AI for Medical Diagnosis Explained
Discover how AI for medical diagnosis is transforming healthcare. This guide explains key technologies, real-world applications, and strategic implementation.
When we talk about using AI for medical diagnosis, we're talking about algorithms and machine learning that dig into complex medical data. The goal is simple: help doctors and specialists identify diseases faster, earlier, and with more accuracy.
Think of AI as an incredibly sharp analytical partner. It can spot subtle patterns in images, records, and even genetic information that are often invisible to the human eye. This directly translates to better patient outcomes and a more efficient healthcare system.
How AI Is Reshaping Medical Diagnosis
Let's clear the air: this isn't about robot doctors taking over. The reality of AI for medical diagnosis is far more collaborative and grounded. It’s not about replacing a physician's expertise but enhancing it with powerful tools that can see what we can’t.
AI algorithms are built to process enormous datasets. They can sift through thousands of CT scans, cross-reference genetic markers, and analyze years of patient histories to find correlations and red flags that point to potential health problems.
This isn't some far-off future concept; it's happening now. A staggering 89% of healthcare executives globally already report using artificial intelligence in some capacity.
Enhancing Clinical Precision and Speed
At its core, AI brings pattern recognition to a scale humans simply can't match. This has a few game-changing effects:
- Earlier Detection: AI can find microscopic signs of disease in medical images long before they become obvious to a radiologist, opening the door for much earlier and more effective treatment.
- Increased Accuracy: By offering a data-backed "second opinion," AI helps reduce the risk of human error or confirmation bias. The result is a more precise diagnosis.
