Care Delivery Optimization: Turn Care Delivery Optimization into Better Outcomes
Explore how care delivery optimization reshapes healthcare with proven AI tools, metrics, and a practical roadmap for better patient outcomes.
At its heart, care delivery optimization is about systematically improving how healthcare is delivered. It’s a strategic approach focused on achieving better patient outcomes and boosting satisfaction, all while making operations more efficient and keeping costs in check. This isn't just about tweaking a few processes; it involves redesigning workflows, aligning resources with patient needs, and using smart technology to build a stronger, more responsive healthcare system.
Why Care Delivery Optimization Is No Longer Optional
The healthcare industry is navigating some serious headwinds right now. We're seeing escalating operational costs, a growing demand for patient services, and a massive industry-wide shift toward value-based payment models. These forces combined are pushing leaders to completely re-evaluate how they run their organizations.
In this climate, care delivery optimization has gone from a "nice-to-have" idea to an essential strategy for survival.
This is about much more than just cutting costs. It’s about building a system that can last. Inefficiencies in everyday operations—like patient scheduling, clinical documentation, and managing supplies—are not just financial drains; they directly impact the quality of patient care. Every minute a doctor or nurse spends bogged down by administrative work is a minute they can't spend with a patient.
The Economic and Clinical Imperative
The financial pressures are undeniable. Healthcare spending is projected to jump by 7.1 percent in 2025, and individual medical costs have already hit a 13-year high. It's no surprise, then, that 53 percent of healthcare executives now say improving efficiency and productivity is their number one goal. This tough financial picture is exactly why organizations are turning to AI-driven solutions to get more value from the data and technology they already have.
The drive to optimize creates a positive ripple effect throughout the entire organization, benefiting everyone involved:
For Patients: This means shorter waits, care plans that feel more personal, and ultimately, better health.
For Clinicians: It leads to less administrative headache, a real reduction in burnout, and more time for the patient interactions that matter.
For Administrators: The result is greater financial stability, smarter use of resources, and stronger performance under value-based care agreements.
At its core, care delivery optimization is a strategic imperative for building a resilient, efficient, and patient-centric healthcare system. It reframes the challenge from simply cutting costs to intelligently reinvesting resources into what matters most—delivering exceptional care.
The table below breaks down the key factors pushing healthcare organizations to adopt these strategies.
Key Drivers For Optimizing Care Delivery
| Driver Category | Description | Impact on Operations |
|---|---|---|
| Economic Pressure | Rising operational costs, labor shortages, and shrinking margins under fee-for-service models. | Demands greater efficiency in resource allocation, supply chain management, and staffing to maintain financial health. |
| Regulatory Shifts | The industry-wide move from fee-for-service to value-based care, which ties reimbursement to patient outcomes. | Requires a focus on preventative care, care coordination, and reducing readmissions to succeed financially. |
| Patient Expectations | Patients today expect a more consumer-like experience: convenient access, clear communication, and personalized care. | Pushes organizations to improve scheduling, streamline patient intake, and enhance digital engagement tools. |
These drivers aren't going away; they're only intensifying, making a proactive approach to optimization more critical than ever.
The Role of Advanced Technology
Getting to this next level of operational performance requires more than just small, incremental changes. It calls for a significant technological step forward. This is where advanced Healthcare AI Services come into play, providing the key to unlocking a new tier of operational intelligence.
By automating routine tasks and delivering deep, data-backed insights, these tools empower organizations to build a smarter, more agile care delivery model that’s ready for whatever challenges come next.
