Top Artificial Intelligence Examples in Healthcare for 2025
Discover key artificial intelligence examples in healthcare transforming medicine in 2025. Explore innovative AI applications shaping the future of healthcare.
Artificial intelligence is no longer a futuristic concept in medicine; it's a present-day reality actively reshaping patient care, diagnostics, and operational efficiency. The healthcare industry is witnessing a profound shift, moving from theoretical AI models to practical, high-impact applications that deliver tangible results. For a comprehensive overview of how artificial intelligence is transforming the medical sector, explore discussions specifically on the role of AI in Health Care And Social Assistance. This transformation is creating unprecedented opportunities for innovation and improvement across the entire healthcare value chain.
This article moves beyond surface-level descriptions to provide a strategic breakdown of real-world artificial intelligence examples in healthcare. We will dissect specific use cases, from AI-powered diagnostic imaging to predictive analytics that forecast patient outcomes. For each example, you will find a detailed analysis of the underlying strategy, tactical insights you can apply, and actionable takeaways for implementation. This is not just a list of what's possible; it’s a playbook designed for leaders looking to understand the mechanics behind successful AI integration. As we explored in our AI adoption guide, the key is a strategic approach. We will explore how these technologies are not just enhancing existing processes but creating entirely new models for drug discovery, personalized medicine, and operational workflow automation.
1. Medical Image Analysis and Diagnostics
Medical image analysis represents one of the most impactful artificial intelligence examples in healthcare, transforming how clinicians interpret complex visual data. This technology uses advanced deep learning algorithms, specifically Convolutional Neural Networks (CNNs), to analyze medical images like X-rays, CT scans, and MRIs. These AI systems are trained on vast datasets of labeled images, learning to identify subtle patterns indicative of diseases that might be missed by the human eye.
The goal isn't to replace radiologists but to augment their capabilities, acting as a powerful second opinion or a preliminary screening tool to prioritize urgent cases. For example, Google's DeepMind can detect over 50 eye diseases from retinal scans with accuracy rivaling leading specialists. Similarly, companies like Zebra Medical Vision and Aidoc have developed FDA-cleared solutions that flag critical abnormalities in real-time, dramatically speeding up diagnoses in emergency settings. This fusion of human expertise and machine precision leads to earlier detection, reduced diagnostic errors, and more efficient workflows.
