Patient Engagement Using Conversational AI to Transform Healthcare
Discover how patient engagement using conversational AI boosts satisfaction and outcomes. Learn practical strategies for implementation and measuring ROI.
Picture a healthcare experience where the "front door" is always open, ready to help a patient whenever they need it. That’s the practical reality of patient engagement using conversational AI. This isn't about basic chatbots; it’s about sophisticated digital assistants that create helpful, personalized, and even empathetic interactions.
Opening the Digital Front Door to Modern Healthcare
Whether someone needs to book an appointment late at night or get a quick answer about their post-op instructions, AI makes communication that used to be slow and frustrating feel instant and easy. This move toward a smoother, AI-guided experience doesn't just improve patient satisfaction—it gives providers the bandwidth to deliver better care more efficiently. These advanced AI solutions are quickly becoming the new standard.

The market data confirms this shift. In fact, the patient engagement and support segment accounted for over ~29.5% of conversational AI healthcare revenue in 2024. Hospitals and clinics were the biggest adopters, making up about 38.1% of the end-user share.
This tells us exactly where the investment is going: improving core functions like scheduling, initial triage, and follow-up for chronic conditions. With its high telehealth adoption rates and strong incentives to lower the cost-per-patient, North America is expected to continue leading the market.
The New Standard of Patient Access
This "digital front door" is more than a convenience. It’s a fundamental change in how people access and receive care. To fully grasp this, it helps to understand how telehealth works, as conversational AI often serves as the intelligent greeter for these virtual services. It guides patients to the right place, whether that’s a video visit, an in-person appointment, or a self-help resource.
This approach directly tackles some of healthcare's oldest frustrations:
- 24/7 Availability: Patients aren't stuck waiting for office hours to get answers. This reduces their anxiety and can stop small problems from becoming bigger ones.
- Reduced Administrative Burden: Automating routine questions and scheduling frees up front-desk staff and nurses to focus on patients needing their direct attention.
- Personalized Communication: The AI can send reminders and information tailored to a patient's specific condition, appointment schedule, and preferred way of communicating.
By meeting patients where they already are—on channels like SMS and web chat—healthcare organizations can dramatically lift engagement and build stronger, more trusting relationships.
Ultimately, the aim is to build a healthcare system that feels more responsive and easier to navigate. By putting smart automation at the very first point of contact, providers can create a better patient journey from the get-go.
For a closer look at how these tools are being applied across the board, see our work on AI for the healthcare industry. Now, let’s explore the specific strategies that make this all possible.
Why Conversational AI Is a Game-Changer for Patient Experience
Conversational AI is fundamentally changing how patients interact with healthcare, moving well beyond the old ways of communicating. It’s about creating 24/7 access to support, personalizing conversations on a massive scale, and, just as importantly, taking a huge administrative load off your clinical staff.
Think about the classic appointment reminder process. It's a grind. Staff members spend hours making phone calls, leaving voicemails, and just hoping someone calls back. It’s a slow, inefficient cycle that frustrates everyone involved.
Now, let's look at an AI-powered approach. A smart system automatically sends a friendly, personalized text message to a patient. It confirms their visit and might even share helpful pre-visit instructions. This one small change frees up nurses and administrators to do the work that actually requires their expertise. These are the kinds of real, tangible wins that well-designed AI solutions bring to the table.
From Administrative Burden to Empowered Staff
The benefits run much deeper than just convenience. When your team isn't tied up with endless repetitive tasks, they can finally dedicate their time and skill to more complex patient needs. This is a direct answer to staff burnout, one of the most pressing issues in healthcare today.
By automating routine outreach, conversational AI allows healthcare professionals to operate at the top of their license. It transforms their roles from managing logistics to delivering high-quality, empathetic care.
This boost in operational efficiency creates a powerful ripple effect across the organization. It builds a solid business case by linking better patient satisfaction directly to measurable health outcomes and a healthier bottom line. The first step is mapping this out with a clear AI strategy consulting plan.
Building Proactive and Personalized Patient Relationships
Real patient engagement isn’t built on one-off phone calls; it's about creating a consistent, supportive dialogue. Conversational AI makes it possible to maintain that connection, supporting patients long after they’ve left the clinic. This is where the technology truly comes alive.
It's a complete shift in how you can support patients:
- Proactive Support: Instead of waiting for a patient to call with a problem, the AI can check in first. A simple message like, "Hi Alex, just checking in on Day 3 post-op. How is your pain on a scale of 1-10?" can flag potential issues before they become serious.
