Generative AI in Healthcare Explained
Discover how generative AI in healthcare is transforming patient care, diagnostics, and clinical workflows. An essential guide to AI in medicine.
Generative AI isn't just another tech buzzword in healthcare; it's a tool that actively creates new things—from drafting clinical notes and patient emails to even designing potential drug molecules. Unlike traditional AI that just analyzes data, this technology generates it.
We're already seeing it take on the heavy lifting of administrative tasks and speed up medical research, which is starting to reshape the day-to-day work of clinicians and the way patients receive care. Let’s break down what this means for medicine, its real-world applications, and how you can strategically bring it into your own organization.
Exploring Medicine's New Frontier
Healthcare is in the middle of a massive transformation, and generative AI is right at the heart of it. This technology isn't just about crunching numbers or finding patterns; it's about creating entirely new solutions. Think personalized treatment plans generated from a patient's unique data or even novel drug compounds designed in a lab.
Here’s a simple way to look at it: Traditional AI is like a brilliant research librarian who can find any piece of information in a massive library. Generative AI, on the other hand, is like an expert author who reads everything in that library and then writes a brand-new book. It’s this creative ability that makes it so valuable for solving the complex, unique challenges we face in medicine.
The Rapid Pace of Adoption
The move toward generative AI in healthcare isn't some far-off idea—it's happening right now. The industry is wasting no time putting these tools to work to make both clinical and operational workflows better.
In fact, a 2025 survey revealed that 54% of healthcare and life science organizations are already using generative AI. Adoption is happening fastest in digital health (71%) and pharma/biotech (69%).
The most popular uses are pretty practical:
- Summarizing clinical documentation (55%)
- Powering medical chatbots (53%)
- Analyzing scientific literature (45%)
This isn't just a trend; it's a clear signal that the future of medicine involves smart systems working alongside human experts.
By automating repetitive tasks and delivering deep analytical insights, generative AI gives medical professionals their time back. They can finally focus on what they do best: caring for patients and making critical clinical decisions.
A Roadmap for This Guide
This guide is designed to give you a clear path for understanding and adopting generative AI in healthcare. We'll walk through everything you need to know to navigate this new landscape, from the basic concepts to a practical strategy.
Here’s a quick look at what we'll cover:
- How the Technology Works: We’ll break down the AI models and explain how they function in a clinical setting, without the confusing jargon.
- Clinical and Operational Use Cases: You'll see concrete examples of how AI is already improving patient outcomes and streamlining hospital management.
- Challenges and Ethics: We’ll take an honest look at the obstacles, including crucial issues like data privacy and algorithmic bias.
- Implementation Strategy: A step-by-step roadmap to help you integrate these powerful tools into your organization thoughtfully.
We'll dig into how this technology doesn't just improve what we already do but opens the door to entirely new ways of delivering care. To see how we apply this expertise, you can learn more about our work in the generative AI in healthcare industry. Consider this your guide to making smart, informed decisions as you step into this new era of medicine.
How Generative AI Works in a Clinical Setting
To really see what generative AI can do in healthcare, we need to peek under the hood at the technologies that make it tick. This isn't about getting a data science degree; it's about understanding the engine driving this shift so you can spot real opportunities in your own organization.
At the core of most of these systems are Large Language Models, or LLMs. Picture an LLM as a brilliant medical resident who has read every single textbook, clinical trial, and research paper ever published. With that massive knowledge base, it can understand and produce human-like text to draft patient summaries, answer clinical questions, or even create educational materials with impressive detail.
But a general-purpose LLM, straight out of the box, isn't equipped for the realities of medicine. It first needs to go through a process called fine-tuning.
From General Knowledge to Medical Expertise
Think of fine-tuning as sending that brilliant resident to medical school. The general model is trained on specialized, high-quality medical data—things like anonymized electronic health records (EHRs), medical imaging reports, and peer-reviewed studies. This process shapes the model’s responses, making them clinically accurate, safe, and relevant to the medical field.
