EHR Optimization Strategy: AI-Driven Workflows to Cut Burnout
Explore an EHR optimization strategy powered by AI-driven workflows to streamline care, reduce clinician burnout, and boost ROI.

An EHR optimization strategy is a game plan, plain and simple. It’s about taking the Electronic Health Record system you already have and making it work for you, not against you. This means going way beyond just storing patient data. We're talking about a deliberate effort to fine-tune clinical workflows, slash the administrative headaches, and ultimately, improve how you care for patients.
It all starts with an honest look at your current state, setting clear goals, and then making smart changes to both technology and processes to get the most out of your EHR investment.
The Urgent Case for EHR Optimization
Let's be blunt. A clunky, slow EHR isn't just an annoyance. It's a direct threat to your organization's bottom line, a massive driver of staff burnout, and a real obstacle to providing top-notch patient care. In today's world of tight margins and even higher expectations, you simply can't afford to let your most important clinical tool underperform.
An EHR optimization strategy isn't about small bug fixes or a simple software update. It's a fundamental rethinking of how your EHR works. The mission is to transform it from a glorified—and often frustrating—data-entry tool into an intelligent partner for your clinical teams. You want an environment that feels intuitive and supportive, not one that gets in the way.
Beyond Convenience: The Tangible Returns
When you get this right, the impact is immediate and you can absolutely measure it. A well-designed strategy hits some of the biggest pain points in healthcare head-on.
Combating Clinician Burnout: By streamlining documentation and putting repetitive tasks on autopilot, optimization gives clinicians back what they need most: time. This directly tackles the crushing administrative burden that we know is a primary cause of burnout.
Slashing Medical Errors: An optimized EHR surfaces the right patient data at the right time, coupled with smart alerts. This is how you prevent medication errors, make sure critical follow-ups don't fall through the cracks, and support better, faster decisions at the point of care.
Elevating the Patient Experience: When your clinicians aren't battling their software, they can focus 100% on the person in front of them. Think about it: faster access to records, smoother check-ins, and better-coordinated care all add up to a much more positive experience for the patient.
And the numbers back this up in a big way. On average, physicians save a staggering 5 hours per week with optimized EHRs. This translates to 86% faster access to patient records and an incredible $5 billion in annual cost savings across the industry.
We've seen clients achieve incredible results firsthand, like 48% fewer medication errors, a 30% drop in readmissions, and 60% higher patient engagement.
A proactive EHR optimization strategy is no longer a “nice to have”—it’s a core requirement for operational excellence. It's what turns a digital record into a strategic asset that actively drives better clinical outcomes and financial health.
Think of this guide as your playbook. We're going to walk you through how to design and execute a complete strategy from the ground up—from rethinking your core workflows all the way to integrating powerful AI solutions that can unlock a whole new level of efficiency. As we go, keep your facility's unique challenges in mind and consider how our specialized Healthcare AI Services could help you drive the most significant value.
Laying the Groundwork for Real-World Success
An EHR optimization strategy that actually works doesn't start with a shopping list of new tech features. It starts with people and process. Before you touch a single setting in the system, you have to get an honest, unvarnished look at how things operate today. This initial groundwork is what separates a successful project from a frustrating waste of resources, ensuring your efforts are aimed at the problems that truly matter to your teams.
The best way to start? Get out of the conference room and onto the floor. Shadow your clinicians, nurses, and front-desk staff. Watch them work. You'll gain an unfiltered view of their daily battles with the EHR. Document every extra click, every clunky workaround, and every sigh of frustration. This isn't about placing blame; it's about collecting raw intelligence on where the system is a roadblock instead of a tool.
Mapping Out the "As-Is"
Once you have those on-the-ground observations, it's time to translate them into detailed workflow maps. These are basically diagrams that trace a patient's entire journey through your organization—from the first scheduling call to the final bill. The goal here is to pinpoint the exact spots where things slow down, information gets dropped, or clinicians are forced into mind-numbing, repetitive data entry.
