Clinical Workflow Optimization: Elevate Care with AI-Driven Efficiency
Discover clinical workflow optimization with practical AI-driven tactics to streamline patient care, cut wait times, and boost healthcare efficiency.
Clinical workflow optimization isn't just a buzzword; it's the meticulous process of re-engineering how work gets done in a healthcare setting. It's about taking a hard look at the way tasks, information, and even patients move through your system to root out inefficiencies, cut down on administrative waste, and ultimately improve patient care. In today's complex healthcare world, this is fundamental to building a resilient, patient-focused operation.
Why Clinical Workflow Optimization Is a Strategic Imperative
Let's be clear: optimizing your clinical workflows is no longer a "nice-to-have" operational tweak. It’s a core business strategy. Healthcare organizations are getting squeezed from every direction—skyrocketing operational costs, crippling staff shortages, and a burnout crisis that threatens the well-being of our clinicians. These aren't minor headaches; they directly threaten your financial stability and the quality of care you provide.

The frustrating part? So many of these problems aren't about the medicine itself. They stem from the clunky, outdated administrative and operational processes that are supposed to support care delivery. When a physician spends more time wrestling with an EHR than talking to a patient, you have a systemic failure on your hands. This is precisely where investing in workflow improvement gives you a powerful competitive edge.
Turning Systemic Challenges into Opportunities
The smartest leaders see these systemic pressures not as threats, but as catalysts for change. By getting to the root causes of inefficiency, you can unlock incredible value. The ultimate goal is to build an environment where your clinical teams can practice at the top of their license, focusing on high-value patient care instead of fighting with clunky software and redundant paperwork.
Making this happen takes more than just a few minor process adjustments. It requires a thoughtful and strategic application of technology. Advanced AI solutions are playing a huge role here, bringing intelligent automation and data-driven insights to the table in ways we couldn't imagine just a few years ago.
The market is moving fast to meet this demand. The global clinical workflow solutions market was valued at USD 9.56 billion in 2022 and is expected to surge to USD 23.71 billion by 2030. With North America alone accounting for a 41.8% market share, it’s obvious that this is one of the most heavily invested areas in healthcare technology today. You can explore more data on the clinical workflow market trends to see just how quickly this space is evolving.
By tackling workflow inefficiencies head-on, you're not just putting out fires. You're building a foundation for sustainable growth, better clinical outcomes, and a workforce that actually wants to stick around.
The Role of Specialized AI in Healthcare
The right strategy uses technology to smooth out those complex processes, turning operational drags into engines of efficiency. Our work delivering specialized Healthcare AI Services is all about pinpointing and fixing the most critical bottlenecks first.
This usually breaks down into three key areas:
- Automating Repetitive Tasks: Get your clinical staff out of the weeds of manual data entry, tedious scheduling, and endless documentation.
- Improving Communication: Make sure information flows effortlessly between departments, care teams, and even patients, eliminating dangerous gaps.
- Providing Decision Support: Give clinicians real-time, actionable insights so they can make faster, more confident decisions right at the point of care.
By zeroing in on these high-impact areas, healthcare organizations can see a real, measurable return on their investment. We're not just talking about saving money; we're talking about tangible improvements in patient safety and a much-needed boost in staff morale. It’s about building a smarter, stronger healthcare system from the inside out.
Before you can fix a problem, you have to know exactly what it is and where it lives. Jumping straight to solutions without a deep dive into your current processes is a recipe for wasted time and money. Real, lasting clinical workflow optimization begins with a clear-eyed audit to find the hidden friction points slowing your team down.
This isn't just about noting that appointments are running late. It's about systematically mapping your clinical pathways to pinpoint precisely where, when, and why those delays are happening. It’s as much about people and processes as it is about technology.
A structured AI requirements analysis is the perfect starting point. It makes sure that any investment in AI tools for business is aimed at solving problems you've actually identified, not just slapping a tech bandage on a symptom.