This step is absolutely critical for a few key reasons:
- Clinical Accuracy: It teaches the model the right medical terminology, how diseases are related, and standard treatment protocols. This drastically cuts down the risk of the AI spitting out incorrect or even harmful information.
- Contextual Understanding: The AI learns the unique language of healthcare. It figures out that a "positive" test result is often bad news, while a "positive" patient outlook is good news—a distinction that’s second nature to us, but not to a machine.
- Safety and Compliance: Fine-tuning helps align the model’s behavior with strict healthcare regulations and ethical guidelines, a non-negotiable part of any successful AI implementation.
Beyond just text, another key technology is the diffusion model. While LLMs are masters of language, diffusion models are artists—they create images. In a medical context, they can generate synthetic medical images like X-rays or MRIs. This is incredibly useful for training other diagnostic AIs without ever touching real patient data, which is a huge win for privacy. They can also clean up or enhance low-quality images, giving radiologists a much clearer picture to work with.
Ensuring Reliability with Advanced Techniques
One of the biggest worries with generative AI is its tendency to "hallucinate"—when the model states something with complete confidence, even though it’s totally wrong. In a clinical setting, that’s a non-starter. To make sure these tools are reliable enough for high-stakes decisions, we use techniques like Retrieval-Augmented Generation (RAG).
RAG works by connecting the AI model to a trusted, up-to-date knowledge base, like a hospital’s internal clinical guidelines or the latest medical journals. When you ask it a question, the model first retrieves relevant information from that trusted source and then uses that data to generate its answer. It effectively grounds its response in verified facts.
This simple but powerful step stops the AI from just making things up. It ensures its outputs are based on the most current and validated information available—a crucial safety net. For instance, a tool like our Clinic AI Assistant relies on these kinds of robust mechanisms to provide dependable support for administrative tasks, making sure the information is both helpful and accurate.
By combining these foundational models with specialized training and verification techniques, generative AI stops being a novelty and starts becoming a powerful, trustworthy partner for medical professionals.
