A Practical Clinical AI Adoption Roadmap for Healthcare
Navigate AI implementation in healthcare with our practical clinical AI adoption roadmap. Learn proven strategies for seamless integration and transformation.
A clinical AI adoption roadmap isn't just a technical document; it's a strategic plan that bridges the gap between an AI concept and its real-world clinical application. It starts by defining a sharp vision with measurable goals, ensuring every step—from assessing your data to running a pilot—is directly tied to improving patient care and operational efficiency.
Building Your Foundation for AI in Healthcare
Diving headfirst into AI without a solid plan is a fast track to expensive, dead-end pilot projects. I've seen it happen too many times. A successful AI journey starts with a clear vision and a strong foundation, not with shiny new technology.
This initial phase is the most important part of your clinical AI adoption roadmap. It's what separates the projects that deliver real value from those that fizzle out. This isn't just about picking the right AI tools for business; it's about fundamentally shifting how your organization thinks about technology and problem-solving. Grounding your efforts in real-world clinical needs is the only way to avoid costly mistakes.
Assemble a Multidisciplinary Steering Committee
Your first move? Form a dedicated AI steering committee. This isn't just another meeting on the calendar; it's the brain trust for your entire AI initiative. You absolutely must bring together diverse expertise to get a balanced, 360-degree view. True buy-in only happens when every key group has a seat at the table.
Your team should include:
- Clinicians: They're on the front lines. They know the pain points and can tell you if a solution will actually work in a real clinical workflow.
- IT Experts: They'll handle the technical feasibility, infrastructure demands, and critical data security protocols.
- Data Scientists: They can realistically assess your data's quality and readiness, and tell you what's possible with the AI models you're considering.
- Administrators: They connect the AI goals to the broader business objectives, manage the budget, and champion the project with leadership.
This collaborative structure is your best defense against "shadow AI"—those one-off tools that departments implement without proper IT oversight. Those rogue projects can introduce massive security and compliance risks.
The process of setting your vision, building a team, and assessing where you stand is the bedrock of your entire strategy.
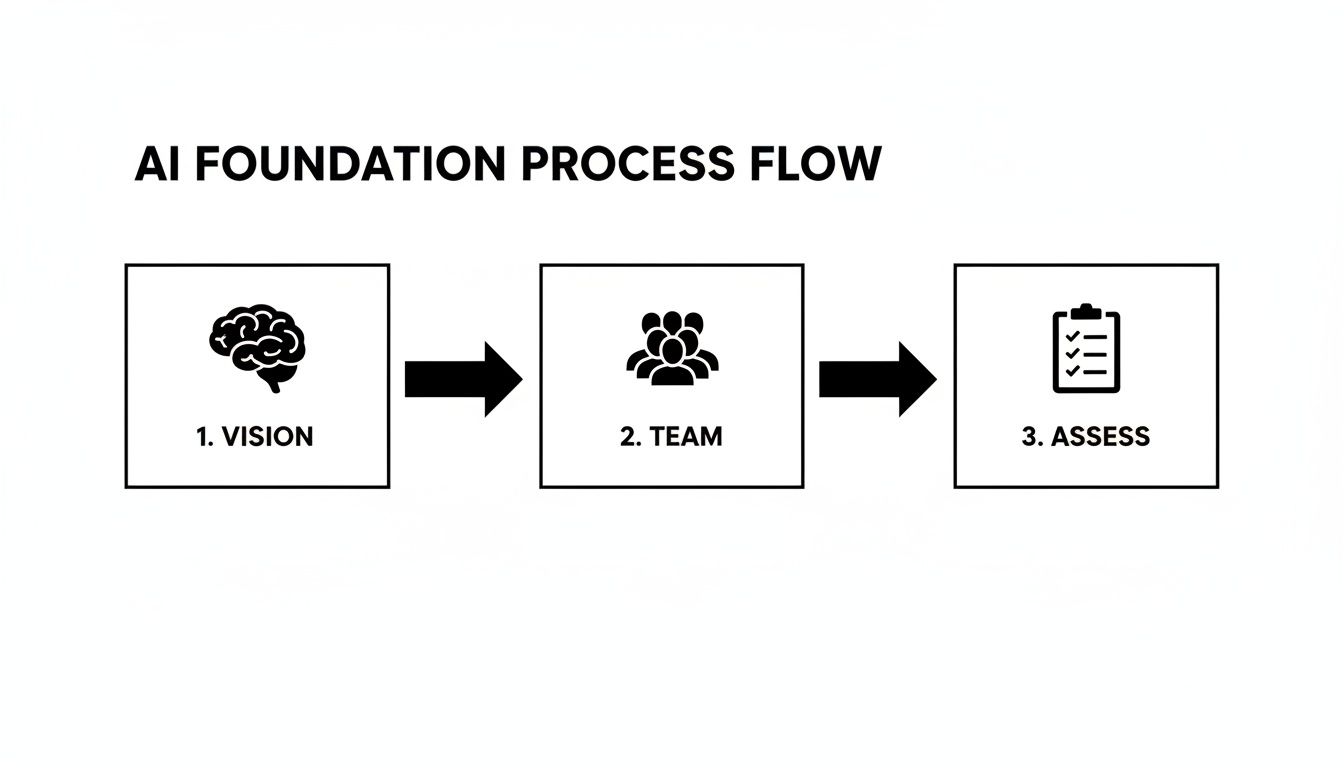
As you can see, it's a sequential process. You can't build the right team without a clear vision, and you can't assess your readiness without knowing what your team needs to accomplish.