Trace the Flow of Patients and Information
The best way to see the whole picture is to map it out. I’ve found that Value Stream Mapping (VSM) is incredibly effective here. This technique forces you to follow a process from start to finish—say, from patient check-in to discharge—and document every single step along the way.
You’ll uncover what adds real value and, more importantly, what’s just waste.
For instance, mapping a patient discharge process might show that the biggest holdup is always waiting for a final pharmacist review. That’s not a vague "communication issue"; it's a specific, measurable bottleneck. Suddenly, you can quantify the average wait time and show exactly how it hurts bed turnover rates. This kind of detail is what builds a powerful business case for change.
Don't Underestimate Frontline Wisdom
Flowcharts and data will only get you so far. The most critical insights almost always come from the people on the ground: your nurses, physicians, schedulers, and medical assistants. Sitting down with them for structured interviews isn't optional—it's essential.
They’ll tell you about the workarounds and shadow processes that never show up on an official diagram. You might discover nurses are losing 30-40 minutes per shift manually cross-referencing medication lists because two key systems don't talk to each other. That’s not just an inefficiency; it’s a direct contributor to burnout and a perfect opportunity for better internal tooling to make a real difference.
"Your frontline staff are the true experts on workflow friction. They know exactly which tasks are soul-crushing and what’s getting in the way of patient care. If you ignore them, your optimization project is doomed from the start."
Dig into Your EHR's Digital Footprint
Your Electronic Health Record (EHR) is a treasure trove of objective data, if you know where to look. The audit logs contain timestamps for virtually every action, from an order being placed to a note being signed. Mining this data can uncover patterns that are impossible to spot just by watching people work.
Here are a few metrics you can pull to get started:
- Order-to-Result Time: How long does it really take from the moment a lab test is ordered until the results are back in the chart?
- Documentation Lag: What’s the average delay between a patient visit and when the clinical notes are finalized? For many physicians, this is a huge source of after-hours work.
- System Latency: Is the EHR grinding to a halt at certain times of day, creating a productivity bottleneck for the entire organization?
This data-driven approach takes the guesswork out of the equation. It gives you a hard baseline to measure against later.
To help you get started, here’s a breakdown of common pain points I've seen in practice and what usually lies beneath the surface.
Common Clinical Workflow Bottlenecks and Their Root Causes
This table identifies frequent points of friction in clinical workflows and connects them to underlying systemic issues, helping leaders diagnose problems accurately.
| Workflow Stage | Common Bottleneck Symptom | Potential Root Cause |
|---|---|---|
| Patient Intake | Long wait times; incomplete registration data | Manual data entry from paper forms; non-integrated scheduling and registration systems. |
| Clinical Encounter | Physicians spending excessive time on documentation | Clunky EHR interface; lack of templates or smart phrases; no mobile access for quick notes. |
| Orders & Referrals | Delays in processing lab orders or specialist referrals | Multi-step approval processes; poor communication between departments; lack of order tracking. |
| Care Coordination | Information gaps during patient handoffs | Inconsistent communication protocols; systems that don't share data (e.g., between hospital and primary care). |
| Patient Discharge | Delayed discharges leading to poor bed turnover | Waiting on medication reconciliation; lack of automated patient education material delivery; coordination delays. |
By identifying which of these symptoms resonate, you can quickly narrow your focus to the most likely root causes and start asking the right questions.
