AI-Assisted Clinical Prioritization: Boost Outcomes and Efficiency
Explore how AI-assisted clinical prioritization improves patient outcomes and efficiency with real-world cases and actionable strategies.
At its core, AI-assisted clinical prioritization is about using smart technology to give clinicians a powerful heads-up. The system sifts through enormous amounts of patient data—vitals, lab results, medical history, even doctors' notes—to find the subtle patterns that signal a patient might be heading for trouble. It’s a way to spot the highest-risk individuals early, ensuring they get the attention they need, right when they need it.
Why AI Prioritization Is So Critical Right Now
Let's be honest: healthcare systems are stretched to their limits. Clinicians are juggling heavy patient loads and mountains of administrative work, leaving them with less time to make critical, high-stakes decisions. In this high-pressure environment, AI-assisted clinical prioritization isn't about replacing a doctor's judgment; it's about amplifying it.

Think of it as an intelligent co-pilot for your clinical team. It works tirelessly in the background, scanning all incoming patient data for early warning signs—the kind of faint signals that a busy human might miss. This directly tackles some of the biggest problems in care delivery, from diagnostic delays to inefficient use of hospital resources. As the entire ecosystem of technology solutions for healthcare advances, tools like these are becoming less of a luxury and more of a necessity.
Solving the Toughest Challenges in Patient Care
The real value here is the shift from being reactive to proactive. Instead of waiting for a patient to crash, AI helps teams intervene before it happens. This fundamental change is key to better outcomes and smarter resource management.
Take a look at how this technology directly addresses common pain points in any healthcare facility. The table below breaks down the problems, the AI-powered solution, and the tangible business value you can expect.
Problems Solved by AI-Assisted Clinical Prioritization
| Clinical Challenge | AI-Assisted Solution | Key Business Value |
|---|---|---|
| Diagnostic Delays & Missed Signals | The AI model continuously analyzes patient data, flagging subtle signs of deterioration hours before they become clinically obvious (e.g., for sepsis or acute respiratory distress). | Improved patient outcomes, reduced mortality rates for critical conditions, and lower costs associated with emergency interventions. |
| Inefficient Resource Allocation | The system provides a real-time risk score, helping staff direct limited resources—like ICU beds or specialist consults—to the most urgent cases first. | Optimized bed management, reduced patient wait times, and more efficient use of high-cost clinical assets. |
| High Clinician Burnout | By automating the manual review of thousands of data points, AI reduces the cognitive burden on clinicians, freeing them to focus on hands-on care and complex decision-making. | Increased staff satisfaction and retention, reduced administrative overhead, and improved focus on high-value clinical tasks. |
This isn't just theory; it's driving real business success. Healthcare AI companies are hitting $100M to $200M ARR in under five years—a pace that took traditional health software a decade to achieve.
We're seeing a fundamental change in how care is managed, and the right partner can make all the difference. At Ekipa, we design AI solutions that give decision-makers a clear, practical path forward, from initial strategy to full-scale implementation. Our work in Healthcare AI Services is built to help organizations navigate this shift and unlock real, measurable value.
How AI Actually Helps Doctors Make Better Decisions
At its heart, AI-assisted clinical prioritization is a powerful data interpreter. It goes far beyond just gathering information. Instead, it weaves together scattered data points from electronic health records (EHRs), lab results, and real-time monitoring to create one clear, actionable signal for the care team. This isn't about replacing clinical judgment—it’s about enhancing it with insights that would be impossible for a human to spot alone.
Imagine the AI as an extra set of eyes that never gets tired. It’s constantly scanning for subtle changes and complex patterns that can easily get missed during a chaotic 12-hour shift. This is what allows hospitals to shift from simply reacting to emergencies to proactively preventing them.
From Data Overload to a Clear Warning Signal
It all starts with feeding the system massive amounts of data. An AI model, trained on millions of anonymized patient records, learns to connect specific combinations of symptoms, lab values, and vital signs with certain health outcomes. This training allows it to generate risk scores and predictive alerts with impressive accuracy.