This mapping process almost always uncovers some surprising inefficiencies. For example, you might find that nurses are spending 15 minutes per patient just manually reconciling medication lists because the EHR doesn't talk to the pharmacy system correctly. Or maybe you'll trace a high rate of billing denials back to one confusing, poorly designed field in the registration screen. These are the gold nuggets—the high-impact problems your optimization strategy needs to fix.
This whole process flow is critical because unoptimized EHRs create a dangerous domino effect, leading to burnout and errors that directly threaten patient safety.
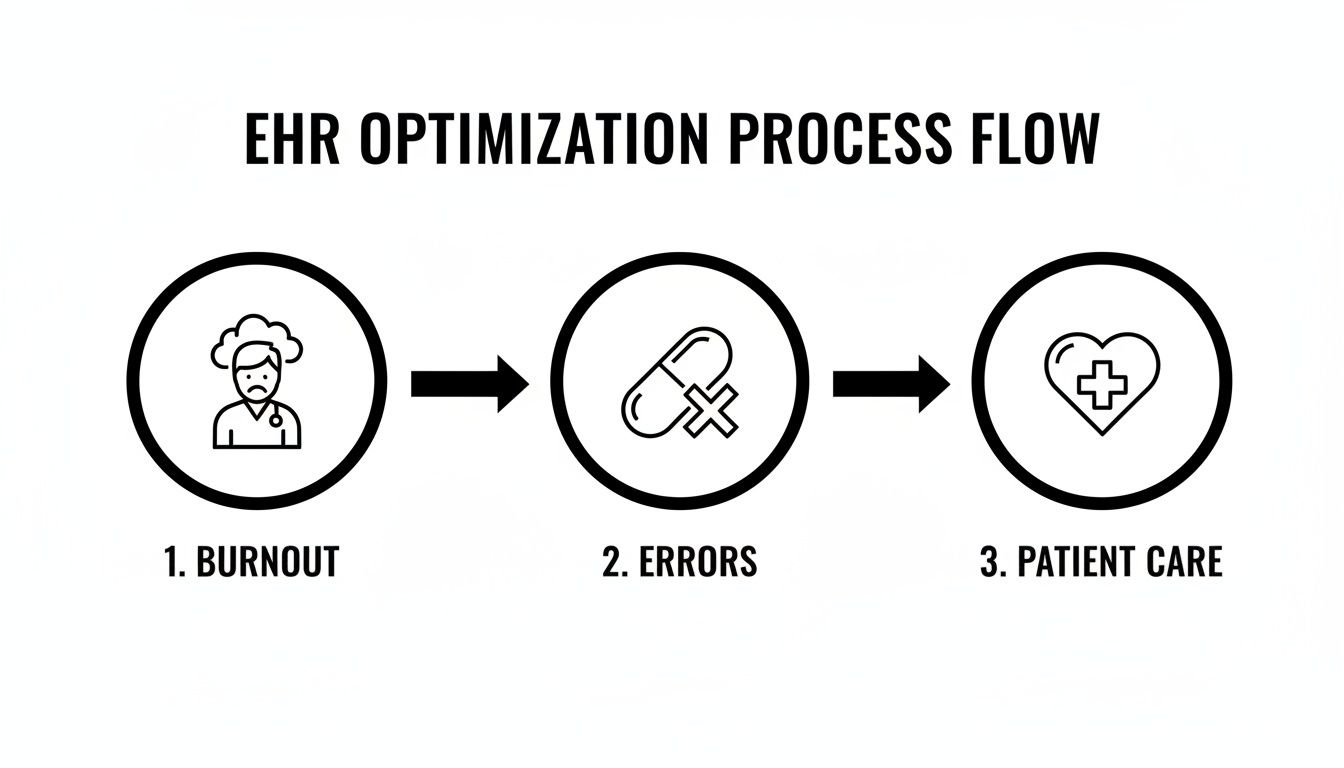
As the visual shows, it's a clear chain reaction: system friction burns out your clinicians, which makes medical errors more likely, ultimately harming patient care.