Define Sharp, Measurable Targets
Vague goals like "improving patient outcomes" are useless. They're impossible to measure and set your project up for failure from day one. Your committee’s first major task is to establish sharp, quantifiable targets that anchor your AI strategy to real-world results.
Don't aim for general improvements. Get specific. A goal like "reduce diagnostic errors in radiology by 15% within 18 months" is powerful. It gives your team a clear finish line and a benchmark for success.
This level of specificity is what gets executive sponsors to sign on and helps you prove the ROI down the line. It turns a cool tech idea into a compelling business case.
Conduct an Honest AI Readiness Assessment
Once you have a team and clear goals, it's time for a brutally honest look at your organization's current state. This isn't the time for wishful thinking. Your assessment needs to cover three core pillars:
- Infrastructure: Do you actually have the computing power, cloud setup, and data storage to handle AI models at scale?
- Data Maturity: Is your data clean, accessible, and standardized? An AI model is only as good as the data it’s trained on. This is non-negotiable.
- Workforce Skills: Does your team have the expertise to manage, interpret, and maintain these AI systems? Find the skill gaps now so you can plan for hiring or training.
Formalizing this vision and assessment is the final step in laying your foundation. Crafting a Custom AI Strategy report provides a documented blueprint that solidifies executive support and prepares you for scalable success. Getting this initial planning right, guided by expert insight, ensures your AI journey begins on solid ground.
Choosing AI Use Cases That Deliver Real Value
Alright, you've got your strategy sketched out. Now comes the hard part: cutting through the marketing noise to find AI applications that actually make a difference on the ground. This is where the rubber meets the road, turning your high-level plans into a real project that delivers tangible results.
Let’s be honest, not all AI solutions are worth your time. The trick is to stop asking, "What's the cool new thing AI can do?" and start asking, "What are our biggest, most persistent problems?" That simple shift in perspective is what separates a successful AI initiative from a costly science experiment.

This isn't about throwing darts at a board. You need to do your homework with a thorough AI requirements analysis. This helps you realistically weigh the feasibility, potential return, and clinical impact of every idea on your list.
Pinpoint High-Impact Areas
So, where do you even start looking? My advice is to hunt for friction. Look for the bottlenecks, the time-sinks, and the frustrating manual tasks that drive your clinicians crazy. That’s usually where you'll find gold.