- On-Demand Education: Patients can get reliable answers about their condition or treatment plan whenever a question pops into their head. This gives them the information they need right when they need it, which helps them stick to their care plan and reduces their anxiety.
- Seamless Escalation: If the AI spots a question it can't handle or a response that signals a medical concern, it can instantly hand off the conversation to a real person. This keeps patients safe while still filtering out the routine inquiries.
These aren't just basic chatbots. The technology behind these interactions is smart enough to understand what a patient means, log structured data for the care team, and tailor its responses to where the patient is in their journey. This is a core focus of our "AI Automation as a Service" offering.
The ultimate goal is to make healthcare feel more responsive, supportive, and personal. As we see more and more real-world use cases emerge, it's clear that the organizations winning with this technology aren't just using it to cut costs—they're using it to build stronger relationships.
Key Use Cases for AI Across the Patient Journey
Theory is great, but to really grasp the impact of conversational AI in healthcare, you have to see it in action. This isn't some far-off concept; it's being used right now to solve some of the most persistent challenges in patient care. Let's break down the typical patient journey and pinpoint exactly where these AI tools make the biggest difference.
The whole idea is to use AI to improve access, make communication more personal, and automate the tedious tasks that bog down your staff. It’s a simple but powerful flow.
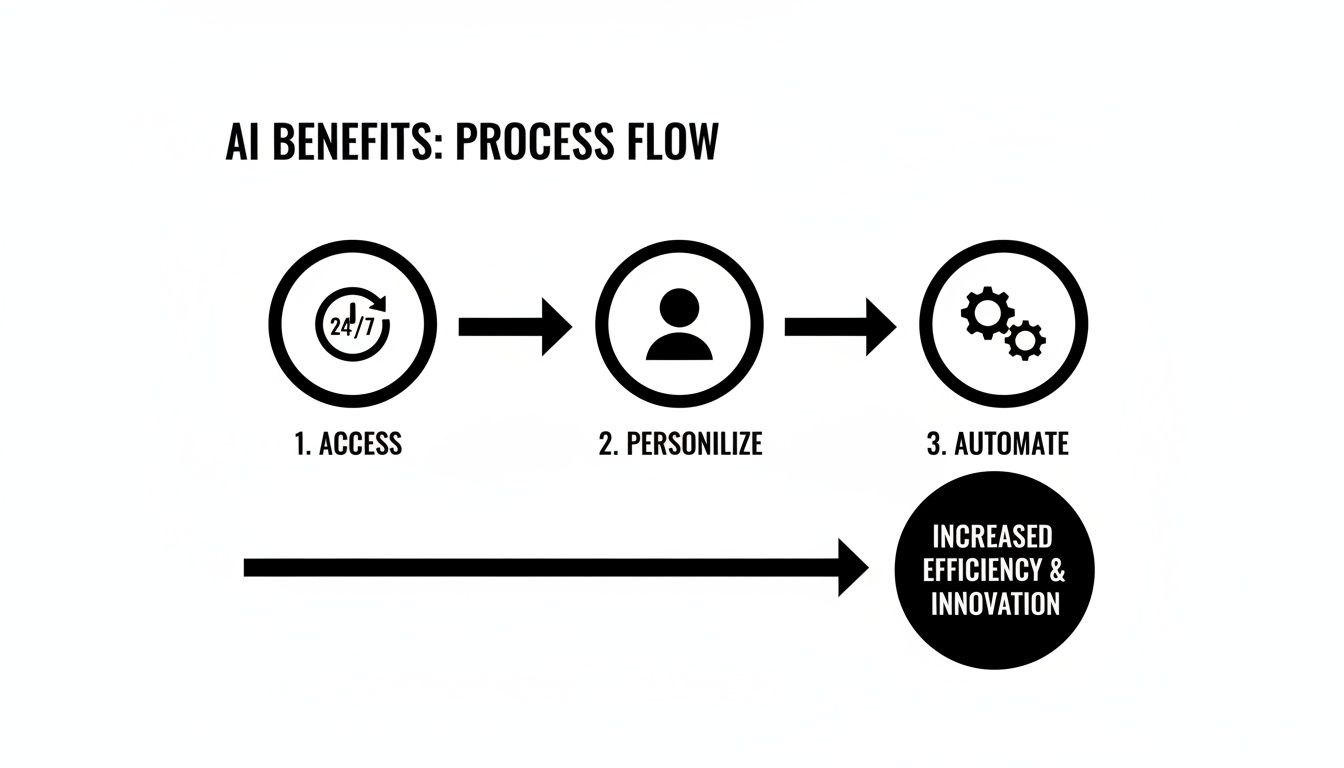
When you look at it this way, you can see how each step feeds the next, creating a positive cycle of better patient outcomes and a more efficient practice.