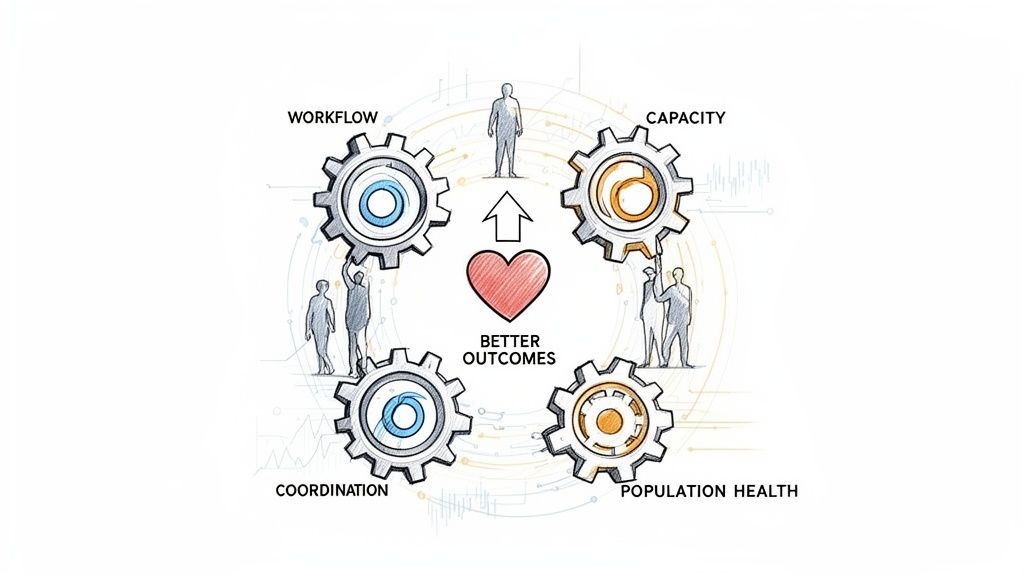
The Foundational Pillars of Optimized Healthcare
When we talk about care delivery optimization, we're not talking about a one-off project. It's a fundamental shift in how a healthcare organization operates, built on several core pillars. Think of it like building a modern skyscraper—each support column is critical. If one is weak, the entire structure is at risk. To build a truly resilient, efficient, and patient-first operation, you have to get these foundational pieces right.
What’s powerful is how these pillars support each other. An improvement in one area inevitably creates positive momentum in another.

Pillar 1: Clinical and Administrative Workflow Redesign
First up, we have to fix broken workflows. Clunky, inefficient processes are a massive drain on resources, directly contributing to clinician burnout and frustrating delays for patients. We've all seen it: the endless, repetitive data entry for clinical notes that eats up hours of a doctor's or nurse's day.
This is where smart interventions can make a world of difference. For example, implementing AI Automation as a Service can handle tasks like transcribing patient notes or pre-filling routine forms. This gives clinical staff back their most valuable asset: time to spend with patients. To spot these high-impact opportunities, it's crucial to understand key healthcare process improvement strategies.
Pillar 2: Demand and Capacity Management
Next is the delicate balancing act between patient demand and your available capacity. When this is out of sync, you get overcrowded waiting rooms, appointments scheduled weeks out, and expensive operating rooms sitting empty. The real challenge is predicting the natural ebb and flow of patient needs and matching your staff, beds, and equipment to it.
A classic example is an emergency department that’s completely swamped during peak hours while, just a floor away, surgical suites are underused. This is a perfect use case for modern AI solutions. Predictive analytics can dig into historical admission data to forecast patient surges, allowing leaders to make proactive staffing changes and get ahead of bed shortages.
An optimized system doesn't just react to demand—it anticipates it. By aligning capacity with predicted patient needs, organizations can smooth out operational peaks and valleys, ensuring resources are always where they are needed most.
Pillar 3: Seamless Care Coordination
Care coordination is all about making sure the patient's journey is smooth and safe as they move between different departments, facilities, or providers. This is where things often fall apart, especially for patients with chronic conditions who are juggling multiple specialists. A simple lack of communication can lead to redundant tests, conflicting prescriptions, and hospital readmissions that were entirely preventable.
True coordination demands a single, unified view of the patient. This is why building better internal tooling is so important. It creates a shared platform where everyone on the care team—from the family doctor to the specialist to the home health aide—is looking at the same real-time information.
Pillar 4: Proactive Patient Engagement
This pillar represents a shift from simply treating sickness to actively partnering with patients in their own health. The old, passive follow-up process after a hospital discharge is a perfect example of what not to do. Patients are often sent home with a stack of complex instructions and left to figure it out, which is a big reason readmission rates are so high.
A modern, optimized approach flips that model on its head. It means:
Automated Check-ins: Using simple text messages or app notifications to ask a patient how their recovery is going.
Personalized Education: Sending helpful articles or videos tailored to a patient's specific condition and care plan.
Easy Scheduling: Giving patients simple digital tools to book their own follow-up appointments without playing phone tag.
Pillar 5: Revenue Cycle Integrity
Finally, none of the other pillars can stand without the financial health provided by a solid revenue cycle. Breakdowns here are common and costly: coding mistakes, delayed claim submissions, and high denial rates all hit the bottom line hard. These problems almost always trace back to complicated, manual administrative work that’s just begging for human error.