A few classic examples I've seen work time and again include:
- Automating Clinical Documentation: Clinician burnout is a crisis, and the "pajama time" spent on charting is a huge contributor. AI that can automate notes or summarize patient histories gives clinicians back precious hours.
- Augmenting Diagnostic Imaging: Think of AI as a second set of expert eyes for your radiologists. It’s brilliant at spotting subtle patterns in scans that a person might miss after a long shift.
- Personalizing Treatment Plans: Instead of relying solely on broad protocols, AI can analyze massive datasets to suggest which treatments are most likely to work for a patient with a very specific profile. It's a huge step toward true precision medicine.
If you’re stuck for ideas, browsing real-world use cases can spark some inspiration. The goal is to match a significant, solvable problem with the data and resources you actually have. For many organizations, bringing in specialized Healthcare AI Services can be a smart move to navigate this critical selection process.
Prioritize Quick Wins to Build Momentum
For your first one or two projects, don't try to boil the ocean. Go for the "quick wins"—initiatives with a clear, direct path to a measurable outcome. A successful early project does more than just solve one problem; it proves the value of your entire AI program to stakeholders and quiets the skeptics.
For instance, an AI tool that predicts patient no-shows to optimize scheduling is a perfect first project. It has a direct, easy-to-calculate financial and operational benefit. Nailing something like this can unlock the political and financial capital you'll need for more ambitious clinical projects later on.
If there's one thing to remember, it's that early success breeds confidence and investment. Don't start with your biggest, gnarliest problem. Pick a manageable challenge, deliver clear results, and build from there.
The industry is moving fast. The era of endless pilot projects is over. With 54% of 2025 digital health funding going to AI startups, the expectation by 2026 is for rapid, full-scale deployments that show real ROI—clinically, operationally, and financially.
Set Clear Key Performance Indicators
Before you write a single line of code, you need to know what success looks like. How will you measure it? You have to define your Key Performance Indicators (KPIs) upfront. And they can’t be fuzzy. They need to be specific, measurable, and tied directly to the problem you set out to solve.
You'd be surprised how often this is overlooked. Here’s what I mean:
| Vague (Bad) KPI | Specific (Good) KPI |
|---|---|
| Improve clinician efficiency | Reduce clinician administrative time per patient by 30% |
| Enhance diagnostic accuracy | Decrease false-negative rates in mammography screenings by 10% |
| Optimize bed management | Lower average patient length-of-stay for post-op recovery by 12 hours |
Setting these targets makes every project accountable. It turns your AI initiative from an interesting tech demo into a core business strategy, which is absolutely essential for getting long-term support and funding. This kind of structured approach is a cornerstone of our AI Product Development Workflow because it ensures value isn’t just promised—it’s proven.
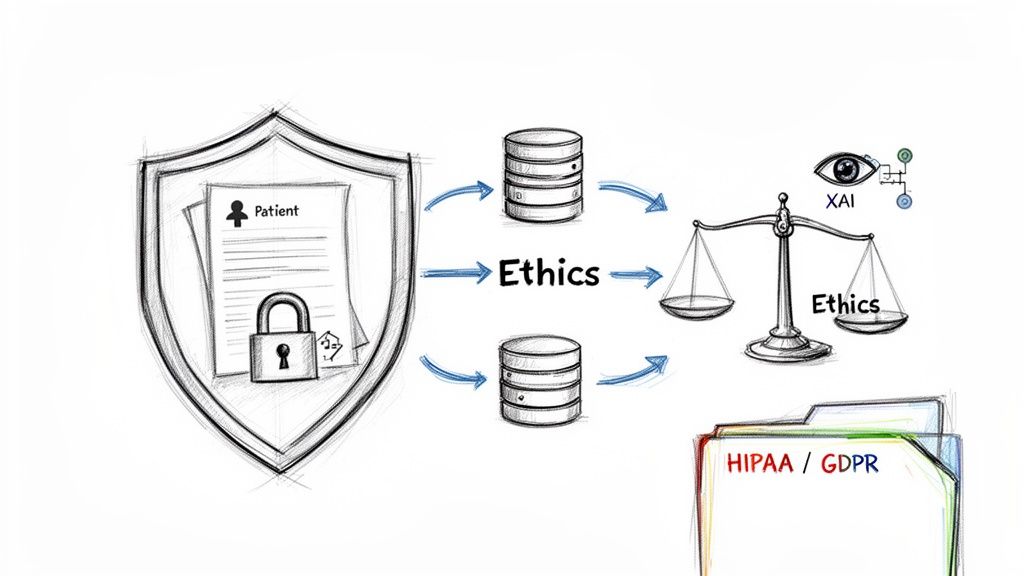
Getting Data Governance and Ethical AI Right
In healthcare, data isn't just data—it's the foundation of every clinical decision. When you bring AI into the mix, the responsibility magnifies tenfold. This is where strong data governance and a practical ethical framework become non-negotiable. They are the absolute cornerstones of a successful clinical AI adoption roadmap.
