A Guide to Unified Patient Data Platforms in Healthcare
Discover how unified patient data platforms create a 360-degree view of patient care, driving better outcomes with AI and analytics. Your guide to success.

Picture this: a doctor is trying to piece together a critical diagnosis, but all they have are a few scattered pages from a patient's massive medical file. This isn't a hypothetical scenario. It's the reality in healthcare today, where essential information is locked away in dozens of different systems. This is why unified patient data platforms have become less of a technical upgrade and more of a clinical necessity.
The Challenge of Fragmented Patient Data
In medicine, data is everything. It’s the raw material for every diagnosis, treatment plan, and clinical decision. The problem is, for most healthcare organizations, that data is a mess. A single patient's story is often fragmented across a bewildering number of systems that don't talk to each other.
Think about it. The primary care doctor has their Electronic Health Record (EHR). The cardiologist uses a separate charting system. Lab results live in another database, billing codes in yet another, and now we have streams of data coming from patient wearables. Each system holds a critical piece of the puzzle, but getting them to work together is a constant struggle.
This fragmentation creates what we call data silos. It’s like a detective trying to solve a crime with just a handful of disconnected clues—a blurry photo from one source, a partial witness statement from another. Without a way to bring it all together, you can't see the full story. In healthcare, that incomplete picture can have serious consequences.
The Real-World Impact of Data Silos
The problems caused by all this scattered data aren't just IT headaches. They directly impact patient care, safety, and the bottom line. When providers can't see the whole picture, they run into major obstacles:
- Inaccurate Diagnoses: A doctor might prescribe a medication without knowing about a critical allergy documented in a specialist's system.
- Redundant and Costly Tests: Without access to recent lab results from another facility, a physician might order the same expensive test again, wasting money and the patient's time.
- Inefficient Care Coordination: Imagine a care team trying to manage a complex case when everyone is looking at a different, incomplete version of the patient's record. It leads to communication breakdowns and frustrating delays.
- Poor Patient Experience: We've all been there. Patients are forced to be human data carriers, filling out the same forms over and over and repeating their medical history at every single appointment.
As the industry moves toward value-based care—where payment is tied to patient outcomes, not the number of services performed—these data silos become an existential threat. They undermine both patient safety and the financial stability of the entire organization.
A unified patient data platform tackles this problem head-on. It acts as a central nervous system, pulling all those clues from every source and assembling them into a single, reliable patient story. This complete, unified view is the bedrock for any serious effort in advanced analytics and AI, and it's the first step toward unlocking the potential of specialized Healthcare AI Services.
Understanding Unified Patient Data Platforms
So, what exactly is a unified patient data platform? Let's clear up a common misconception right away: this isn't just another piece of software you add to your tech stack. It’s better to think of it as a specialized data refinery, meticulously designed to handle the sheer volume and complexity of healthcare information.
Essentially, it acts as the central nervous system for a modern healthcare organization.
Its primary job is to pull in raw, often messy, and completely disconnected data from dozens of different places. We're talking about everything from EHRs and lab systems to pharmacy records, billing software, and even patient-generated data streaming in from wearables. The platform then gets to work, cleaning, standardizing, and organizing all that disparate information into a single, usable format.
The most crucial function of a unified patient data platform is identity resolution. Using sophisticated algorithms, it meticulously links every single piece of incoming information to the correct individual. This creates a "golden record"—a complete and trustworthy profile that follows the patient across their entire care journey. This is where the magic happens, turning fragmented data points into a high-value, holistic view of a person's health.
The diagram below shows what this looks like in practice, moving from fragmented data silos to a unified, intelligent solution.
