AI in Remote Patient Monitoring Systems: Transforming Healthcare Outcomes
AI in remote patient monitoring systems delivers insights for proactive care, improving outcomes. Explore benefits, use cases, and implementation tips.

Remote Patient Monitoring (RPM) isn't just about collecting data anymore; it's about finding life-saving insights buried inside that data. When you add AI to remote patient monitoring systems, you turn a passive data-gathering tool into a truly proactive system of care. It's designed to spot subtle health changes long before they escalate into a crisis.
This change is fundamental. It moves us from simply reacting to problems to actively preventing them.
The New Era of Proactive Healthcare
Traditional healthcare has always had blind spots. It relies on periodic check-ups and whatever symptoms a patient thinks to mention, leaving huge gaps where a condition could quietly worsen. RPM was a great first step to closing those gaps, but it created a new problem: a firehose of raw data that clinicians had to manually sort through.
This is where AI completely changes the game.
By embedding powerful AI solutions, providers can analyze continuous data streams from wearables and home sensors as they happen. An AI doesn't just see a single blood pressure reading. It sees the subtle trends, patterns, and anomalies over days or weeks—connections that are often invisible to the human eye.
From Reactive to Predictive Care
This evolution marks a shift from a reactive care model to one that is genuinely predictive and preventive. Think about managing chronic diseases like heart failure or diabetes, which are responsible for a huge number of hospital readmissions.
-
Catching Problems Early: An AI can spot a slight but steady increase in a patient's weight combined with a minor dip in oxygen saturation. This might indicate fluid retention, a key warning sign of heart failure, days before the patient even feels symptoms.
-
Smarter, Personalized Alerts: Instead of generic high/low alerts, AI learns each patient's unique baseline and only flags deviations that matter. This cuts down on the "alarm fatigue" that plagues clinical staff, letting them focus on alerts that truly need intervention.
-
Better Use of Clinician Time: By automating that first layer of data analysis, AI frees up skilled nurses and doctors. They can spend less time sifting through data and more time on complex decisions and actual patient care, which improves efficiency and outcomes.
This intelligent approach to monitoring is essential for managing our aging population and the growing burden of chronic illness, a challenge we discussed in our AI adoption guide. By developing a clear strategy for AI in healthcare, organizations can dramatically improve patient health while making their own operations more efficient.
The real value of AI in RPM is its ability to turn a flood of data into a single, actionable insight. It’s the difference between hearing a wall of background noise and hearing someone whisper a specific warning.
Ultimately, this proactive approach doesn't just keep patients healthier—it delivers serious business value. By cutting down on expensive hospital readmissions and enabling more efficient models of care, AI becomes a cornerstone of sustainable, modern healthcare. A thoughtful AI strategy consulting process can help organizations identify the highest-impact opportunities, unlocking both clinical and operational wins that will define the new standard of patient care.
Understanding the Core Components of an AI-Powered RPM System
Think of an AI-powered RPM system less like a piece of software and more like a high-tech security detail for a patient's health. It has distinct layers, each with a crucial job, all working in concert to turn a stream of raw data into a life-saving action plan.
The high-level flow is pretty straightforward: you gather the data, send it somewhere safe, let the AI figure out what it means, and then present those findings to a clinician who can step in. But as with anything in healthcare, the devil is in the details. If any one of these steps falters, the whole system's value drops.
This process shows how AI acts as the central engine, turning a constant flow of data from remote devices into real clinical intelligence.