Get this wrong, and you risk everything: eroding patient trust, facing steep regulatory fines, and derailing your entire AI program before it even gets off the ground. This isn't about ticking compliance boxes; it's about building a system that your clinicians and patients can actually trust.
First, Get Your Data House in Order
You can't build a powerful AI model on a shaky data foundation. Before you even write a single line of code, you have to establish a robust data governance strategy. This is the unglamorous but essential work that ensures the quality, security, and integrity of the information that will eventually fuel your algorithms.
Your strategy needs to be crystal clear on a few key points:
- Data Quality Standards: How are you defining and enforcing data accuracy, completeness, and consistency? Remember, AI models trained on garbage data produce garbage results—a gamble you can't afford to take with patient care.
- Data Security Protocols: Who can access patient data, and under what specific circumstances? This means defining everything from encryption standards and access controls to a schedule for regular security audits.
- Interoperability: How will you pull together and standardize data from disparate systems like EHRs, labs, and imaging archives? Most meaningful AI requires a holistic patient view, which is impossible when your data lives in disconnected silos.
Untangling the Regulatory Web
The regulatory environment for AI in healthcare is a complex, shifting maze. Your governance plan has to be nimble enough to navigate a web of rules that, while varying by region, all point toward protecting patient privacy and safety.
You’ll be dealing with heavy hitters like:
- HIPAA (Health Insurance Portability and Accountability Act): The bedrock of patient data privacy in the United States.
- GDPR (General Data Protection Regulation): Europe’s comprehensive data privacy law.
- EU AI Act: A groundbreaking regulation imposing strict requirements on high-risk AI systems, a category that includes many medical applications.
Staying compliant is a continuous process, not a one-and-done task. It demands constant vigilance and a deep understanding of how each rule applies to your specific AI projects. For a more detailed look at building these frameworks, this article offers excellent guidance on AI ethics, compliance, and risk management.
Building an Ethical Framework That Earns Trust
Beyond the letter of the law lies the spirit of it: ethics. Your ethical AI framework is your public commitment to fairness, transparency, and accountability. It's how you show clinicians and patients that you're building technology with their best interests at heart.
Algorithmic bias is a silent but potent threat. Many older algorithms used race as a biological factor when it is, in fact, an entirely social construct. This flawed logic reinforces inequities and can lead to deprived communities receiving delayed or inappropriate care.
Your framework must tackle this head-on. A smart move is to establish a dedicated AI ethics review board. This team—made up of clinicians, data scientists, ethicists, and patient advocates—should vet every proposed AI project for potential bias before a single dollar is spent on development.
Another key piece of the puzzle is what we call "explainable AI" (XAI). Clinicians are rightfully skeptical of "black box" algorithms that spit out recommendations without any reasoning. XAI tools pull back the curtain, showing the "why" behind an AI's conclusion. This gives doctors the context they need to confidently make the final call, ensuring AI acts as a trusted co-pilot, not an opaque oracle. This commitment to ethical guardrails is what truly defines a mature clinical AI adoption roadmap.