These algorithms are game-changers when every second counts. For instance, by picking up on the earliest, faintest signs of organ dysfunction, an AI system can predict sepsis hours before a patient shows obvious symptoms. That early warning gives clinicians a critical window to intervene, which can make all the difference for the patient. Getting this right requires deep expertise, which is where specialized Healthcare AI Services are so crucial for a safe and successful rollout.
The real magic of AI in a clinical setting is its ability to turn a firehose of data into a clear, prioritized to-do list. It answers the simple but vital question, "Which patient needs me most right now?" and then shows you the data to prove it.
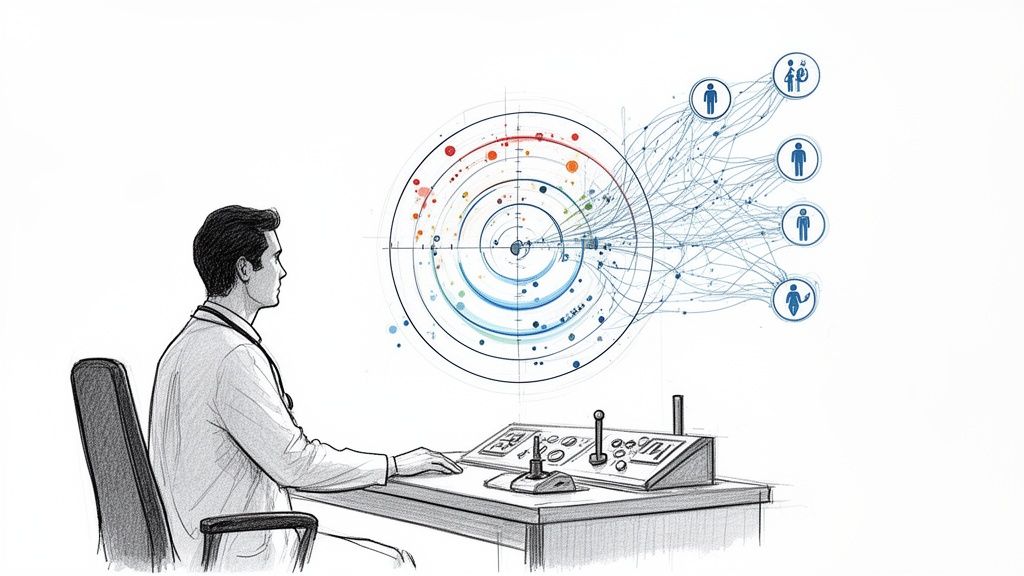
Keeping the Clinician in Control
A common fear is that AI will start making decisions on its own. In reality, the best and most trusted approach is the "clinician-in-the-loop" model. Here, the AI acts as a co-pilot, not the pilot. It flags a high-risk patient or a worrying trend, but the final call always rests with the human expert.
This partnership is essential for building trust and meeting regulatory standards. It plays to the strengths of both sides: the incredible pattern-recognition power of AI and the nuanced, contextual understanding that only a seasoned clinician can provide. This collaborative approach is fundamental to responsible AI implementation and a core tenet of our AI solutions. The goal is always to empower, not replace.
How This Looks in a Real-World Hospital
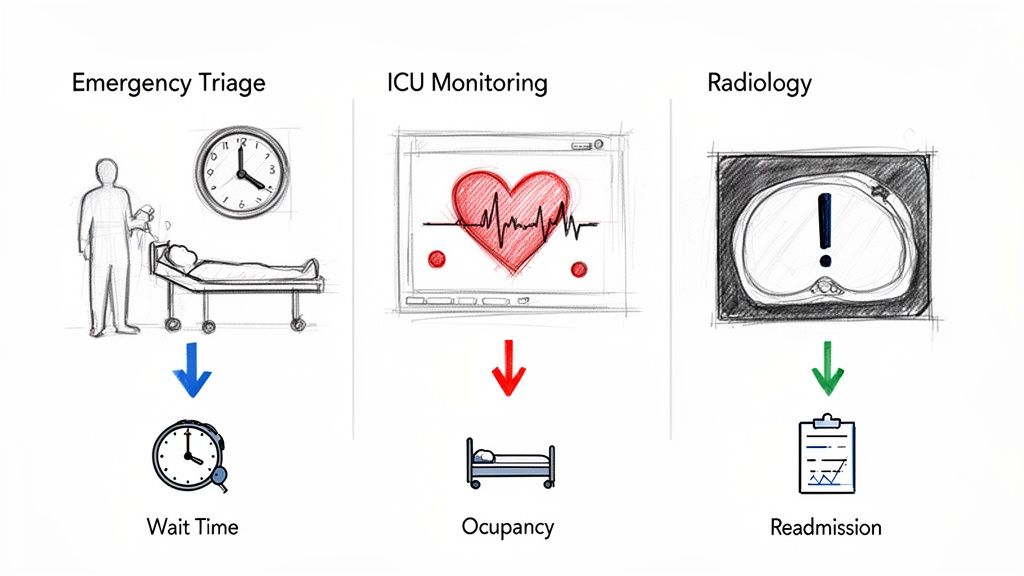
AI-assisted clinical prioritization isn't some far-off concept; it’s already delivering real value across different departments. Here are a few concrete examples:
Smarter ER Triage: In the emergency department, AI models can instantly analyze a new patient's data to flag those at high risk for a stroke or heart attack, making sure they get seen immediately.