Setting Goals That Actually Mean Something
With a clear map of your problems, you can finally move from vague complaints like "the EHR is slow" to specific, measurable goals. An objective like "improve efficiency" is useless because you can't measure it. Instead, every goal should be SMART: Specific, Measurable, Achievable, Relevant, and Time-bound.
Here’s what that looks like in practice:
Reduce clinician documentation time: Cut the average time spent writing progress notes by 20% within six months by rolling out specialty-specific templates and voice-to-text dictation.
Improve billing accuracy: Drop the claim denial rate from 8% to 3% in the next quarter by automating charge capture for the top 10 most common procedures.
Enhance patient communication: Boost patient portal message response rates by 50% in 90 days by creating pre-built, standardized replies for common questions.
A huge part of this is remembering the end-user: the patient. Many of the best EHR improvements are tied to better strategies to improve patient experience. When you can directly link a system fix to a higher patient satisfaction score, you build a much stronger case for the project.
Expert Tip: This discovery phase is the perfect time to start thinking about AI. By scoping out high-impact opportunities early—like automating prior authorizations or using predictive analytics to flag at-risk patients—you make sure your technical roadmap is directly aligned with your biggest operational headaches from day one.
By building this solid foundation first, you turn your EHR optimization project from a series of random IT tweaks into a focused, data-driven mission. This initial discovery work is absolutely non-negotiable if you want to see real results and prove the ROI to leadership. Every insight you gather here will shape all the decisions that follow.
Redesigning Workflows for Peak Efficiency
Alright, you’ve done the assessment and set your goals. Now comes the part where the rubber meets the road: redesigning the clinical and administrative workflows that are bogging everyone down. This isn't about minor tweaks. We're talking about a fundamental re-engineering of processes to slash clicks, save precious minutes, and kill off those frustrating manual workarounds for good.
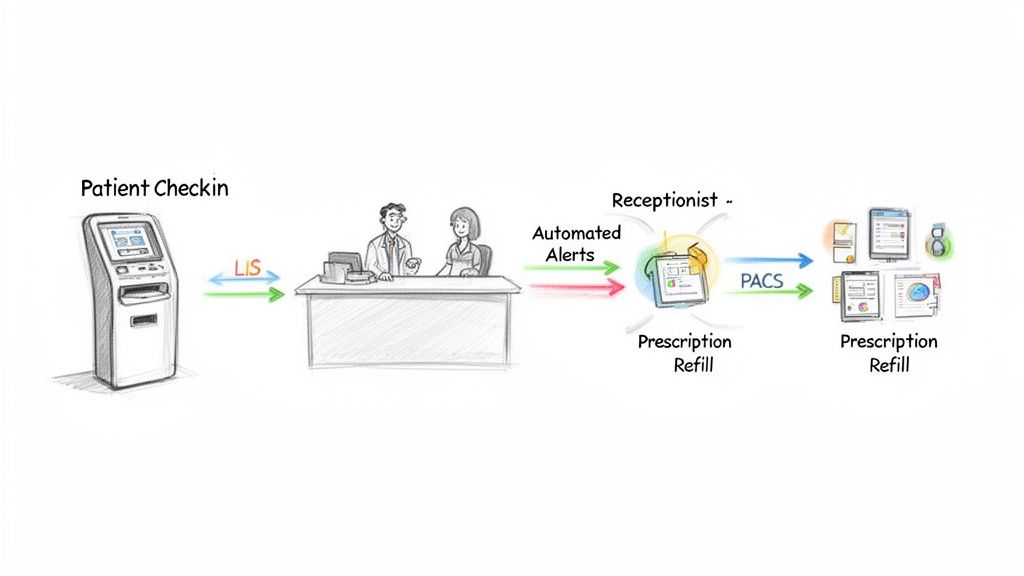
First, pull out those workflow maps you made during the discovery phase. This time, you're not just spotting bottlenecks—you're actively designing solutions for them. A classic example, and often a great place to start, is the patient check-in process. Instead of having your front desk staff manually key in every piece of demographic and insurance info, what if patients handled it themselves? A redesigned flow could use pre-registration forms sent through the patient portal or even self-service kiosks in the waiting area. This one shift can free up staff for more valuable patient interactions, cut down on typos, and shorten wait times.
