How AI Enhances Telemedicine Services in Modern Healthcare
Discover how AI enhances telemedicine services with real-world applications in diagnostics, patient monitoring, and workflow automation to improve healthcare.
Healthcare leaders are constantly asking how AI can really improve telemedicine. The answer is surprisingly straightforward: AI is already overhauling remote care. It’s a powerful tool for automating clinical workflows, boosting diagnostic accuracy, creating personalized patient experiences, and enabling predictive remote monitoring. This isn't some far-off future—it's happening right now, leading to incredible gains in efficiency and better outcomes for patients.
The AI Revolution in Telemedicine
This guide is designed to break down the real-world value of bringing artificial intelligence into your remote healthcare services. If you're a healthcare executive or a technology leader, getting a handle on these advancements is key to staying ahead and delivering superior care. We’ll dig into how AI improves everything from initial triage and diagnostics to round-the-clock patient monitoring and back-office automation.
The global telemedicine market was already valued at $101.2 billion in 2023, and AI is one of the biggest reasons it's projected to keep growing. Bringing AI into the fold is no longer an option; it's a core component of modern, high-quality healthcare.
Why AI is a Game-Changer for Remote Care
The real magic of AI in telemedicine is its ability to sift through massive datasets faster and more accurately than any human ever could. This single capability opens up a whole new world of strategic advantages for healthcare providers.
- Enhanced Efficiency: AI takes over the repetitive, time-consuming tasks like data entry and initial symptom checks. This frees up your clinicians to focus on what they do best: handling complex cases and making critical decisions. It’s a direct response to the professional burnout that plagues so much of the industry.
- Improved Accuracy: AI algorithms are trained to spot subtle patterns in medical images or patient data that the human eye might overlook. The result? Earlier, more precise diagnoses. To put a number on it, some AI-driven systems have achieved a 94% accuracy rate in virtual triage situations.
- Scalable Personalization: Imagine delivering a unique care plan to every single patient without burning out your staff. AI makes that possible. It allows for highly personalized patient engagement at a scale that was once unthinkable, leading to better compliance and healthier patients.
- Proactive Interventions: By constantly analyzing data from wearables and other remote devices, AI can flag potential health problems before they escalate. This shift from reactive to proactive care is a huge win, often preventing costly and stressful hospital visits.
Making this shift requires a clear, strategic approach. Expert guidance can help align this powerful technology with your core clinical and business goals. You can explore more about purpose-built AI solutions for the healthcare industry to see how this comes to life.
Supercharging Diagnostics and Triage with AI
One of the most impactful ways AI is changing telemedicine is by giving a serious boost to diagnostics and triage. Picture an AI algorithm as a tireless, incredibly focused specialist on call 24/7. These systems can analyze medical images—think skin scans or X-rays—and patient-reported symptoms with lightning speed, often spotting subtle patterns that a human eye might miss.
This is completely reshaping the "front door" of virtual care. AI is making a real difference in diagnostic accuracy and operational efficiency, putting remote consultations on par with in-person visits. The numbers back this up: the global AI healthcare market hit $19.27 billion in 2023 and is projected to grow at a blistering 38.5% CAGR through 2030. In US hospitals alone, AI adoption is taking off, with physician usage jumping 78%—from 38% in 2023 to 66% in 2024. A great example is how AI in neurology can process scans in seconds, significantly cutting down on errors.

Intelligent Triage for Better Care Delivery
Before a patient even speaks to a clinician, AI-powered triage chatbots can intelligently sort their inquiries. By walking through a series of targeted questions, these bots quickly figure out how urgent a situation is. This automated first step fast-tracks critical cases for immediate attention and helps schedule routine appointments for less severe issues.
Essentially, this system acts as a smart gatekeeper, optimizing clinician schedules and making sure high-priority cases don't get lost in a crowded virtual queue. A patient reporting chest pain would be instantly flagged for an emergency consult, while someone with mild allergy symptoms might be guided to schedule a visit for the next day. This kind of efficiency is a cornerstone of advanced AI solutions.