Strategic Breakdown & Key Benefits
The following infographic highlights the core benefits of integrating AI into medical imaging workflows, showing quantifiable improvements in accuracy, speed, and availability.
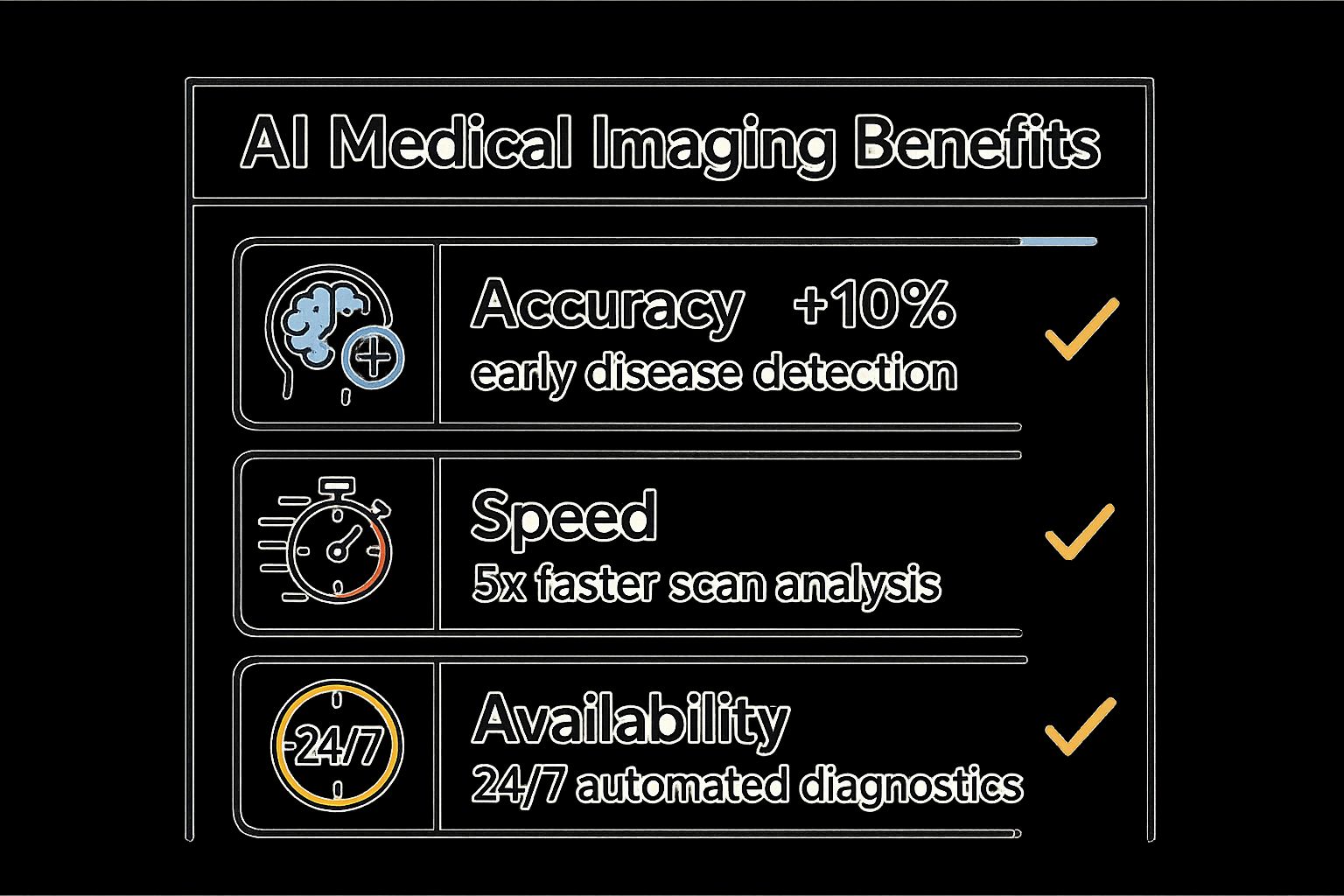
As the data shows, the strategic advantage lies in enhancing diagnostic capabilities across the board, from improving early detection rates to providing round-the-clock support for clinical teams.
Actionable Takeaways
Implementing this technology requires a measured, strategic approach to ensure seamless integration and clinical validation.
- Start with a Focused Pilot: Begin with a specific department, like emergency radiology, to validate the AI's performance and measure its impact on workflow efficiency before a full-scale rollout.
- Prioritize Clinician Training: Ensure radiologists and technicians are thoroughly trained not just on how to use the tool, but on understanding its strengths and limitations.
- Establish Human-in-the-Loop Protocols: Maintain that a qualified clinician makes the final diagnosis. The AI's role is to assist, not to have ultimate authority. Platforms specializing in medical image analysis, like Diagnoo, are built with this collaborative framework in mind. Learn more about intelligent diagnostic tools on ekipa.ai.
2. Drug Discovery and Development
Accelerating pharmaceutical research is another of the most transformative artificial intelligence examples in healthcare. This application leverages machine learning and predictive analytics to dramatically shorten the drug development pipeline. AI algorithms analyze massive datasets of genetic information, molecular structures, and clinical trial results to identify promising drug candidates, predict their efficacy, and optimize their chemical composition, a process that traditionally takes over a decade.
The primary objective is to make drug discovery faster, cheaper, and more effective. AI can predict how a molecule will behave and its potential side effects before it ever reaches a lab, saving immense resources. For example, DeepMind's AlphaFold has revolutionized biology by predicting protein structures with incredible accuracy, opening new avenues for targeted drug design. Similarly, companies like Atomwise and Exscientia use their AI platforms to screen billions of compounds, leading to AI-designed drugs entering human clinical trials in record time.
Strategic Breakdown & Key Benefits
The strategic application of AI in this domain shifts the paradigm from trial-and-error to a data-driven, predictive model. This significantly de-risks the early stages of development and focuses investment on the most viable candidates.