This is an area where specialized Healthcare AI Services can be a game-changer. AI can automatically "scrub" claims to catch errors before they're submitted and even predict which claims are likely to be denied, giving staff a chance to fix them first. A healthy revenue cycle isn't just about money; it's what gives an organization the stability to keep investing in patient care and innovation.
Putting AI to Work: From Theory to the Clinic Floor
All those big ideas about care delivery optimization sound great on paper, but where does the rubber meet the road? This is where artificial intelligence stops being a buzzword and becomes a practical, problem-solving tool for your teams. The real wins don’t come from a single, massive tech overhaul. They come from deploying targeted AI solutions that fix specific, high-friction points in your daily clinical and administrative work.
Let’s look at a few tangible, real-world use cases where AI is already making a huge difference.
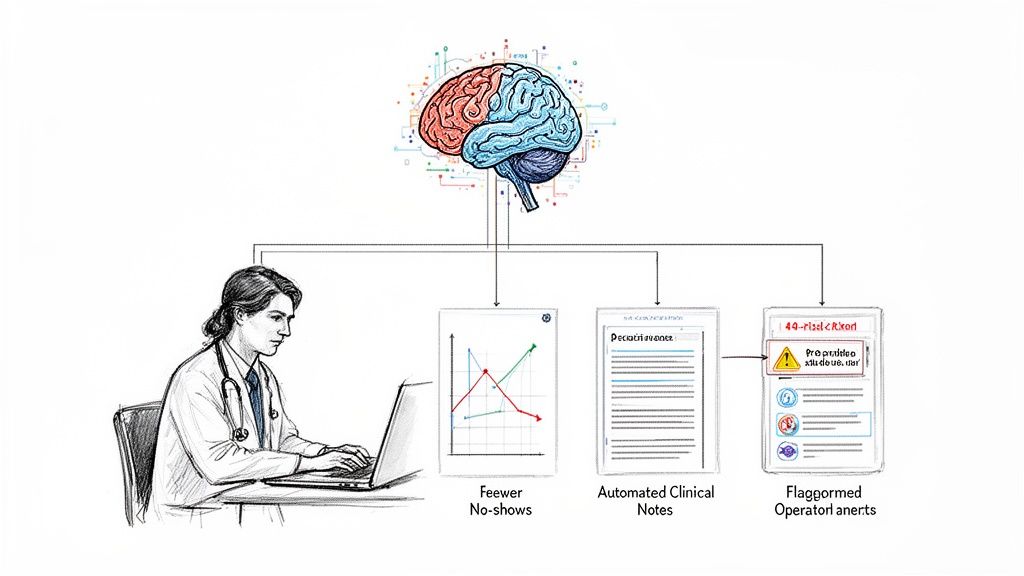
Predictive Analytics for Demand and Capacity
Matching your staff and resources to patient demand is one of healthcare's oldest headaches. We’ve all been there—relying on last year's averages only to get caught flat-footed by a sudden flu outbreak or a quiet week that leaves staff overscheduled and budgets strained.
Predictive analytics completely changes this guessing game. By feeding machine learning models a mix of historical admissions data, local public health reports, and even things like weather patterns, you can forecast patient volumes with impressive accuracy.
This gives hospital leaders the foresight to:
Optimize Staff Schedules: Instead of reacting to a surge in flu cases, you can proactively adjust nursing shifts to meet the expected demand.
Manage Bed Availability: You can anticipate the need for ICU beds and begin coordinating patient flow and transfers well in advance.
Reduce Patient No-Shows: AI can pinpoint patients likely to miss appointments, triggering personalized reminders that cut down on wasted slots and lost revenue.