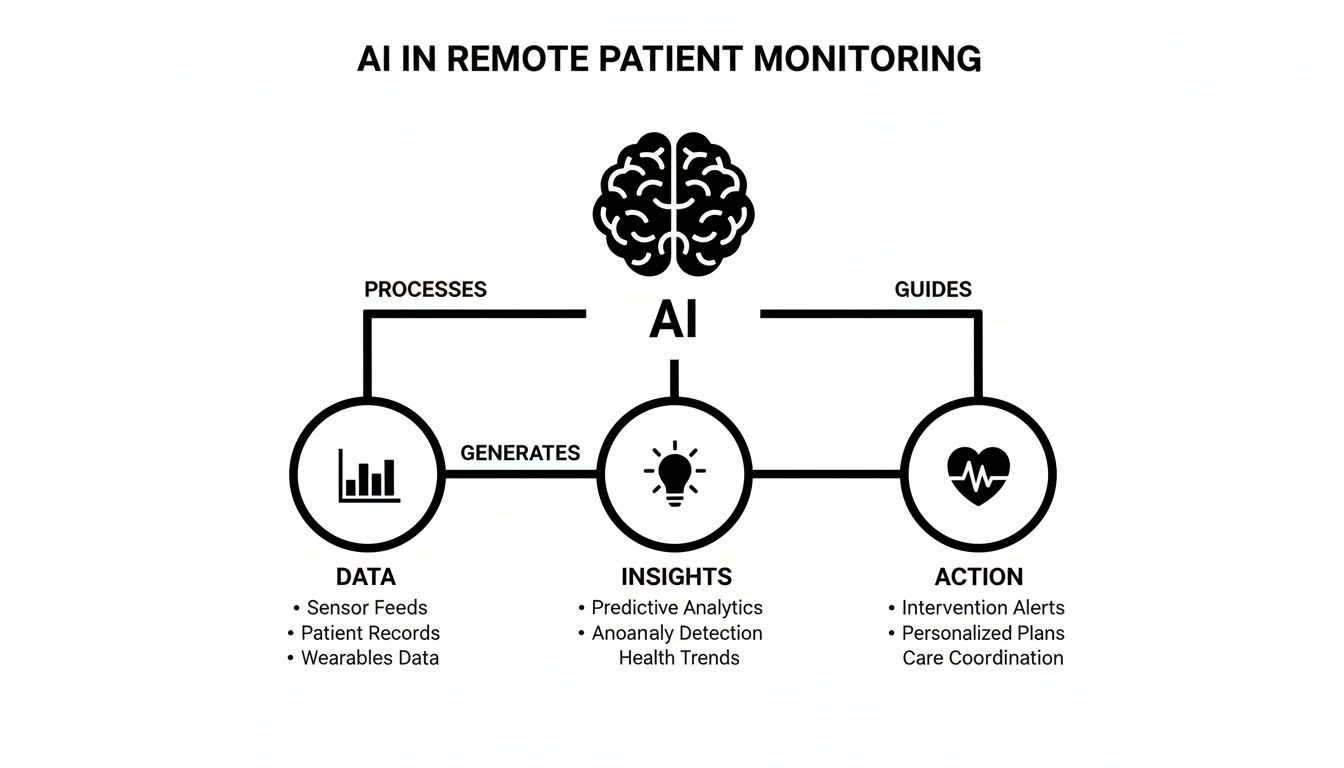
You can see the clear path from data collection to intelligent insights and, finally, to a decisive clinical response. The AI is what makes this entire loop proactive instead of reactive.
The Four Foundational Layers
A solid AI-powered RPM architecture really comes down to four essential components. Each one hands off to the next, creating a complete ecosystem that connects the patient's home directly to the care team.
-
Data Acquisition Layer: This is where it all starts, right in the patient's hands. We're talking about the physical hardware—wearables, smart blood pressure cuffs, continuous glucose monitors, and even smart scales. These are the "eyes and ears" on the ground, gathering the vital physiological data that fuels the entire system.
-
Data Transmission Layer: Once a reading is taken, it has to go somewhere. This layer is the secure pipeline, using IoT networks like cellular or Wi-Fi to move that information from the patient's device to a central cloud platform. Security here is non-negotiable; everything has to be locked down to protect patient privacy and stay compliant with regulations like HIPAA.
-
AI Analytics Engine: Welcome to the brains of the operation. This is where all that raw data gets crunched by machine learning models and sophisticated algorithms. It’s here that the system spots subtle trends, flags anomalies that a human might miss, and even predicts potential health crises before they happen. Getting this right demands a thorough AI requirements analysis to ensure the models are trained on the right data to produce clinically meaningful alerts.