By automating the initial patient intake, healthcare organizations can manage a much higher volume of inquiries without letting the quality of care slip. It’s all about getting the right level of medical attention to the right patient at the right time.
Boosting Diagnostic Accuracy with Machine Learning
But AI’s role doesn’t stop at triage. It’s also a powerful partner in the diagnostic process itself. Machine learning models, trained on vast datasets of millions of medical images and patient records, can help clinicians make faster, more confident diagnoses. These tools are especially valuable in fields that lean heavily on visual assessment.
Here are a few real-world examples of this in action:
- Dermatology: A patient uploads a photo of a skin mole. An AI algorithm analyzes the image for characteristics of malignancy, giving the dermatologist a risk assessment before the virtual consultation even starts. This is similar to the approach used by our own diagnostic support tool, Diagnoo.
- Radiology: AI can pre-screen X-rays or CT scans, highlighting potential trouble spots for the radiologist to focus on. This not only speeds up the reading process but also serves as a reliable second set of eyes.
- Symptom Analysis: Before a video call, an AI platform can run a preliminary symptom check, cross-referencing a patient's issues with their medical history to suggest possible diagnoses for the clinician to explore.
The shift from traditional to AI-enhanced diagnostics is striking, especially when you look at the key metrics side-by-side.
AI's Impact on Telemedicine Diagnostics
| Metric | Traditional Telemedicine | AI-Enhanced Telemedicine |
|---|---|---|
| Triage Time | Manual, often 15-20 minutes per patient | Automated, typically under 5 minutes |
| Diagnostic Speed | Relies solely on clinician's real-time assessment | AI provides pre-analysis, accelerating decisions |
| Accuracy | Dependent on individual clinician expertise | Improved by AI's pattern recognition from vast datasets |
| Clinician Workload | High administrative burden, repetitive tasks | Reduced workload, focus on complex cases |
| Patient Waiting Time | Can be long due to manual queues | Significantly shorter with automated triage and scheduling |
For CTOs and operations leaders, the benefits are clear. Investing in these AI diagnostic tools directly translates into fewer misdiagnoses, faster care delivery, and stronger patient trust—a compelling ROI that’s hard to ignore.
From Reactive to Predictive: The New Era of Remote Patient Monitoring
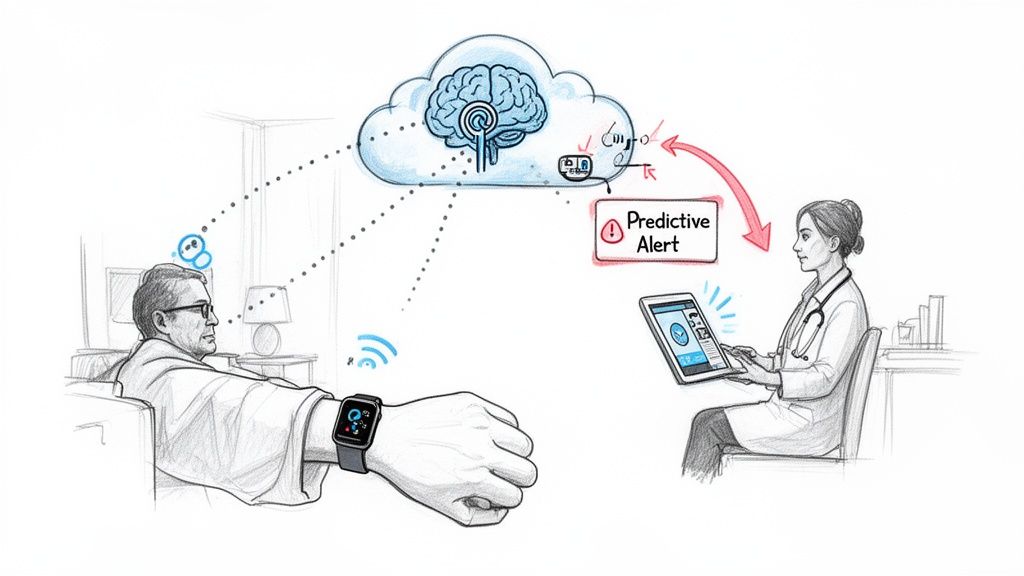
Artificial intelligence is taking remote patient monitoring (RPM) out of the past. Instead of just gathering data, AI is turning it into a powerful tool for predicting and preventing health problems. This fundamental change is shifting how we manage chronic illnesses, moving from reactive responses to proactive care.