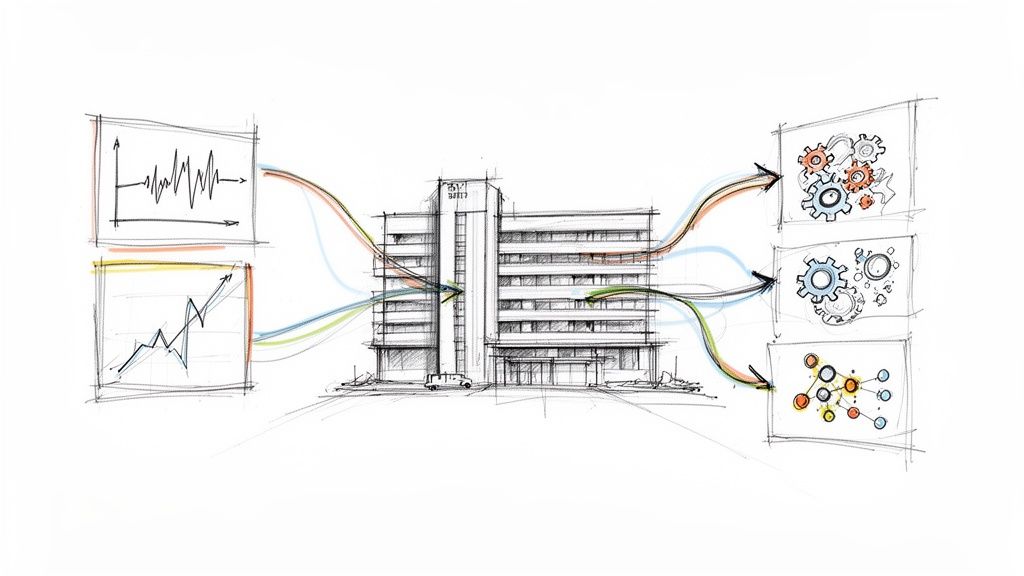
When you bring these three diagnostic methods together—process mapping, stakeholder interviews, and data analysis—you get a complete, 360-degree view of what’s really going on. This holistic diagnosis is the essential foundation for any successful workflow strategy and a core part of our Custom AI Strategy report.
Designing and Piloting AI-Augmented Workflows
You've done the diagnostic work and pinpointed the bottlenecks. Now it's time to move from analysis to action. This is where you start designing and piloting targeted solutions to fix what’s broken. The idea isn't to rip and replace everything overnight, but to strategically weave in AI and automation where they'll make the biggest difference.
We're talking about redesigning specific, frustrating processes—think automating prior authorizations or using predictive analytics to finally get patient scheduling right. Then, you test these new workflows in a controlled, real-world setting. A well-chosen pilot is your secret weapon for building momentum. It needs to be important enough to make an impact but small enough to deliver a quick, undeniable win.
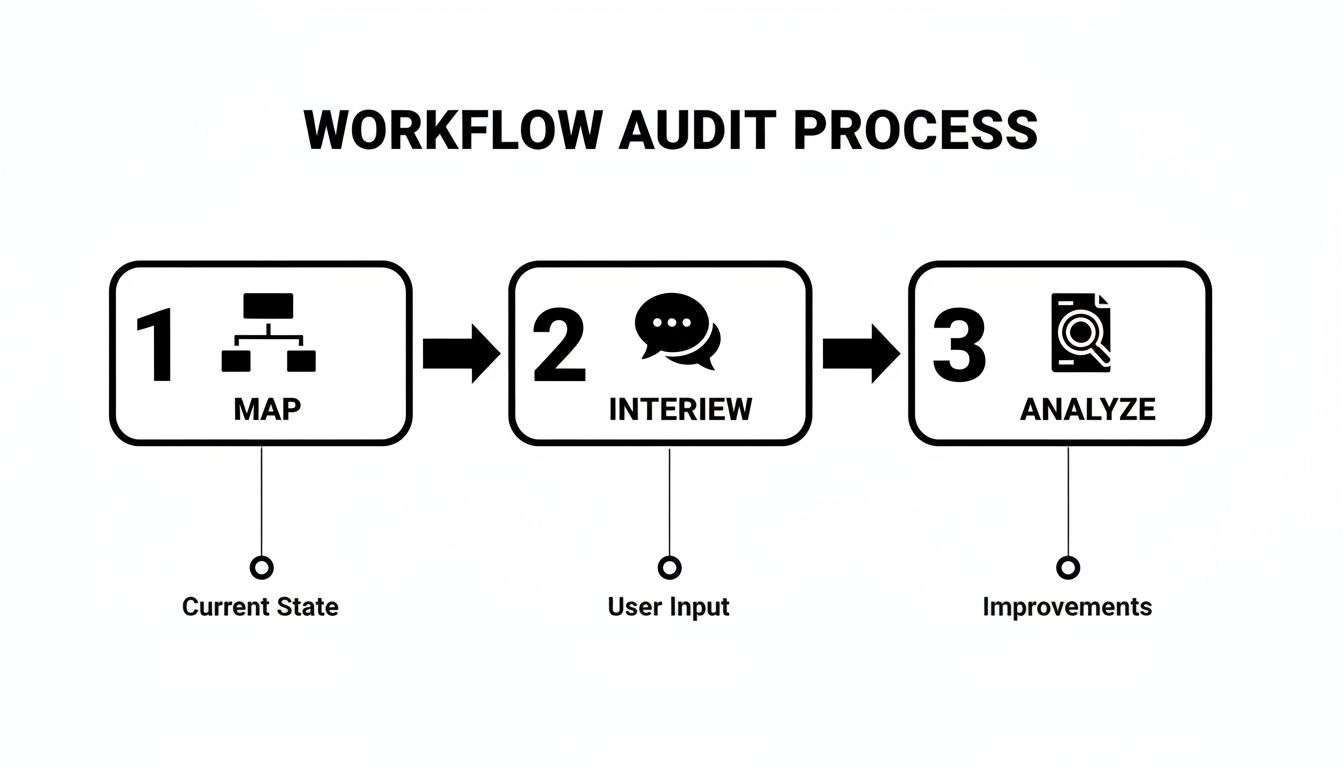
This process—Map, Interview, Analyze—is the bedrock of any successful redesign. It ensures your new workflow isn't just a tech solution looking for a problem, but a genuine fix based on how things actually work on the ground.
Finding the Right Place to Start
Let's be honest, not all bottlenecks are created equal. The trick is to find the ones that, if you solved them, would send positive shockwaves through the entire system. These are usually the repetitive, soul-crushing tasks that eat up clinical time without requiring a lot of complex thought.
Here are a few classic examples that are ripe for AI:
- Automating Prior Authorizations: This is the big one. It's a huge source of administrative bloat and, worse, delays in care. AI can be trained to pull the right documents from the EHR, submit the request, and track its status, only looping in a human when there's an exception.