-
User Interface Layer: The final piece is how people interact with all this intelligence. For clinicians, it’s a dashboard that surfaces the most urgent alerts. For patients, it might be a mobile app offering health tips. This interface must translate complex AI insights into simple, actionable information. Designing effective internal tooling for care teams is absolutely critical for driving adoption and making the system genuinely useful.
The Different AI Tools in the Engine's Toolbox
Not all "AI" is the same, and different tools are used for different jobs inside that analytics engine. Knowing what they are and what they do is key to building a robust system or working with an AI Strategy consulting tool to map out an implementation.
The table below breaks down the key AI technologies and what they actually do in an RPM system.
Key AI Technologies in RPM and Their Functions
| AI Technology | Primary Function in RPM | Example Application |
|---|---|---|
| Machine Learning (ML) | Sifts through huge datasets to find patterns and predict what might happen next. | Forecasting a patient's risk of hospital readmission by analyzing their daily vitals against historical data. |
| Natural Language Processing (NLP) | Pulls meaningful information from unstructured text, like notes or messages. | Analyzing a patient's free-text journal entries in an app to spot signs of depression or unreported symptoms. |
| Deep Learning | A specialized form of ML using neural networks for complex data like images or EKG waveforms. | Spotting subtle irregularities in an EKG reading that could point to an undiagnosed arrhythmia. |
| Rule-Based Expert Systems | Uses a set of predefined "if-then" clinical rules to automatically trigger alerts. | Sending an instant alert when a diabetic patient's blood glucose reading crosses a specific, clinically-set danger threshold. |
By weaving these technologies together, an RPM system becomes more than just a data collection tool. It becomes an intelligent partner in care delivery, capable of surfacing insights that were previously impossible to find at scale. This is the foundation for any serious custom healthcare software development project in this space.
What's the Real Payoff? The Business Case for AI in RPM
Bringing AI into your remote patient monitoring program isn't just a shiny new tech upgrade—it's a smart business decision with a clear, measurable return. Yes, better patient outcomes are always the North Star. But for the C-suite, the financial and operational wins are what make this a can't-miss opportunity. AI takes RPM beyond simple data gathering and turns it into a powerful engine for value.
This isn't some niche experiment; it's a massive market shift. In 2024, the global AI in RPM market was already valued at $1.99 billion. Fast forward to 2030, and it's projected to explode to $8.51 billion. That's a compound annual growth rate of about 27.5%, fueled by the desperate need for better ways to manage chronic diseases that are overwhelming our healthcare system. You can discover more about this market expansion on Grand View Research.
Slashing Your Operational Costs
One of the first places you'll see the impact is on the balance sheet. AI-powered RPM is a fantastic tool for cutting down on hospital readmissions, which are a huge financial drain on any healthcare organization. By flagging high-risk patients before they crash, your clinical teams can step in early and keep them out of the hospital.
It also brings much-needed sanity to clinical workflows. Think about it: instead of your nurses drowning in a sea of data alerts, AI acts as the first line of defense. It intelligently triages the noise, only escalating the truly urgent cases that need a human eye. This frees up your highly-trained clinicians to do what they do best—caring for patients, not staring at dashboards.
By automating routine data analysis and intelligently prioritizing alerts, AI turns a high-volume, low-signal data stream into a low-volume, high-signal source of clinical intelligence. This shift is the core of its operational value.
Unlocking New Ways to Generate Revenue
But it's not all about saving money. AI in remote patient monitoring systems actually opens up entirely new ways to bring in revenue. You could, for instance, launch premium monitoring services for post-surgical patients or those managing complex conditions. For patients, it’s an extra layer of peace of mind; for you, it's a brand-new service line.
Then there’s the data itself. The enormous amount of anonymized health data you collect is an incredibly valuable asset. This data can fuel population health studies, support partnerships with pharmaceutical companies on clinical trials, or even be used to build your own proprietary predictive models. A structured AI Product Development Workflow can help turn these ideas into reality.