Prioritizing Data Quality and Interoperability
Here’s the hard truth: a redesigned workflow is only as good as the data running through it. If your EHR data is a mess—inconsistent, incomplete, or stuck in silos—even the most brilliant process will fall flat. This is why data quality and genuine interoperability have to be at the heart of your optimization strategy. Without clean, reliable data, your clinical decision support tools are useless, and your analytics are just noise.
The first step is to establish and enforce strict data governance standards. This means creating clear, standardized protocols for data entry, covering everything from patient demographics to diagnoses. For example, mandate the use of structured data fields for allergies instead of letting clinicians type them into free-text notes. That simple change ensures the information is captured consistently and can trigger critical automated safety alerts.
A huge driver of clinician burnout is bad data. When doctors and nurses have to waste time hunting down missing lab results or second-guessing a patient's medication history, it adds a massive cognitive load and pulls them away from actual patient care.
Scrubbing your existing data is just as crucial. It can feel like a monumental task, but you can get the biggest clinical bang for your buck by focusing on high-impact areas like medication lists and problem lists first. The ultimate goal is to build a single source of truth that your clinicians can trust implicitly.
For a closer look at how to get these processes humming, you can learn more about workflow automation strategies in our detailed guide.
Building Bridges Between Systems
In today's healthcare environment, the EHR can't be an island. To get real efficiency, it has to talk seamlessly with all the other critical systems you rely on. This is where you unlock the most significant gains.
Imagine a world where your EHR can freely and automatically exchange data with:
Laboratory Information Systems (LIS): Lab orders and results flow directly into the patient's chart, eliminating manual entry and getting critical information to clinicians faster.
Picture Archiving and Communication Systems (PACS): Clinicians can pull up X-rays, CTs, and MRIs right from the EHR, giving them the complete clinical picture without having to log in to another system.
Billing and Practice Management Software: Clinical activities automatically generate the correct billing codes, which cleans up the revenue cycle and slashes claim denials.
Sometimes, your EHR vendor’s built-in tools or off-the-shelf solutions just don’t cut it for your specific needs. When you hit that wall, it’s time to think about strategic custom healthcare software development. Building custom APIs and middleware can connect disparate systems, creating the truly integrated information ecosystem you need to operate at peak efficiency. This approach ensures the technology bends to your workflow, not the other way around.
Integrating AI to Supercharge Your EHR
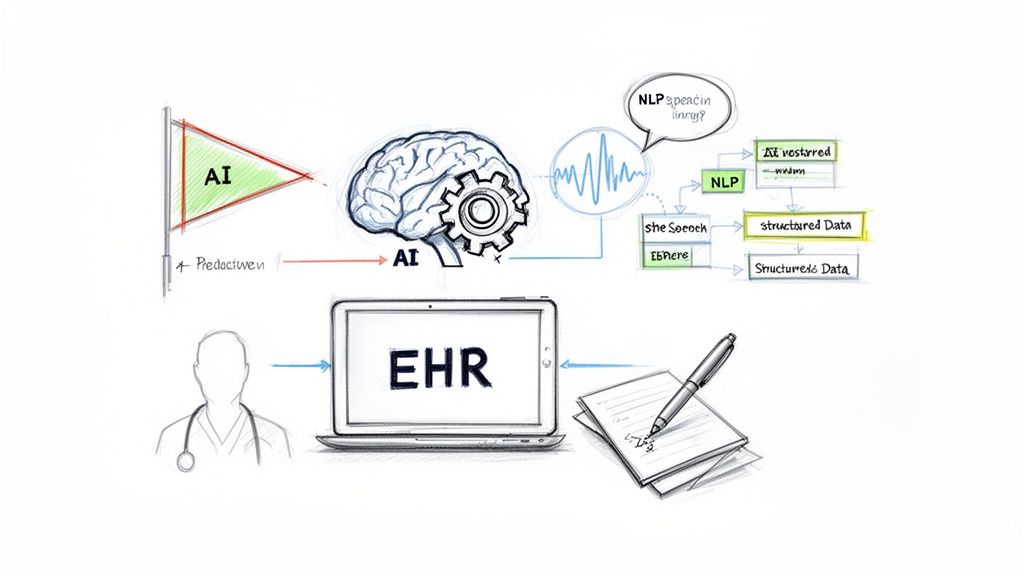
Once you've ironed out your core workflows, it's time for the next big leap in your EHR optimization strategy: infusing it with intelligent automation. This is the point where your EHR stops being just a digital filing cabinet and starts acting like a proactive, smart clinical assistant. By carefully weaving in AI, you can automate the soul-crushing repetitive tasks, uncover insights buried in patient data, and give your clinicians back their most valuable resource—time.