- Personalized Insights: AI can look at a patient's unique genetic code and lifestyle data to predict disease risk, suggesting truly personalized diagnostic paths.
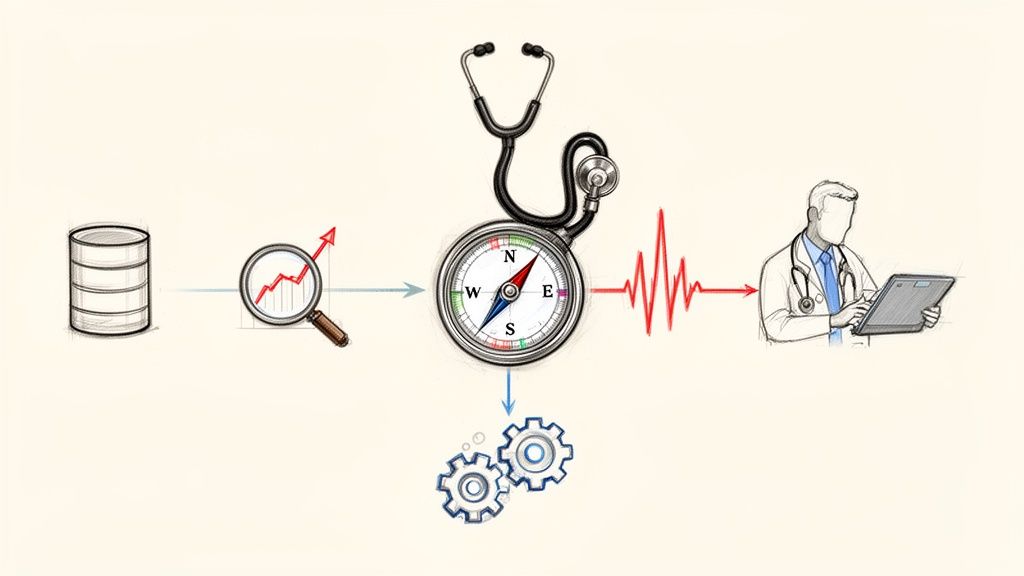
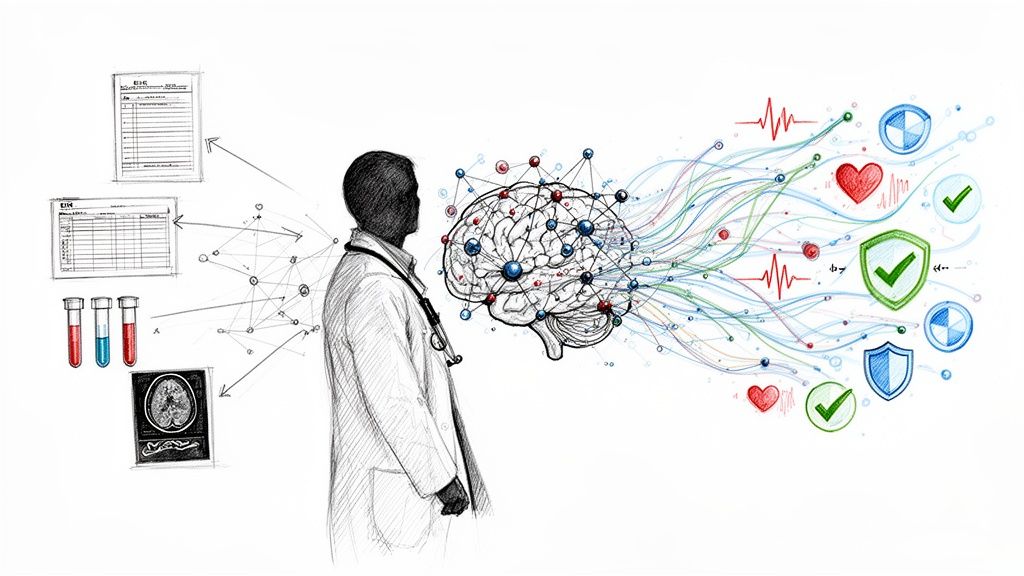
This image really captures the essence of how AI works alongside a doctor, pulling together different streams of patient data to form a complete picture.
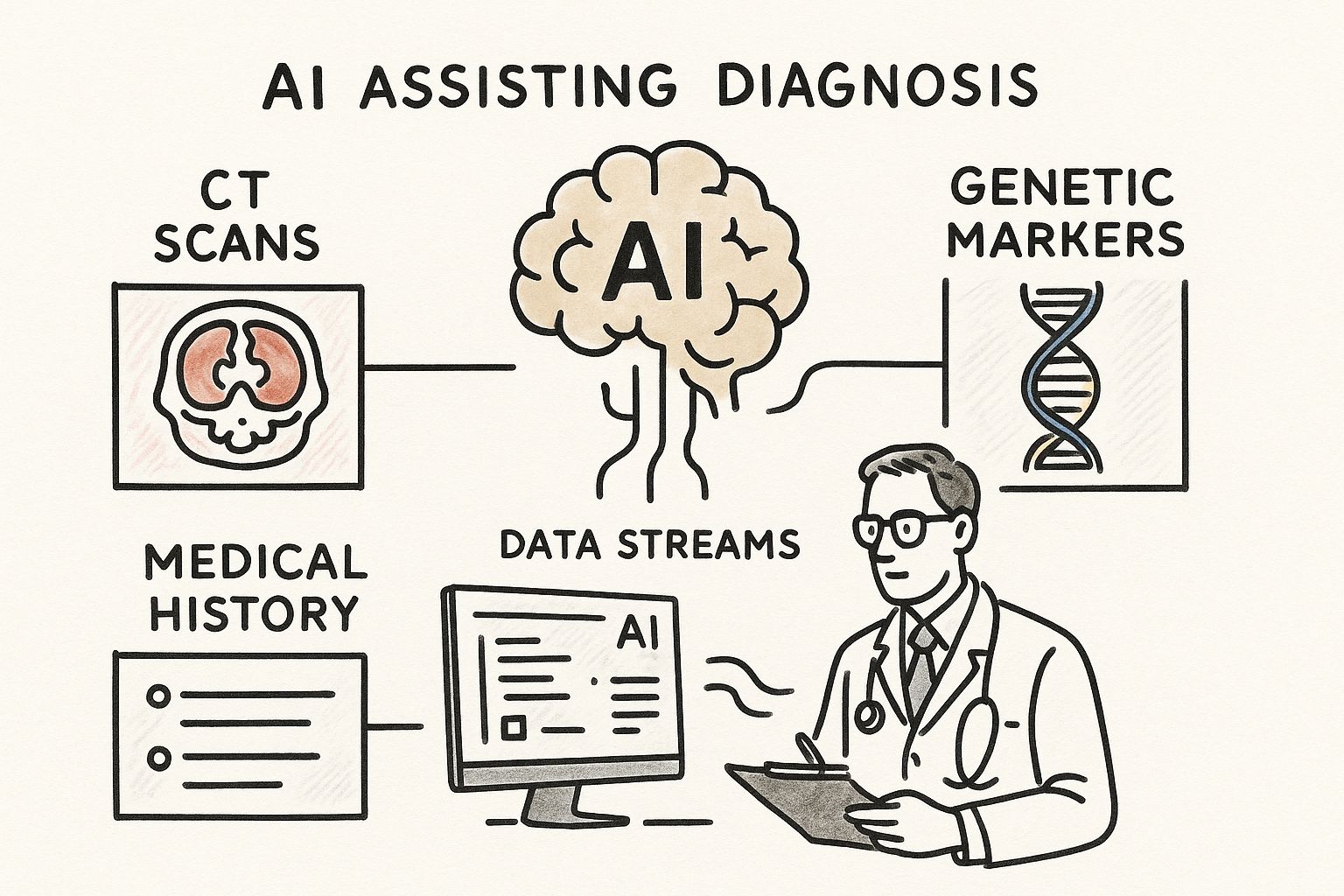
You can see how the AI acts as a powerful partner, making sense of all that complex information so the clinician can make the best possible call.
By processing vast and varied datasets simultaneously, AI provides a multidimensional view of patient health, moving diagnostics from a reactive to a proactive discipline.
This shift is already underway in hospitals all over the world. Our specialized work in AI applications in the healthcare industry shows just how practical these advancements have become. For a deeper look at a specific field, you can see real-world examples of AI-driven diagnostics in physical therapy. The change is here, and it’s fundamentally altering how we understand and fight disease.
The Engines of Diagnostic AI
To really get a handle on how AI works in medical diagnosis, you have to look past the hype and understand the actual technology making it happen. It's not some black box. It's a collection of powerful, data-driven tools, and knowing what they are and what they do is the first step in seeing how AI goes from an idea to a real-world clinical asset.
The foundation of nearly all diagnostic AI is Machine Learning (ML). The best way to think about it is like training a new medical resident. You don’t just hand them a textbook and wish them luck. You immerse them in real-world cases, showing them thousands of X-rays, patient charts, and lab results.
Slowly but surely, that resident learns to connect the dots, spot subtle anomalies, and make sound judgments. ML algorithms do the exact same thing, just at a scale and speed that humans can't match. They’re fed massive datasets of medical information until they can pinpoint patterns linked to specific diseases with incredible accuracy. This is the bedrock of many modern AI Solutions.
