AI Automation in Healthcare Operations: Boosting Efficiency and Outcomes
Explore AI automation in healthcare operations and learn how to streamline workflows, cut costs, and improve patient outcomes with practical guidance.

Picture a hospital where the mountain of administrative work just...melts away. Staff are freed up, focusing their full attention on patients. This isn't a futuristic dream; it's the real-world promise of AI automation in healthcare operations, and it’s quickly becoming the new standard. Think of AI as the hospital's digital nervous system—handling the repetitive, data-intensive tasks so your team doesn't have to.
How AI is Redefining Healthcare Operations
Let’s be clear: AI automation in healthcare isn't about replacing talented people. It's about giving them superpowers. It’s a set of smart tools that untangles the complex, non-clinical tasks that eat up precious time and resources. This gives doctors, nurses, and administrators the breathing room to do what they do best: care for people.
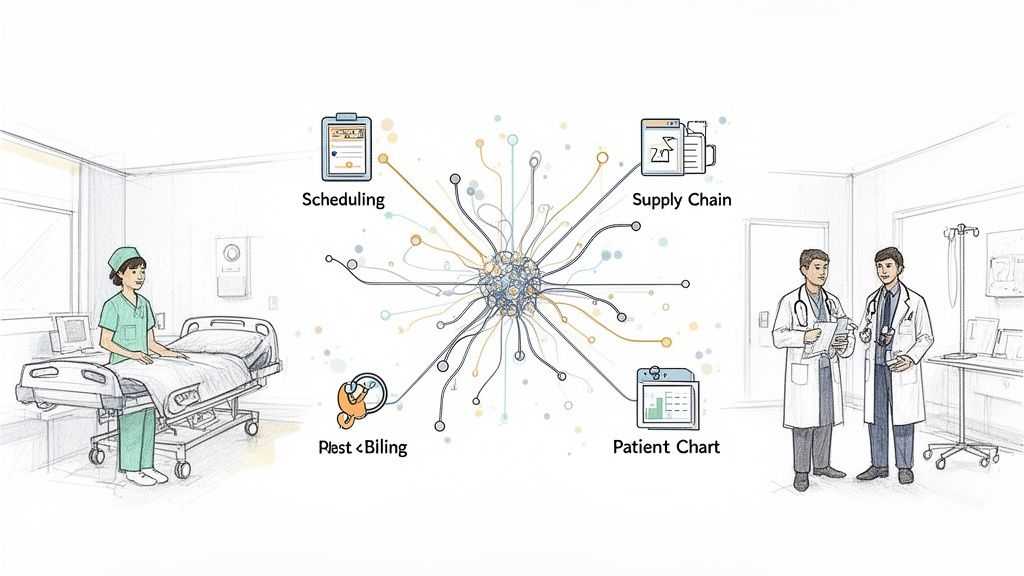
The reach of this technology is surprisingly wide, touching almost every corner of a healthcare organization. From the front desk to the supply closet and the billing office, AI brings a new level of precision and order to an often-chaotic environment.
The Core Functions of AI in Hospital Administration
At its most basic level, AI is incredibly good at spotting patterns in data, making sense of huge information streams, and performing rule-based jobs with flawless accuracy. In a hospital, that ability translates into some powerful capabilities:
Predictive Analytics: AI digs into historical data to forecast things like patient admission spikes, when a critical machine will need maintenance, or when you might run low on essential supplies. It sees problems coming before they disrupt care.
Intelligent Process Automation (IPA): This is where AI takes over multi-step workflows. Think about patient intake, verifying insurance eligibility, or processing claims. IPA handles it all, slashing manual entry and the costly mistakes that come with it.
Natural Language Processing (NLP): These tools allow AI to understand human language. It can automatically transcribe a doctor's spoken notes into a patient's chart, analyze patient survey feedback for common themes, or power a chatbot that helps people schedule appointments 24/7.
By automating these foundational tasks, a healthcare facility can build a more agile, efficient, and patient-focused operation. The whole idea is to remove the friction so that every process—from billing to bed management—just works.
To give a clearer picture, the table below breaks down where AI is making the biggest difference in day-to-day operations.