The potential here is huge. Think about natural language processing (NLP). It can sift through all those unstructured clinical notes—the free-form text where the real story often lies—and extract structured, usable data. This means a physician's dictated comments can automatically populate problem lists, medication records, and allergy information, saving hours of tedious manual entry.
Unlocking Predictive Power and Efficiency
Beyond just cleaning up documentation, AI is brilliant at spotting patterns a human simply can't see. Predictive analytics models can chew through thousands of data points in your EHR—from lab results to vitals—and flag patients who are at risk before their condition spirals. This opens the door for early interventions, which can prevent costly hospital readmissions and dramatically improve patient outcomes. In fact, effective big data analytics has been shown to contribute to a 25% reduction in readmissions, a massive win both clinically and financially.
Another game-changer is the rise of AI-powered scribes and ambient listening tools. These technologies run quietly in the background during appointments, automatically creating clinical notes. For any CTO, the business case is compelling: the ambient voice market is projected to hit $1 billion in 2024 and can slash physician documentation time by 20-50%. Even more impressively, it can cut after-hours "pajama time" charting by up to 70%. This is a direct attack on the root causes of clinician burnout.
With the recent 36% surge in healthcare data from diagnostics and genomics, platforms that can adapt and make sense of this flood of information are no longer a luxury—they're essential.
Choosing the Right AI Tools and Strategy
Let’s be clear: integrating AI isn't about just buying a new piece of software and hoping for the best. It demands a deliberate strategy. You need to pick tools that solve the specific, tangible problems you uncovered during your initial workflow analysis.
Here are a few high-impact areas to focus on:
Clinical Documentation: Look for tools that automate note-taking, summarize patient histories, or suggest relevant order sets. An example is an AI-powered assistant that helps draft documentation from a conversation, like what's detailed in a Clinic AI Assistant.
Predictive Analytics: Prioritize models that can identify patients at high risk for conditions like sepsis, readmission, or specific chronic diseases where early intervention matters most.
Administrative Automation: Target the administrative headaches. AI can be a lifesaver for managing prior authorizations, offering coding suggestions, and optimizing patient scheduling through AI Automation as a Service.
To really get ahead of the curve, it's worth exploring more advanced technologies like Large Language Models (LLMs). These are the engines powering the most sophisticated new tools for clinical NLP and summarization.
The real goal of bringing AI into your EHR isn't to replace clinicians—it's to augment them. A smart strategy uses AI to take on the heavy cognitive load of data management, which frees up your providers to focus on what they're truly there for: complex decision-making and caring for patients.
Getting Your Team On Board and Keeping the System Healthy
You can have the most powerful EHR on the planet, but it's just expensive software if your team doesn't actually use it—or use it well. This is where so many optimization projects fall flat. They focus entirely on the tech and forget about the people. To make any change stick, you need two things: widespread user adoption and a smart governance plan.