Deep Learning: Going Beyond the Obvious
If Machine Learning is the resident, then Deep Learning (DL) is the seasoned specialist who’s developed an almost gut-level instinct for their work. Deep Learning is a more advanced form of ML that uses structures called neural networks, which are loosely inspired by the wiring of the human brain.
These networks have layers upon layers of "neurons," which allows them to learn from data in a much deeper, more abstract way. For instance, you don't have to tell a Deep Learning model what specific features to look for in a CT scan. It can teach itself to identify the faint textures, shapes, and gradients that might signal a growing tumor—details that might be missed by the human eye.
Natural Language Processing: Finding Clues in a Patient’s Story
Think about all the crucial information locked away in unstructured text—doctors' notes, pathology reports, patient histories. So much of a patient's story is written out, not neatly filed in a database. This is where Natural Language Processing (NLP) steps in.
NLP is the technology that gives AI the ability to read and understand human language. In diagnostics, this is a massive leap forward. An NLP algorithm can sift through millions of clinical reports to find correlations between certain phrases and patient outcomes, or it can pull key symptoms from a doctor's narrative to help piece together a diagnosis.
By transforming messy, unstructured text into clean, actionable data, NLP gives us access to a goldmine of diagnostic insights that were previously impossible to analyze at scale.
This is absolutely essential for building effective internal tooling and making clinic workflows more efficient. As we explored in our AI adoption guide, getting a handle on your data is always the first step.