Key Areas of AI Impact in Healthcare Operations
| Operational Area | Primary AI Function | Key Outcome |
|---|---|---|
| Revenue Cycle Management | Intelligent Process Automation (IPA) | Faster claims processing, fewer denials, and improved cash flow. |
| Patient Flow & Bed Management | Predictive Analytics | Reduced patient wait times and optimized bed turnover. |
| Workforce & Staffing | Predictive Analytics & Automation | Optimized staff schedules and reduced administrative overhead for HR. |
| Supply Chain & Inventory | Predictive Analytics | Prevention of stockouts and reduced waste from expired supplies. |
| Clinical Documentation | Natural Language Processing (NLP) | Reduced physician burnout and more accurate, complete patient records. |
Each of these areas represents a significant opportunity to not only cut costs but also to dramatically improve the experience for both patients and staff.
From Strategy to Reality
Putting these systems to work effectively starts with a clear plan. Platforms offering specialized AI solutions are making this shift far more achievable, helping organizations bridge the gap between their strategic goals and on-the-ground operational wins. A focused approach on AI in the healthcare industry is absolutely essential to make sure the technology aligns perfectly with both clinical workflows and business objectives.
To see how organizations are already succeeding, you can explore specific AI use cases in healthcare and learn from their experience. By targeting the most urgent operational bottlenecks first, health systems can build momentum and show a clear return on investment, paving the way for wider, more ambitious adoption.
Unlocking the Business Case for AI in Healthcare
So, why has AI automation in healthcare operations suddenly gone from a "nice-to-have" idea to a mission-critical investment? It really boils down to a powerful one-two punch: serious cost savings paired with a major leap in patient care. For any healthcare leader trying to build a resilient, patient-first organization, that’s the combination you can’t ignore.
Let’s get specific. Picture a hospital's revenue cycle department before AI. It's often a scene of organized chaos—staff are buried in paperwork, spending hours on the phone chasing prior authorizations, and manually fixing tiny coding errors. The whole process is sluggish, expensive, and riddled with mistakes that lead straight to denied claims and hemorrhaging revenue.
Now, let's look at that same department with AI woven into its fabric. Smart bots instantly verify a patient's insurance eligibility. AI algorithms read through clinical notes and suggest the right medical codes, catching errors before they happen. Predictive analytics even flag claims that are likely to be denied, giving the team a chance to fix them before they’re sent. This isn't some far-off dream; it's the new reality where efficiency is hardwired into the system.
From Operational Gains to Financial Wins
The numbers behind AI are impossible to argue with. When you automate all those repetitive, soul-crushing administrative tasks, you can slash overhead costs in a big way. Think about staff scheduling—using AI to predict patient surges and lulls means you’re not overstaffed on a quiet Tuesday or dangerously understaffed during a holiday rush. That alone hits the bottom line directly.
But it’s not just about cutting costs. AI is also a powerful tool for protecting the revenue you’ve already earned. It can untangle complex billing cycles to find and plug the leaks that quietly drain millions of dollars a year from a hospital's budget. This isn't about asking people to work harder; it's about giving them smarter tools so the organization gets paid fully and fairly for the incredible care it provides. Making this shift isn't always straightforward, and that's where expert AI strategy consulting can bridge the gap between seeing the potential and actually cashing in on it.
The real win here isn't just on the balance sheet. Every dollar you stop wasting on administrative friction is a dollar you can pour back into what actually matters: better patient care, new treatments, and supporting your clinical staff.
The market is clearly catching on. Projections show that by 2025, a staggering 90% of hospitals will be using AI for things like early diagnosis and remote patient monitoring. The AI healthcare market in the USA is expected to skyrocket from $11.8 billion in 2023 to $102.2 billion by 2030. We're already seeing AI-assisted surgeries cut hospital stays by over 20%, which could unlock $40 billion in yearly savings. At the same time, AI-powered nursing assistants are trimming maintenance tasks by 20%, freeing up another $20 billion for hands-on care. You can discover more insights about these AI healthcare statistics on dialoghealth.com.
Connecting Efficiency to Better Patient Outcomes
Here’s the most important part: these operational improvements have a direct and positive impact on patients. When the back-office runs like a well-oiled machine, the entire patient journey gets smoother.
Shorter Wait Times: Automated scheduling and smarter patient flow management mean people spend less frustrating time in the waiting room.