Sharpening Your Competitive Edge
In today's healthcare landscape, standing out is everything. Offering sophisticated, AI-driven care is a massive differentiator. Patients are savvy; they're actively looking for providers who use technology to make care more personal, proactive, and convenient. Adopting these systems helps you attract and retain patients while building a reputation as an innovator.
This forward-thinking approach also makes you a far more appealing partner for insurance companies and corporate wellness programs. It signals that you're focused on efficiency and superior outcomes, which aligns perfectly with an AI Automation as a Service mindset. The goal is to create a sustainable advantage, and a Custom AI Strategy report can provide the roadmap to get you there.
Real-World AI in Patient Monitoring: From Theory to Lifesaving Action
Knowing the architecture behind AI in remote patient monitoring systems is one thing, but seeing it in action is where its true value becomes clear. These real-world use cases show that across medicine, AI isn't just a concept anymore—it's actively preventing crises, personalizing treatments, and fundamentally changing patient outcomes. It’s the engine that turns a constant flood of data into precise, life-saving interventions.
Let's move past the theory and look at a few powerful examples of how these systems are working today.
This kind of seamless connection between patient data and clinical oversight is the heart of effective RPM. The right AI tools for business are designed to bridge this exact gap, making sure data always leads to decisive action.
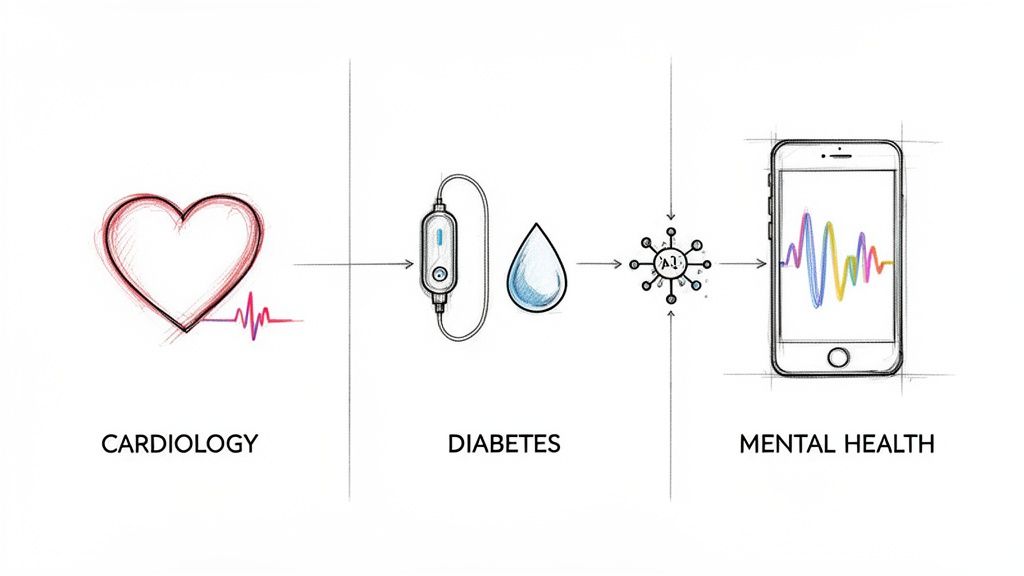
Predictive Analytics in Cardiology
For anyone living with a chronic heart condition, the fear of a sudden cardiac event is always present. AI-powered RPM offers a new kind of safety net, shifting care from simply monitoring to actively predicting.
Instead of just flagging a single high blood pressure reading, AI algorithms look deeper. They analyze subtle, interconnected patterns over time—correlating a slight increase in weight (a sign of fluid retention) with a minor drop in oxygen saturation and tiny shifts in heart rate variability. These combined signals can predict an acute cardiac event days before it happens.
This gives care teams a crucial window to intervene. A quick medication adjustment or a telehealth visit can often prevent a dangerous and expensive trip to the hospital.
The real goal here is to spot the "silent signals" that come before a crisis. AI is uniquely capable of detecting a combination of seemingly minor changes that, when pieced together, paint a clear picture of escalating risk.