To put it all together, let’s look at a quick comparison of these core technologies and how they’re actually used in a clinical setting.
Key AI Technologies in Medical Diagnosis
| AI Technology | Core Function | Example Diagnostic Application |
|---|---|---|
| Machine Learning (ML) | Learns patterns from labeled data to make predictions. | Predicting a patient's risk of developing heart disease based on their health records and lifestyle factors. |
| Deep Learning (DL) | Uses multi-layered neural networks to learn from vast, raw datasets. | Analyzing thousands of retinal scans to detect signs of diabetic retinopathy earlier than human experts. |
| Natural Language Processing (NLP) | Understands and interprets human language from text and speech. | Extracting key patient symptoms and medical history from unstructured doctors' notes to support a diagnosis. |
As you can see, each of these technologies plays a unique but often complementary role. They are the fundamental AI tools for business that empower healthcare professionals to make faster, more accurate decisions.
Once you understand what each tool does, it becomes much easier to build a smart adoption plan. A clear vision, backed by solid AI strategy consulting, is what ensures these powerful technologies are actually put to work in a way that truly improves patient care.
How AI Fits Into the Day-to-Day Clinical Workflow
Bringing AI for medical diagnosis into a hospital isn't about ripping out existing systems and starting from scratch. It’s more subtle and, frankly, much smarter than that. The real goal is to embed intelligent tools directly into the daily routines of healthcare professionals, making their existing workflows more efficient and powerful. It’s about augmenting their expertise, not replacing it.
Imagine an AI algorithm working quietly in the background of a radiology department. It scans a lung CT and instantly flags suspicious nodules, highlighting them for the radiologist. But it doesn't stop there. The system can intelligently re-prioritize the entire worklist, bumping the most urgent cases to the top of the queue. This small change means critical patients get a diagnosis faster, which can directly improve their outcome.
This kind of seamless integration is happening across the entire diagnostic journey, not just in the imaging suite.
From Tedious Data Entry to Powerful Predictive Insights
The true magic of AI in clinical workflows is its ability to handle the cognitive heavy lifting and spot patterns that are nearly invisible to the human eye. It acts like a tireless assistant, taking over repetitive tasks so clinicians can dedicate their brainpower to complex decisions and patient care.
For example, newer systems can pull key information from unstructured, free-text patient notes automatically. This frees up doctors from the soul-crushing task of manual data entry, a key benefit of smart workflow automation. The result? Clinicians can spend more time actually talking to their patients and less time wrestling with paperwork.
But it goes way beyond simple automation. These tools offer a glimpse into the future:
- Genomic Analysis: AI can chew through massive genetic datasets to find the one rare mutation linked to a specific disease—a job that could take a human researcher years.
- Disease Progression Forecasting: By looking at a patient's data over time, predictive models can forecast how a chronic illness might progress, paving the way for proactive treatment.
- Risk Stratification: Algorithms can identify patients at the highest risk for developing conditions like sepsis or suffering a cardiac arrest, allowing medical teams to intervene early and save lives.
Making these integrations work requires thoughtful healthcare software development that ensures AI tools fit neatly into a hospital's specific operational needs.
The Rise of Specialized Diagnostic Assistants
In certain fields, the accuracy of these AI-powered systems is already staggering. CognoSpeak, for instance, is an AI tool that can detect early signs of Alzheimer’s disease just by analyzing speech patterns, achieving an impressive 90% identification rate.
In oncology, AI precision medicine tools now generate 31% of the revenue, a testament to how central they've become in creating personalized cancer treatments.
By handling the data-heavy lifting, AI gives clinicians the mental space to focus on what matters most: interpreting complex cases, communicating with patients, and applying their years of experience to make the final call.
This collaborative model is where medicine is headed. A great real-world example is the development of a clinic AI assistant, a piece of internal tooling designed to manage appointments, transcribe consultations, and even offer real-time decision support. It's a perfect illustration of how technology can empower clinicians and improve the patient experience all at once.