Faster Access to Care: AI-driven prior authorizations get the green light for critical procedures and treatments in a fraction of the time.
More Personalized Treatment: When you free up clinicians from tedious paperwork, they have more time to actually talk to their patients, listen, and develop personalized care plans.
At the end of the day, building the business case for AI is about connecting the dots. It’s about showing how investing in smart automation isn't just a good financial move—it's a fundamental commitment to providing the best possible care for your community.
Where Do You Even Begin? Prioritizing Your First AI Projects
Knowing your organization needs to get on board with AI is one thing; figuring out where to actually start is another challenge entirely. The key is to sidestep the buzzwords and pinpoint real-world opportunities for AI automation in healthcare operations. We’re talking about projects that deliver tangible value fast, creating the momentum you need for bigger changes down the road.
A smart launch begins by zeroing in on the foundational areas where clunky, manual processes cause the most headaches and drain the most resources. Three areas are almost always ripe for improvement: Revenue Cycle Management (RCM), patient flow, and supply chain logistics. Think about it: an AI tool that predicts patient no-shows can instantly optimize schedules and stop revenue leakage, while another that automates prior authorizations can slash the time it takes to get paid.
A Practical Way to Cut Through the Noise
To escape "analysis paralysis," a simple scoring model is your best friend. It helps you objectively weigh and rank potential AI initiatives, forcing you to base decisions on data instead of gut feelings. As we explored in our AI adoption guide, picking the right first project is often the single most important factor for long-term success.
Run each potential use case through this three-part filter:
Impact: How much will this actually move the needle on a metric that matters? Are we talking about cutting costs, shrinking claim denials, shortening wait times, or just making your staff's lives easier?
Feasibility: Can we realistically pull this off? Do we have the right data, the right tech infrastructure, and the people who can make it happen? Is the AI technology for this specific task mature and reliable?
Cost & Resources: What’s the real price tag, including the software, the implementation effort, and the training? How much of your team's time will this soak up?
By scoring each idea on a simple scale (say, 1 to 5 for each category), you’ll end up with a clear, prioritized list. Suddenly, a vague goal like "implement AI" becomes an actionable roadmap that balances big wins with what's actually possible.
The most successful AI strategies don't start with a moonshot. They begin with a well-chosen "quick win" that solves a real, painful problem, proves the value of the technology, and gets everyone in the organization excited about what's next.
Finding Your Starting Line
While every hospital and health system is different, some AI use cases just consistently deliver a great return. The table below lays out some foundational "low-hanging fruit" projects alongside more advanced initiatives to help you think about a phased rollout. For a plan built specifically around your challenges, a Custom AI Strategy report can translate your operational hurdles into well-defined AI projects, drawing from a library of real-world use cases that fit your environment.
High-Impact vs. Low-Hanging Fruit AI Use Cases
This table contrasts foundational projects, which are great for getting started, with more ambitious initiatives that can truly reshape operations over time.
| Operational Area | Foundational Use Case (Quick Win) | Transformative Use Case (Long-Term Impact) |
|---|---|---|
| Revenue Cycle Management | AI-powered medical coding suggestions to improve accuracy and reduce manual review. | Predictive analytics to flag claims with a high probability of denial before submission. |
| Patient Flow & Scheduling | Automated appointment reminders and confirmations via chatbot to reduce no-show rates. | AI-driven bed management systems that forecast discharge times and optimize patient placement. |
| Supply Chain Logistics | Automated inventory tracking for high-value medical supplies to prevent stockouts. | Predictive demand forecasting for pharmaceuticals and equipment based on patient volume trends. |
Choosing where to start is all about finding that sweet spot where a nagging operational problem meets a proven AI solution. Whether that means building powerful internal tooling or deploying existing AI tools for business, the goal is to get tangible results that make the case for going further. For organizations that want to move faster, an "AI Automation as a Service" model can bridge the gap from concept to reality, ensuring your first step with AI is a confident one.
Charting Your Course: An AI Implementation Roadmap That Works
Bringing AI automation into your healthcare operations isn't a flip-of-the-switch event. It’s a journey, and like any important trip, it requires a good map. A phased, step-by-step approach is the only way to manage risk, get everyone on board, and ensure your investment starts paying off from day one.