Transforming Patient Care and Clinical Workflows
The real magic happens when generative AI leaves the lab and shows up at the bedside and in the clinic. This is where the technology stops being a fascinating concept and becomes a hands-on tool that tangibly improves patient outcomes and, just as importantly, eases the crushing burden on clinicians.
Let's look past the hype and see how these tools are actually changing the day-to-day grind of medical practice. One of the biggest wins so far has been tackling the mountain of administrative work that, according to studies, eats up more than a third of a clinician's week. By automating these repetitive, draining tasks, AI gives doctors and nurses back their most valuable resource: time to focus on patients.
This is what a more streamlined, AI-assisted workflow looks like in practice. Imagine an interface that instantly summarizes a patient’s entire history, flags key findings in a scan, and drafts clinical notes in real time.
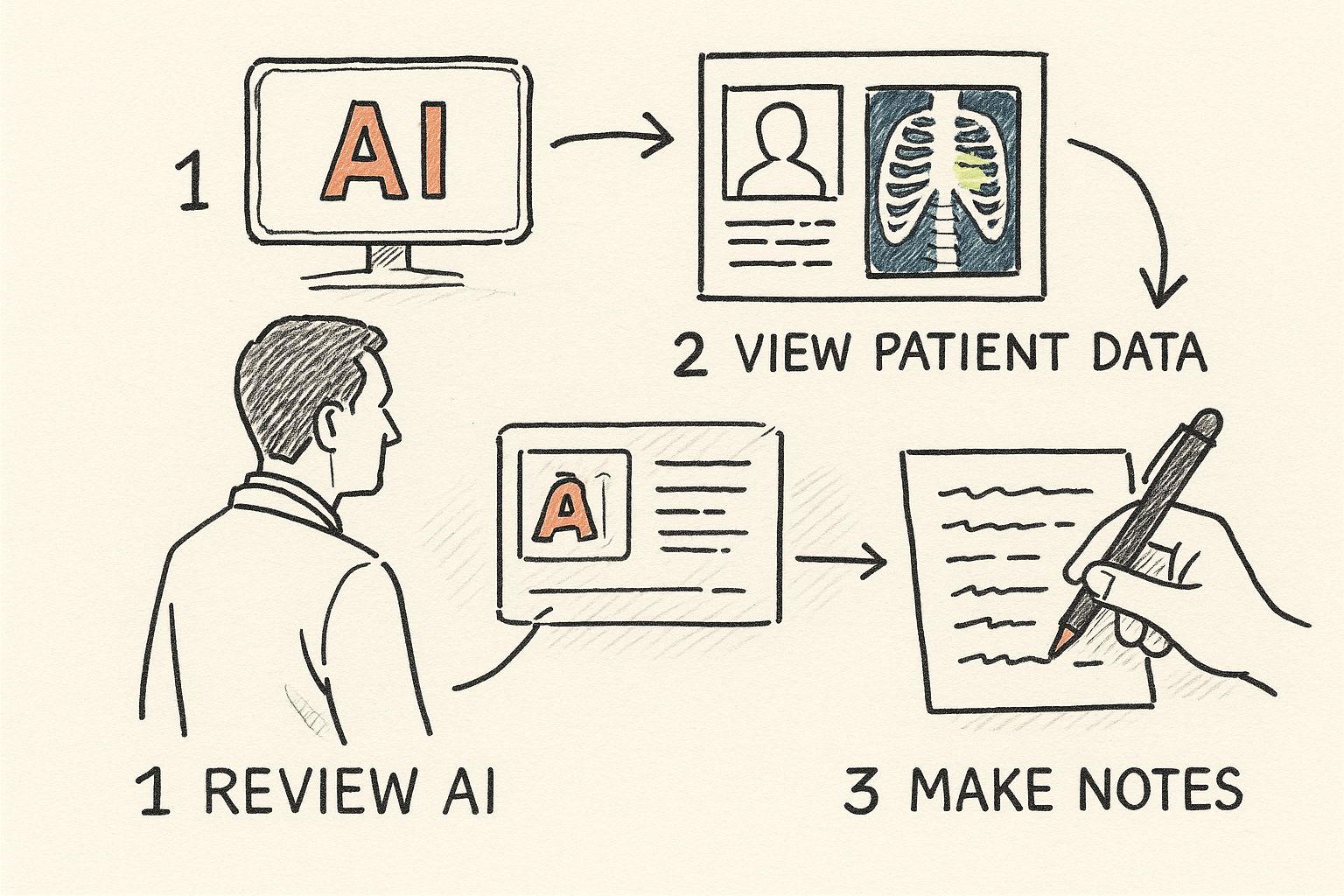
As the infographic shows, it’s about creating a fluid system where critical information is surfaced at the right moment, empowering clinicians to make faster, better-informed decisions without getting bogged down in clicks and keystrokes.
The Rise of the AI-Powered Ambient Scribe
One of the most immediate game-changers is the "ambient scribe." For years, physicians have spent hours after their last appointment hunched over a keyboard, typing detailed notes into Electronic Health Records (EHRs). It's a soul-crushing process and a notorious driver of burnout.
Ambient scribe technology flips the script. It listens securely to the natural conversation between a doctor and patient during an exam. The AI then intelligently filters, transcribes, and structures that dialogue into a clear, medically accurate clinical note. Often, it's ready for the physician's final review in just a few minutes.
This shift is profound. By automating documentation, generative AI gives clinicians back hours in their day, allowing for more meaningful patient interaction and reducing the clerical workload that pulls them away from medicine.
This isn't some far-off dream; it's a practical application of workflow automation that directly solves one of healthcare's biggest headaches. The efficiency boost allows practices to either see more patients or spend more quality time on complex cases.
The table below illustrates just how significant this shift can be across several common clinical tasks.