- Smarter Patient Scheduling: Instead of just plugging names into slots, predictive models can analyze patterns to anticipate no-shows, optimize schedules for expensive equipment like MRI machines, and even proactively fill last-minute cancellations.
- AI-Powered Scribes: We all know documentation is a leading cause of physician burnout. AI scribes can listen in on a patient visit and draft the clinical note automatically. This gives doctors their focus back—on the patient, not the keyboard. Our own Clinic AI Assistant was built to solve this exact problem.
My advice? Pick a fight you can win. Focus on a problem that everyone in the organization already hates. Solving a universally despised frustration is the fastest way to get people on your side for the next, bigger project.
How to Design a Pilot That Actually Works
Once you've picked your target, it’s time to design a controlled pilot. Think of it less like a trial run and more like a scientific experiment. You're testing a hypothesis. For instance: "Using an AI scribe in our primary care clinic will cut physician documentation time by 50% without hurting the quality of the notes."
A solid pilot plan must include:
- A Tight Scope: Don't try to boil the ocean. Pick a single department or a small, motivated group of clinicians. Piloting a new workflow across an entire health system is a classic rookie mistake.
- Clear Metrics for Success: How will you know if it worked? Define your KPIs upfront. This could be time saved, error rates, patient throughput, or even staff satisfaction scores.
- A Control Group: This is critical. If you can, compare your pilot group to a control group still using the old method. It's the only way to get hard, evidence-based proof of the impact.
- A Feedback Loop: Set up a simple, structured way to get feedback from the clinicians involved. Their hands-on insights are gold for refining the workflow before you even think about scaling it.