The core benefits are a direct response to the industry's biggest challenges: high costs, long timelines, and a high failure rate. By automating complex analysis and providing predictive insights, AI offers a clear path to a more efficient and successful R&D process. This also opens doors for personalized medicine by identifying drug targets for rare diseases or specific patient subpopulations. Custom healthcare software development plays a key role in building the platforms needed for this research.
Actionable Takeaways
Integrating AI into the pharmaceutical R&D workflow requires a foundational investment in data infrastructure and cross-disciplinary expertise.
- Invest in High-Quality Datasets: The predictive power of an AI model is entirely dependent on the quality and diversity of its training data. Secure and structure vast biological, chemical, and clinical datasets.
- Focus on a Specific Therapeutic Area: Start by applying AI to a single disease or drug class. This allows your team to build expertise and validate the technology's ROI before expanding to other R&D areas.
- Foster Human-AI Collaboration: The most successful outcomes arise from combining AI's computational power with the intuition of experienced pharmacologists and chemists. Design a collaborative AI Product Development Workflow where AI generates hypotheses and human experts validate and refine them.
3. Virtual Health Assistants and Chatbots
Virtual health assistants are a prime example of how artificial intelligence examples in healthcare are improving patient engagement and accessibility. These AI-powered conversational tools use natural language processing (NLP) to understand patient queries and provide instant, 24/7 support. They can handle tasks like symptom assessment, medication reminders, appointment scheduling, and answering basic health questions, acting as a first line of contact for non-emergency issues.
The primary goal is to triage patient needs efficiently, freeing up clinical staff to focus on more complex cases while ensuring patients receive timely guidance. For instance, platforms like Ada Health and Buoy Health offer sophisticated symptom checkers that guide users through a series of questions to suggest potential causes and recommend appropriate next steps, such as seeing a doctor or self-care. This technology enhances patient experience by providing immediate answers and reduces the administrative load on healthcare providers, leading to more streamlined and efficient operations.
Strategic Breakdown & Key Benefits
The strategic value of virtual assistants lies in their ability to scale patient support and improve operational efficiency. By automating routine interactions, healthcare organizations can better manage patient flow and resource allocation. This approach simultaneously empowers patients to take a more active role in managing their health with accessible, on-demand information and support.
The integration of these AI tools creates a more responsive and patient-centric healthcare model, where initial triage and routine queries are handled instantly. This not only improves patient satisfaction but also allows clinical teams to dedicate their valuable time to direct patient care and complex medical decisions, optimizing the entire care delivery process.
Actionable Takeaways
Deploying a virtual health assistant requires careful planning to ensure it is both effective and safe for patient use.
- Define a Clear Scope: Clearly communicate the assistant's capabilities and limitations to users. Emphasize that it is a support tool, not a replacement for professional medical advice.
- Implement Robust Escalation Protocols: Create a seamless and reliable pathway for escalating conversations to a human provider when the AI detects a potentially serious condition or cannot address the user's query.
- Ensure Data Privacy and Compliance: Build the assistant on a HIPAA-compliant framework with end-to-end data encryption to protect sensitive patient health information. Platforms like Clinic AI Assistant are designed with these security protocols in mind. Learn more about intelligent clinic assistants on ekipa.ai.
4. Predictive Analytics for Patient Outcomes
Predictive analytics is one of the most proactive artificial intelligence examples in healthcare, enabling providers to shift from reactive to preventive care. This technology leverages machine learning algorithms to analyze vast datasets, including electronic health records (EHRs), real-time vital signs, and genetic information. By identifying subtle patterns and correlations within this data, these systems can forecast future health events, such as disease onset, patient deterioration, or hospital readmissions.
The goal is to empower clinical teams with foresight, allowing them to intervene before a patient's condition becomes critical. For instance, Johns Hopkins' real-time TREWS system predicts sepsis development hours earlier than traditional methods, significantly improving survival rates. Similarly, Google Health's AI model can forecast acute kidney injury up to 48 hours in advance, providing a crucial window for preventive action. This forward-looking capability transforms population health management and personalizes patient care at scale.