Clinical Workflow Transformation with Generative AI
Here's a side-by-side look at how traditional clinical processes stack up against their new, AI-enhanced counterparts, highlighting the concrete improvements in both efficiency and patient care.
| Clinical Task | Traditional Method | Generative AI-Enhanced Method | Key Benefit |
|---|---|---|---|
| Clinical Documentation | Manual typing of notes into EHR after patient visits, often hours later. | AI ambient scribe listens to doctor-patient conversations and drafts notes automatically in real-time. | Drastic reduction in administrative time; improved note accuracy and clinician focus on the patient. |
| Medical Imaging Review | Radiologist manually inspects scans, identifies findings, and dictates a report from scratch. | AI pre-analyzes scans, flags potential anomalies, and drafts a preliminary report for the radiologist to review. | Faster diagnostic turnaround and a valuable "second set of eyes" to catch subtle findings. |
| Patient Communication | Staff manually drafts patient education materials or post-visit summaries. | AI generates personalized, easy-to-understand summaries and follow-up instructions based on the clinical note. | Improved patient understanding and adherence to care plans. |
| Treatment Planning | Clinicians manually research latest guidelines and case studies for complex conditions. | AI synthesizes the latest medical literature and patient data to suggest evidence-based treatment options. | Accelerated, data-driven decision-making tailored to the individual patient. |
As you can see, the theme isn't about replacing human expertise but augmenting it. AI handles the rote, time-consuming parts of the job, freeing up medical professionals to apply their critical thinking and empathy where it matters most.
Sharpening the Accuracy of Medical Imaging
Medical imaging is another field where generative AI is making a huge impact. Radiologists face an immense workload, examining hundreds of complex images daily under intense pressure. A tiny detail missed can have life-altering consequences.
Generative AI models, trained on millions of anonymized scans, are becoming powerful assistants. They can help in a few key ways:
- Drafting Preliminary Reports: The AI can analyze an X-ray or CT scan and generate a draft report highlighting potential areas of concern. This lets the radiologist zero in on the most critical findings right away.
- Enhancing Image Quality: For grainy or low-resolution images, certain models can generate a cleaner, higher-quality version, making subtle abnormalities much easier to see.
- Identifying Anomalies: The system can flag unusual patterns that might evade the human eye, acting as a reliable second check to boost diagnostic accuracy.
This partnership between human expertise and AI precision is at the heart of modern healthcare software development. The goal is never to replace the radiologist. It’s to arm them with smarter tools that lead to faster, more reliable diagnoses.
Accelerating Research with Synthetic Data
Medical research and drug discovery are incredibly slow and expensive processes. A major bottleneck is the lack of available patient data, which is rightly locked down by strict privacy rules. Generative AI offers a brilliant workaround: synthetic data generation.
Using real, de-identified patient data as a blueprint, AI models can create entirely new, artificial datasets that perfectly mirror the statistical properties of the original. This synthetic data is a goldmine for researchers because it can be shared and studied freely without ever risking patient privacy.
They can use it to:
- Train other predictive AI models without needing sensitive data.
- Simulate clinical trials to quickly test new treatment ideas.
- Study rare diseases where real-world data is almost impossible to find.
This shows how generative AI in healthcare isn't just about making old processes better; it's about unlocking entirely new avenues for medical science.
Beyond the clinic and the lab, AI is also smoothing out the patient journey from the very first phone call. For instance, smart virtual medical receptionist solutions are already helping practices manage appointments and patient queries far more efficiently. From the front desk to the research bench, these advancements all point toward a smarter, more responsive, and more patient-focused healthcare system.
Boosting Healthcare Operational Efficiency
While the clinical applications of generative AI grab most of the headlines, its impact on the administrative side of healthcare is just as profound. Behind every patient visit is a mountain of operational work. When you can streamline that work, the result is better care, lower costs, and happier staff. The right AI Solutions turn these burdensome processes into genuine sources of efficiency.
This is where generative AI in healthcare shifts from the exam room to the back office. It's all about tackling the repetitive, yet essential, tasks that keep clinics and hospitals afloat. By automating these functions, AI gives skilled staff their time back to focus on more complex, patient-centered priorities.
Automating Medical Coding and Billing
Anyone who has worked in healthcare knows that medical coding and billing are a nightmare of complexity. A single mistake can trigger a denied claim, delayed payment, and a whole chain of administrative headaches. In fact, research shows that clinicians and their teams lose nearly 28 hours each week to this kind of administrative work, which is a massive driver of burnout.