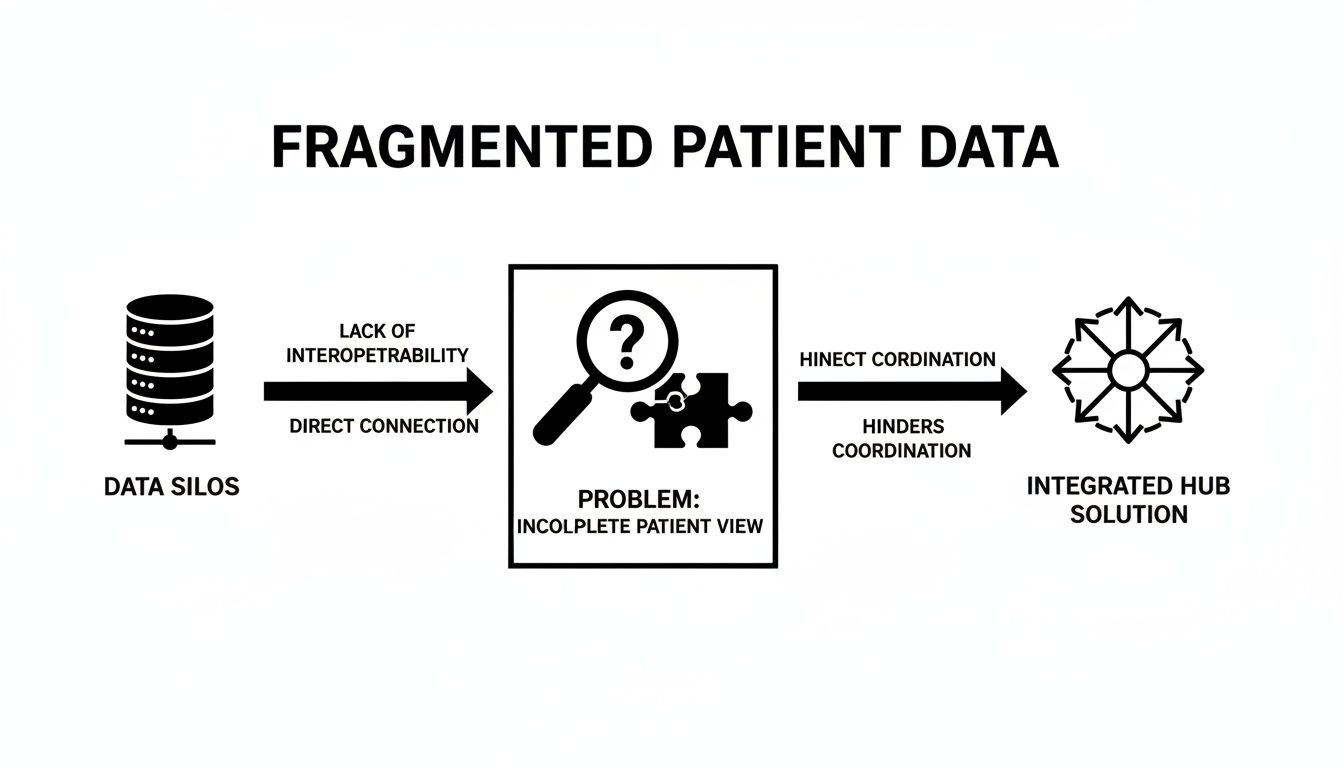
As you can see, isolated systems create a confusing and incomplete picture. A unified platform cuts through that noise, acting as a central hub to bring clarity and deliver actionable intelligence.
Core Components of a Unified Platform
While the technology can vary, these platforms are almost always built around three core components working together to create that single source of truth:
- Secure Data Connectors: These are the digital pipelines that safely pull data from all your sources. They need to be robust enough to handle different formats (like HL7v2 and FHIR) and secure enough to meet strict HIPAA requirements.
- Identity Resolution Engine: This is the brain of the operation. It uses advanced matching logic to analyze names, birthdates, addresses, and other identifiers to ensure that "John Smith" in the hospital's EHR is the same "J. Smith" in the outpatient clinic's system.
- Segmentation and Analytics Tools: Once all the data is unified and clean, these tools allow your team to group patients based on specific criteria—for example, all diabetic patients over 65 with a history of hypertension. This is the foundation for effective population health management and predictive modeling.
How It Differs from a Standard EHR
It's easy to confuse a unified patient data platform with an EHR, but their jobs are fundamentally different.