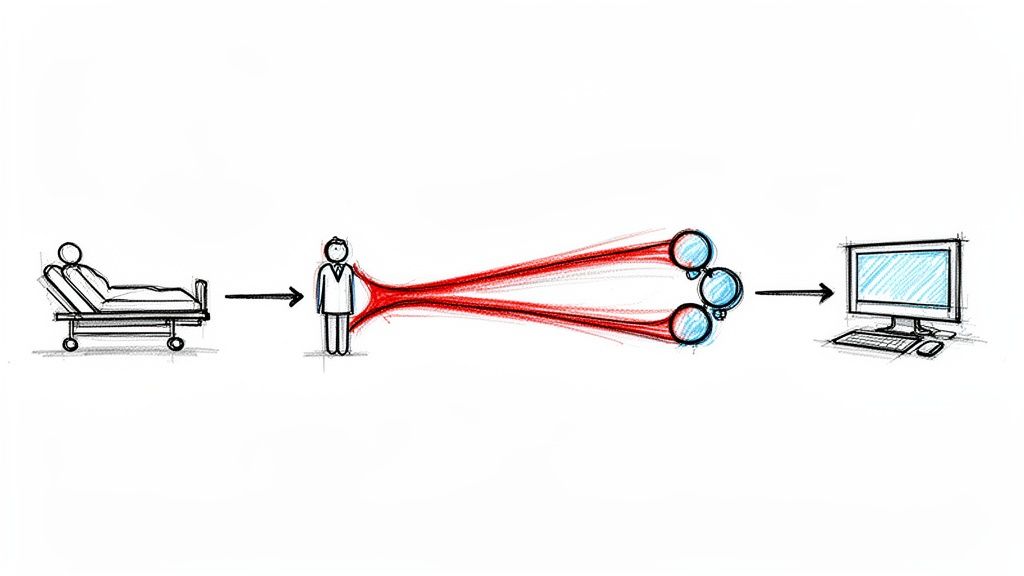
NLP for Slaying the Documentation Dragon
Physician burnout is a real crisis, and we all know a huge part of the problem: the soul-crushing administrative burden. Doctors and nurses spend far too much time clicking boxes and typing into EHRs. That’s time stolen directly from patient care.
This is where Natural Language Processing (NLP) comes in. Think of ambient clinical intelligence tools that can listen in on a natural conversation between a doctor and a patient. The AI then automatically transcribes, structures, and summarizes the important details into a compliant clinical note.
It’s like giving every clinician a virtual scribe, finally freeing them from the keyboard. This doesn’t just boost morale; it leads to better, more complete clinical records, which are vital for coordinating care and ensuring the revenue cycle runs smoothly.
For instance, a dedicated clinic AI assistant can take on the heavy lifting of transcription and summarization, directly tackling one of the biggest sources of administrative drag.
Machine Learning for Proactive Patient Care
The entire healthcare system is trying to move from reactive treatment to proactive prevention. Machine learning is perfectly suited for this mission. It can spot faint signals and complex patterns across massive datasets that a human could never see, making it an incredible tool for finding at-risk patients before things get serious.
Imagine a health system using a model that sifts through thousands of data points in a patient's EHR—lab results, medications, past diagnoses—to calculate their real-time risk of developing sepsis or being readmitted within 30 days.
When the algorithm flags a high-risk patient, it can trigger an alert to the care team. This gives them a chance to step in early with a follow-up call, a home health visit, or a medication tweak. It’s about preventing a dangerous and expensive hospital stay before it ever happens.
This isn't just good medicine; it's good business. With the number of patients in value-based care models set to more than double to 90 million by 2027, data-driven prevention is a financial necessity. In one striking example, a regional health plan used advanced analytics and machine learning to slash member hospitalizations by 30 percent. This resulted in $3.6 million in savings, proving the direct line between smarter care and a healthier bottom line.
These examples aren't science fiction. They show that AI is a set of practical tools ready to solve today’s biggest healthcare challenges. By automating tedious work and delivering deep insights, this technology empowers organizations to build a more efficient, resilient, and truly patient-centered system.
How to Measure What Truly Matters in Optimization
Without the right metrics, care delivery optimization is just a feel-good buzzword. To make your strategy real, you need a way to track what’s working and what isn’t. We have to move past vague ideas of "improvement" and build a culture that can point to hard numbers and prove the value of every single initiative.
This means setting up Key Performance Indicators (KPIs) that cover the three pillars of a healthy organization: operational efficiency, financial stability, and clinical quality. These metrics become the common language for everyone—from the C-suite to the frontline staff—to understand progress and justify future investments. Of course, this is impossible without the right internal tooling to give you real-time dashboards and show a clear return on every dollar spent.
Operational Efficiency Metrics
Operational KPIs get into the nitty-gritty of your daily workflow. They show you how smoothly your hospital or clinic is actually running and shine a spotlight on the friction points that burn through time, money, and staff morale. Fixing these is the first step to creating a better environment for everyone.
A few good places to start are:
Average Patient Wait Times: How long is a patient sitting in the waiting room after check-in before they see a provider? Long waits are a dead giveaway that you have a scheduling or staffing bottleneck.