The results speak for themselves. Projects like Kaiser Permanente's AI in mortality reduction prove how predictive models can lead to dramatically better outcomes.
Proactive Management in Diabetes Care
Managing diabetes is a constant balancing act. AI-driven RPM systems function like an intelligent co-pilot for patients, offering continuous support to prevent dangerous hypoglycemic or hyperglycemic episodes.
Continuous Glucose Monitors (CGMs) generate a nonstop stream of data, which AI models use to:
-
Predict Glucose Spikes and Dips: The AI learns a patient’s individual response to different foods and activities, allowing it to forecast glucose trends hours in advance.
-
Offer Personalized Nudges: The system can send timely reminders, like suggesting a short walk after a big meal or alerting someone that their levels are trending low.
-
Automate Insulin Dosing: In the most advanced setups, AI connects directly with insulin pumps to create a "closed-loop" system that automatically adjusts insulin delivery based on real-time data.
This proactive approach empowers patients to take better control of their condition while reducing the mental fatigue that comes with making constant decisions.
The Emerging Role in Mental Healthcare
Perhaps the most exciting frontier for AI in RPM is mental health. This is the fastest-growing segment in the field, with the highest projected CAGR from 2025 to 2030. AI-powered monitoring is helping to address a global crisis where the demand for continuous, stigma-free support far outpaces what traditional therapy can provide.
These platforms analyze data from wearables, smartphone usage patterns, and self-reported inputs to detect the early signs of anxiety, depression, or mood shifts. This enables personalized interventions exactly when they're needed most. As mental health concerns continue to rise, this kind of accessible, immediate support is critical.
Navigating the Realities of Implementation
Bringing AI into your remote patient monitoring system is more than just a tech upgrade; it’s a fundamental shift in how you operate. Getting it right means looking beyond the algorithms and tackling the thorny issues of data privacy, technical integration, and, most importantly, getting your team on board. The path is complex, but navigating it successfully is what separates a stalled project from one that genuinely improves patient outcomes.
The journey starts by being honest about the roadblocks. We're talking about everything from locking down sensitive patient data to getting brand-new AI tools to play nice with decades-old hospital software. Every single step demands a thoughtful plan.
Overcoming the Big Three Hurdles
Interestingly, the toughest challenges often have less to do with the AI itself and more to do with the environment it has to live in. If you lose patient trust, run afoul of regulators, or disrupt clinical workflows, the best algorithm in the world won't save you.
Three hurdles consistently pop up:
-
Data Privacy and Regulatory Compliance: We're dealing with patient health information, which is as sensitive as it gets. Your system has to be completely locked down and compliant with regulations like HIPAA. This isn't optional. It means end-to-end data encryption, airtight access controls, and crystal-clear patient consent processes are non-negotiable.
-
System Integration and Interoperability: An AI-powered alert is worthless if a clinician never sees it. The biggest technical headache is usually interoperability—making your new AI system communicate seamlessly with existing Electronic Health Records (EHRs). This requires building secure APIs and using established healthcare data standards to ensure critical insights land directly in the clinical workflow, not in some isolated new dashboard.
-
Staff Training and Adoption: Technology is only a tool; people have to actually use it. Your clinicians need to understand not just how to click the buttons, but why they should trust the AI-generated alerts and how this new information helps them care for patients better. Skimp on training, and you’ll be met with resistance and skepticism, dooming the entire investment.
Best Practices for a Smooth Rollout
To get past these challenges, you need a methodical, structured approach. Rushing an implementation is a recipe for costly mistakes and a project that goes nowhere. The key is to build a solid foundation by sticking to what works.
The goal of implementation isn't just to launch new technology. It's to integrate a new way of working. That means focusing just as much on people and processes as you do on platforms and algorithms.
Here are a few best practices to keep you on track:
-
Start Small with a Focused Pilot: Don't try to boil the ocean. Pick one specific, high-impact problem to solve first—like reducing hospital readmissions for patients with congestive heart failure. A successful pilot proves the system's value, lets you iron out the wrinkles, and builds momentum for a broader rollout.