Getting buy-in from your clinicians and staff isn't about sending a memo. It's about showing them, very clearly, how these changes will make their chaotic workdays a little bit easier. You have to answer the "What's in it for me?" question for every single person, from the front-desk scheduler to the chief of surgery. The goal is to connect every new feature or workflow directly to less administrative headache and more time for patient care.
Training That Actually Works
Forget one-size-fits-all training sessions. They don't work. People tune out information that isn't relevant to their specific job. To get real traction, your training has to be tailored to the daily realities of each role.
For Physicians: They're always short on time. So, show them how the new shortcuts, voice-to-text dictation, and smarter order sets can shave precious minutes off their documentation. The real win for them is getting out the door on time.
For Nurses: Their world revolves around patient safety and seamless team coordination. Focus your training on how improved alerts prevent errors, how better data views help during handoffs, and how communication tools keep everyone on the same page.
For Administrators: They're focused on the bottom line and operational efficiency. Train them on the new dashboards that track key metrics, automated billing functions that slash claim denials, and smarter scheduling tools that optimize patient flow.
A great tactic is to create a network of "super-users" within each department. These are the clinicians who are naturally a bit more tech-savvy and respected by their peers. Empower them to be the go-to resource for quick questions and on-the-floor support. This peer-to-peer help is often more effective than a call to the help desk. If you're struggling to build this kind of program, our expert team has deep experience in creating champions for change.
The Rules of the Road: A Strong Governance Framework
If adoption is about getting people to use the system, governance is about making sure they use it correctly and safely for the long haul. Think of it as the EHR's immune system—it protects the integrity of your data, ensures you're meeting compliance standards, and provides a clear process for making future changes.
A solid governance model needs a few key things:
Data Ownership: Who is ultimately responsible for the quality of lab data? Or scheduling information? You need to assign clear owners.
Access Controls: Implement strict, role-based access. A scheduler shouldn't see clinical notes, and a physician in one department might not need access to another's. This is non-negotiable for protecting patient privacy and staying HIPAA compliant.
Update Protocols: You need a formal process for handling change requests. Without one, you'll have chaos. Create a system to request, test, and roll out any system updates to avoid breaking critical clinical workflows.
This structure creates a predictable and secure environment that everyone can trust. It’s also what allows your EHR to evolve with your organization instead of becoming a rigid, outdated system. While progress has been made, significant gaps remain—behavioral health EHR use is still under 25%, and many rural hospitals are behind. For leaders, closing these gaps is a huge opportunity. A well-tuned EHR can lead to 30% fewer readmissions and a 30% boost in adherence to preventive care. As we explored in our AI adoption guide, getting buy-in at every level is crucial for success.
Measuring Success and Building for the Future
An EHR optimization strategy isn’t a one-and-done project. There's no finish line you cross where the work is suddenly complete. The real magic happens when you treat it as a continuous cycle of improvement, always measuring your impact and building a culture that’s hungry for the next enhancement.
Once you go live with a change, the job simply shifts. You move from implementation mode into a state of constant refinement, making sure your EHR grows right alongside your organization.
From Data to Decisions
Remember those KPIs you set way back in the discovery phase? It's time to bring them back to center stage. They are your compass, giving you the hard evidence of what’s working and, just as importantly, what’s falling flat.
But just pulling raw data isn't enough. The trick is to translate that data into something your teams can actually use. Think role-specific dashboards that clinicians and administrators can understand in a heartbeat. A department head, for example, might get a dashboard showing clinician documentation time, while the revenue cycle manager’s view would be all about claim denial rates and days to payment.
This is how you take the guesswork out of your EHR strategy. When you see a metric like “patient portal response time” start to creep up, you have a clear signal to dig in. Is the interface clunky? Is the workflow inefficient? The data points you in the right direction. For organizations ready to formalize their innovation roadmap, a Custom AI Strategy report can offer a clear path forward.
An EHR that isn’t evolving is already becoming obsolete. The most successful organizations treat their EHR as a living system, continuously fed by user feedback and performance data to guide its growth.