Bed Turnover Rate: Once a patient is discharged, how fast can that bed be prepped and ready for the next person? Slow turnover is a classic sign of process snags that tie up your available capacity.
Operating Room Utilization: What percentage of your scheduled OR time is actually used for surgery? Every unused minute is a missed opportunity for both revenue and patient care.
Financial Health Metrics
Financial KPIs give you an honest look at your organization's bottom line. They measure how well you're managing costs, bringing in revenue, and plugging financial leaks. After all, a solid financial footing is what allows you to keep investing in top-tier clinical care and new innovations.
A strong financial dashboard isn't a nice-to-have; it's essential. It connects the dots between operational changes and financial impact, proving that optimization isn't just another cost—it’s how you create lasting value.
Key financial metrics to watch closely include:
Claim Denial Rate: What percentage of your claims are being kicked back by payers? Anything above 5% is a red flag, pointing to problems with documentation, coding, or billing that need fixing now.
Average Cost Per Discharge: What’s the all-in cost for a patient's entire stay? This metric is fantastic for spotting inconsistencies in care protocols and finding smart ways to standardize without sacrificing quality.
Days in Accounts Receivable (A/R): How long does it take you to get paid? High A/R days can seriously strain your cash flow and point to big inefficiencies in your revenue cycle.
Clinical Quality and Patient Experience Metrics
At the end of the day, the whole point of care delivery optimization is to help patients get better. These KPIs measure how your efforts are directly impacting the quality of care and how patients feel about their experience. They are the ultimate proof that all your operational and financial tweaks are actually leading to better health outcomes.
The must-haves for clinical and experience metrics are:
Hospital Readmission Rates: What percentage of your patients are back in the hospital within 30 days of being sent home? This is a core indicator of how well your care coordination and discharge planning are working.
Hospital-Acquired Condition (HAC) Rates: How often are patients developing infections or other conditions while under your care? Driving this number down is a direct reflection of your patient safety protocols.
HCAHPS Scores: These standardized surveys are a goldmine of direct patient feedback on everything from nurse communication to hospital cleanliness. They give you an unfiltered look into the patient’s journey.
Tracking progress in care delivery optimization requires a balanced view across operations, finance, and clinical quality. The table below outlines a core set of KPIs that provide a comprehensive snapshot of performance, helping leaders pinpoint successes and identify areas needing more attention.
Essential KPIs For Care Delivery Optimization
| Domain | Key Performance Indicator (KPI) | What It Measures |
|---|---|---|
| Operational Efficiency | Average Patient Wait Times | The time from patient check-in to being seen by a clinician, indicating scheduling and staffing effectiveness. |
| Bed Turnover Rate | The speed at which a patient bed is made available for the next patient, reflecting process efficiency. | |
| Operating Room Utilization | The percentage of available OR time used for procedures, highlighting scheduling and resource management. | |
| Financial Health | Claim Denial Rate | The percentage of claims rejected by payers, signaling revenue cycle issues. A rate above 5% is problematic. |
| Average Cost Per Discharge | The total cost of a patient's entire hospital stay, used to identify care variations and cost-saving opportunities. | |
| Days in Accounts Receivable (A/R) | The average number of days it takes to collect payments, reflecting cash flow and billing efficiency. | |
| Clinical Quality & Patient Experience | 30-Day Readmission Rate | The percentage of patients readmitted within 30 days, measuring care coordination and post-discharge support. |
| Hospital-Acquired Condition (HAC) Rate | The frequency of conditions developed during a hospital stay, indicating patient safety protocol effectiveness. | |
| HCAHPS Scores | Standardized patient satisfaction survey results, providing direct feedback on the patient's care experience. |
By consistently monitoring these metrics, healthcare organizations can create a data-informed feedback loop. This ensures that every optimization initiative is not just an isolated project but a measurable step toward a more efficient, financially sound, and patient-centered system.