Appointment and Pre-Visit Management
Let’s start with one of the biggest headaches for any clinic: scheduling. Missed appointments aren't just an inconvenience; they're a massive financial drain, costing the U.S. health system an estimated $150 billion every year.
AI-powered reminders and two-way messaging can cut no-show rates by as much as 30%. This isn't just about efficiency; it's about meeting patients where they are. A recent study showed that 76% of patients actually want to communicate with their providers via a simple, automated text message.
Before a patient even walks through the door, AI can handle the pre-visit work. It can send digital intake forms and collect their medical history through a simple, guided chat. This means less time in the waiting room filling out clipboards and more time for your staff to focus on actual care.
Post-Discharge and Follow-Up Care
Those first few days and weeks after a patient leaves the hospital are absolutely critical. This is where conversational AI can serve as a vital safety net, ensuring no one falls through the cracks.
- Automated Check-ins: The AI can send a quick text asking how a patient is feeling, what their pain level is, or if they're experiencing any side effects. This creates a clear, structured log of their recovery.
- Proactive Education: Depending on their condition, the AI can send helpful, bite-sized content, like a quick video on how to change a dressing or a tip for managing a new medication.
- Intelligent Triage: This is the game-changer. If a patient replies, "my pain is an 8 out of 10," the system can instantly flag that message and alert a nurse. This allows for early intervention before a small problem becomes a real emergency.
This kind of consistent, automated follow-up gives patients peace of mind and helps clinical teams spot trouble early.
Chronic Care and Medication Adherence
Managing a chronic condition is a marathon, not a sprint. It requires constant attention and support, which is a role conversational AI is perfectly built for. Think of it as a personal health coach that’s available 24/7.
It can send a daily reminder to check blood sugar or take medication. But it’s smarter than a simple alarm clock. If a patient reports that they missed a dose, the AI can ask a follow-up question to understand why and offer helpful advice, all while logging that information for their doctor. For these kinds of high-touch workflows, dedicated tools like a Clinic AI Assistant can be configured to manage the specifics.
By making it easy for patients to track their health and stay on plan, conversational AI empowers them to take a more active role in their own care, leading to better long-term outcomes.
As more digital health tools enter the market, it's also important to understand their real-world clinical application. For anyone interested in how this is playing out, exploring professional perspectives on integrating smartwatch data into patient care provides some excellent context.
To really drive home the difference, let’s look at a side-by-side comparison. The table below puts the old, manual way of doing things right next to the new, AI-powered approach. The advantages become pretty clear, pretty quickly.
Traditional vs. AI-Powered Patient Engagement Workflows
This table compares key patient communication tasks, showing the advantages of using conversational AI over traditional manual methods in terms of efficiency, scalability, and patient experience.
| Engagement Task | Traditional Method (Manual) | Conversational AI Method (Automated) | Key Benefit |
|---|---|---|---|
| Appointment Reminders | Staff makes individual phone calls, leaves voicemails. | AI sends personalized, two-way SMS/chat reminders. | Reduces no-shows by up to 30% and frees up staff time. |
| Post-Discharge Follow-Up | A nurse calls patients sporadically when time permits. | AI sends scheduled check-in messages and collects structured data. | Ensures consistent follow-up for all patients and early issue detection. |
| Medication Adherence | Relies on patient memory and occasional verbal reminders. | AI sends daily prompts and provides on-demand educational support. | Improves adherence rates and provides data on patient behavior. |
| Patient Questions | Patients call the front desk, wait on hold, and leave messages. | AI provides instant answers to common questions 24/7. | Boosts patient satisfaction and lowers call center volume. |
Looking at this, you can see it’s not just about doing the same things faster. It’s about creating a fundamentally better, more supportive, and more efficient experience for both patients and staff.