The concept is simple but incredibly powerful. AI algorithms are constantly sifting through data streams from wearables and at-home devices—think glucose monitors, smart scales, and blood pressure cuffs. It acts like a vigilant digital assistant, looking for tiny trends or patterns that could hint at an upcoming health crisis, long before a human might notice.
This shift is a true game-changer for managing long-term conditions like diabetes, congestive heart failure, and COPD. It’s also a major force behind the explosive growth in the AI-powered telemedicine market. Valued at USD 5.3 billion in 2025, the market is expected to skyrocket to USD 86.31 billion by 2034, growing at an incredible 36.35% each year. Remote patient monitoring is set to be the fastest-growing piece of that pie. You can dig into more data on AI's impact in the telemedicine market to see just how big this opportunity is.
Pinpointing At-Risk Patients Before a Crisis Hits
With traditional RPM, clinicians often find themselves drowning in data, making it nearly impossible to figure out who needs help right now. AI changes this by getting to know each patient individually, establishing a unique health baseline of what’s "normal" for their body.
When the system spots a deviation—maybe a slow but steady weight gain for a heart failure patient or unusual blood sugar spikes for someone with diabetes—it does more than just update a chart. It sends a predictive alert, flagging that patient for intervention well before they’d even think to call their doctor. This early warning can make all the difference. In fact, pioneering AI monitoring systems have already shown they can achieve a 40% reduction in hospital readmissions for high-risk patients.
By catching subtle signs of declining health days or even weeks in advance, AI gives clinical teams the power to step in early. This not only improves a patient's quality of life but also prevents expensive ER visits and hospital stays.
Turning Data Points into Actionable Insights
AI’s real magic lies in its ability to translate raw biometric data into clear, useful insights that help clinicians make smarter decisions. A care manager no longer has to spend hours poring over patient logs. Instead, they get a prioritized list of who needs a follow-up call, a medication tweak, or a quick telehealth check-in.
Here’s what that looks like in the real world:
- Diabetes Management: An AI might notice a patient’s glucose is consistently high in the mornings. By cross-referencing this with their food log, it could suggest a specific dietary change to discuss with their provider.
- Heart Failure: The system could flag a slight weight gain combined with lower activity levels over a week, triggering an alert for the care team to check for fluid retention.
- Post-Operative Care: After a patient goes home, AI can monitor their vitals for any early signs of infection or complications, allowing the surgical team to intervene immediately.
For business leaders, this opens up a huge opportunity to build premium RPM services. It creates a far more scalable and effective model for chronic care, which can be brought to life with a structured AI Product Development Workflow. The key is to first identify the most valuable RPM use cases for your patient population. A Custom AI Strategy report can give you the clarity you need to make the right investment.
Automating Workflows and Slashing Administrative Burden
Beyond the clinical benefits, one of the most immediate and tangible wins for AI in telemedicine is its ability to tackle the mountain of administrative work that bogs down clinicians. If you're running operations, you know that efficiency is everything. AI delivers by automating the repetitive, draining tasks that are a fast track to burnout.
By taking over the grunt work, AI unshackles clinicians from paperwork and lets them focus on what they’re actually there to do: care for patients.