Finding the Needle in the Haystack for Radiology: An AI can scan a radiologist's queue of thousands of images, instantly flagging scans with critical findings—like a brain bleed or pulmonary embolism—and bumping them to the top of the list.
Spotting Trouble on the Ward: For patients on general hospital floors, AI can predict when someone is starting to decline. This allows a team to intervene long before a "code blue" is called, often preventing an ICU transfer.
Reducing Readmissions: Before a patient is discharged, AI can analyze their entire record to score their risk of being readmitted within 30 days. This flags them for extra follow-up care to ensure they stay healthy at home.
Diagnostic errors are a major problem, showing up in about 20–25% of patient records. AI offers a powerful way to support clinicians and reduce these errors at the point of care. As researchers point out, these models can help surface medically relevant data that might otherwise be overlooked due to human bias, though work remains to ensure these tools are fair and trustworthy for everyone. You can learn more about these developments in the latest 2026 healthcare technology trends.
These aren't just theories—they are practical, real-world applications making a difference today. Our expert team has deep experience helping healthcare organizations identify and implement these high-impact use cases.
Building Your Implementation Roadmap
Taking a promising concept like AI-assisted prioritization and making it a functional reality in your hospital requires a clear, strategic plan. For any healthcare organization ready to get serious about this, a structured roadmap isn't just helpful—it's essential for success. This plan is your guide through each phase, ensuring the technology actually works and, just as importantly, is embraced by the clinicians who will use it every single day.
The journey begins by zeroing in on a specific, high-impact clinical problem. Forget trying to overhaul the entire organization at once. Successful implementations almost always start with a focused use case, like cutting down diagnostic delays in the emergency department or getting ahead of patient deterioration in the ICU. Starting small lets you score early wins, which are absolutely crucial for building confidence and momentum with stakeholders.
From there, you need to conduct a thorough analysis of your AI requirements. This means taking a hard look at your data readiness, figuring out the technical infrastructure you'll need, and defining what success actually looks like in measurable terms. To pull this off, a well-defined AI adoption playbook can be a game-changer, giving you a proven framework to navigate these early stages.
At its core, the workflow for an AI decision support tool is pretty straightforward: it pulls in data from sources like EHRs, runs it through an AI model for analysis, and then pushes a clear, simple alert to the clinical team.