Your AI Implementation Roadmap: A Step-by-Step Guide
Bringing conversational AI into your patient engagement strategy is more like a carefully planned expedition than flipping a switch. You need a clear map. A phased approach is the only way to manage the complexity, show value quickly, and set yourself up for long-term success without overwhelming your entire organization.
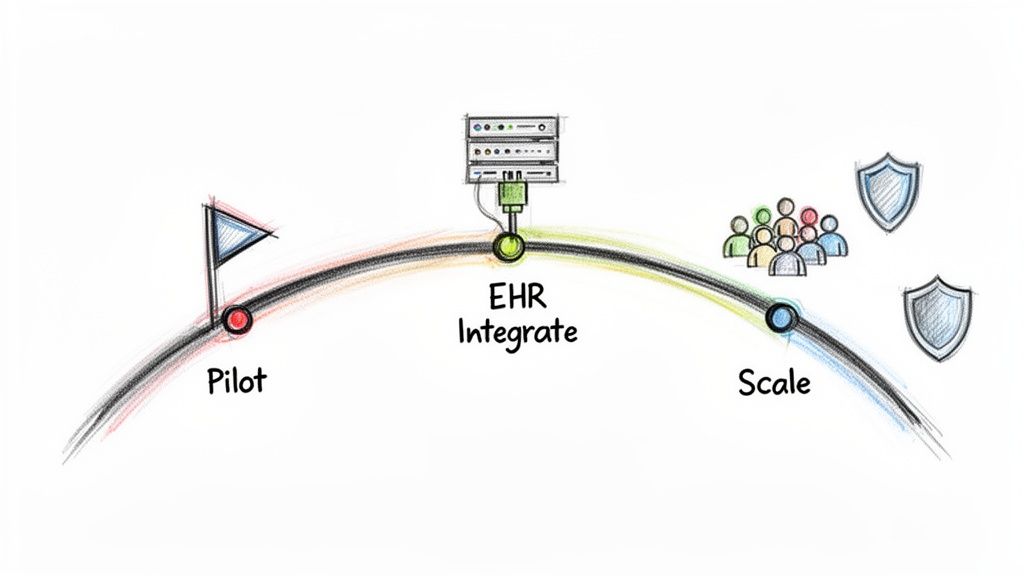
The very first move is to get specific. Vague goals like "improving patient communication" won't cut it. Instead, you need something you can actually measure, like "reduce our no-show rate by 15% in six months" or "automate 50% of our post-discharge follow-up calls." This kind of clarity will guide every single decision you make from here on out.
Phase 1: Define Your Goals and Figure Out What You Need
Before you even look at a single piece of technology, you have to get your own house in order. That means sitting down with your clinical, administrative, and IT teams to figure out precisely what you need the AI to do. This is all about asking the right questions to build a solid foundation.
Here’s what to dig into:
- Pinpoint High-Impact Problems: Where is the most friction in your patient’s journey right now? Is it the nightmare of scheduling appointments? Or maybe it’s poor medication adherence after they leave the hospital? Find one or two problems where AI can deliver a clear, undeniable win.
- Map Out Your Tech Needs: What systems does this AI absolutely have to talk to? Your EHR is the big one, of course, but don't forget about billing or pharmacy systems. Get this documented early, as it will be critical when you start talking to vendors.
- Check Your Data Readiness: What patient data does the AI need to be effective, and how will you get it there securely? This is a huge piece of the puzzle, touching on both functionality and compliance.
Phase 2: Launch a Focused Pilot Project
Once you know what you’re trying to solve, it's time to start small. Don't try to boil the ocean with a massive, system-wide deployment. That’s a recipe for failure. Instead, run a pilot project to test your concept in a controlled, real-world setting.
A great pilot project is narrow in scope but high in impact. Think about choosing a single department or a specific patient group—like automating appointment reminders just for cardiology patients. This lets you measure results and fine-tune everything before you even think about rolling it out more broadly.
This approach does two things beautifully. First, it minimizes disruption. Second, it builds a groundswell of support. When other departments see real, tangible results—like a lighter workload for your staff and happier patients—they’ll become your biggest champions. A structured approach, like our AI Product Development Workflow, is designed to guide you through this exact process, making the jump from pilot to production feel natural.
Phase 3: Nail Down Compliance and Integration
As you get ready to scale up, two things become non-negotiable: rock-solid security and seamless technical integration. In healthcare, these aren't just nice-to-haves; they are the absolute bedrock of any successful project.