Generative AI provides a pretty elegant solution here. By reading and understanding clinical notes, AI models can suggest the correct medical codes (like ICD-10 and CPT) with incredible accuracy. This doesn't just cut down on human error; it speeds up the entire revenue cycle.
- Fewer Errors: The AI flags inconsistencies and potential problems before a claim is ever sent out.
- Faster Payments: Clean, accurate claims get approved much faster, which is a huge boost for an organization's cash flow.
- Smarter Staffing: Coders are no longer stuck doing manual data entry. Instead, they become reviewers, validating the AI's suggestions and handling a higher volume of claims with better precision.
This is a perfect example of an effective AI Automation as a Service model in action—it transforms a major cost center into a lean, efficient operation.
Optimizing Patient Scheduling and Support
Long waits and clunky appointment systems are a universal patient complaint. Generative AI can power intelligent scheduling tools that optimize the calendar based on urgency, available doctors, and even the predicted length of an appointment. The goal is to minimize both patient wait times and clinician downtime.
By intelligently managing the flow of patients, healthcare organizations can improve satisfaction, reduce front-desk workload, and see more patients without sacrificing the quality of care.
Beyond just scheduling, AI-powered chatbots can handle routine patient questions around the clock. These virtual assistants can answer FAQs about appointments, offer pre-visit instructions, and point patients to the right information. This frees up staff to handle more urgent and complex calls. This is a great application of internal tooling that creates a much smoother experience for patients and staff alike.
Enhancing Prior Authorizations and Administrative Workflows
The prior authorization process is another huge bottleneck. It's a constant source of delays and frustration for providers and patients. AI can attack this problem by automatically filling out forms, checking requests against payer rules, and flagging things that are likely to cause a denial.
This kind of targeted workflow automation can slash the time it takes to get approvals, making sure patients get the care they need without sitting around waiting for paperwork.
From billing and coding to scheduling and authorizations, generative AI is proving its worth by tackling the operational headaches that have bothered healthcare for decades. These aren't just about saving money. They're about building a healthcare system that's more responsive, resilient, and focused on the patient. Crafting a plan around these operational wins is a key part of our AI strategy consulting approach, because it delivers results you can actually see and measure.
Frequently Asked Questions
How does AI improve medical billing accuracy?
Generative AI reads unstructured clinical notes and matches the information to the correct billing codes. It catches key terms, procedures, and diagnoses that a person might overlook, leading to more complete and accurate claims that are far less likely to be denied.
Can AI chatbots handle sensitive patient questions?
AI chatbots are best suited for administrative tasks—things like scheduling, appointment reminders, and answering general questions. For anything involving sensitive medical information, the AI is designed to seamlessly hand the conversation over to a human provider. Patient safety and privacy always come first.
What is the first step to automating operational workflows?
Start by identifying the tasks in your current workflow that are the most repetitive, time-consuming, and prone to errors. A great first step is a focused pilot project, like automating claim submissions for a single department. This helps you show value quickly and makes the case for expanding later. Consulting with our expert team can help you find these high-impact opportunities.
Grappling with the Hurdles and Ethical Dilemmas
For all its promise, bringing generative AI into healthcare isn't a simple plug-and-play operation. It's a path filled with very real challenges and deep ethical questions. We have to be clear-eyed and responsible about this, because getting it wrong could have serious consequences for patients. The only way to build a future where AI in medicine is trustworthy is to face these hurdles head-on.
It's a delicate dance between innovation and patient protection. We absolutely have to nail down our strategy for handling core issues like data privacy, algorithmic bias, and the complex web of regulations.
The Elephant in the Room: Patient Data Privacy
Generative AI models have a massive appetite for data. To get smart enough to be clinically useful, they need to learn from enormous datasets of patient information, which immediately sets off privacy alarm bells. Protecting sensitive health data isn't just a good idea—it's a fundamental requirement.
This goes way beyond standard IT security. We're talking about advanced techniques like data de-identification, which scrubs personal identifiers from records, and federated learning. That's a clever approach where models train on data locally, right inside a hospital's secure network, so the sensitive information never has to leave.