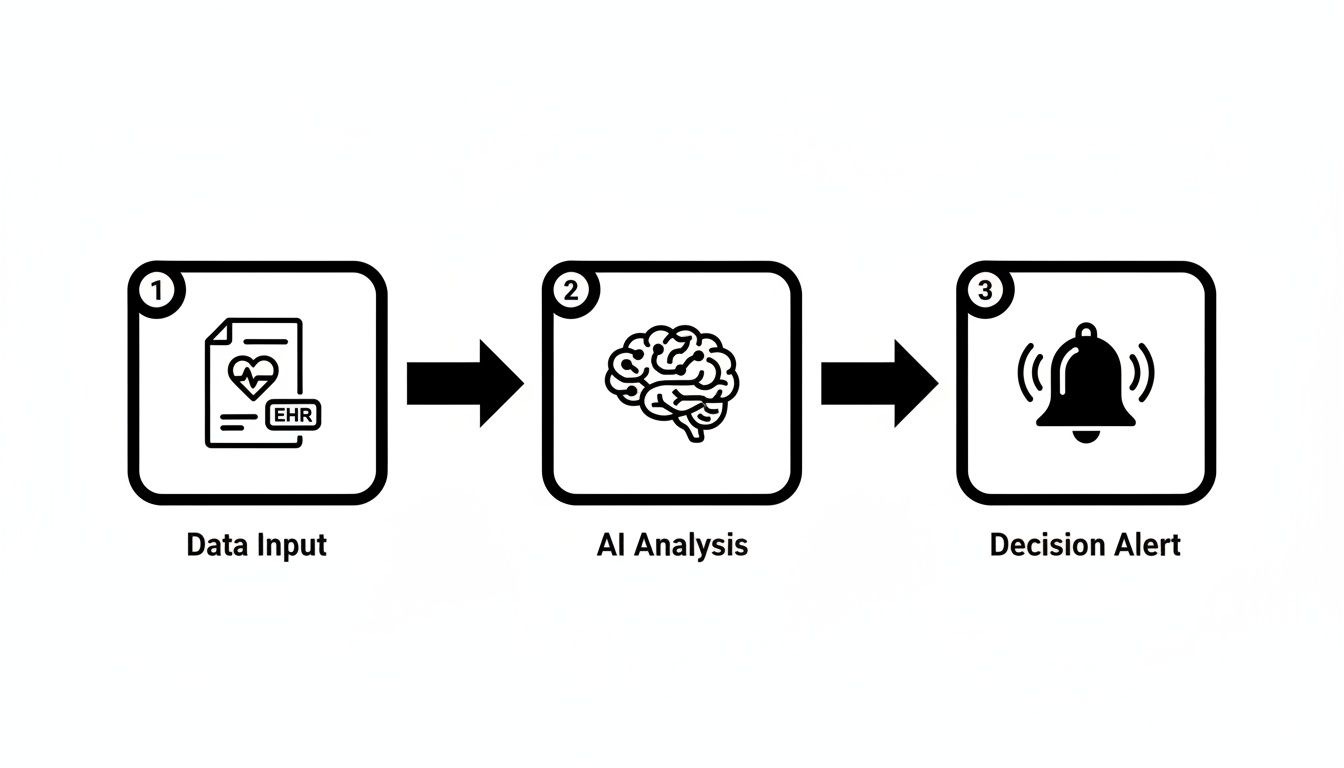
This process turns a flood of raw data into a single, actionable insight. It’s what allows clinicians to shift from being reactive to proactive, intervening before a situation becomes critical. The beauty is in its simplicity—transforming complex data streams into a signal that anyone on the care team can understand and act on.
Defining Your Pilot Program
Once you've chosen a use case and confirmed your data is ready, the next step is a carefully designed pilot program. This is where the rubber meets the road—testing the AI model in a controlled, real-world setting. The goal here is to validate its accuracy, measure its real impact on clinical workflows, and get direct, unfiltered feedback from the people who will be using it.
A successful pilot program always includes these key steps:
Establish a Baseline: Before you flip the switch, you have to know where you're starting from. Collect data on your current performance, whether that's average triage times, sepsis mortality rates, or readmission figures. This baseline is non-negotiable for proving the AI's value later on.
Train the Clinical Team: Great technology is useless if nobody trusts it or knows how to use it. Proper training is critical. Clinicians need to understand what the tool does, how it arrives at its recommendations, and how it fits into their day-to-day responsibilities. This is how you build trust and head off resistance.
Run in a "Silent" Mode: A smart first move is to run the AI in the background, without its alerts actually going live to clinicians. This lets you compare the AI's predictions against actual patient outcomes, giving you a chance to fine-tune the model without disrupting care.
Gather Continuous Feedback: Set up a formal feedback loop. Give users an easy way to report issues, suggest improvements, and even share success stories. This user-first approach is what ensures the final tool is genuinely practical and effective.