An Electronic Health Record (EHR) is a system of documentation, built to record clinical encounters within a single healthcare system. In contrast, a unified patient data platform is a system of intelligence, built to aggregate data from many systems to provide a comprehensive view.
An EHR is fantastic at capturing what happens during a specific visit. But a unified platform tells the full story of what happens between those visits and across different providers. It's all about data aggregation and enrichment, turning raw information into actionable insights, often powered by advanced AI solutions that lead to better clinical and operational decisions.
This market is absolutely exploding. The global Customer Data Platform (CDP) market is projected to hit USD 9.72 billion in 2025 and skyrocket to USD 37.11 billion by 2030. With healthcare applications making up nearly 25% of these deployments, these platforms are helping providers build 360-degree patient profiles, slash administrative burdens by up to 40%, and unlock AI-driven predictions. You can learn more about the explosive growth of the CDP market to see just how fast this is moving. For healthcare leaders, understanding this distinction is key to recognizing the technology’s true strategic value.
The Real-World Payoff: Why Unifying Patient Data Matters
We've talked about the technical side of unified data platforms, but let's get to the heart of the matter: what does this actually do for a healthcare organization? When you break down the data silos and bring a patient's entire story into a single, coherent view, the impact is felt everywhere. It’s not just a minor improvement; it’s a fundamental shift that touches clinical care, day-to-day operations, and the financial bottom line.

Better, Safer Clinical Outcomes
The most direct and meaningful benefit lands squarely with patient care. A complete, 360-degree view of a patient’s journey gives clinicians the context they need to make smarter, faster decisions.
Imagine a doctor treating a new patient. Instead of piecing together a medical history from memory or waiting for faxed records, they can instantly see a full list of medications from multiple pharmacies, recent lab results from an outpatient clinic, and a specialist's notes from across town. It’s all right there.
This kind of clarity leads to very real clinical improvements:
- More Accurate Diagnoses: Clinicians can connect the dots between symptoms and test results over time, spotting subtle patterns that would otherwise be missed. This leads to catching conditions earlier and with greater precision.
- Truly Personalized Medicine: With access to everything from genetic markers to lifestyle data from wearables, care teams can finally move beyond one-size-fits-all protocols and design treatment plans that fit the individual.
- Proactive Care, Not Reactive Treatment: A unified system can automatically flag at-risk patients. For instance, it could alert a care manager when a diabetic patient has missed several prescription refills, allowing for an intervention before a small problem becomes a full-blown health crisis.
Smoother, More Efficient Operations
Fragmented data doesn't just put patients at risk; it’s a massive drain on your staff. Clinicians and administrators burn precious hours chasing down records, manually re-entering data, and wrestling with disconnected systems. A unified platform eliminates that friction by automating data aggregation, giving that time back to the people who need it most.
Think about the emergency room. When a new patient arrives, the registration team can pull their complete record in seconds instead of asking a person in distress to fill out pages of paperwork. This simple change makes the entire patient journey smoother and less stressful for everyone involved. Our dedicated Healthcare AI Services are built to find and amplify these kinds of efficiencies.
A Stronger Financial Foundation
The financial upside of unified data is just as compelling. By reducing medical errors and catching unnecessary or redundant procedures, these platforms cut costs directly. How many times has a costly MRI been repeated simply because the radiologist couldn't access one done at another facility last week? A unified view prevents that.
Beyond direct savings, these platforms are the engine for powerful predictive analytics. The market for healthcare customer data platforms is booming—it was projected to hit USD 939.34 million in 2025, a 32.4% jump in a single year, largely because of the drive toward AI. Organizations are now building models to identify patients with a high risk of readmission, deploying targeted interventions that can cut those costly events by 20-30%.
The table below breaks down how these benefits ripple across the entire organization, with supporting data that underscores the tangible value.