Think of it as "privacy-by-design." Security can't be a bandage you apply at the end. It has to be part of the DNA of any AI system from the very first line of code, a principle we follow in our own AI Product Development Workflow.
Algorithmic Bias and the Fight for Health Equity
One of the most dangerous pitfalls is algorithmic bias. If an AI model is trained on data that carries the baggage of historical biases in healthcare, the AI will learn and even amplify those same prejudices. The result? AI tools that work better for some groups of people than others, making health disparities even worse.
Imagine a diagnostic tool trained mostly on data from a single ethnic group. It might be less accurate for everyone else, leading to missed diagnoses or flawed treatment plans. To prevent this, data scientists have to be deliberate about curating diverse, representative datasets and constantly check their models for any signs of bias. The end game is to build AI tools for business and healthcare that serve every single person fairly.
The 'Black Box' Problem and Why Humans Must Remain in Control
Many of the most powerful AI models are a "black box." In simple terms, even the people who built them can't fully explain the logic behind a specific output. In a high-stakes field like medicine, that lack of transparency is a huge problem. Doctors can't be expected to trust and act on a recommendation if they don't understand the 'why' behind it.
This is exactly why a human-in-the-loop approach is non-negotiable. AI should be the co-pilot, not the pilot. It can sift through mountains of data and flag potential issues, but the final call must always belong to a qualified clinician. They bring the context, experience, and human empathy that no algorithm can replicate, ensuring accountability and keeping the heart of medicine right where it belongs: with people.
Why Healthcare Is Lagging in AI Adoption
It’s no secret that healthcare has been slower on the uptake with AI compared to other industries. A 2024 analysis showed that in healthcare, only about 1 in 1,850 job postings mentioned AI skills. That’s a world away from the tech sector (1 in 71) or even finance (1 in 175). You can dig into the complete findings in this AI adoption analysis.
So what's holding things back? It boils down to a few key issues:
- Fragmented Data: Patient information is scattered across dozens of disconnected systems—EHRs, imaging archives, lab reports. Trying to pull all that messy, siloed data together to train an AI model is a massive technical headache.
- Regulatory Mazes: Healthcare is, for good reason, a tightly regulated field. Getting new technology approved, especially anything that qualifies as a medical device, is a long and expensive journey that requires strict regulatory compliance for medical devices.
- The Human Factor: Bringing AI into a hospital isn't just a software installation. It's a fundamental change to how clinicians work. It requires a major cultural shift and a commitment to helping people and intelligent machines learn to collaborate effectively.
Your Roadmap to Implementing Generative AI
Moving from theory to practice with generative AI in healthcare requires a clear, deliberate plan. The potential is massive, but actually getting it to work in a real-world clinical setting depends on a smart strategy—one that balances exciting innovation with the practical demands of patient care. This roadmap lays out a practical framework for healthcare leaders ready to make it happen.
The secret? Start small and prove the value quickly. Forget about a massive, organization-wide overhaul. A "start small, scale smart" approach that delivers tangible results is far more effective. This builds momentum and, just as importantly, gets buy-in from clinicians and other key stakeholders.
Step 1: Identify High-Impact Use Cases
The first step has nothing to do with technology. It’s all about the problem you’re trying to solve. Start by identifying the most significant pain points in your daily workflows, both on the clinical and operational sides. Are your doctors drowning in paperwork? Is patient scheduling a constant bottleneck? Are claim denials eating into your revenue?
Focus on areas where AI can deliver a clear, measurable win. Good candidates for those first projects usually involve things like:
- Automating repetitive administrative tasks that nobody wants to do.
- Making documentation faster and more accurate.
- Improving how you communicate with and support patients.
Nailing down these high-impact opportunities is the bedrock of a successful AI journey. If you need some inspiration, looking at real-world use cases is a great place to start.