Following a proven implementation support plan provides a structured way to move from pilot to full-scale deployment, making sure each stage builds on the success of the last.
Integrating AI Without Creating Friction
One of the biggest hurdles to adoption is plopping a new tool into a busy clinical environment that disrupts workflows or adds to clinician burnout. A truly successful implementation should feel like a natural extension of a clinician's existing process, not just another screen to check or another system to log into.
The ultimate goal of integration is invisibility. The AI should deliver the right information to the right person at the right time, directly within the systems they already use, like the EHR.
Getting to that point takes a thoughtful strategy. Instead of building a standalone dashboard that lives outside the main workflow, the AI's alerts and risk scores should be embedded directly into the primary clinical interface. This approach respects the clinician's time and cognitive load, positioning the AI as a helpful assistant rather than another burdensome task.
Comparing AI Implementation Strategies
When it comes to implementation, healthcare organizations have a few different paths they can take, and each one has its pros and cons. The right choice really depends on your internal resources, your timeline, and your long-term strategic goals.
This table breaks down the main options to help you decide which path makes the most sense for your organization.
| Implementation Strategy | Key Advantages | Potential Challenges | Best For |
|---|---|---|---|
| Buy an Off-the-Shelf Solution | Faster deployment, lower upfront development costs, and proven technology from a vendor. | Less customization, potential integration difficulties with legacy systems, and ongoing subscription fees. | Organizations needing a quick, reliable solution for a common clinical problem without extensive in-house AI talent. |
| Build a Custom In-House Model | Fully tailored to your specific patient population and workflows, with complete control over the data and intellectual property. | High development costs, long timeline, requires a dedicated team of data scientists and AI engineers. | Large health systems with mature data infrastructure and the resources to invest in a long-term, bespoke solution. |
| Co-develop with a Partner | A balanced approach combining external expertise with internal knowledge, leading to a customized solution with shared risk. | Requires strong project management and clear communication between teams to align on goals and timelines. | Organizations that want a customized solution but lack the full in-house team to build it from scratch. |
Choosing the right strategy is a critical decision point on your roadmap. Each path can lead to success, but only if it aligns with your organization's unique capabilities and culture.
Ultimately, building a successful implementation roadmap is all about making deliberate, informed choices. By starting small, focusing on seamless integration, and picking the right strategy for your team, you can deploy AI-assisted clinical prioritization in a way that delivers real, lasting value for both your clinicians and your patients.
Real-World Use Cases and Measurable ROI
Let's move from the abstract to the concrete. This is where AI-assisted clinical prioritization stops being a concept and starts proving its worth in the real world. We're not talking about minor tweaks; we're seeing fundamental improvements in how care is delivered, with measurable results happening today in hospitals globally.
To build a powerful business case, you need to see the clear "before and after." Here are a few examples of this technology in action, showing how small clinical shifts translate into major financial and operational wins.
Transforming Emergency Department Triage
The emergency department (ED) is a pressure cooker where every second matters. Our traditional triage methods are good, but they depend on initial impressions and static protocols. Sometimes, this means subtle but critical warning signs get missed in the chaos.
Before AI: A patient comes in with vague symptoms—fatigue, a little shortness of breath. Based on their initial vitals, they're flagged as non-urgent and settle in for a long wait. What no one can see is the early stage of a pulmonary embolism quietly developing.
After AI: The moment that patient's data hits the system, an AI model cross-references it with millions of similar cases. It spots a high-risk pattern and immediately pings the triage nurse with an alert, recommending a D-dimer test and CT scan. The embolism is found hours earlier than it would have been, preventing a potential catastrophe and significantly shortening the patient's hospital stay.
The real magic of AI in the ED is its ability to see what the human eye can't—those faint, interconnected data patterns that point to a high-risk patient. It’s like adding a layer of data-driven vigilance to your front lines.
Enhancing ICU and Inpatient Monitoring
On the general wards and in the ICU, a patient's condition can turn on a dime. AI acts as a constant, digital watchdog, giving clinical teams a crucial head start before a patient begins to decline.