Impact of Unified Patient Data Platforms Across Healthcare
| Benefit Area | Specific Outcome | Supporting Data Point |
|---|---|---|
| Clinical | Improved Patient Safety | Unified data helps reduce adverse drug events, a leading cause of hospital-related complications. |
| Clinical | Enhanced Diagnostic Speed & Accuracy | Access to comprehensive patient histories can reduce diagnostic errors by up to 50% in some scenarios. |
| Clinical | Personalized Care Delivery | Enables tailored treatments based on genomics and lifestyle, improving chronic disease management outcomes. |
| Operational | Reduced Administrative Burden | Clinicians can spend up to 45 minutes per day searching for patient information; unified data nearly eliminates this. |
| Operational | Optimized Resource Allocation | Predictive analytics help hospitals better forecast patient flow, improving bed management and staffing. |
| Operational | Streamlined Care Coordination | Seamless data sharing between departments and facilities reduces patient handoff errors and delays. |
| Financial | Lower Readmission Rates | Proactive interventions for at-risk patients can reduce 30-day readmission rates by 20-30%. |
| Financial | Decreased Unnecessary Procedures | Eliminating duplicate tests and scans can save healthcare systems millions annually. |
| Financial | Improved Revenue Cycle Management | Accurate, complete patient data streamlines billing and reduces claim denials. |
As you can see, the benefits are interconnected. Better care leads to fewer costly complications, and more efficient operations free up resources that can be invested back into care delivery.
By lowering readmission rates, optimizing the allocation of expensive resources like ICU beds, and improving the overall patient experience, unified data directly contributes to a stronger, more sustainable financial foundation for the healthcare organization.
Bringing a patient's data together isn't just an IT project. It's one of the most powerful strategic moves a modern healthcare organization can make.
Fueling Next-Generation Healthcare with AI
Clean, structured, and comprehensive data isn't just a nice-to-have organizational asset; it's the high-octane fuel that powers any serious Artificial Intelligence initiative. While the benefits of unified data are huge on their own, its true potential is unlocked when it becomes the foundation for AI. A unified patient data platform is the launchpad for advanced AI applications that were, until now, stuck on the drawing board.
Without a single source of truth, AI algorithms are essentially flying blind. They get fed incomplete or contradictory information, which leads to unreliable and often biased results. But when you train an AI model on a complete, longitudinal patient record, it can start to see patterns and connect dots that are invisible to the human eye. This is the turning point where healthcare shifts from being reactive to truly proactive and predictive.
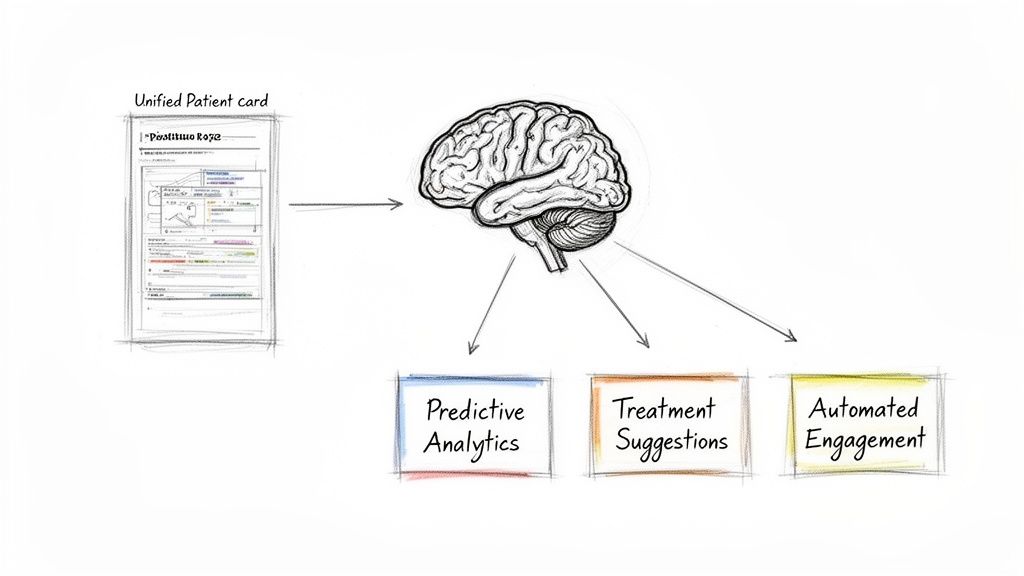
Unlocking Previously Impossible AI Applications
With a steady stream of high-quality data flowing in, healthcare organizations can finally put powerful AI tools to work—tools that have a direct impact on patient outcomes and operational efficiency. The possibilities are massive, stretching far beyond simple analytics and into the realm of intelligent automation and real-time decision support.