The entire process kicks off with discovery. Before you even think about vendors or code, you have to get to the root of your operational pain points. What’s causing the most friction? This means conducting a thorough AI requirements analysis—sitting down with department heads, mapping out their daily workflows, and finding exactly where manual processes are creating bottlenecks in patient care or revenue. This groundwork ensures your AI strategy is focused on solving real, tangible problems, not just chasing the latest tech trend.
Getting Everyone on the Same Page and Defining the Project
Once you’ve zeroed in on some high-impact opportunities, your next job is to get buy-in from the people who matter most. This includes everyone from the C-suite holding the purse strings to the clinicians on the floor who will actually use these new tools. A rock-solid business case, packed with data, is your best friend here. You need to clearly explain why this matters: how a specific AI tool will cut down on administrative headaches, smooth out patient flow, or speed up the revenue cycle.
This is also where you’ll face the classic "build vs. buy" decision. Creating custom internal tooling gives you a solution perfectly molded to your unique processes, but it’s a heavy lift in terms of time and resources. On the other hand, working with a specialized partner can get you to the finish line much faster.
To figure out where to start, you need a simple but effective way to prioritize. Think of it in three parts: impact, feasibility, and cost.
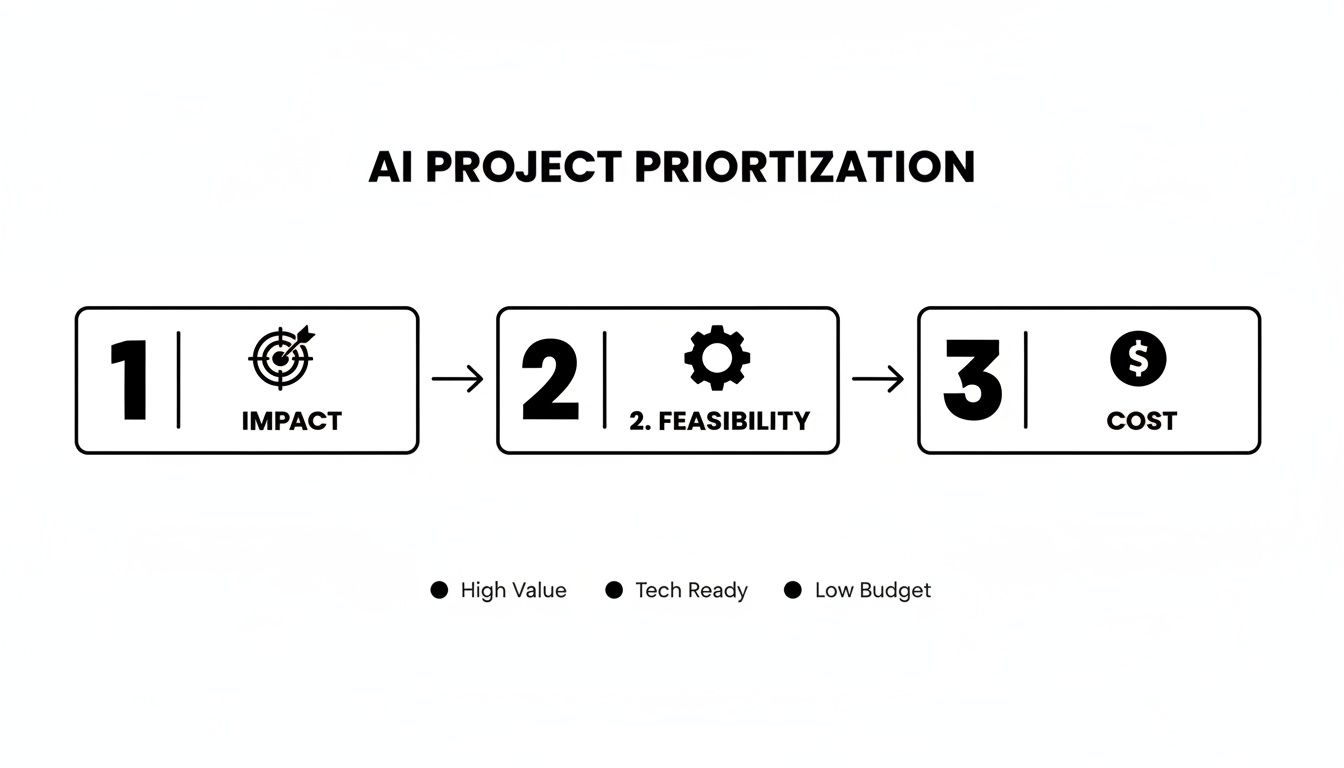
This framework helps you pick pilot projects that offer the biggest bang for your buck with the least amount of initial risk.