Before AI: A post-op patient’s vitals look fine during hourly checks. But between those rounds, a slight but steady increase in their respiratory rate and a small dip in oxygen saturation go unnoticed. By the time a nurse sees obvious signs of trouble, the patient is already sliding into respiratory failure, triggering an emergency transfer to the ICU.
After AI: The AI system monitors that patient's data stream continuously. It picks up on those subtle negative trends long before they become a full-blown crisis, generating a predictive alert for sepsis or respiratory distress. The team can then step in early with fluids and oxygen, stabilizing the patient and preventing a costly, high-risk ICU admission.
Revolutionizing Radiology Workflows
Radiology departments are drowning in an ever-growing mountain of imaging studies, leading to serious backlogs. AI can help radiologists dig out by automatically flagging the most critical scans for immediate attention.
Before AI: A radiologist plows through a long worklist, "first-in, first-out." Buried in that queue is a CT scan showing a critical intracranial hemorrhage, but it sits unread for hours while more routine studies are cleared.
After AI: An AI triage tool scans every incoming study the second it arrives. It instantly identifies the hemorrhage and rockets that scan to the top of the radiologist’s list with a critical alert. The referring physician knows within minutes instead of hours, completely changing the patient's prognosis. This kind of intelligent sorting has been shown to slash average turnaround times for critical findings from 11.2 days to just 2.7 days.
By focusing on these high-impact areas, health systems can clearly connect the dots between better clinical processes and a solid return on investment. The trick is to pick a use case where the AI directly solves a major pain point, whether that's patient safety, a frustrating operational bottleneck, or a resource drain. You can learn more about getting clinical teams on board with our HCP Engagement Co-Pilot.
Navigating Ethical and Regulatory Hurdles
Bringing AI into a clinical setting is far more than a tech project—it's an ethical one. When we talk about AI-assisted clinical prioritization, we're dealing with systems that directly impact patient care. The responsibility is immense, and navigating the tangle of regulations and moral obligations is non-negotiable. Getting this right isn't just a best practice; it's fundamental to patient safety.
The journey has to start with confronting the hidden biases baked into historical medical data. AI models are only as good as the data they learn from. If that data carries echoes of past inequities—and most of it does—the AI will not only learn those biases but can actually make them worse. The last thing anyone wants is a system that systematically deprioritizes certain groups of people, completely defeating the purpose of improving care.
Addressing Algorithmic Bias and Fairness
To build an AI solution that clinicians and patients can actually trust, you have to be relentless in auditing your datasets. This means actively hunting for biases linked to race, gender, income, or even zip code. This isn't a one-and-done task; it's a constant process of vigilance.
Here are a few key strategies that are essential for promoting fairness:
Diverse Data Sourcing: Go out of your way to pull data from the widest possible range of patient populations. Your model has to reflect the real community it will serve.
Bias Mitigation Techniques: As you build the model, use sophisticated statistical methods to find and correct for biases. The goal is to ensure predictions aren't skewed by demographics.
Continuous Performance Monitoring: Once the system is live, you have to keep a close watch on how it performs across different patient groups. This is the only way to catch and fix new disparities as they pop up. We build these fairness checks into our AI requirements analysis from day one.
Ensuring Transparency with Explainable AI
A doctor isn't going to trust a risk score that appears out of thin air. For an AI recommendation to be useful, the clinician needs to understand why the model made it. This is exactly why Explainable AI (XAI) is so important. A "black box" model is a non-starter in a clinical environment.
Explainable AI turns a mysterious prediction into a transparent, data-backed suggestion. It allows a clinician to see the specific factors—like a rising lactate level or a subtle change in respiratory rate—that triggered an alert, empowering them to make the final call with confidence.
XAI isn't just about building trust; it's about accountability. When a decision is influenced by AI, the care team must be able to trace the logic. This kind of transparency is a bedrock principle in any responsible AI strategy consulting.
Adhering to Regulatory Frameworks like HIPAA
Compliance is simply not optional. Any AI system that touches patient data must be built to meet strict standards like the Health Insurance Portability and Accountability Act (HIPAA). This means rock-solid data security, protecting patient privacy, and ensuring data is used correctly.