Creating a Powerful Feedback Loop
Data tells you what is happening, but it’s your users—your doctors, nurses, and schedulers—who tell you why. You absolutely need a structured way to capture their feedback to identify the next round of high-impact improvements. This has to be more than just a digital suggestion box nobody checks.
Here’s what works in the real world:
Regular User Groups: Get clinicians from different departments in a room (virtual or physical) every month or quarter. Let them talk openly about their pain points and brainstorm solutions together.
Targeted Surveys: After you launch a new feature, send out a quick, focused survey. Ask directly about its usability and whether it actually made their job easier.
"A/B" Testing Workflows: Before you roll out a major workflow change to everyone, pilot it with a small, willing group. Compare their efficiency metrics against the old way of doing things. The results will speak for themselves.
When you blend the hard numbers with these on-the-ground insights, you turn your team from passive users into active partners in the process. This continuous cycle ensures your EHR delivers more and more value over time, proving the ROI of your initial work and setting you up for whatever comes next. You can dive into some real-world use cases to see what this kind of continuous improvement looks like in practice.
Frequently Asked Questions About EHR Optimization
Let's tackle some of the most common questions that come up when healthcare leaders start thinking seriously about getting more out of their EHR.
Where on Earth Do We Start with EHR Optimization?
I always tell people the same thing: you can't know where you're going if you don't know where you are. The absolute first step is a deep, honest assessment of your current situation.
This means you need to get in the trenches. Map out how your clinicians actually use the system day-to-day, not just how the manual says they should. Sit down with them and listen to their frustrations—what's clunky, what takes too long, what makes them want to throw their computer out the window? This AI requirements analysis pairs that qualitative feedback with hard system data on performance and usage.
Without this baseline, you're just guessing. This discovery work is what lays the foundation for setting goals that will actually make a difference.
How Do We Actually Measure the ROI? Is It Just About Saving Money?
Measuring the return on investment for EHR optimization is a blend of art and science. You have to look at both the hard numbers and the softer, but equally important, benefits.
On the "hard metrics" side, you're looking for things you can count:
Reduced clinician documentation time (every minute saved is a win)
A drop in billing and coding error rates
Lower patient readmission numbers
But don't stop there. The "soft metrics" are where you often see the biggest impact on culture and quality of care. Think improved clinician satisfaction scores—which directly correlates with retention—and higher patient engagement through better portal use. The trick is to connect these improvements back to a financial impact to paint the full ROI picture.
What Are the Biggest Roadblocks We're Likely to Face?
From my experience, the biggest challenges are rarely about the technology itself. They're almost always about people.
The top three hurdles I see over and over are:
Clinician Resistance: People are creatures of habit. Any change, even for the better, can feel like a disruption to a finely tuned (and often stressful) workflow.
Bad Data: Your EHR is only as good as the data inside it. If you're dealing with poor data quality or a system that can't talk to other platforms, you're fighting an uphill battle.
Weak Change Management: You can build the most amazing system, but if you don't properly train people and support them through the transition, adoption will fail. Period.
A smart strategy anticipates these human factors from the very beginning.
How Does AI Fit into All of This?
AI is the game-changer that turns an EHR from a simple digital filing cabinet into a proactive, intelligent partner in care. It’s not about futuristic robots; it's about practical tools that solve real problems.
For instance, you can use predictive analytics to flag patients at high risk for sepsis or readmission, allowing for earlier intervention. Or, you can deploy Natural Language Processing (NLP) to pull structured data automatically from unstructured clinical notes, saving clinicians countless clicks.
Working with an AI strategy consulting partner helps you focus these powerful tools on your biggest operational headaches. It’s how you get a serious boost in efficiency and, more importantly, in the quality of patient care. To dig deeper, you can always connect with our expert team.
Ready to turn your EHR from a source of frustration into a true strategic advantage? Ekipa AI has the experience to help you design and execute an AI-driven optimization plan that lowers costs, fights burnout, and elevates patient outcomes. Start building your AI roadmap today.