It's Not Just About the Software
As you navigate this, remember that implementation is more than just buying a new piece of software. In fact, while software made up 71.89% of the clinical workflow solutions market recently, the services segment is where the real growth is—projected at 14.62% through 2030. This tells you something important: organizations are realizing they need expert guidance to make these tools stick.
This trend highlights why understanding the broader landscape of AI in healthcare is so essential for making informed decisions. It's about combining powerful technology with the expertise needed to ensure it gets adopted and delivers real value.
Successfully designing and piloting AI into your workflows is a methodical game. It demands a deep understanding of your current problems, a smart selection of where to start, and a disciplined approach to testing and measuring. By starting small, proving value, and listening to your team, you'll build the trust and the evidence you need to transform care across your entire organization.
Measuring Outcomes and Demonstrating ROI
So, you’ve piloted a new, AI-augmented process. That's a huge step. But the real work begins now: proving it was worth the effort. A redesigned workflow is only as good as its results, and to get the buy-in you need to scale, you have to show a clear, data-driven return on investment (ROI). It's time to move past feel-good stories and dig into the numbers that matter in a clinical setting.
This measurement process is a core component of our Custom AI Strategy report, where we help organizations nail down these critical metrics right from the start.

Defining Your Key Performance Indicators
The smartest way to measure the success of clinical workflow optimization is to track KPIs across three core domains: operational, clinical, and financial. This gives you a complete picture of the impact, creating a compelling story for everyone from frontline nurses to the CFO. The trick is to make sure your KPIs link directly back to the bottlenecks you uncovered in your initial diagnostic phase.
Setting Baselines and Tracking Progress
Before you even think about launching the pilot, you need to establish a clear baseline for every single KPI you plan to track. This "before" picture, pulled from your initial diagnostic data, is non-negotiable. Without it, you can't prove the "after" was a success.
Once the new workflow goes live, data collection has to be consistent. I’ve found that a real-time dashboard is the best way to visualize progress and share results with leadership. Don't just dump numbers on them; present the data as a clear, compelling narrative showing trends over time.
To truly understand the impact of your workflow changes, it's essential to track metrics across different facets of the organization. Below is a framework we use to ensure nothing gets missed, from patient flow to the bottom line.
KPIs for Measuring Clinical Workflow Optimization Success
A framework for tracking the impact of workflow changes across key healthcare domains, ensuring a comprehensive view of ROI.
| Metric Category | Key Performance Indicator (KPI) | Measurement Method |
|---|---|---|
| Operational Efficiency | Patient Throughput | Number of patients seen/discharged per day, week, or month. |
| Average Patient Wait Times | Time from check-in to provider consultation, logged in the EMR. | |
| Bed/Room Turnover Rate | Time from patient discharge to the room being ready for the next patient. | |
| Staff Time Allocation | Time-motion studies comparing time spent on administrative vs. clinical tasks. | |
| Clinical Quality | Medical Error Rate | Tracking medication administration errors or diagnostic inaccuracies. |
| Adherence to Care Protocols | Audits of patient charts against evidence-based guidelines. | |
| Patient Safety Incidents | Rate of falls, hospital-acquired infections, or other adverse events. | |
| Clinician Satisfaction Scores | Anonymous surveys (e.g., Net Promoter Score) conducted pre- and post-pilot. | |
| Financial Impact | Operational Costs | Analysis of overtime pay, supply costs, and equipment utilization rates. |
| Revenue Cycle Metrics | Days in accounts receivable, claim denial rates, or time-to-bill. | |
| Procedure/Encounter Volume | Number of billable procedures or encounters per time period. |
This table isn't just a checklist; it’s a strategic tool. By tracking these metrics, you can directly connect a smoother workflow in the ER to a healthier financial statement, making your case for expansion undeniable.
A common mistake I see is stopping the measurement process too early. Real change takes time to bake in. Keep tracking your KPIs for at least three to six months after implementation to see the full, sustained impact of what you’ve built.