Getting Your Data in Order for a Pilot Run
With a project chosen and stakeholders on board, the spotlight turns to data. An AI is only as good as the information it learns from, which makes data readiness a non-negotiable step. Your data needs to be clean, accessible, and properly structured, and it absolutely must integrate smoothly with core systems like your EHR.
Now, it’s time for the pilot program—your real-world test drive. Start small and keep the scope tight. For example, you could automate a single, repetitive task in the billing department. Or, you could pilot a tool like our Clinic AI Assistant to handle routine patient intake questions, proving its value in a controlled environment before rolling it out everywhere.
The whole point of a pilot is to learn fast. You’ll collect feedback, check performance against your initial goals, and smooth out any technical kinks. A successful pilot gives you the hard evidence you need to make the case for a full-scale deployment.
Scaling Up and Never Standing Still
Once your pilot has proven its worth, it's time for the full rollout. This means expanding the solution across the entire department or organization, which demands solid training, thoughtful change management, and a technical backbone that can handle the increased load.
Make no mistake, this is where the industry is heading. By 2025, an estimated 80% of hospitals globally will be using AI to improve operations and patient care. This isn't just a trend; it's driven by a compelling ROI of $3.20 for every $1 invested, often paid back in just 14 months. From scheduling to claims processing, intelligent automation is quickly becoming the new standard for building a modern, efficient healthcare system.
Getting AI Right: Navigating Risks and Compliance
Let's be clear: bringing AI into your healthcare operations isn't just a technical challenge. It's a high-stakes balancing act between innovation and responsibility. You're dealing with sensitive patient data and decisions that affect lives, so managing the risks isn't just a box to check—it's the very foundation of a successful AI strategy.
Get it wrong, and the consequences are severe. A data breach or a biased algorithm that leads to unequal care can destroy patient trust and ruin your organization's reputation overnight. This is why a proactive, transparent approach to risk isn't optional; it's essential.
Building a Foundation of Trust and Safety
Everything starts with a rock-solid data governance plan. Think of it as the rulebook for your AI. You need clear, enforceable policies on how patient data is handled—from collection to storage to its use in AI models—ensuring every single step is compliant with regulations like HIPAA.
But compliance is just the table stakes. True success requires building ethical principles into your strategy from the very beginning. That means actively hunting for and rooting out potential bias in the algorithms you use.
Here’s how to do it right:
Keep a Human in the Loop: This is non-negotiable for critical decisions. The AI can analyze data and suggest a course of action, but a qualified clinician must always have the final say. This model prevents over-reliance on the tech and ensures human expertise remains the ultimate authority.
Demand Algorithmic Transparency: You can't trust a black box. Work with partners who are open about how their models work. If you don't understand the logic behind an AI's recommendation, you can't troubleshoot it, and your clinicians will never fully trust it.
Vet Your Vendors Rigorously: Don't just look at the tech specs. Scrutinize a potential partner's security credentials, compliance certifications, and their actual track record in the healthcare space. A great partner provides more than just powerful AI solutions; they guide you through the regulatory maze.
The goal is to make AI a trusted co-pilot, not an autonomous pilot. When you keep clinicians in control and prioritize transparency, you create the psychological safety needed for people to actually embrace and use these new tools.
When Off-the-Shelf Isn't Enough
While many vendors provide fantastic tools, sometimes the best way to guarantee compliance is to build it yourself. For health systems with unique workflows or exceptionally strict security needs, investing in custom healthcare software development can be a game-changer. This way, you ensure every data protocol and workflow is designed from the ground up to meet your specific operational and regulatory demands.
As we explored in our AI adoption guide, choosing the right path forward is key. Whether you buy or build, the core principles don't change: data governance, ethical oversight, and a human-centered design are the pillars of responsible AI in healthcare.