Real-World Examples of Diagnostic AI in Action
The real test of any new technology isn’t in a lab; it’s in the clinic, with real patients. When we talk about AI for medical diagnosis, we're not discussing far-off concepts. We’re seeing practical tools being used today that are making a genuine, life-saving difference.
Let's move past the theory and look at a few powerful examples of how this technology is actually working in hospitals and specialty practices right now.
Uncovering Early-Stage Lung Cancer in Radiology
The great challenge with lung cancer is that it's often silent. By the time a patient feels symptoms, the disease has usually progressed to a dangerous stage. Catching it early is everything, but spotting a tiny, developing tumor on a CT scan is like finding a needle in a haystack for a busy radiologist.
This is where AI is making a massive impact. Algorithms, trained on millions of past CT scans, can meticulously analyze every pixel of an image. They act as a hyper-vigilant assistant, flagging subtle nodules or faint growths that the human eye might overlook. The AI doesn’t make the diagnosis; it draws the expert’s attention directly to the most critical areas.
The results are stunning. Studies have shown that AI-assisted screening can boost the early detection rate of lung cancer by as much as 30%. This means more diagnoses are happening at Stage I or II, where treatment is far more likely to be successful.
It's not just about finding more; it's about working smarter. By pre-screening scans, AI helps radiologists prioritize their efforts on the most suspicious cases, cutting down on backlogs and delivering answers to anxious patients much sooner.
Differentiating Moles from Melanoma in Dermatology
Dermatologists are experts at visually identifying suspicious skin lesions, but the sheer volume of cases can be overwhelming. Telling a harmless mole from an early-stage melanoma is a high-stakes judgment call that often ends in a biopsy—a necessary but invasive step.
AI is providing a powerful, non-invasive first look. Deep learning models have been trained on huge image libraries of both benign and malignant skin lesions. These tools can analyze a smartphone photo of a mole, assessing its asymmetry, border, color, and other key traits with remarkable accuracy.
This technology is already helping in a few key ways:
- Smarter Triage: It helps primary care doctors quickly identify high-risk patients who need an immediate referral to a specialist.
- Fewer Unnecessary Biopsies: A reliable risk score from an AI tool gives clinicians more confidence to "watch and wait" on lesions that are clearly benign.
- Greater Access: Because the tech can run on a smartphone, it has the potential to bring expert-level screening to people in rural or underserved areas.
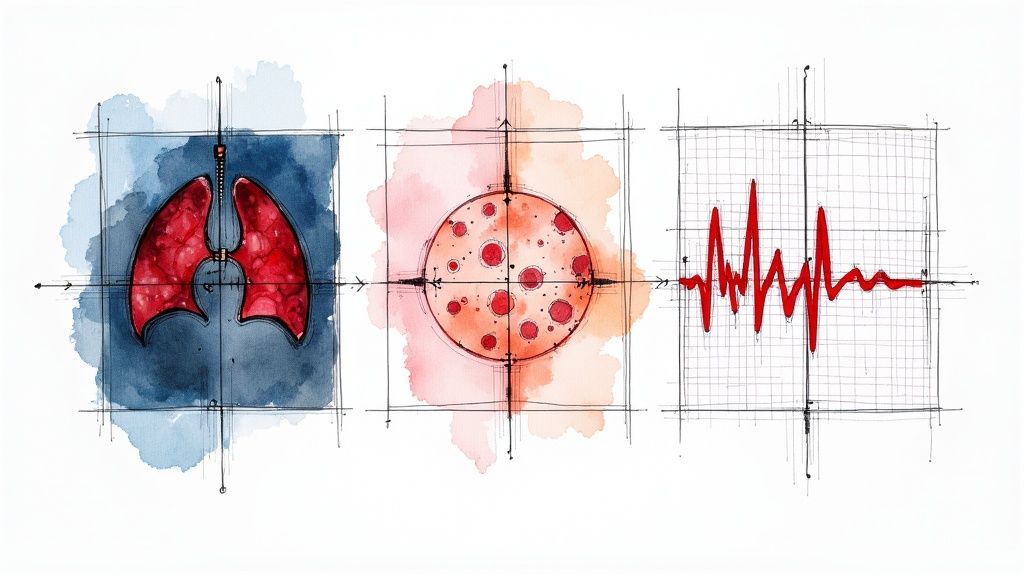
Predicting Cardiac Events Before They Happen
In cardiology, prevention is the ultimate goal. A heart attack that never happens is a far better outcome than one that's treated in the emergency room. While traditional risk factors give us a good general idea of who's in danger, they don’t always tell the full story for an individual.