-
Follow a Structured Workflow: A clear, repeatable process is your best defense against risk. Adopting a structured AI Product Development Workflow ensures that every stage, from the initial idea to final integration and user training, is planned and executed with precision.
-
Go All-In on Training and Change Management: You can't over-invest here. Set aside real time and resources for hands-on staff training. Be transparent about the benefits, listen to their concerns, and identify clinical champions who can help guide their peers through the transition.
-
Take it One Step at a Time: A phased rollout is almost always the right answer. This iterative approach allows you to learn and make adjustments as you go, ensuring the final system is truly built for the real-world needs of your patients and providers.
The Future of Intelligent Patient Care
The horizon for AI in remote patient monitoring systems is expanding at a breakneck pace. We're moving beyond simple predictive alerts and into a new era of deeply personal, proactive healthcare. The next wave of innovation is all about the fusion of healthcare, smart environments, and sophisticated AI, making patient monitoring a seamless, almost invisible part of daily life.
This isn't just a futuristic concept; the momentum is real and measurable. Projections show that by 2025, over 71 million Americans—a staggering 26% of the population—will be using remote patient monitoring. And it’s not just patients; a recent survey found that 87% of U.S. healthcare organizations are already weaving RPM into their care models, proving that AI-guided care at home is rapidly becoming the new standard.
The Dawn of Digital Twins and Generative AI
One of the most powerful developments on the horizon is the concept of a "digital twin" in healthcare. Think of it as a dynamic, virtual copy of a patient, continuously updated in real-time with data from their RPM devices. This isn't science fiction. This digital replica lets clinicians run simulations, testing how different treatments or lifestyle adjustments might affect that specific person, paving the way for a truly personalized approach to medicine.
At the same time, generative AI is poised to completely change how we communicate with patients. Forget generic, one-size-fits-all reminders. Soon, AI will craft personalized messages, educational content, and motivational coaching based on an individual's unique health data, their preferred communication style, and even their current emotional state. This is what's shaping the future of physical therapy and so many other fields.
Seamless Monitoring in Smart Environments
The future of RPM is also ambient, meaning it will blend into the background of our lives. Monitoring will evolve beyond just wearables and will be embedded into the smart home devices people already use. Imagine sensors that passively track vital health data—like a person's gait, sleep quality, and respiratory patterns—without them ever having to lift a finger.
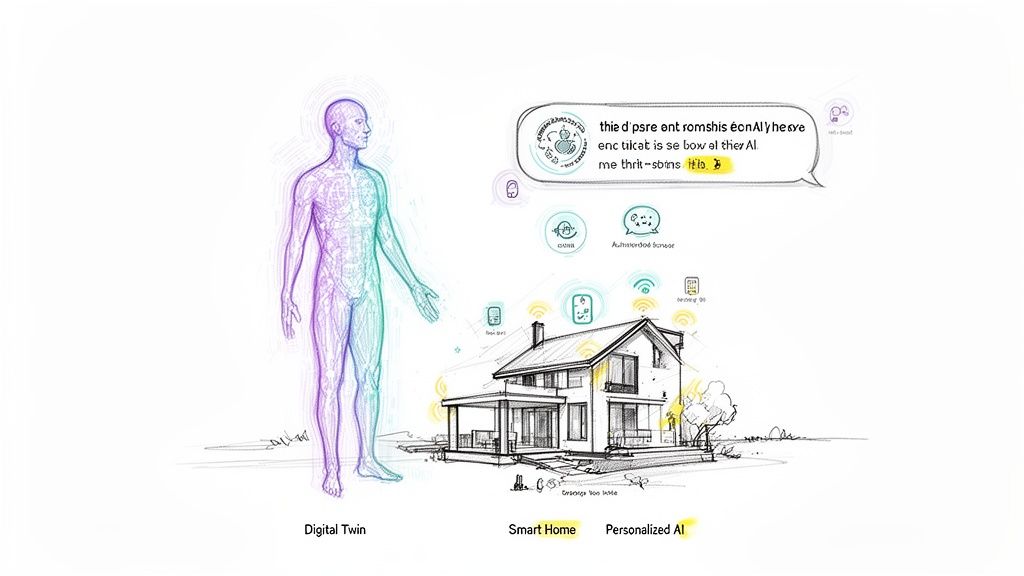
This holistic view connects clinical metrics with everyday lifestyle data, giving healthcare providers a much richer, more complete picture of a patient's overall well-being.