These aren't futuristic ideas. They're practical applications being built today on the backbone of unified data:
- Predictive Analytics for Population Health: Imagine AI models sifting through thousands of patient records to flag individuals at high risk for developing chronic conditions like diabetes or heart failure. This lets care teams step in with preventative care before a costly hospitalization is even on the horizon.
- Optimized Treatment Pathways: Machine learning can take a new patient's complete profile and compare it against the outcomes of thousands of similar cases. This helps point to the most effective treatment pathways right from the start, minimizing trial-and-error and boosting the chances of a positive result.
- AI-Driven Patient Engagement: Forget generic appointment reminders. AI can personalize every communication based on a patient's specific condition, history, and even how they prefer to be contacted. This could be anything from sending helpful content about managing a new diagnosis to a gentle nudge to schedule a crucial follow-up.
Empowering Clinicians with Intelligent Internal Tooling
Beyond these large-scale predictive models, unified data is also the key to creating powerful internal tooling that helps clinicians in their day-to-day work. This isn't about replacing doctors; it's about augmenting their expertise with data-driven insights right at the point of care.
For instance, an AI-powered clinical decision support tool built into the EHR can analyze a patient's complete record in real-time. It can flag potential drug interactions that might be missed if medications are prescribed across different, siloed systems. It could also instantly serve up a concise summary of a complex patient history, saving a physician precious time.
The market is clearly taking notice. The healthcare CDP segment is expanding at a 27.2% CAGR, growing from USD 500 million in 2021 to a projected USD 1.6 billion by 2028. And for CTOs planning their AI strategies, 80% of adopters report better predictive capabilities, confirming that data unification is the bedrock of precision care. Discover more insights about these industry statistics at cdp.com.
Data unification isn't an IT project; it is the essential prerequisite for a modern AI strategy in healthcare. Without it, even the most advanced algorithms will fail to deliver meaningful results.
Bridging the Gap Between Data and Action
This is where having a clear plan is absolutely critical. Ekipa AI helps organizations close the gap between having raw data and turning it into tangible action. Our AI strategy consulting is designed to pinpoint the most impactful AI opportunities within your specific operational landscape. We move past the theory to help you build a practical roadmap.
Once those opportunities are clear, our AI Automation as a Service offering helps put those insights into practice. We partner with you to build and deploy the smart, automated workflows that make your unified data a real competitive advantage. Success here relies on a proven AI Product Development Workflow that ensures every project is tied to clear, measurable business outcomes. A great example is our work developing specialized tools like an HCP Engagement Co-pilot to improve interactions through AI.
To see the full range of what's possible, check out our portfolio of AI tools for business and our library of real-world use cases. The journey starts with data, but it ends with intelligent action. Having the right partner to guide you through that process makes all the difference.
How to Choose and Implement the Right Platform
Picking and rolling out a unified patient data platform is a massive undertaking—it’s far more than just another IT project. To get it right, you need a solid strategy that ties the technology directly to your clinical and business goals. This section is your playbook, laying out what to look for in a platform and how to implement it without derailing your operations.
Frankly, getting this right from the start is make-or-break. A well-thought-out plan ensures your investment pays off. Think of it like building a house—you wouldn't start without a blueprint. The same logic applies here.
Key Evaluation Criteria for Platform Selection
Let's be clear: not all unified patient data platforms are built the same. You have to cut through the marketing fluff and focus on the core capabilities that will actually deliver value. Your selection process needs to be tough, with a heavy emphasis on security, interoperability, and the ability to grow with you.