AI is making cardiac risk assessment incredibly personal. New algorithms can comb through electrocardiogram (ECG) data, detecting tiny electrical fluctuations and hidden patterns that are invisible to the human eye. These subtle signals can be strong predictors of future problems like atrial fibrillation or even sudden cardiac death.
This gives cardiologists a chance to get ahead of the problem. Armed with this deeper insight, they can intervene earlier with lifestyle changes, preventative medication, or closer monitoring. It represents a fundamental shift from reacting to a crisis to proactively stopping one from ever happening, all by finding the quiet signals hidden in the noise of cardiac data.
Navigating the Challenges and Ethical Hurdles
While the promise of AI for medical diagnosis is enormous, getting it into the clinic isn't as simple as installing new software. Adopting this technology responsibly means we have to tackle some pretty big challenges and ethical questions head-on. These aren't just roadblocks; they're critical issues that require careful planning, real expertise, and a firm commitment to keeping patients safe and care equitable.
One of the biggest concerns right out of the gate is algorithmic bias. An AI is only as smart as the data it learns from. If that data overwhelmingly represents one demographic, the tool might not work well for patients from different backgrounds, which could actually make health disparities worse. This is a core reason why our AI strategy consulting services emphasize a thoughtful, risk-aware approach from the very beginning.
Ensuring Data Privacy and Security
It goes without saying that patient data in healthcare is incredibly sensitive. Using AI means handling huge volumes of this information, which naturally rings alarm bells for privacy. A single data breach could expose thousands of confidential health records, shattering patient trust and causing real harm.
Because of this, rock-solid security isn't just a "nice-to-have"—it's an absolute must. Key measures include:
- Anonymization: Systematically stripping all personal identifiers from data before it's ever used to train an AI model.
- Secure Infrastructure: Using top-tier encryption and strict access controls to guard data, whether it's stored or being transmitted.
- Compliance: Following regulations like HIPAA to the letter, ensuring every single step of data management is legally sound.
The Black Box Problem and Regulatory Oversight
Another significant hurdle is what we call the "black box" problem. Some of the most powerful AI models, especially in deep learning, can be a bit of a mystery. They might give a highly accurate diagnosis, but doctors—and their patients—can't always see how the AI reached its conclusion. This lack of transparency can make it tough for clinicians to fully trust and verify the AI's output.
This issue brings up a crucial question: who's accountable when an AI-assisted diagnosis is wrong? Is it the developer who built the algorithm, the hospital that deployed it, or the doctor who followed the recommendation? These are thorny legal and ethical questions that don't have simple answers.
On top of all this, regulatory bodies are still catching up. Any AI tool used for diagnosis, particularly if it's considered Software as a Medical Device (SaMD), must pass a high bar. Navigating that landscape is essential. You can get a sense of the general requirements by reading up on the FDA approval process for medical devices.
A recent large-scale analysis put some numbers to these concerns, finding that generative AI models hit a diagnostic accuracy of 52.1%. That's on par with non-expert doctors, but it's also 15.8% lower than human experts. It helps explain why even though 66% of physicians are already using AI in some capacity, many are still wary of potential errors and bias. You can explore the full findings over at Nature.com. The key is to see these challenges not as stop signs, but as solvable problems on the path to successful, ethical implementation.
Building Your AI Diagnostic Implementation Plan
Making the leap from understanding what AI can do in medical diagnosis to actually putting it to work requires a thoughtful, strategic plan. A successful rollout isn't about grabbing the latest shiny technology; it’s about systematically solving a real clinical problem to make patient care better and your operations smoother. Everything has to start with a clear purpose.