The future of remote care isn't about more devices; it's about more intelligence. It's about creating an ecosystem where technology fades into the background, providing continuous, invisible support that keeps people healthier at home.
Organizations that get ahead of this curve are the ones laying the groundwork for their AI strategy today. Getting started means turning these ambitious concepts into a practical roadmap. Navigating this complex but rewarding journey is the key to defining and building the future of intelligent patient care.
Your AI in RPM Questions, Answered (FAQ)
As a leader in healthcare, you're naturally going to have some tough questions about bringing AI into your remote patient monitoring programs. It’s a big step. Let's tackle some of the most common ones.
Where Do We Even Start with Implementing AI in Our Current RPM Services?
The first move isn't technical at all—it’s strategic. Before you start looking at cool algorithms or talking to vendors, you have to get crystal clear on the one big problem you want to solve. Is it about cutting down 30-day readmissions for your heart failure patients? Or maybe it's boosting medication adherence for people managing diabetes?
You have to start with a deep dive, essentially an AI requirements analysis, to take stock of what you have: your data sources, your current tech infrastructure, and what success actually looks like. Bringing in some help with AI strategy consulting can really speed this up. They can help you map out a small, focused pilot project with clear goals to prove the concept before you think about a larger rollout.
How Can We Be Sure AI Is Handling Patient Data Securely and Stays HIPAA Compliant?
This is non-negotiable, and compliance has to be baked in from the very beginning. Any trustworthy AI-powered RPM system protects patient data with several layers of security.
-
Encryption: Think of it like a digital armored truck. All patient data is encrypted, both when it's moving between systems and when it's sitting in a database.
-
Access Controls: Strict, role-based controls are put in place. This ensures that only the right clinicians with the right permissions can access specific patient information. No exceptions.
-
Data Anonymization: The AI models themselves are typically trained on vast datasets that have been anonymized or de-identified. This means the AI learns the critical patterns of a disease without ever knowing the personal identity of the patients involved.
When you're looking for a partner for custom healthcare software development, you absolutely must confirm they have a proven track record of building HIPAA-compliant platforms from the ground up.
Will This AI System Actually Work with Our Existing EHR?
Yes, it has to. Seamless integration with your Electronic Health Record (EHR) is a make-or-break feature for any modern AI RPM platform. If it doesn't plug into your existing workflow, your clinicians won't use it.
This connection is usually made using secure Application Programming Interfaces (APIs) and by following standard healthcare data protocols like HL7 and FHIR. A proper integration means the smart alerts and insights from the AI pop up right where your care teams are already working. Any solid AI Product Development Workflow will dedicate a specific phase to planning and testing this critical link to make sure it’s smooth and genuinely useful.
What’s the Real ROI on an AI Investment for Remote Monitoring?
The return on investment here isn't just a single number; it shows up in a few different, powerful ways across your organization.
The ROI isn't just about saving money on readmissions; it's about reallocating your most valuable resource—clinician time—to where it matters most, creating a more efficient and effective care delivery model.
On the financial side, the ROI is clear: lower costs from fewer hospitalizations and more efficient staffing. Operationally, you'll see it in smoother workflows and less time spent on administrative tasks. And most importantly, the clinical return is measured in what matters most: better patient outcomes and the ability to intervene earlier, potentially saving lives. A Custom AI Strategy report can help you build a model to see what that potential ROI could look like for your specific patient groups and goals.
Ready to build your AI advantage? Ekipa AI delivers tailored AI strategies and execution support to turn your vision into scalable impact. Our work is driven by our expert team of strategists and developers dedicated to your success. Explore our AI solutions and start your transformation today.