Putting Your AI to the Test: Running Pilots That Prove Real-World Value
Alright, you’ve laid the groundwork with a solid strategy and clear ethical guardrails. Now comes the moment of truth: moving your AI solution from a controlled environment into a live clinical setting. This is the pilot phase, and it’s where the theoretical benefits of your model must prove themselves against the chaotic, unpredictable reality of day-to-day patient care.
Let's be clear: a successful pilot isn't about a flawless launch. It's about learning, and learning quickly. This is where you unearth the hidden friction points—the workflow snags and integration bugs—that you simply can't predict on a spreadsheet.
Design a Pilot with a Laser-Sharp Focus
The single biggest mistake I see teams make is trying to boil the ocean. A successful pilot has a tightly defined, almost narrow, scope. Don't try to test every feature for every patient in every department. Start small, get it right, then expand.
Before you begin, get your core team in a room and hammer out the answers to these questions:
- What’s our number one hypothesis? Be specific. For example, "This AI tool will reduce nurse documentation time on evening shifts by 25%."
- Who is our ideal pilot team? You need champions. Look for a clinical group that's not just tech-savvy but is genuinely open to change and willing to provide honest feedback.
- What’s a realistic timeline? I’ve found that a 90 to 120-day window is the sweet spot. It’s long enough to collect meaningful data but short enough to keep everyone engaged and maintain momentum.
A focused scope stops your pilot from turning into a never-ending research project and keeps the entire team zeroed in on proving tangible, measurable value.
Make Integration Invisible
Clinician adoption lives and dies by one simple rule: don’t disrupt the workflow. If your shiny new AI tool forces a doctor to log into another system, remember a separate password, or click through five extra screens, they won’t use it. End of story.
The technical goal of your pilot should be to embed the AI so deeply into existing systems—ideally the EHR—that it feels like a natural extension of the tools they already use every day. It should be a helpful assistant, not another administrative burden.
Collect the Numbers and the Stories
To truly validate your pilot, you need to look beyond the algorithm's performance. You need to capture both the hard data and the human experience. They are two sides of the same coin.
The quantitative metrics provide the objective proof you need for executive buy-in. These are your non-negotiables:
- Improvements in diagnostic accuracy
- Reductions in false positive or negative rates
- Time saved on specific administrative tasks
But numbers alone don't tell you why something is or isn't working. That's where qualitative feedback from your frontline staff becomes invaluable.
You have to talk to them. Set up regular, informal check-ins. Ask direct questions: "Does this tool actually make your day easier? Do you trust its recommendations?" This is where you’ll find the gold—the crucial insights needed to refine the solution before you even think about a full-scale rollout. A hands-on AI strategy workshop can be a fantastic way to gather this kind of direct user feedback in a structured setting.
Fortunately, you're pushing on an opening door. Clinicians are more receptive to AI than ever. Recent data shows that 52% feel somewhat positive and another 25% feel very positive about AI's role in healthcare. This growing acceptance means a well-designed pilot has a real chance to turn a promising idea into a proven clinical asset.
To help structure your evaluation, a validation framework is essential. It ensures you're assessing the pilot from every critical angle—clinical, technical, and operational.
Clinical AI Pilot Project Validation Framework
This framework outlines the key areas to assess during a clinical AI pilot project, ensuring you have a comprehensive view of its performance and readiness before making decisions about scaling.