Beyond the letter of the law, creating a dedicated AI ethics committee or governance board is one of the smartest moves an organization can make. This group should bring together clinicians, data scientists, ethicists, and even patient advocates to provide oversight for all internal tooling and patient-facing applications.
Their job is to vet AI projects, establish clear ethical guardrails, and make sure every system aligns with the organization's core commitment to patient well-being and equity. With that kind of structured oversight, you can be confident that your approach to AI-assisted clinical prioritization is effective, ethical, and compliant from the very beginning.
Finding the Right Partner for Your AI Journey
Bringing AI-assisted clinical prioritization into your healthcare system isn't just a far-off idea anymore—it's a critical step for staying ahead. We've walked through how this technology can give clinicians a much-needed edge, lead to better patient outcomes, and make the whole operation run smoother. But let's be realistic: the road from a good idea to a successful, working system is rarely a straight line.
It takes more than just cool technology. It requires a clear vision and a solid, practical strategy. To get this right, you need a partner who gets it—someone who understands the realities of the clinic floor just as well as the technical details under the hood. As we explored in our AI adoption guide, having a smart plan from the very beginning is the only way to see a real return on your investment.
From a Smart Strategy to Real-World Impact
Trying to tackle this transformation on your own can feel overwhelming. You're dealing with messy data, trying to keep up with regulations, and, most importantly, getting clinicians on board. This is precisely where a strategic partner makes all the difference. We help healthcare organizations get past the "what if" stage and start seeing real results.
Our approach always starts with listening. We dig deep into your specific challenges and what you're hoping to achieve. A cookie-cutter solution just won't cut it in healthcare, so we work with you to build a plan that fits your workflows and clinical priorities. Often, the first step is creating a Custom AI Strategy report that lays out a clear, actionable roadmap.
A successful AI implementation isn't about just plugging in a new tool. It's about fundamentally rethinking how you deliver care to make it safer and more efficient—and that requires a partner who sees the entire picture.
We're Your End-to-End AI Team
From the initial brainstorming sessions during AI strategy consulting to getting a new system up and running across your organization, we’re here to guide you through every phase. Our goal is to make sure your AI initiatives aren't just interesting projects, but that they deliver real, measurable value.
Here's how we can help:
Expert Guidance: Our team is skilled at pinpointing high-impact real-world use cases and helping you build a business case that makes sense.
Seamless Integration: We specialize in AI Automation as a Service designed to fit right into your existing clinical workflows without causing disruption.
Custom Solutions: Whether you need specialized internal tooling or full-scale custom healthcare software development, we have the deep expertise to build it from the ground up.
AI has incredible potential to change clinical care for the better, but unlocking it takes a thoughtful, well-executed plan. Let's start building that plan together.
Get in touch with our expert team today. We can talk through how to turn your vision for AI into a reality that truly helps your clinicians and your patients.
FAQ: Your Questions on AI in Clinical Settings Answered
How does AI-assisted clinical prioritization integrate with existing Electronic Health Record (EHR) systems?
Any good AI solution is built to fit right into your existing world. They typically use secure APIs to pull data from your EHR in real time and then push insights—like alerts and risk scores—back into the clinician's workflow. The whole point is to avoid creating new dashboards or logins. The intelligence should show up right where your team already works.
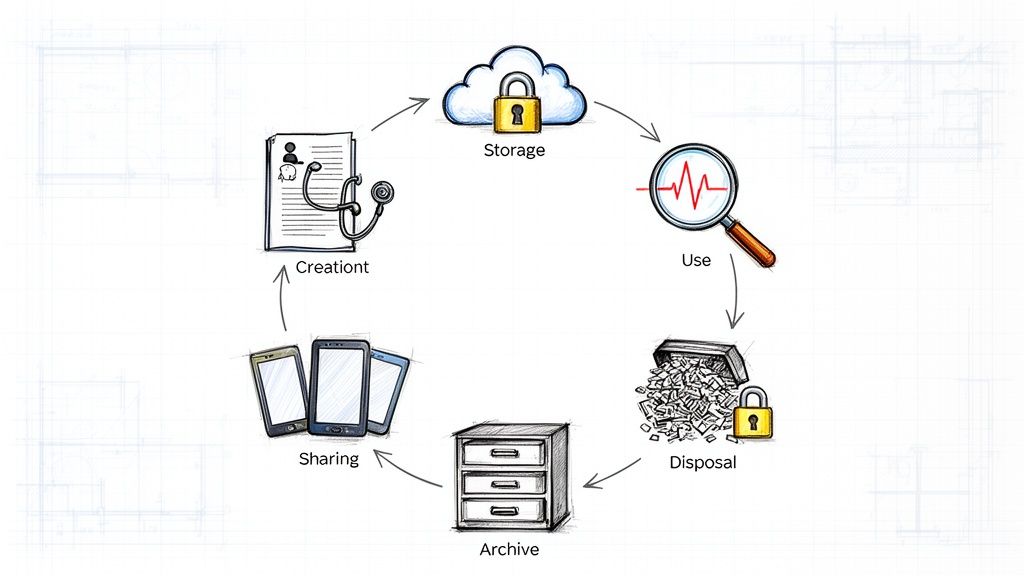
What kind of data is required to train and run these AI models?