Here are the non-negotiable features you should be digging into with any potential vendor:
- Rock-Solid Security and Compliance: The platform absolutely must be built for HIPAA compliance from the ground up. This means end-to-end data encryption (both when it's moving and when it's stored), tight, role-based access controls, and detailed audit trails. If you're looking at cloud platforms, you need to understand What Is SOC 2 Type 2 and why it's a critical security benchmark for any SaaS vendor you trust with patient data.
- Seamless Interoperability: A platform isn't "unified" if it can't talk to your existing systems. Look for proven connectors for major EHRs and deep support for modern healthcare standards like HL7 and FHIR. This is the only way to ensure data flows cleanly and accurately from one system to another.
- Scalability and Performance: Your data volume is only going to increase. The platform’s architecture must be able to handle millions of patient records and a constant flood of data from sources like wearables and remote monitoring devices without slowing to a crawl.
- Advanced Identity Resolution: This is the heart of the whole operation—creating that single, definitive "golden record" for every patient. You need to grill vendors on their identity resolution engine. Ask them how they handle the messy reality of patient data: name changes, typos, multiple addresses, and incomplete information. If they can't solve this, you'll just end up with a new system full of duplicate records.
To help you stay organized during vendor discussions, here’s a checklist to guide your evaluation process.
Platform Evaluation Checklist
| Evaluation Criteria | Key Questions to Ask | Importance (High/Medium/Low) |
|---|---|---|
| Security & Compliance | Is the platform fully HIPAA compliant? Can you provide your latest SOC 2 Type 2 report? How is data encrypted at rest and in transit? | High |
| Interoperability | Which EHRs do you have pre-built connectors for? Do you fully support both HL7v2 and FHIR APIs? Can we see a demo of the integration workflow? | High |
| Identity Resolution | What matching algorithms do you use (deterministic, probabilistic)? How does your engine handle phonetic misspellings, nicknames, and missing data? | High |
| Scalability | What is the largest patient population you currently support on the platform? How does the system handle sudden spikes in data ingestion? | High |
| Data Governance | How does the platform track data lineage? What tools are available for data quality monitoring and remediation? | Medium |
| Analytics & AI Readiness | Does the platform support real-time analytics? Is the data structured in a way that’s ready for machine learning models? | Medium |
| Vendor Support | What does your implementation support model look like? What are your standard SLAs for critical issues? Can we speak with current clients? | Medium |
| Total Cost of Ownership | What is included in the license fee? Are there extra costs for data ingestion, storage, or additional connectors? | Low |
This checklist isn't exhaustive, but it covers the core areas that will determine whether a platform will be a strategic asset or a technical headache.
A Practical Roadmap for Implementation
A successful implementation is a marathon, not a sprint. Forget the high-risk, "big bang" approach where you try to do everything at once. A phased rollout delivers value at each step, gets your clinical teams on board, and gives you room to make adjustments as you go.
Data Source Discovery and Prioritization: First, map out every single system that holds patient data. Sit down with clinical and administrative leaders to prioritize the most critical sources—this is usually the main EHR, key lab systems, and the billing software.
Define the Unified Data Model: Work with your stakeholders to agree on what the "golden record" for a patient should actually look like. This is where you standardize data fields and create a common language for things like diagnoses and medications across the entire organization.
Phased Integration and Validation: Don't try to connect everything at once. Start with your top one or two priority systems. Pull in the data, let the platform’s identity engine do its work, and then—critically—have your clinical teams validate the unified records for accuracy. This step is essential for building trust.
Launch an Initial Use Case: Instead of trying to boil the ocean, as we explored in our AI adoption guide, pick a single, high-impact problem to solve first. Maybe it's reducing hospital readmissions for a specific patient group or improving care management for diabetics. Get a clear, measurable win under your belt.
Iterate and Expand: Once that first use case proves its value, you can start connecting more data sources and launching new projects. This creates a powerful cycle of continuous improvement and demonstrates ongoing ROI.
Common Pitfalls to Avoid
Even with the best technology, an implementation can go sideways if you're not careful. One of the biggest mistakes is underestimating the sheer messiness of your existing data. Data from legacy systems is often inconsistent and riddled with errors. You have to dedicate real resources to data cleansing; it’s not optional.