| Validation Area | Key Questions to Answer | Example Metrics |
|---|---|---|
| Clinical Efficacy | Does the AI model perform accurately and reliably in a live clinical environment? Does it improve diagnostic or therapeutic outcomes? | - Model accuracy, sensitivity, specificity - Reduction in diagnostic errors - Time to diagnosis/treatment |
| Workflow Integration | How seamlessly does the tool fit into existing clinical workflows? Does it add or reduce administrative burden? | - Clicks to complete task - Time spent interacting with the AI - User satisfaction scores (SUS) |
| User Adoption & Feedback | Are clinicians actually using the tool? Do they trust it? What are the biggest points of friction or delight? | - Daily/weekly active user rates - Qualitative feedback from interviews - Error reporting frequency |
| Technical Performance | Is the system stable, fast, and reliable? Can it handle real-world data loads and user queries without crashing? | - System uptime/availability - Latency/response time - Number of technical support tickets |
| Operational & Financial Impact | Does the solution demonstrate a potential for positive ROI? Does it impact resource allocation or operational efficiency? | - Time saved per patient/case - Reduction in supply waste - Estimated cost-per-use |
By systematically working through a framework like this, you can move beyond a simple "it works" conclusion. You’ll have a rich, evidence-based understanding of the AI's true value and a clear path forward for broader implementation.
Scaling Solutions for Enterprise-Wide Impact
Getting a pilot program off the ground and seeing it succeed is a huge win. But let's be honest—that's not the finish line. The real test is taking that validated AI solution and scaling it across the entire organization. This is the moment where many promising AI initiatives either stall out or truly prove their worth.
Moving from a controlled experiment with a handful of users to a system-wide reality is a massive leap. It introduces a whole new set of technical and, more importantly, human challenges. You're no longer just managing a small, enthusiastic group; you're fundamentally changing how hundreds or even thousands of people work.

Fortifying Your Technical Backbone
The first reality check comes from your infrastructure. An AI model that runs smoothly for a 50-person pilot will absolutely buckle under the weight of 5,000 users. Your IT team’s focus has to pivot from proving a concept to building a resilient, enterprise-grade cloud architecture.
At this stage, the conversation shifts from the algorithm itself to the scaffolding that supports it. You have to nail a few key things:
- Scalability: Can your system automatically ramp up computing resources to meet fluctuating demand without a human touching it?
- Data Pipelines: You need to build efficient, automated pathways to get data from all your different sources into the AI model and back out again.
- Security: This is non-negotiable. You must implement robust, enterprise-level security protocols to protect sensitive patient data at a massive scale.
This is often where bringing in specialized Healthcare AI Services can make a world of difference. They’ve built these systems before and can help you avoid common pitfalls.
Navigating the Human Side of Change
I'll say it again: technology is the easy part. The people are what make or break a rollout. The single biggest barrier to scaling AI is almost always resistance from the very clinicians it's supposed to help. Change management can't be an afterthought—it has to be at the core of your deployment strategy.
Your mission is to make the AI tool an indispensable part of daily care, not just another piece of software clinicians are forced to learn. To get real buy-in, you need an empathetic, clear strategy that puts them first.
I’ve seen so many organizations get this wrong. They focus training exclusively on the "how"—which buttons to click. You have to lead with the "why." Show clinicians how this tool will directly solve their biggest frustrations, whether that’s slashing documentation time or giving them a reliable second opinion on a tricky scan.
When you frame it that way, the conversation shifts. It’s no longer a top-down mandate; it’s a collaborative effort to improve patient care and fight burnout.
Continuous Monitoring and Model Management
An AI model is not a piece of equipment you install and forget about. It's a dynamic system that can degrade over time in a process we call model drift. This happens when the real-world data the model sees in production starts to look different from the data it was trained on, causing its accuracy and reliability to slowly erode.
For patient safety and clinical efficacy, you must have a plan for continuous monitoring and lifecycle management. This isn't optional. It involves:
- Performance Tracking: Constantly keeping an eye on the model’s accuracy, fairness, and outputs against your established benchmarks.
- Feedback Loops: Creating dead-simple ways for clinicians to report anomalies or incorrect outputs right from their workflow. A "flag for review" button is a great start.
- Scheduled Retraining: Planning regular intervals to retrain the model with fresh, real-world data to keep it sharp and relevant.
Managing this lifecycle is complex, which is why platforms offering AI Automation as a Service are becoming more common. They can handle the heavy lifting of keeping models performant.