Your AI solution must be HIPAA compliant, full stop. This means your vendor must be willing to sign a Business Associate Agreement (BAA) without hesitation.
Just as critical is a deep, functional integration with your Electronic Health Record (EHR) system. This AI can't live on an island. It needs to read data from the EHR (like appointment times) and write information back (like a confirmed visit or a patient's reported symptoms). This two-way street is what creates a single source of truth and really unleashes the power of automation.
Frankly, this is often the trickiest part of the whole implementation. It’s where you need real expertise. A good technology partner will have proven experience connecting with major EHRs, ensuring your new AI tool feels like a natural extension of the workflows your clinicians already use every day. Getting this technical foundation right is what separates the projects that succeed from those that fizzle out.
So, What's the Real ROI on This AI Stuff?
Getting the green light for a major tech investment means you have to talk dollars and sense. When it comes to patient engagement using conversational AI, proving that return on investment (ROI) goes way beyond just "we're saving a little money." You need a solid way to measure what's working, not just to get the initial sign-off, but to keep making your AI tools for business even better over time.
The best way I’ve seen this done is to break the ROI down into three separate but connected buckets. Each one tells a crucial part of the story, with its own numbers to back it up.
Are We Actually Making Things Run Smoother?
The first place you'll see a difference is in your team's daily grind. This is all about measuring the time and effort you get back by letting the AI handle the simple, repetitive tasks. The goal here is to prove that you’re freeing up your skilled staff to do the more human, high-touch work they were hired for.
Here’s what to keep an eye on:
- Less Phone Tag: How much has your call volume dropped for things like appointment confirmations, directions, or "can I get a refill?" inquiries? Track that percentage decrease.
- Time Back in Your Day: Think about all the hours spent on manual reminder calls, pre-op instructions, and post-visit check-ins. A quick calculation—(Avg. time per manual call) x (Number of AI interactions)—gives you a powerful "hours saved" metric.
- Quicker Rooming Times: Measure how long it takes to get a patient from the front desk into an exam room. When AI handles the forms digitally beforehand, that time shrinks.
These numbers give you a crystal-clear picture of how the technology is cutting down on busywork, making your team more productive, and even helping to take the edge off staff burnout.
Following the Money: Direct Financial Wins
Operational improvements are great, but leadership really lights up when they see the direct impact on the bottom line. This is where you connect the dots between the AI and your organization's financial health, focusing on both cutting costs and boosting revenue.
You can talk about efficiency all day, but the real financial muscle of conversational AI is its knack for plugging revenue leaks. Automating the simple stuff prevents no-shows and tightens up the whole payment process.
Key financial numbers to watch:
- The No-Show Killer: This one gets attention. Figure out how much revenue you’ve saved by reducing missed appointments. The math is simple: (Revenue per appointment) x (Number of appointments saved) = Revenue Recovered.
- A Healthier Revenue Cycle: Are you seeing fewer claim denials because the AI is capturing more accurate patient data upfront? Are payments coming in faster thanks to automated reminders? Track those improvements.
Is This Actually Helping Patients?
At the end of the day, it’s all about the patient. These results can feel a bit softer than hard dollar figures, but they are the bedrock of value-based care and what keeps patients coming back. This is where your investment in things like custom healthcare software development truly shows its worth.
Patient-focused metrics you can't ignore:
- Happier Patients: Keep a close eye on your Patient Satisfaction (CSAT) or Net Promoter Scores (NPS). A 10-15% jump in these scores after implementation is a huge win.
- Better Medication Adherence: For patients with chronic conditions, use the AI to track prescription refill rates and gather patient-reported data on how well they're sticking to their regimen.
- Fewer Readmissions: If you're using AI for post-discharge follow-up, a drop in 30-day hospital readmissions is one of the most powerful indicators that your proactive engagement is making a real clinical difference.
By tracking success across these three areas—operations, finance, and patient outcomes—you build a complete, undeniable story about your AI's value. This data-driven approach doesn't just justify the initial cost; it gives you the insights you need for ongoing AI strategy consulting to ensure the technology keeps delivering real results.
What's Next? Putting Your Patient Engagement Strategy into Action
We’ve covered a lot of ground, from defining conversational AI to mapping out specific use cases that can genuinely improve patient care and your bottom line. But understanding the potential is one thing; making it a reality is another. The real challenge—and opportunity—is moving from knowledge to decisive action.