Measuring the True Impact of Healthcare AI
So, you've invested in AI automation in healthcare operations. How do you actually prove it's working? The real test isn't just a collection of success stories; it's about establishing a rock-solid way to measure your success with tangible Key Performance Indicators (KPIs). Without hard data, even the best AI projects can look like expensive science experiments instead of smart business wins.
The trick is to connect every single AI initiative to a specific, measurable operational metric. This simple step turns vague goals into concrete results and gives you the proof you need to justify future investments.
Key Performance Indicators for Operational AI
You can't use the same ruler to measure every project. Different AI applications demand different metrics.
For an AI system tackling Revenue Cycle Management, you’d want to keep a close eye on your claim denial rate (watching it drop, of course) and the average days in Accounts Receivable (A/R). Seeing those numbers improve means more cash is flowing into the organization, faster.
On the other hand, if you're using AI to optimize patient flow, your go-to KPIs are average patient wait time and bed turnover rate. A successful AI tool will cut down those frustrating waits and free up beds more quickly, which keeps patients happier and lets you serve more people.
Calculating Your Return on Investment
Calculating the ROI for AI isn't just about subtracting costs from savings. Sure, reducing administrative overhead is a big piece of the puzzle, but the real value often lies in the "softer" benefits that are just as critical. Think about the boost in staff morale when tedious tasks disappear, or the higher patient satisfaction scores that come from a seamless, efficient experience.
A solid ROI model should always include:
Direct Cost Savings: Add up the real dollars saved from fewer labor hours, less supply waste, and a drop in denied claims.
Increased Revenue: Track the gains from things like smarter patient scheduling and faster, more accurate billing cycles.
Soft Benefits: Use simple surveys to measure how staff and patient satisfaction levels change over time.
The most convincing arguments for AI funding combine hard financial data with clear proof of a better experience for both patients and clinicians. This gives you the full picture of the value AI delivers.
We're seeing a rapid acceleration in AI adoption for a simple reason: the ROI is becoming too big to ignore. Recent studies show that between 70-85% of healthcare organizations are already exploring generative AI for their operations, and a whopping 82% are reporting moderate to high ROI. These aren't just small wins; they're driving major cost reductions and revenue growth, which is why most leaders are planning to increase their AI budgets.
Ultimately, proving AI's impact boils down to a disciplined, data-first approach. It starts with setting clear baselines before you roll anything out, which allows you to track progress and quantify your success with undeniable accuracy. This data doesn't just validate your initial investment—it builds a powerful case for making AI a core part of your organization's future.
Frequently Asked Questions (FAQ)
How can we ensure AI tools comply with HIPAA?
Compliance is non-negotiable. Prioritize partners with a proven healthcare track record and look for HIPAA-compliant platforms with robust data encryption, access controls, and audit trails. Always establish clear data governance policies and ensure vendor agreements include a Business Associate Agreement (BAA). Implementing a 'human-in-the-loop' system, where clinicians review AI-driven decisions, is a best practice for maintaining accountability and patient safety.
Where do we even begin with AI automation?
The best starting point is to identify a real, pressing operational problem. Is it patient scheduling, revenue cycle bottlenecks, or staff allocation? Conduct a focused discovery phase and a thorough [AI requirements analysis](https://www.ekipa.ai/) to pinpoint where automation can provide the biggest impact. This ensures you’re investing in a solution to a known problem, guaranteeing a clear return from the start.
How do we manage staff concerns about job replacement?
Frame AI as a tool that augments human expertise, not replaces it. Focus the narrative on eliminating tedious administrative tasks to free up clinicians for higher-value work like patient care. Involve your team in the implementation process from the beginning, ask for their input on which tasks are most burdensome, and provide comprehensive training. When staff see AI as a supportive 'digital assistant' that reduces burnout, adoption and enthusiasm will grow.
If you have more specific questions about your own organization's challenges, our expert team is always ready to talk. We can help you navigate everything from initial strategy to a full-scale rollout.
Ready to turn your operational challenges into a clear, actionable AI strategy? Ekipa AI can deliver a Custom AI Strategy report in just 24 hours, giving you a roadmap for building scalable AI solutions.