By meticulously measuring outcomes and weaving them into a powerful ROI story, you build an ironclad case for change. This data-driven approach doesn’t just justify the initial investment; it creates the momentum needed to turn a successful pilot into a system-wide transformation. The insights you gather are also gold for refining your broader AI strategy consulting efforts and fostering a culture of continuous improvement.
Mastering Change Management and Scaling Success
Let's be honest: introducing new tech or redesigning a deeply ingrained process is only half the battle. You can have the most elegant, AI-driven workflow on the planet, but it's doomed if the people using it every day aren't on board. This is especially true in a clinic, where routines are built on years of practice and patient safety is everything. The human element of clinical workflow optimization is where most initiatives either succeed spectacularly or quietly wither away.
Successfully navigating this takes a real change management strategy. You can't just send out a memo and hope for the best. You have to build a coalition of supporters, relentlessly communicate the "why" behind the change, and design a new system that’s genuinely easier than the old one. It’s a common stumbling block, but it's a core part of how we approach problems.
Building a Coalition for Change
First thing's first: change can't be dictated from the top down. You need champions on the ground floor—people who can advocate for the new workflow and help their peers through the bumps.
Identify Clinician Champions: Look for those respected physicians, nurses, and techs who are naturally curious and open to innovation. Get them involved from the very beginning. Listen to their feedback, make them part of the design process, and empower them to be the go-to experts for their teams. A peer's endorsement is always more powerful than an executive's mandate.
Secure Leadership Sponsorship: While your frontline champions are essential, you also need unwavering support from the top. Clinical and administrative leaders have to consistently talk about why this project matters and be ready to clear any organizational roadblocks that pop up.
From Pilot to System-Wide Standard
So, your pilot was a success. The data looks great. Now what? The next challenge is scaling that win across the entire organization. A victory in one department doesn't guarantee a smooth rollout everywhere else. This is where a new level of planning and standardization comes in.
A successful rollout isn't just about expanding technology; it's about scaling a new standard of care. This is where a detailed AI Product Development Workflow becomes your best friend, giving you a structured path from a single successful pilot to an enterprise-wide transformation. It's the framework that ensures you maintain the quality and impact you worked so hard to prove in the first place.
The goal is to create a playbook that can be adapted for different departments while keeping the core principles intact. This means standardized training materials, clear documentation, and a solid support system to handle questions as they arise. What worked for the ED might need a few tweaks for the outpatient surgical center, but the fundamental process should remain consistent.
A critical mistake I see is treating the scale-up as a simple copy-and-paste of the pilot. Each department has its own subculture and operational quirks. You have to engage leaders from each new area to adapt the rollout plan, making them co-owners of the success.
Creating Feedback Loops for Continuous Improvement
Your work isn't over once the new workflow goes live. The best organizations treat workflow optimization as a continuous process, not a one-time project. For that, you absolutely need feedback loops.
This means creating simple, accessible ways for staff to report issues, suggest improvements, and share what's going well. Regular check-ins, quick surveys, even informal huddles can help you gauge satisfaction and spot small friction points before they become major headaches. This iterative approach keeps your workflows evolving and improving, ensuring they stay aligned with the real-world needs of your clinicians and patients.
By mastering both the technical implementation and the human side of change, you can turn a promising pilot into a new, better way of delivering care across your entire health system.
Common Questions & Straight Answers
When you start digging into clinical workflow optimization, a lot of questions come up. Leaders and tech teams often face the same hurdles. Here are some of the most common ones I hear, along with some practical advice.
So, Where Do We Even Begin?
The first move is always the same: diagnose your current state. Seriously. Before you even think about a new tool or AI, you have to get a crystal-clear picture of what's actually happening on the ground.
This isn't a quick meeting. It means mapping out your processes, digging into your EHR data to find the real chokepoints, and—most importantly—talking to your frontline staff. They know where the friction is. Jumping straight to a solution without this deep diagnostic work is the number one reason these projects fail. We designed our Custom AI Strategy report specifically to handle this heavy lifting and give you a clear, data-backed starting point.
How Can We Get Clinicians on Board, Especially the Skeptics?