The numbers tell a compelling story. The global AI in healthcare market is projected to skyrocket from $39 billion in 2025 to $504 billion by 2032. Yet today, only a tiny 2% of health systems are actually operating AI at an enterprise-wide scale. That gap represents the scaling challenge—but also the immense opportunity for organizations that get it right. You can discover more insights about the global health care outlook to understand this trend better. This final, crucial phase is what determines whether your AI investment delivers a lasting, meaningful return.
Frequently Asked Questions (FAQ)
Embarking on a clinical AI adoption roadmap is a major undertaking, and it’s natural to have questions. Here, we tackle some of the most common ones we hear from healthcare leaders.
Where Do We Even Begin with AI?
The right place to start has nothing to do with algorithms or software. It’s all about your strategy. Before you ever think about a vendor, you need to get crystal clear on what specific problems you need AI to solve.
Your first move should be to pull together a team with leaders from clinical, IT, and administrative departments. The goal isn't just to talk about AI; it's to set concrete, measurable goals. Don't settle for "improve patient outcomes." Get specific: "Reduce readmission rates for congestive heart failure by 20%."
Getting this strategic alignment right from the beginning, often with the help of specialized AI strategy consulting, is what separates successful projects from stalled ones. It ensures every dollar spent and every hour worked is aimed at a target that truly matters to the organization.
How Do You Actually Measure the ROI of Clinical AI?
Thinking about ROI purely in financial terms is a common mistake. A true measure of success looks at the return from three different angles.
- Clinical ROI: Are patient outcomes improving? Think better diagnostic accuracy, fewer medical errors, or faster recovery times.
- Operational ROI: Is the hospital running more smoothly? This is about efficiency gains, like clinicians spending less time on paperwork or optimizing patient flow with better internal tooling.
- Financial ROI: Are we saving money or generating new revenue? This is where you see the direct impact on the bottom line, like a shorter average length of stay for patients.
The trick is to benchmark everything before you start. You need to know your baseline to prove the investment paid off. Honestly, some of the most powerful returns come from simply giving clinicians more time to focus on patient care. That single change has a ripple effect that touches everything from patient satisfaction to your finances.
If you only chase financial ROI, you'll miss the bigger picture. The operational wins—like reducing clinician burnout—often deliver the most significant long-term financial benefits by improving staff retention and patient safety.
What Are the Biggest Roadblocks to Adopting AI in a Hospital?
From our experience, the technology itself is rarely the biggest hurdle. The real challenges are almost always cultural and operational. We see the same three roadblocks time and time again.
- Messy Data: AI is completely dependent on the data it's trained on. Healthcare data is notoriously siloed, inconsistent, and incomplete. Getting your data house in order is a non-negotiable first step.
- Clunky Workflow Integration: If a new AI tool disrupts how clinicians work or feels like just another screen to click, they won't use it. It has to feel like a natural part of their day, which usually means seamless EHR integration. Some health systems even opt for custom healthcare software development to get this just right.
- Lack of Trust: You can't just drop a new AI tool on your staff and expect them to embrace it. Building trust requires total transparency about how the tool works, extensive training, and clear proof that it genuinely makes their jobs easier, not harder.
Realistically, How Long Does It Take to Implement an AI Solution?
This is the classic "it depends" question, but the timeline really does vary dramatically. A tightly focused pilot project, like implementing an AI-powered documentation scribe for a single department, could go from planning to live in about 4-6 months.
On the other hand, a massive, system-wide initiative like a sepsis prediction model that needs to be integrated across multiple hospitals could easily take 18-24 months or longer. The timeline is dictated by the cleanliness of your data, regulatory hoops you have to jump through, and the sheer complexity of IT integration.
As we explored in our AI adoption guide, the smartest approach is almost always to start small, prove the value, and then scale up.
Ready to move from vision to reality? Ekipa AI provides the hands-on strategy and execution support to truly transform your clinical operations. Let our expert team build a practical roadmap that delivers a real impact. Get your custom AI strategy.