The numbers here are staggering. Bringing in AI can trim administrative costs by 5-10%, which adds up to hundreds of billions of dollars a year in the U.S. healthcare system. This isn't just about saving cash; it's about shifting resources back into patient care and expanding capacity. When you automate things like scheduling and billing, you can see more patients without burning out your team.
Let NLP Handle the Paperwork
Natural Language Processing (NLP) is the engine behind this administrative overhaul. Think of it as a smart assistant that can understand and process human language. For telemedicine, this is a game-changer, especially for clinical documentation—a task that’s as critical as it is time-consuming.
Picture an AI scribe sitting in on a virtual visit. It transcribes the conversation live, but it doesn't just create a wall of text. The NLP goes to work, pulling out the important details, summarizing the discussion, and neatly populating the electronic health record (EHR) for the clinician. This alone can give a provider back up to two hours every single day.
AI documentation tools are completely changing the feel of virtual care. By taking over the clerical tasks, they let providers be fully present and engaged with their patients, which makes for a much better, more human interaction.
Smoothing Out the Entire Patient Journey
This kind of automation isn't just about taking notes. AI can intelligently manage the entire administrative flow of a telemedicine appointment, making the whole process smoother for everyone involved. To get a deeper sense of how these pieces fit together, it’s worth understanding strategic workflow automation.
Here’s a look at how it plays out:
- Smarter Scheduling: Instead of endless phone calls, an AI chatbot can handle patient questions, collect their info, and find the right appointment slot. No more phone tag, no more scheduling mistakes.
- Faster Billing and Claims: AI can look at the clinical notes from a visit and automatically generate the correct billing codes. It can even check insurance claims for errors before they're sent, which means fewer rejections and faster payments.
- Automated Follow-up: After an appointment, AI can send out reminders for medications, share helpful educational materials, or dispatch check-in surveys to make sure patients are sticking to their care plans.
One of the biggest time-savers is the use of advanced voice recognition software for healthcare, which can automatically document conversations and simplify note-taking. By bringing in this level of automation, healthcare organizations build more resilient and efficient operations from the ground up.
Giving Each Patient a Personal Touch, at Scale
Let's be honest, healthcare often feels anything but personal. AI is changing that by giving telemedicine platforms the ability to ditch the one-size-fits-all model for good. Instead, algorithms can look at a patient's unique mix of genetic data, lifestyle habits, and their full medical history to build a truly bespoke care plan. We're talking about a level of individual attention that was simply unthinkable on a large scale until now.
This personal touch goes way beyond just the treatment plan. It weaves its way through every single interaction a patient has. Imagine AI systems that automatically send out educational content picked just for them, medication reminders that are actually helpful, and follow-up messages that are genuinely proactive, all based on their specific condition and how they're progressing. It's this kind of thoughtful engagement that really gets patients to stick with their care plans.
A Personal Health Concierge for Every Patient
What this really creates is a personal health concierge for every single patient. Even though the care is remote, this kind of automated, high-touch support makes people feel seen and supported. It strengthens that crucial patient-provider bond. For healthcare organizations, this pays off directly in happier patients who stick around.
This is worlds away from the generic, impersonal messages we've all come to expect. Instead of a bland "take your pill" reminder, a patient with diabetes might get a message with a link to an article on managing blood sugar during the holidays, sent right when they need it. These are the kinds of thoughtful, relevant interactions that keep people engaged—a core idea we explore in many of our real-world use cases.
By digging into patient data to offer tailored advice and support, AI builds a relationship that’s proactive and continuous. It shifts telemedicine from a chain of separate appointments into one connected, supportive health journey.
Building Truly World-Class Experiences
Pulling off this level of sophisticated personalization isn't accidental; it needs a solid strategy. A well-defined AI Product Development Workflow is what turns a generic platform into a world-class system for delivering care. The whole process is about carefully designing algorithms that can make sense of complex patient data and then trigger the right action at the right time.
Creating these experiences usually means bringing together specialized AI tools for business with deep expertise in the healthcare field. The end goal is a system that doesn't just understand a patient's clinical needs but can also get ahead of their questions and challenges before they even ask.