You can't force buy-in; you have to earn it. The secret is to bring clinicians into the process from day one. Don't design a new workflow for them; co-design it with them.
Find your clinical champions—those respected doctors or nurses who other staff members listen to. Get them involved early. Frame the project not as a top-down mandate, but as a genuine effort to reduce their administrative headaches and burnout, so they can get back to what they love: patient care. Your best weapon against skepticism? A small, successful pilot. When people see it working and making a colleague's life easier, they'll be lining up to try it.
What's a Realistic ROI for a Project Like This?
The return on investment here isn't just about dollars and cents, though that's certainly part of it.
- Financial: You'll see lower operational costs because things just run smoother. Revenue cycle management often gets a nice bump, too.
- Operational: Patient throughput improves, and those frustrating wait times start to shrink.
- Clinical: This is the big one. We're talking about fewer medical errors and better, more consistent standards of care.
While every organization is different, most successful projects start showing major efficiency gains within 6-12 months. The trick is to lock down your baseline metrics before you change a single thing.
Key Takeaway: Build your business case around both financial and clinical metrics. That's how you get everyone from the CFO to the Chief Medical Officer excited about the possibilities.
Should We Build Our Own Solution or Buy Something Off the Shelf?
This really comes down to how unique your problem is. For standardized tasks like basic appointment scheduling or billing, an off-the-shelf product is often the fastest way to get a win.
But when you're talking about core clinical pathways that define your institution's quality of care, internal tooling or a custom build is often the smarter long-term play. It gives you a system that fits like a glove and can become a real competitive advantage.
Often, the best answer is a hybrid. You might use a commercial system as the base but build custom integrations or automated alerts on top of it. An AI strategy consulting partner can help you navigate this build-vs-buy maze by looking at your specific needs. Getting familiar with different real-world use cases can also bring a lot of clarity to the decision.
When a bespoke solution is the right call, finding a partner that specializes in custom healthcare software development is critical. The goal is always the same: align the technology with the specific workflow problems you diagnosed from the start.
Frequently Asked Questions (FAQ)
What is clinical workflow optimization?
Clinical workflow optimization is the process of analyzing, redesigning, and improving the sequences of tasks and information flow in a healthcare setting. The primary goal is to enhance efficiency, reduce administrative burdens on clinicians, minimize errors, and ultimately improve the quality and safety of patient care. It involves a combination of process mapping, technology implementation (like AI and automation), and change management.
How does AI help in optimizing clinical workflows?
AI can significantly optimize workflows by automating repetitive, low-value tasks like prior authorizations and data entry, freeing up clinicians to focus on patient care. It also provides predictive insights for smarter scheduling, offers real-time decision support at the point of care, and can even power tools like AI scribes to reduce documentation burnout, as we explored in our AI adoption guide. These capabilities lead to greater efficiency, reduced errors, and improved staff satisfaction.
What are the biggest challenges in a workflow optimization project?
The biggest challenges are typically human-centered, not technical. Securing buy-in from busy clinicians who are often resistant to change is a major hurdle. Other challenges include accurately diagnosing the true root cause of a bottleneck, integrating new tools with legacy systems like EHRs, and demonstrating a clear ROI to justify the investment. Overcoming these requires a strong change management strategy, starting with a small, successful pilot to build momentum.
How do you measure the success of clinical workflow optimization?
Success is measured by tracking Key Performance Indicators (KPIs) across three main areas: operational, clinical, and financial.
- Operational: Metrics like patient wait times, bed turnover rates, and staff time spent on administrative tasks.
- Clinical: Metrics like medical error rates, adherence to care protocols, and clinician satisfaction scores.
- Financial: Metrics like operational costs, claim denial rates, and overall revenue. Tracking these from a pre-defined baseline is essential to prove impact.
Ready to stop talking and start fixing? At Ekipa AI, we help healthcare organizations find the hidden inefficiencies in their workflows and implement smart, AI-powered solutions that actually work. Let our expert team help you build a more efficient and resilient clinical operation.