Strategic Breakdown & Key Benefits
The strategic application of predictive analytics focuses on early intervention and resource optimization. By identifying high-risk patients, healthcare systems can allocate clinical resources more effectively, improve patient safety, and reduce costly emergency interventions. The key is moving from a one-size-fits-all approach to a data-driven, personalized care model that anticipates patient needs. This proactive stance is essential for value-based care.
The core benefits include enhanced patient outcomes through early warnings, reduced hospital readmission rates, and optimized staff and resource allocation. This leads to both better care quality and significant operational cost savings.
Actionable Takeaways
Integrating predictive analytics requires a strong data foundation and a clear strategy for turning predictions into clinical action.
- Ensure Data Quality and Integrity: Start by standardizing and cleaning data from disparate sources like EHRs and wearable devices. High-quality, comprehensive data is the bedrock of accurate predictive models.
- Validate Models Across Diverse Populations: Rigorously test and validate algorithms against different patient demographics to eliminate bias and ensure the model performs reliably across your entire patient population.
- Establish Clear Clinical Protocols: Develop clear, actionable protocols for clinicians to follow when the AI flags a high-risk patient. The prediction is only valuable if it triggers a standardized, effective intervention. This requires a well-defined workflow automation strategy to ensure alerts are handled consistently.
5. Robotic Surgery and Surgical Assistance
AI-powered robotic surgery is one of the most advanced artificial intelligence examples in healthcare, revolutionizing the operating room. This technology combines robotics with AI to enhance a surgeon's capabilities, enabling them to perform minimally invasive procedures with unparalleled precision, stability, and control. AI algorithms provide real-time guidance, eliminate natural hand tremors, and offer enhanced 3D visualization, which are critical in delicate operations.
The primary role of these systems is to augment, not replace, the surgeon. Systems like Intuitive Surgical's da Vinci platform translate a surgeon's hand movements into smaller, more precise movements of tiny instruments inside the patient's body. Others, like Medtronic's Hugo and Stryker's Mako, assist in everything from complex cardiac procedures to orthopedic joint replacements. This synergy of human skill and AI precision leads to smaller incisions, reduced blood loss, shorter hospital stays, and faster recovery times for patients.
Strategic Breakdown & Key Benefits
Integrating AI-assisted robotics into surgery introduces a new paradigm of precision and data-driven performance. The core benefits extend beyond the operating table to impact hospital efficiency and patient outcomes system-wide.
The strategic advantage is clear: leveraging machine precision to enhance human expertise, resulting in safer procedures, better outcomes, and a wealth of data that can be used to refine surgical techniques and training protocols for continuous improvement.
Actionable Takeaways
Successfully implementing robotic surgery systems requires significant capital investment and a long-term strategic commitment to training, maintenance, and process integration.
- Start with Less Complex Procedures: Begin deployment in procedures where the learning curve is less steep to build surgeon confidence and establish efficient workflows before tackling more complex cases.
- Invest in Comprehensive Training: Ensure surgeons, nurses, and technicians receive extensive, ongoing training to master the system's operation and troubleshoot effectively.
- Track Performance Metrics Rigorously: Continuously monitor surgical outcomes, procedure times, and complication rates to quantify the technology's ROI and identify areas for improvement. This data is essential for optimizing both patient selection and workflow automation in the surgical department.
6. Personalized Treatment and Precision Medicine
Precision medicine is one of the most transformative artificial intelligence examples in healthcare, shifting the paradigm from a one-size-fits-all model to individualized patient care. This approach leverages AI to analyze vast and complex datasets, including a patient's genetic makeup, lifestyle, and medical history. Machine learning algorithms identify subtle patterns and correlations within this data to predict disease risk and determine the most effective treatment pathways for a specific individual.
The objective is to deliver the right treatment to the right patient at the right time, minimizing adverse effects and maximizing therapeutic success. For instance, platforms like Tempus and Foundation Medicine use AI to analyze genomic data from tumors, helping oncologists select targeted therapies that are most likely to be effective. Similarly, Guardant Health's liquid biopsy tests use machine learning to detect cancer signals in the bloodstream, enabling non-invasive monitoring and personalized treatment adjustments. This data-driven approach is paving the way for hyper-personalized healthcare.