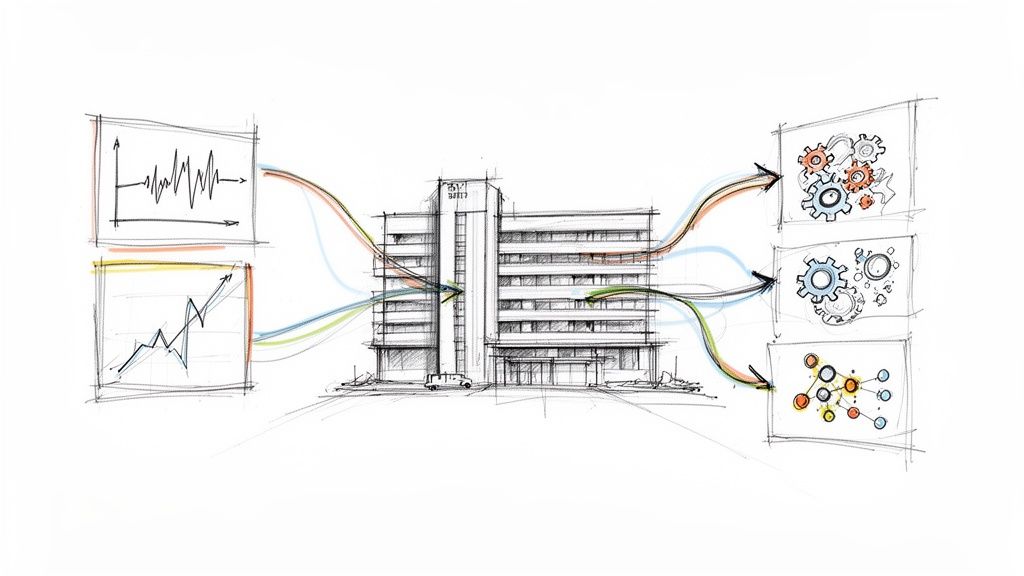
Your Strategic Roadmap to AI-Powered Optimization
Trying to overhaul something as complex as care delivery optimization can feel overwhelming. The secret isn't a single, massive project. Real success comes from a clear, phased roadmap that guides your organization from a smart idea to a system-wide reality. A manageable, step-by-step process takes the risk out of the investment, builds momentum, and makes sure every stage delivers real, measurable value.
This whole journey kicks off with a solid Discovery and Strategy phase. As we explored in our AI adoption guide, this is all about looking before you leap. It means doing a thorough AI requirements analysis to find the opportunities that will give you the most bang for your buck and getting the right clinical and administrative leaders on board from day one.
Phase 1: Discovery and Strategy
This first step is everything. It's where you lay the groundwork for all the work that follows. The goal here isn't to just pick some flashy technology; it's to get a deep, honest understanding of the problems you actually need to solve. I’ve seen organizations rush this stage, and it almost always leads to them investing in a solution that doesn’t quite fit their core operational needs.
A proper discovery process involves a few key things:
Workflow Mapping: You have to go beyond what you think is happening and map out your actual clinical and administrative workflows. This is how you find the specific bottlenecks, redundant steps, and manual tasks that are eating up time and money.
Stakeholder Interviews: Go talk to the people doing the work—the nurses, doctors, schedulers, and billing staff. Their on-the-ground insights are pure gold for pinpointing the real-world friction points that sophisticated AI tools for business are designed to fix.
Data Readiness Assessment: Take a hard look at your data. How good is it? Is it accessible? Can your systems talk to each other? You can't optimize what you can't measure, so getting a clear picture of your data landscape is non-negotiable before you even think about building an AI model.
By the end of this phase, you should have a prioritized list of potential projects and a solid business case for each one, all backed by expert AI strategy consulting. This data-first approach ensures you’re aiming your efforts where they’ll make the biggest impact, right from the start.
Phase 2: Pilot and Validation
With a clear strategy in your back pocket, it’s time to prove the concept with a controlled pilot program. Think of a pilot as a small-scale, real-world test. It's designed to confirm your chosen solution works as expected and to help you iron out any kinks before you bet the farm on a full-scale rollout. It's your chance to learn fast and fail small.
For example, if you’ve figured out that patient no-shows are a huge problem, you could pilot a predictive scheduling tool in just one department. During this test run, you'd keep a close eye on KPIs like the no-show rate, appointment wait times, and what the staff thinks. This focused experiment gives you the hard data you need to prove the ROI and build confidence across the organization.
The key to a successful pilot is setting clear success criteria before you even start. What specific metric needs to move the needle for this to be considered a win? Answering that question lets you make a clear-headed decision on whether to scale it up, tweak it, or move on.
Many health systems find that telehealth and site-of-care optimization are great candidates for pilot programs. These tech-driven models have already achieved an 84 percent reduction in specialist wait times and contribute to $42 billion in annual industry savings, showing they can deliver a rapid, measurable impact.