The first, and most important, step is to zero in on a specific, high-impact diagnostic challenge. Don't ask, "Where can we use AI?" Instead, ask, "What's our biggest diagnostic bottleneck or most common source of error?" Maybe it's the long wait times for radiology reports or the struggle to improve early sepsis detection in the ICU. When you start with a well-defined problem, your AI project is set up to deliver real value right away.
Laying the Groundwork for Success
Once you’ve identified your target, the focus needs to shift to your most important assets: your data and your people. AI models are only ever as good as the data they learn from. This means you need a large, high-quality, and diverse dataset that’s clean, well-organized, and truly reflects the patients you serve.
At the same time, you have to get everyone working together. An AI project built in a silo is doomed to fail. It absolutely requires a partnership between clinicians, who bring the deep medical context, and data scientists, who understand the technology inside and out. Building these cross-functional teams ensures the final tool is both technically robust and genuinely useful in a clinical setting, which is the key to building trust from the very beginning. This collaborative approach is at the heart of a solid AI Product Development Workflow.
A successful AI strategy is built on purpose, not platforms. It starts by identifying a genuine clinical need and then assembling the right data, people, and processes to solve it effectively.
From Pilot to Full-Scale Integration
With a clear problem and the right foundation in place, you’re ready to launch a pilot project. Think of this as a small-scale test run—your chance to prove the concept works, smooth out any technical wrinkles, and show the AI's value to stakeholders who might be a bit skeptical. Pick a controlled environment where you can keep a close eye on performance and get direct feedback from clinicians.
A successful pilot needs to hit clear, predefined goals, like boosting diagnostic accuracy by a certain percentage or slashing report turnaround times. Once you have those proven results in hand, you can build a roadmap for scaling the solution across the entire organization. This is about more than just a wider technical rollout; it demands careful change management, comprehensive staff training, and ongoing monitoring to make sure the tool is adopted and used correctly.
Structured services can make this phased approach much more manageable. For instance, AI Automation as a Service can help weave the new tool into your existing hospital systems, while a detailed Custom AI Strategy report can give you a clear, step-by-step guide for expansion. The ultimate goal is to build a system that enhances the clinical environment, not disrupts it.
For organizations ready to build their own roadmap, the first step is to connect with our expert team to translate your clinical needs into a viable, impactful AI implementation plan.
Frequently Asked Questions (FAQ)
Let's tackle some of the most common questions that come up when we talk about bringing AI into the world of medical diagnosis.
Will AI replace doctors and radiologists?
That’s probably the biggest question on everyone’s mind, and the short answer is no. The consensus among people working in this field is that AI will augment, not replace, medical professionals. Think of it less as an artificial replacement and more as ‘augmented intelligence.’ AI is brilliant at sorting through massive amounts of data and flagging things a human might miss, but it can’t replicate a doctor's critical thinking, empathy, or holistic judgment. The real power comes from combining the machine's precision with human expertise.
How accurate is AI compared to human doctors?
This really depends on the specific job. For certain, highly focused tasks—like scanning thousands of medical images for early signs of cancer or diabetic retinopathy—the best AI models can perform on par with, or sometimes even better than, a human expert. This is where we're seeing some of the most exciting real-world use cases emerge. However, when a diagnosis is more complex and requires a deep understanding of a patient's history and other contextual clues, AI often performs more like a junior clinician. The gold standard is, and will likely remain, a partnership: AI provides the initial analysis, but a seasoned physician makes the final call.
What is the first step for a hospital to implement diagnostic AI?
The first move should always be about strategy, not technology. Before you even think about vendors or algorithms, you need to pinpoint a specific, high-impact clinical problem you want to solve. Are you trying to cut down on diagnostic errors in a particular department? Or maybe speed up lab results with workflow automation? Once you have a clear goal, you can look at your data readiness and launch a small, focused pilot project. This is the best way to prove the tool's value and get clinicians on board before you even consider a large-scale rollout. A Custom AI Strategy report can help map this out, giving you a clear path forward. If you want to talk through your own situation, our expert team is here to help you build that initial roadmap.
Ready to see what this could look like in your organization? At Ekipa AI, we help turn these strategic ideas into real-world, scalable solutions. Our expert team is ready to guide you. Let's explore how we can bring your AI vision to life. Explore Our AI Solutions