This isn't just a nice-to-have feature; it's a massive competitive advantage. Healthcare providers who go all-in on personalization will be the ones who lead the pack in patient loyalty and, more importantly, in better health outcomes. This is exactly where our expert team can help, guiding you through the ins and outs of custom healthcare software development to make sure the final product is as powerful as it is patient-focused. The right AI solutions put this seemingly ambitious goal well within reach.
Your Roadmap to AI-Powered Telemedicine
Jumping into an AI transformation can feel like a massive undertaking, but a phased approach makes the whole process manageable. It's one thing to understand how AI can improve telemedicine; it's another thing entirely to get it implemented correctly. This roadmap lays out a practical path, from the initial idea to a full-scale launch, making sure your investment pays off in both clinical outcomes and operational efficiency.
The whole journey starts with building a solid foundation. Think of it as a methodical process designed to minimize risk and set you up for success right from the start.
Phase 1: Discovery and Strategy
First things first: you need a clear target. Before a single line of code is written, your entire organization needs to agree on what "success" actually means. This is about cutting through the hype to find specific, high-impact problems that AI is uniquely suited to solve.
A thorough AI requirements analysis is absolutely essential here. This isn't just a box-ticking exercise; it's a deep dive to find the best opportunities. Are you trying to slash diagnostic wait times? Automate mind-numbing administrative tasks? Or get better at predicting patient risk? The goal is to build a prioritized list of real-world use cases that connect directly to your core business goals. This is exactly where experienced AI strategy consulting can make a huge difference, pointing you toward the projects with the biggest potential payoff.
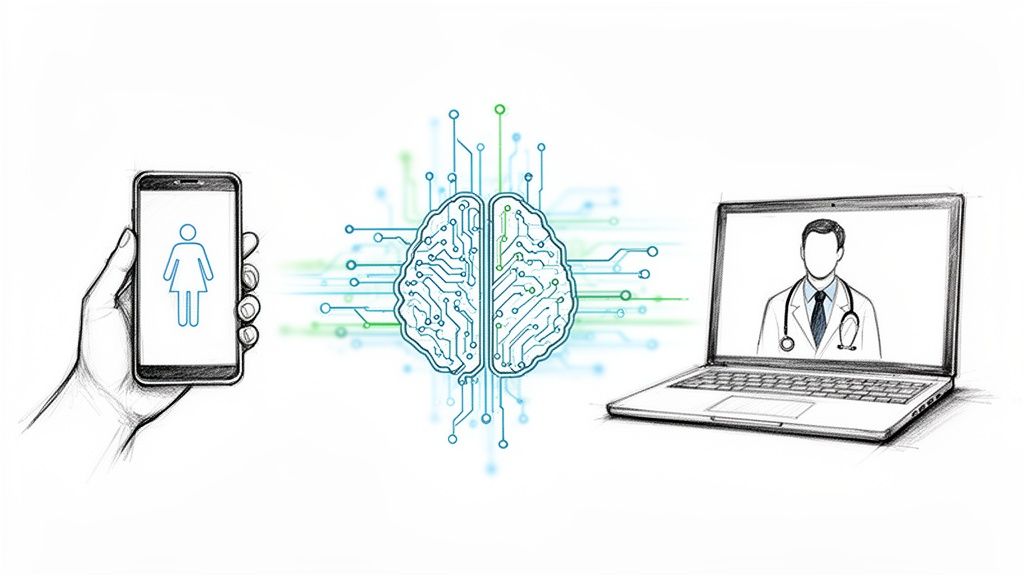
Phase 2: Data Readiness and Preparation
AI runs on data. Simple as that. The quality of your algorithms will never be better than the quality of the data you feed them. This phase is all about getting your data house in order—making sure it’s clean, secure, and ready to go. You'll be looking at your current data infrastructure, finding any gaps, and setting up strict governance to maintain HIPAA compliance and protect patient privacy.
