it." They can degrade over time, a phenomenon we call model drift. This happens when the data the model sees in the real world starts to look different from the data it was trained on. Your governance plan absolutely must include ways to spot this drift early and a clear process for retraining or recalibrating the model to keep it accurate.
This is also the moment to get serious about the financial model. Investment in healthcare AI is exploding. Research shows that by 2025, 22% of healthcare organizations had implemented domain-specific AI tools—a seven-fold jump from the year before. Provider organizations are driving this trend, making up $1 billion of the $1.4 billion spent on healthcare AI.
Measuring What Actually Matters
Success isn't just about model accuracy or system uptime. To justify the cost and secure long-term support, you have to connect your AI deployment to measurable improvements in what the C-suite and clinicians care about: patient outcomes and operational efficiency.
Think about tracking metrics like these:
Lower patient readmission rates: Is the AI tool helping your team identify at-risk patients before they fall through the cracks?
Reduced administrative burden: Has a tool like our Clinic AI Assistant automated tedious tasks and given valuable time back to your staff?
Faster diagnostic turnaround: Are clinicians getting the critical information they need sooner?
Better patient satisfaction scores: Is the new, AI-assisted workflow creating a smoother, better experience for patients?
When you focus on these tangible results, you build a powerful, evidence-based case for the value your AI initiative is delivering. This data doesn't just prove the ROI; it reinforces the trust of your clinical teams, creating a positive feedback loop of adoption and improvement.
Your Path Forward in Healthcare AI
Getting AI right in healthcare isn't about flipping a switch on a single project. Think of it as a continuous journey that rests on four critical pillars: strategic readiness, bulletproof data management, seamless technical integration, and perhaps most importantly, human-centered change management. It’s an iterative loop—you learn, adapt, and improve with an unwavering focus on better patient outcomes and smarter operations.
The financial momentum behind this shift is staggering. Global spending on healthcare AI was already at $19.3 billion in 2023, but it’s expected to explode to $613.8 billion by 2034. Venture capital is pouring in too, hitting $11.1 billion in 2024, a 54% jump from the year before. The industry is placing its bets, and you can read the full report on these market insights to see just how big this wave is.
Charting Your Next Steps
So, where do you start? The most practical first move is an honest, no-fluff assessment of where your organization stands today. From there, pinpoint a single, high-impact pilot project. Starting small and focused is the key to building momentum and learning invaluable lessons you can apply to larger, more ambitious rollouts down the road.
A well-chosen pilot project is more than just a test run. It’s your internal proof of concept—the very thing that will generate the buy-in and hard evidence you need to justify a broader AI strategy.
Navigating this complex territory is much easier with a seasoned partner. At Ekipa, we specialize in turning ambitious healthcare AI ideas into scalable, real-world impact. Whether you need a powerful AI Strategy consulting tool to map your course or hands-on help building out internal tooling that works with your existing systems, we provide the expertise to get you there faster.
To see how we can help you build and deploy effective AI solutions that make a difference, get in touch with our expert team today.
FAQs on Healthcare AI Deployment
What is the biggest challenge in healthcare AI deployment?
The single biggest hurdle isn't developing the algorithm, but integrating it seamlessly into complex clinical workflows. This includes ensuring interoperability with existing EHR systems, managing data governance and HIPAA compliance, and—most importantly—earning the trust and buy-in of frontline clinicians who must use the tool every day.
How do you choose the first AI project for a hospital?
Start small with a high-impact, low-risk project. Focus on solving a specific, measurable problem like reducing patient no-show rates, automating prior authorizations, or optimizing operating room scheduling. Choosing a use case with clear ROI and readily available data, such as leveraging AI Automation as a Service, builds momentum and demonstrates value quickly.
What are the key steps for deploying AI in healthcare?
A successful deployment follows a clear path:
Readiness Assessment: Evaluate your data infrastructure, team skills, and strategic goals.
Use Case Selection: Prioritize a project with high clinical or operational impact.
Data Governance: Establish robust protocols for data security, privacy, and compliance (HIPAA/GDPR).
Pilot Program: Test the solution in a controlled environment to validate its effectiveness and usability.
Integration & Training: Embed the AI into clinical workflows (e.g., EHR) and provide comprehensive training.
Scale & Monitor: Roll out the solution more broadly while continuously monitoring performance and outcomes.
How do you measure the success of an AI implementation in healthcare?
Success should be measured across multiple domains. Key performance indicators (KPIs) should include:
Clinical Outcomes: Improved diagnostic accuracy, reduced readmission rates, better patient safety.
Operational Efficiency: Decreased administrative costs, shorter patient wait times, optimized resource allocation.
Financial ROI: Increased revenue, reduced operational expenses, faster billing cycles.
User Adoption & Satisfaction: High engagement rates from clinicians and positive feedback.
Ready to turn your AI vision into a clinical reality? Ekipa AI delivers tailored AI strategies and end-to-end execution to help you navigate the complexities of healthcare innovation. Start building your custom AI roadmap today.