Phase 3: Implementation and Scaling
Once your pilot has proven its worth, it's go-time. This is the implementation and integration phase. But it’s about so much more than just flicking a switch on new technology; it's about weaving the new solution into the very fabric of your organization. This is where you need a flexible and iterative AI Product Development Workflow that can adjust as you get feedback from the people actually using it.
This timeline shows how the metrics you focus on will naturally evolve as your optimization strategy matures—starting with operational fixes and building toward broader clinical and financial gains.
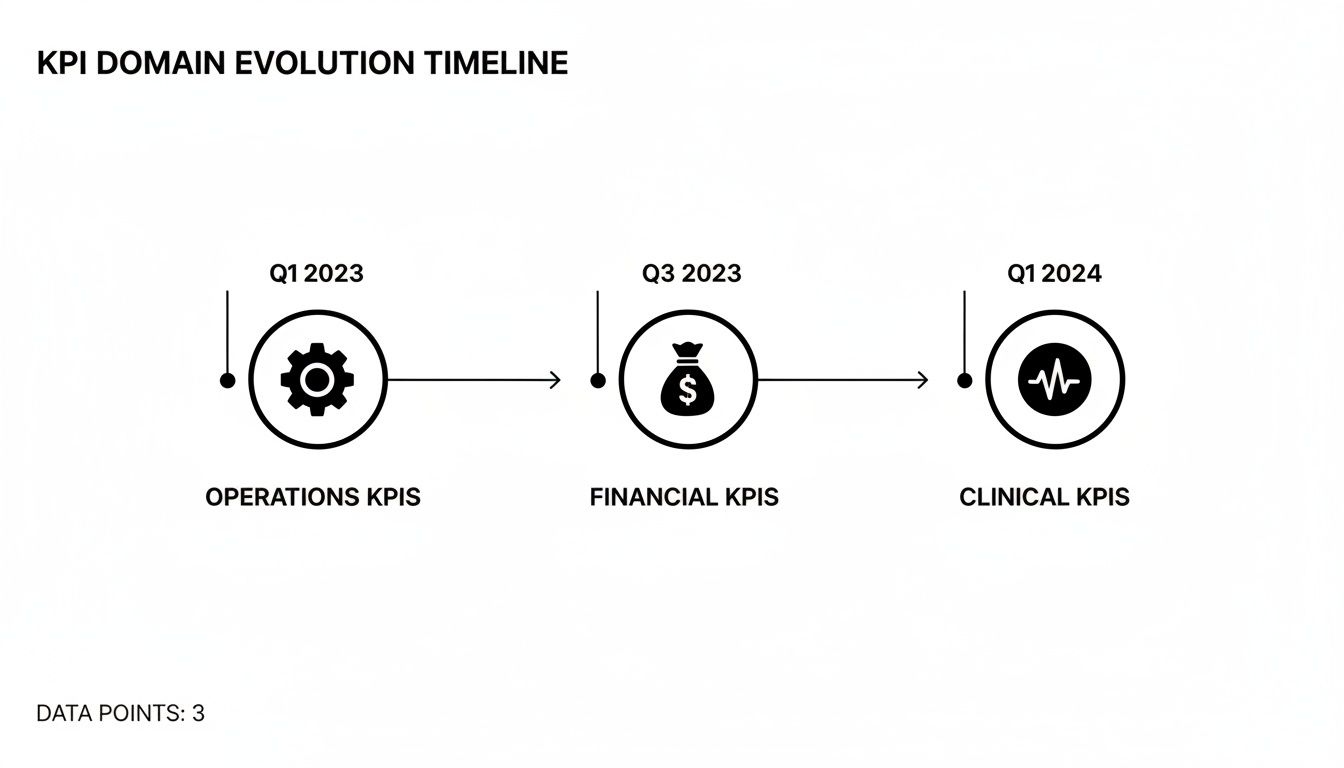
As you can see, the initial wins are often operational. Those early successes then create the foundation you need to achieve the really significant financial and clinical improvements down the line.
Scaling effectively really comes down to three things:
Robust Training Programs: Make sure everyone who will touch the new system is comfortable and skilled with the new tools and workflows.
Change Management: Don't just tell people what is changing; tell them why. When you highlight the benefits for both staff and patients, you'll see adoption skyrocket.