These models are trained on massive, anonymized patient datasets that include everything from vital signs and lab results to medication histories and clinical notes. To run in real time, the system needs a live feed of data from your EHR and other clinical sources. The old saying holds true: garbage in, garbage out. High-quality, clean data is absolutely essential for the model to be accurate and reliable.
How do you measure the ROI of an AI prioritization tool?
You measure ROI by looking at a mix of clinical, operational, and financial KPIs. Here’s what that looks like:
Clinical: Are you seeing fewer deaths from conditions like sepsis? Are adverse events and readmission rates going down?
Operational: Are wait times in the ED getting shorter? Is the average length of stay decreasing? Are you making better use of your ICU beds?
Financial: Are you spending less on treating complications? Are you saving money by preventing ICU transfers? Is your hospital able to handle more patients efficiently?
How Is AI Prioritization Really Different From Traditional Triage?
Think of traditional triage as relying on a seasoned clinician's experience and established, static protocols. It's effective, but it can be subjective and vary from person to person. AI-assisted clinical prioritization adds a powerful new layer. It's constantly sifting through a massive stream of real-time patient data—vitals, lab results, medical history, you name it—to generate a completely objective, data-backed risk score. It’s not about replacing that experienced clinician, but about giving them a superpower. The real game-changer is its ability to spot subtle patterns that signal a patient is starting to decline, often hours before a human might notice. This shifts care from reactive to truly proactive. The AI provides the predictive insight, but the clinical expert always makes the final call, a core principle of our AI solutions.
What Are the Biggest Hurdles to Getting This Implemented?
Interestingly, the toughest challenges usually aren't about the technology itself. They're about people, processes, and the data that fuels the system. From what we've seen, the three biggest roadblocks are:
Data Quality and Access: An AI model is only as good as the data it's trained on. If your data is messy, incomplete, or siloed, the AI's predictions will be unreliable. Getting this right is step one.
Integrating into the Workflow: This is crucial. The tool has to feel like a natural part of a clinician's day, not another annoying pop-up or extra step. If it creates alert fatigue or feels clunky, your team just won't use it.
Earning Clinician Trust: You can't just drop a "black box" AI on a clinical team and expect them to trust it. Building that confidence requires transparency about how the model works, solid proof that it's accurate, and reinforcing that the human expert is always in charge. A well-designed AI Product Development Workflow is built to address these human factors from the start.
How Can We Be Sure the AI Model Is Fair and Unbiased?
This is one of the most important questions, and the answer is that ensuring fairness is a continuous commitment, not a one-and-done task. It starts by carefully auditing the training data to root out historical biases tied to race, gender, or other demographics. During the development phase, we use specific techniques to test the model and actively correct for any emerging bias in its predictions. But the work doesn't stop at launch. We have to keep a close eye on the model's performance across all patient groups to make sure no new disparities creep in over time. A best practice is to establish a diverse governance committee to uphold ethical standards—a central part of our Healthcare AI Services.
Ready to build a smarter, more efficient clinical workflow? Ekipa AI provides the strategic guidance and technical expertise to implement AI solutions that deliver real-world results. Explore our AI tools for business and connect with our expert team to see what’s possible.