This means pulling together information from all over the place—EHRs, wearables, lab results, imaging systems—and getting it into a single, usable format. Think of it like a chef prepping ingredients before cooking a complex meal. If you start with bad ingredients, you're going to end up with a bad dish, no matter how skilled the chef.
The image below shows how AI takes raw data and turns it into a personalized journey for each patient by analyzing, planning, and engaging.
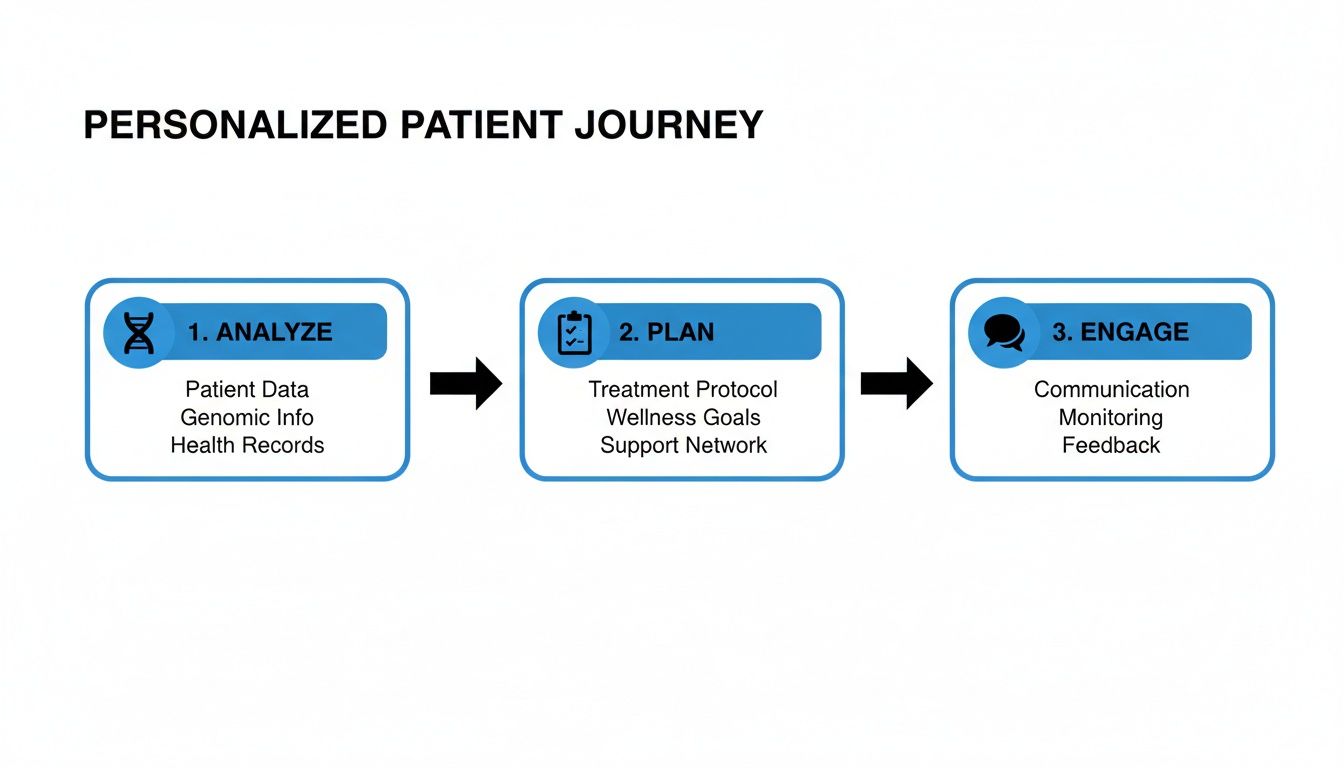
This really brings home the point that a successful AI project is all about turning patient data into concrete, personalized care plans.