Continuous Monitoring: Keep a close watch on the KPIs you established from the start. This ensures the solution keeps delivering value and helps you spot new opportunities for improvement.
By following this phased approach, your organization can navigate the tricky waters of transformation with confidence. It turns ambitious goals for care delivery optimization into results you can see and measure, ensuring you build a solid foundation, prove value at every step, and achieve an impact that lasts.
Partnering for Success on Your Optimization Journey
Let’s be honest: tackling care delivery optimization and diving into healthcare AI is a massive undertaking. It’s not just about buying new software. You're dealing with entrenched workflows, complex data systems, and the immense challenge of managing change. This is where having the right partner makes all the difference, helping you move from a good idea to a real-world execution with speed and confidence.
We get it. Healthcare doesn't wait. That's why our approach is built for agility. We can deliver a tailored Custom AI Strategy report in just a few weeks, not months. This initial deep dive gives you a clear, data-backed foundation for your entire project, cutting straight to the chase and accelerating your path to real value.
From Strategy to Scaled Impact
Our support doesn't stop at the strategy session. We're with you for the entire journey. We kick things off with our AI Strategy consulting tool to pinpoint the most promising opportunities and lay out a clear roadmap. From there, our flexible AI Product Development Workflow ensures that new solutions fit right into your existing systems without causing chaos.
Think of it as a de-risked path to success. You don't need to spin up an entire AI department overnight. By working with our expert team, you can start making a real impact much faster. We work hand-in-hand with your people, boosting their capabilities and making sure every project is built on solid ground.
The right partnership transforms an ambitious goal into an achievable reality. When you combine your deep clinical expertise with our AI strategy and execution capabilities, you can build a more resilient, efficient, and patient-centric organization—minus the long timelines and heavy upfront investment.
To get the most out of any new technology, your foundational infrastructure has to be rock-solid. Exploring comprehensive IT services for health care organizations can provide that crucial backbone, ensuring your systems are primed and ready for advanced tools. For specialized needs, we also bring in trusted partners in custom healthcare software development to bring even the most complex visions to life.
Frequently Asked Questions
What's the First Step in Optimizing Care Delivery?
Before you even think about technology, the first step is always to take a hard, honest look at where you are right now. You need to map out your current workflows, figure out what's causing the biggest headaches and delays, and then decide what success actually looks like for your organization. We call this an AI requirements analysis. It's about digging into the data you have, talking to the people on the front lines—your clinical and administrative staff—and getting a clear picture of reality. From there, you can identify the handful of opportunities where change will make the biggest difference. A Custom AI Strategy report is the perfect tool for this, giving you a solid, data-backed plan to build on.
How Is AI-Driven Optimization Different from Traditional Methods?
Traditional process improvement, using methods like Lean or Six Sigma, is great. But it often depends on manual analysis and can be slow, especially when you're dealing with massive amounts of complex data. It creates static, one-size-fits-all fixes. AI takes this to a whole new level. It can analyze thousands of data points in real-time to spot patterns a human simply couldn't. For instance, instead of just giving every patient the same discharge checklist, an AI model can identify the specific patients who have a high risk of readmission. This lets you intervene proactively with targeted support, moving from a rigid protocol to a dynamic, personalized approach.
What Are the Biggest Implementation Hurdles?
Honestly, the technology is rarely the hardest part. The real challenges are almost always about people and processes. We see three main roadblocks pop up again and again:
Data Silos: Critical patient information is often locked away in different systems—the EHR, billing, labs—that don't talk to each other.
Change Management: Getting your team on board is crucial. If they don’t understand the "why" behind the new workflows or see how it makes their lives easier, they'll resist.
Integration Complexity: Any new AI tools for business have to fit into your existing ecosystem without a hitch. If they just create more clicks and logins, you've made the problem worse, not better.
Navigating these issues is where an expert team with experience in healthcare transformation becomes invaluable.
How Can We Measure the ROI of These Initiatives?
Measuring your return on investment isn't just about one number; you need to look at a mix of financial, operational, and clinical metrics. You have to establish your baseline before you start so you can prove the impact later. For financial ROI, look at direct cost savings from things like reduced staff overtime or less supply waste, plus revenue boosts from fewer denied claims. Operationally, you'll see it in shorter patient wait times, decreased length of stay, and better use of your operating rooms. Most importantly, the clinical ROI shows up in what matters most: better patient outcomes. This means tracking metrics like lower readmission rates and improved patient satisfaction scores.