Step 2: Launch a Focused Pilot Project
Once you’ve picked a use case, launch a tightly focused pilot project. The goal here is simple: prove the concept and show real value without turning the entire organization upside down. This lets you test the tech in a controlled environment, get honest feedback from your staff, and build a rock-solid business case for expanding later.
A successful pilot project is your internal proof point. It shows skeptical stakeholders that the technology works, delivers real benefits, and can be safely woven into existing workflows. This is what paves the way for future investment.
Defining clear success metrics is absolutely critical during this phase. Whether your goal is to reduce documentation time by 20% or slash claim denial rates, you need measurable targets. This stage is a key part of any well-designed AI Product Development Workflow.
Step 3: Assess Your Data and Assemble Your Team
With a successful pilot in the bag, it's time to get ready to scale. This means tackling two crucial things at once: evaluating your data infrastructure and building the right team. Generative AI is only as good as the data it learns from, so making sure you have clean, accessible, and secure data is non-negotiable.
At the same time, you need to pull together a cross-functional team. This can't be just an IT project. You need clinical champions who believe in the vision, operational leaders who understand the workflows, and of course, data experts. The market for AI in healthcare has exploded from $1.1 billion in 2016 to $22.4 billion in 2023, and it's projected to hit a staggering $188 billion by 2030. This growth underscores the urgent need for skilled teams to manage this expansion. You can discover more AI healthcare statistics to get a feel for the market's incredible pace.
Step 4: Develop a Change Management Plan
The technology is only half the battle. The other half is the people. A thoughtful change management plan is essential to get your clinical staff on board. This means clearly communicating the "why" behind the new tools, providing excellent training, and creating feedback channels so your team feels heard and valued.
The future of medicine will be built on the synergy between human expertise and intelligent technology. For organizations ready to build that future, a solid plan is the first step. A Custom AI Strategy report can offer the tailored guidance needed for this journey, a path our expert team is ready to help you navigate.
Answering Your Questions About Generative AI in Healthcare
As with any major new technology in medicine, there are always tough questions that need answers. Let's tackle some of the most common ones we hear from healthcare leaders who are looking at bringing generative AI into their organizations.
How Can We Protect Patient Privacy With Generative AI?
This is, without a doubt, the most critical question. Protecting patient data isn't just a goal; it's a non-negotiable requirement.
The good news is that we have proven methods to do this. Techniques like data de-identification strip out personal details before any analysis happens. Even better is an approach called federated learning, which is a game-changer for privacy. It allows the AI model to train on data right where it lives—inside the hospital's secure network—without that sensitive information ever being moved or exposed.
Ultimately, any AI system used in healthcare must be built from the ground up with privacy at its core and be fully compliant with regulations like HIPAA.
What's the Single Biggest Hurdle to AI Adoption in Hospitals?
It really comes down to two things that are deeply intertwined: data and people.
First, the data itself is a huge challenge. Most hospital data is locked away in various electronic health record (EHR) systems and other legacy software. These systems don't talk to each other, making it incredibly difficult to get the clean, consolidated data needed to train a reliable AI model.
Second, you have the human element. For AI to succeed, you need buy-in from the clinicians who will use it every day. Doctors and nurses are rightfully skeptical of new tools. They need to trust that the AI is accurate and that it will genuinely help them, not just add another layer of complexity to their already demanding jobs. As we explored in our AI adoption guide, building this trust takes a careful, phased approach.
Is Generative AI Going to Replace Doctors and Nurses?
Let's be clear: absolutely not. The goal of generative AI isn't to replace healthcare professionals, but to empower them.
Think of it as the ultimate assistant. It’s here to take over the tedious, repetitive work—like clinical documentation, summarizing patient histories, or drafting insurance appeals. By automating these tasks, we free up doctors, nurses, and other staff to focus on what they do best: providing hands-on patient care, making complex clinical judgments, and offering the uniquely human empathy that no algorithm can ever replicate.
Ready to build your AI roadmap? Ekipa AI can help. Our platform delivers a tailored strategy in 24 hours, turning your AI ambitions into scalable impact. Learn more from our expert team.
Transform your healthcare operations with Ekipa AI. Get your Custom AI Strategy report today.