Strategic Breakdown & Key Benefits
Integrating AI into precision medicine offers a strategic advantage by tailoring therapies to an individual's unique biological profile. This enhances treatment efficacy, reduces trial-and-error prescribing, and improves patient outcomes by focusing on the underlying molecular drivers of a disease rather than just its symptoms. The core benefit is a more targeted and effective healthcare delivery system.
Actionable Takeaways
Implementing a precision medicine program requires careful planning around data management, clinical integration, and patient education. A thoughtful approach is key to harnessing its full potential.
- Establish Robust Data Privacy Protocols: Given the sensitive nature of genomic and personal health information, implementing stringent data security and privacy measures is non-negotiable. Ensure compliance with regulations like HIPAA.
- Collaborate with Specialized Laboratories: Partner with accredited labs specializing in genomic sequencing and analysis to ensure high-quality, reliable data for your AI models.
- Educate and Train Providers: Healthcare providers need to understand the principles of genomic medicine to interpret results and communicate them effectively to patients. Ongoing education is critical for successful adoption. Building a clear AI Product Development Workflow with clinical teams ensures the technology is both useful and usable.
7. Mental Health and Behavioral Analysis
AI-driven mental health support is one of the most rapidly growing artificial intelligence examples in healthcare, offering scalable and accessible solutions for behavioral analysis. This technology leverages machine learning and natural language processing (NLP) to analyze text, speech, and behavioral data for early signs of mental health conditions like depression, anxiety, or PTSD. These systems can provide immediate, personalized interventions, acting as a first line of support.
The primary goal is not to replace human therapists but to augment their reach and provide continuous support between sessions. For instance, AI chatbots like Woebot and Wysa offer cognitive behavioral therapy (CBT) exercises and empathetic conversations 24/7. Meanwhile, platforms like Ellipsis Health analyze speech patterns during routine check-ins to create an objective, data-driven severity score for depression and anxiety, helping clinicians track patient progress more effectively. This makes mental healthcare more proactive, accessible, and integrated into daily life.
Strategic Breakdown & Key Benefits
The strategic advantage of using AI in mental health is its ability to lower access barriers and provide continuous, data-informed care. By analyzing behavioral biomarkers, these tools can flag at-risk individuals earlier and offer personalized support at scale, which is crucial given the global shortage of mental health professionals.
Strategic Insight: AI's role in mental health is to bridge the gap between clinical appointments by providing consistent monitoring and on-demand support. This shifts the care model from reactive to proactive, improving patient engagement and long-term outcomes through early and continuous intervention.
Actionable Takeaways
Implementing AI for mental health requires a strong focus on ethics, privacy, and clinical validity to build user trust and ensure efficacy.
- Implement Robust Privacy Protocols: Since you are handling highly sensitive patient data, ensure end-to-end encryption and compliance with regulations like HIPAA. Be transparent with users about how their data is used.
- Establish Clear Escalation Paths: The AI should never be the final authority. Create a human-in-the-loop system where the AI can flag severe cases or user distress to a qualified human therapist for immediate intervention.
- Prioritize Clinician Validation: Regularly validate the AI's effectiveness against established clinical outcomes. Partner with mental health professionals during the development of your AI Product Development Workflow to ensure the tool is safe, appropriate, and genuinely helpful.
8. Healthcare Operations and Workflow Optimization
Efficient hospital management is a critical yet often overlooked area where AI is making a substantial impact. This application stands as one of the most practical artificial intelligence examples in healthcare, focusing on optimizing the complex, interconnected processes that define daily operations. AI systems leverage predictive analytics and machine learning to analyze vast amounts of historical data, forecasting patient admissions, optimizing staff schedules, and managing bed allocation to reduce wait times and prevent bottlenecks. This can range from high-level strategic planning to the deployment of specific internal tooling for departmental tasks.