Successful patient engagement using conversational AI isn't just about plugging in new software. It’s about being thoughtful and strategic, and that often means working with a partner who gets both the technology and the intricacies of healthcare. The future of patient interaction is already here—it's responsive, personal, and works around the clock. This means shifting away from old-school, reactive processes and embracing proactive, automated support. As we explored in our AI adoption guide, a clear plan is what separates a successful transition from a frustrating one.
From Big Idea to Real-World Impact
So, how do you turn your vision into a concrete plan? Whether you're ready to go all-in or just figuring out where to start, you need a clear path forward.
This is where having an expert partner makes all the difference. The right strategy connects your investment directly to your most pressing challenges, whether that’s slashing no-show rates, better supporting patients with chronic conditions, or simply freeing up your staff from repetitive tasks.
Here are a couple of ways to get started:
- Ready to jump in? A platform like our "AI Automation as a Service" offers tools you can deploy right away for immediate, high-impact results.
- Need a detailed plan first? A Custom AI Strategy report can give your leadership team the clear, data-driven roadmap they need to move forward with confidence.
Building a Foundation of Trust
At the end of the day, any AI initiative lives or dies on trust. Your patients need to trust that the interaction is helpful and secure. Your internal teams need to trust that the technology makes their jobs easier, not harder.
That trust is built by pairing smart, reliable technology with deep expertise. It’s about making sure every automated conversation is not just efficient, but also safe, compliant, and genuinely empathetic.
We believe in starting with a thorough AI requirements analysis and working together transparently all the way through deployment. This is a big step toward creating a more connected and engaged patient community, but you don't have to take it alone. Get to know our expert team—we’re ready to talk about your specific goals and how to achieve them.
Frequently Asked Questions
When you're considering bringing conversational AI into your patient engagement strategy, a few critical questions always come up. Let's walk through the most common ones healthcare leaders ask about security, integration, and what happens day-to-day.
How Can We Be Sure Conversational AI is HIPAA Compliant?
This is the big one, and rightly so. Protecting patient data isn't just a priority; it's a legal and ethical mandate. Any reputable conversational AI platform built for healthcare operates on a foundation of security. Think of it like a digital fortress.
This includes end-to-end encryption for all data, both when it's moving and when it's stored. It also means strict access controls and detailed audit logs that track every interaction. Before you partner with any vendor, you must have a signed Business Associate Agreement (BAA) in place, and you need to dig into their data protocols to ensure they meet every HIPAA requirement.
A crucial point is that Protected Health Information (PHI) should never be used to train general AI models. The system must be designed to keep this sensitive data completely isolated and secure unless it's properly de-identified, which is a cornerstone of any trustworthy healthcare AI.
Will This AI Actually Work with Our EHR?
Yes, it absolutely has to. Without a solid connection to your Electronic Health Record (EHR) system, the AI is just a chatbot in a silo. The goal is seamless integration, which is usually handled through secure APIs.
A good integration means the AI can read necessary information (like open appointment slots) and write data back (like a newly scheduled visit). This creates a single, reliable source of truth and prevents staff from having to manually update multiple systems. When you're vetting potential partners, their experience integrating with major EHRs like Epic, Cerner, or Allscripts should be at the top of your checklist.
How Long Does It Realistically Take to Get a Pilot Running?
You can get a pilot off the ground faster than you might think. For a well-defined use case like appointment scheduling, a typical timeframe is about 6 to 12 weeks.
That window covers everything from initial planning and technical setup to the EHR integration, designing the conversational flow, testing, and getting your team up to speed. Kicking off with a focused pilot is the smart move—it lets you demonstrate real value quickly and learn valuable lessons before you expand to other areas.
What Happens When the AI Gets a Question It Can’t Answer?
This is a key part of the design. No AI knows everything, and it shouldn't pretend to. A well-built system knows its own limits.
When a patient asks something too complex, sensitive, or that requires a clinical opinion, the AI is programmed to escalate it. This isn't a failure; it's a feature. The system will perform a smooth handoff to the right person—a nurse, a scheduling coordinator, or another staff member—through a secure message, a phone call, or by creating a task in your team's workflow. This "human-in-the-loop" approach ensures patients get the care they need and your team's time is used for the moments that matter most.
Ready to transform your patient engagement strategy? Ekipa AI provides the expertise and tools to turn your vision into reality. Start building a more connected, efficient, and patient-centric healthcare experience today by exploring our AI Strategy consulting tool.