Phase 3: Pilot Implementation and Scaling
Once your strategy is set and your data is clean, you can finally start building. The smartest way to do this is with a small, focused pilot project. Pick one of the high-impact use cases you identified in the discovery phase and build a minimum viable product (MVP). This lets you test the concept in a real but controlled setting without betting the farm.
For any pilot, you need clear Key Performance Indicators (KPIs) to know if it's working. These should be specific, like "a 15% reduction in clinician administrative time" or "a 10% improvement in diagnostic accuracy for a specific condition."
If the pilot delivers on its promise, you're ready to scale. This means weaving the new AI solutions into your existing workflows, properly training your staff, and making sure all regulatory boxes are checked. This entire journey, from concept to scale, can be de-risked and sped up with a Custom AI Strategy report and the guidance of our expert team who are there to help you succeed.
A structured roadmap is the key to turning an ambitious vision into a tangible reality. The table below provides a high-level executive summary of the journey.
Executive Roadmap for AI Integration in Telemedicine
| Phase | Key Objective | Critical Considerations |
|---|---|---|
| 1. Discovery & Strategy | Define clear business goals and identify high-impact AI use cases. | Involve clinical and operational stakeholders. Focus on solving real problems, not just adopting technology for technology's sake. |
| 2. Data Readiness | Assess, clean, and consolidate data sources for AI model training. | Ensure strict HIPAA compliance and data governance. Data quality is non-negotiable and directly impacts AI performance. |
| 3. Pilot Program | Develop and test a Minimum Viable Product (MVP) for a single use case. | Set clear KPIs to measure success. Gather user feedback from clinicians and patients early and often. |
| 4. Scaling & Integration | Roll out the proven AI solution across the organization. | Plan for system integration challenges. Develop comprehensive staff training programs and monitor performance continuously. |
By following these phases, you can methodically build an AI-powered telemedicine platform that not only enhances efficiency but also delivers a higher standard of patient care.
Frequently Asked Questions
What is the role of AI in telemedicine services?
Artificial intelligence significantly enhances telemedicine by automating administrative tasks, improving diagnostic accuracy through machine learning, enabling proactive remote patient monitoring with predictive analytics, and delivering personalized patient care plans at scale. It transforms remote healthcare from a reactive service into a more efficient, accurate, and proactive system.
How does AI improve diagnostic accuracy in remote consultations?
AI algorithms, trained on vast medical datasets including images and patient records, can identify subtle patterns that a human eye might miss. In fields like dermatology or radiology, AI can pre-analyze images, flag potential areas of concern, and provide a risk assessment to the clinician. This acts as a powerful "second opinion," leading to faster, more confident, and more accurate diagnoses.
What are the main benefits of using AI for remote patient monitoring (RPM)?
The primary benefit is the shift from reactive to predictive care. Instead of just collecting data, AI analyzes real-time streams from wearables and devices to detect early signs of a potential health decline. This allows clinical teams to intervene proactively, often preventing hospitalizations, improving management of chronic conditions, and enhancing patient quality of life.
How can AI reduce the administrative burden on healthcare professionals?
AI tools, particularly those using Natural Language Processing (NLP), can automate time-consuming administrative workflows. This includes transcribing virtual consultations, summarizing clinical notes, automatically populating electronic health records (EHRs), and streamlining billing and scheduling. This frees up clinicians to focus more on direct patient care and less on paperwork.
Is it secure to use AI with sensitive patient data?
Yes, provided that security is a core priority. Secure AI platforms are built with HIPAA compliance in mind, utilizing techniques like end-to-end encryption and data anonymization. It is crucial for healthcare organizations to partner with technology providers who have robust data governance policies and conduct regular security audits to ensure patient data remains protected at all times.
Ready to see what AI can do for your telemedicine services but not sure about the next step? Ekipa AI can give you that strategic clarity. Our AI Strategy consulting tool delivers a Custom AI Strategy report in hours, not months, helping you pinpoint and act on the AI opportunities with the most impact. Let our expert team guide you through it.