The primary objective is to enhance operational efficiency, reduce administrative overhead, and ultimately lower costs while improving patient care. For instance, GE Healthcare's Command Centers provide real-time, hospital-wide visibility, using AI to orchestrate patient flow and resource deployment. Similarly, platforms like Qventus and LeanTaaS predict operational challenges before they occur, allowing administrators to proactively manage everything from emergency room congestion to operating room scheduling. This data-driven approach transforms reactive problem-solving into proactive, strategic management.
Strategic Breakdown & Key Benefits
Integrating AI into hospital operations creates a more resilient, responsive, and efficient healthcare system. The strategic advantage comes from turning operational data into actionable intelligence that drives smarter resource allocation and smoother patient journeys.
- Predictive Staffing: AI analyzes historical patient flow data to predict future demand, ensuring optimal staffing levels that prevent both overstaffing and burnout.
- Optimized Patient Flow: By forecasting admissions and discharges, AI helps manage bed capacity effectively, significantly reducing patient wait times in emergency departments and for inpatient beds.
- Supply Chain Automation: Machine learning algorithms predict the need for medical supplies and pharmaceuticals, automating procurement and preventing costly stockouts or wastage.
- Reduced Administrative Burden: AI-powered automation handles routine administrative tasks, freeing up clinical and administrative staff to focus on higher-value activities and patient care. This is often delivered through AI Automation as a Service.
Actionable Takeaways
Successfully deploying AI for operational optimization requires a blend of technical integration and strong change management.
- Start with a Departmental Pilot: Begin with a specific area like the operating room or emergency department to demonstrate value and refine the implementation strategy before a hospital-wide rollout.
- Engage Staff Early and Often: Involve clinical and administrative staff from the beginning to ensure the AI solution addresses their real-world pain points and to foster buy-in.
- Ensure Robust Data Integration: The success of operational AI depends on clean, integrated data from various hospital systems (EHR, scheduling, etc.). Prioritize creating a unified data pipeline. To learn more about how this can be achieved, explore the benefits of workflow automation.
AI in Healthcare: 8 Use Cases Comparison
AI Application Area Implementation Complexity Resource Requirements Expected Outcomes Ideal Use Cases Key Advantages
Medical Image Analysis and Diagnostics
High: requires extensive training data, regulatory approval
High: deep learning models, integration with PACS systems
Faster, accurate diagnoses; reduced human error
Radiology departments, emergency diagnostics
Increased detection accuracy; 24/7 availability
Drug Discovery and Development
Very High: complex molecular modeling, validation needed
Very High: large datasets, computational resources
Reduced drug development time and costs
Pharmaceutical R&D, clinical trial optimization
Faster drug candidate identification; cost savings
Virtual Health Assistants and Chatbots
Moderate: NLP and integration challenges
Moderate: ML models, system integration
24/7 patient support; reduced workload
Patient engagement, symptom triage
Scalability; improves patient adherence
Predictive Analytics for Patient Outcomes
High: data integration, validation across populations
High: comprehensive patient data, EHR connectivity
Early intervention; reduced readmissions
Hospital care management, chronic disease monitoring
Better resource allocation; improved outcomes
Robotic Surgery and Surgical Assistance
Very High: expensive hardware, specialized training
Very High: advanced robotics, maintenance costs
Increased surgical precision; faster recovery
Minimally invasive surgeries
Enhanced accuracy; reduced surgeon fatigue
Personalized Treatment and Precision Medicine
High: requires genomic data, complex interpretation
High: genetic testing, multi-omics data analysis
Improved treatment efficacy; fewer adverse effects
Oncology, rare genetic diseases
Tailored treatments; higher patient satisfaction
Mental Health and Behavioral Analysis
Moderate: NLP and behavior analysis, privacy concerns
Moderate: sensor and data integration, clinical oversight
Early detection and intervention
Mental health monitoring and therapy
Accessible support; stigma reduction
Healthcare Operations and Workflow Optimization
Moderate to High: multi-system integration challenges
Moderate to High: data analytics infrastructure
Cost reduction; increased efficiency
Hospital administration, supply chain
Significant operational savings; improved patient flow
The Future is Now: Integrating AI into Your Healthcare Strategy
As we’ve explored, the landscape of healthcare is being fundamentally reshaped by artificial intelligence. The powerful artificial intelligence examples in healthcare we've examined, from AI-powered medical imaging and accelerated drug discovery to predictive analytics and robotic surgery, are not futuristic concepts; they are tangible solutions delivering value today. These applications demonstrate a clear trajectory towards a more efficient, precise, and patient-centric healthcare ecosystem.