Another classic pitfall is failing to get clinical buy-in from day one. If your doctors and nurses don't trust the data or see the platform as just another piece of software to learn, they won't use it. Period.
For organizations with specialized workflows or a patchwork of unique systems, an off-the-shelf platform might not be the answer. In these cases, custom healthcare software development may be required to deliver trustworthy, actionable data to the people on the front lines. And if your team is struggling to make sense of unstructured data like clinical notes or reports, it's worth understanding the benefits of an AI-powered data extraction engine.
Finding the Right Partner for Your Data-Driven Journey
Bringing a unified patient data platform to life is more than just an IT project. It’s a fundamental change in how you deliver care, a strategic move that lays the groundwork for better outcomes, smarter operations, and a real competitive edge. When the stakes are this high, the partner you choose to guide you through this journey makes all the difference.
At Ekipa AI, we specialize in translating complex data strategies into tangible, real-world results. We help you build that solid data foundation and then use it to power intelligent AI solutions that will define the future of your organization. Our approach cuts through the bloat of traditional consulting—we’re lean, fast, and obsessed with delivering real value.
From a Smart Plan to Real-World Impact
We're with you from start to finish, making sure your data unification project delivers measurable returns at every step. Our entire process is built to speed up your progress and take the risk out of your AI investments.
It all starts with our hands-on AI strategy consulting. We roll up our sleeves with you to map out a clear path forward, beginning with a deep-dive AI requirements analysis. The result is a Custom AI Strategy report that connects your tech ambitions directly to your business goals. From there, we help you make it happen, whether that means deploying our AI Automation as a Service or building custom internal tooling that your teams will actually love to use.
A successful data strategy doesn’t end with a clean database. It begins there. The real value is unlocked when that unified data becomes the fuel for intelligent automation and predictive insights that improve patient care.
Our Healthcare AI Services are purpose-built to tackle the industry’s toughest problems. By following a proven AI Product Development Workflow, we make sure every solution we build is ready for real-world impact and widespread adoption.
The future of healthcare is intelligent and interconnected. To see how we can help your organization get there faster, have a chat with our expert team today.
FAQs: Your Unified Patient Data Questions Answered
What is a unified patient data platform?
A unified patient data platform is a system that collects, cleans, and combines patient health information from multiple sources—like different hospitals, labs, and pharmacies—into a single, comprehensive record. This "golden record" provides a complete view of a patient's health journey, enabling better care coordination and advanced analytics.
How is a unified platform different from an Electronic Health Record (EHR)?
An EHR is designed to document clinical encounters within a single healthcare system. In contrast, a unified patient data platform aggregates data from many different systems (including multiple EHRs) to create a holistic, longitudinal view of a patient's health over time and across all points of care.
How do these platforms ensure patient privacy and HIPAA compliance?
Security is paramount. These platforms use multiple layers of protection, including end-to-end data encryption, strict role-based access controls, and detailed audit logs. They are built from the ground up to meet HIPAA requirements and often use data de-identification techniques for analytics to protect patient privacy.
What is the typical ROI for implementing a unified patient data platform?
Return on investment comes from several areas:
- Clinical: Improved patient outcomes and reduced medical errors.
- Operational: Saved staff time from automating data collection.
- Financial: Lower hospital readmission rates and fewer redundant tests. Organizations often see a 20-30% reduction in costs related to managing chronic diseases.
How long does implementation usually take?
The timeline depends on the project's scope. A phased approach is best. An initial project connecting a few key systems to solve a specific problem can take 3-6 months. A full, enterprise-wide implementation connecting dozens of sources typically takes 12-18 months. Working with an expert partner can significantly accelerate this process. For more personalized guidance, contact our expert team.
Ready to turn your data into a strategic asset? Ekipa AI provides the expertise to help you build a solid data foundation and leverage it with intelligent AI solutions. Discover how we can accelerate your transformation at https://www.ekipa.ai.