The core takeaway is that AI's impact is not confined to a single department or function. It is a transformative force capable of optimizing everything from clinical diagnostics and personalized treatment plans to administrative workflow automation and operational efficiency. The strategic advantage no longer lies in whether to adopt AI, but in how and where to integrate it for maximum impact.
From Insight to Action: Your Next Steps
Moving from understanding these examples to implementing them requires a clear, strategic approach. The journey begins not with technology, but with identifying the most critical challenges and opportunities within your organization.
- Identify High-Impact Areas: Review the use cases discussed. Do you face challenges in diagnostic accuracy, operational bottlenecks, or patient engagement? Start by pinpointing the areas where AI can deliver the most significant return on investment and improve patient outcomes.
- Develop a Phased Roadmap: Successful AI integration is a marathon, not a sprint. A well-defined AI Product Development Workflow is crucial. Begin with a pilot project to prove value, gather data, and build internal support before scaling across the organization. For more on this, review our real-world use cases to see how others have started.
- Foster a Data-Centric Culture: AI thrives on data. Ensure your organization has robust data governance, infrastructure, and security protocols in place. This foundational work is non-negotiable for any successful AI initiative, particularly in a highly regulated field like healthcare.
- Partner for Expertise: You don’t have to navigate this complex journey alone. Leveraging external expertise through AI co creation or AI strategy consulting can accelerate your timeline, mitigate risks, and ensure your strategy aligns with both clinical and business objectives.
Strategic Imperative: The true value of AI in healthcare is unlocked when technology is strategically aligned with specific clinical needs and business goals. The goal isn't just to implement AI tools for business; it's to create integrated systems that empower clinicians, improve patient care, and streamline operations.
By embracing these principles, healthcare leaders can transition from observing the AI revolution to actively leading it. The potential to enhance diagnostic speed, personalize medicine, and create a more resilient healthcare system is immense. For leaders looking to stay ahead of the curve, it is also beneficial to follow publications that offer fresh perspectives. For instance, you can find valuable insights from the Salthea blog on evolving applications and strategies. The time to build your AI-powered future is now, and with a strategic, deliberate approach, the transformative benefits are well within reach. To begin your journey, connect with our expert team to see how we can help.
Frequently Asked Questions (FAQs)
What are the main benefits of using AI in healthcare?
The primary benefits include enhanced diagnostic accuracy and speed, accelerated drug discovery timelines, personalized treatment plans, improved operational efficiency in hospitals, and increased patient engagement through tools like virtual health assistants. Ultimately, AI helps improve patient outcomes while reducing costs.
Is AI intended to replace healthcare professionals like doctors and radiologists?
No, the goal of most AI applications in healthcare is to augment and support human professionals, not replace them. AI acts as a powerful tool that can analyze vast amounts of data quickly, flag potential issues, and handle routine tasks, freeing up clinicians to focus on complex decision-making, patient care, and the human aspects of medicine.
What are the biggest challenges to implementing AI in healthcare?
Key challenges include ensuring data quality and privacy (especially with HIPAA regulations), the high cost of implementation and infrastructure, the need for robust clinical validation to ensure safety and efficacy, overcoming potential algorithmic bias, and integrating AI systems seamlessly into existing clinical workflows.
How does AI help in personalizing medicine?
AI analyzes a patient's unique genetic data, lifestyle factors, and clinical history to predict their risk for certain diseases and determine which treatments will be most effective for them. This allows oncologists, for example, to select targeted therapies based on a tumor's specific genomic profile, leading to better outcomes and fewer side effects.
Ready to translate these powerful AI examples into a competitive advantage for your organization? Ekipa AI specializes in crafting and implementing bespoke AI strategies that drive real-world results in the healthcare sector. Let us help you navigate the complexities of AI adoption, from building a Custom AI Strategy report to deploying powerful automation solutions. Contact our expert team today to get started.