Hospital Operational Intelligence: A Guide to Building a Smarter Hospital
Discover how hospital operational intelligence boosts patient care and efficiency through AI-driven insights and streamlined operations.
Imagine a hospital that runs with the precision of a Swiss watch. Patients move smoothly from admission to discharge, vital resources are always in the right place at the right time, and staff can see a problem coming long before it ever happens. This isn't a futuristic dream; it's the reality made possible by hospital operational intelligence (OI).
At its core, OI is a strategic approach that combines real-time data, analytics, and AI to give leaders a living, breathing view of their entire organization, moment by moment.
Understanding Hospital Operational Intelligence
Think of it this way: managing a hospital without OI is like trying to navigate a bustling city with a static paper map. You can see the streets, but you have no idea about the traffic jam just around the corner or the detour that just opened up. You’re constantly reacting.
Hospital operational intelligence is the upgrade to a live GPS with predictive traffic alerts. It allows you to anticipate bottlenecks in the emergency department, optimize surgical schedules based on real-time demand, and allocate life-saving equipment with incredible efficiency. It’s about shifting from reactive chaos to proactive, predictable control.
This isn't just another reporting tool that tells you what happened last week. An OI system shows you what's happening right now and uses that data to forecast what’s likely to happen next. This power to see around the corner enables immediate, data-backed decisions that make a real difference in patient outcomes and the hospital's financial health.
Core Components of Hospital Operational Intelligence
A robust OI system isn't a single piece of software you install. It’s more like an integrated ecosystem of technologies designed to work together. Its main job is to smash the data silos that have long kept clinical, financial, and administrative departments from seeing the whole picture. By creating one unified view, OI establishes a single source of truth that everyone can rely on.
This table breaks down the foundational pillars of a hospital OI system.
| OI Component | Primary Function | Key Benefit |
|---|---|---|
| Real-Time Data Integration | Continuously pulls live data from EHRs, admission systems, pharmacy, labs, and even IoT sensors on medical equipment. | Creates a complete, up-to-the-minute operational picture. |
| Predictive Analytics | Uses AI and machine learning to forecast patient volumes, flag at-risk patients, or predict equipment maintenance needs. | Moves decision-making from reactive to proactive. |
| Interactive Dashboards | Translates complex data into intuitive, visual charts and graphs that display key performance indicators (KPIs) at a glance. | Enables quick, informed decisions for leadership and frontline staff. |
| Automated Alerts | Pushes instant notifications to the right people when critical thresholds are met (e.g., ICU capacity hits 90% or ER wait times exceed targets). | Triggers immediate action to prevent problems from escalating. |
These components work in concert to deliver a holistic, intelligent operational framework.
Understanding how these elements connect is key. For example, OI can dramatically improve processes like Revenue Cycle Management (RCM) by identifying billing bottlenecks in real-time. The ultimate objective is to build a healthcare environment that is more responsive, highly efficient, and laser-focused on the patient.
Harnessing this technology effectively is where specialized expertise comes in. A well-defined strategy, often supported by Healthcare AI Services, helps facilities unlock this new level of operational command and clarity.
Why You Can't Afford to Ignore Operational Intelligence
In healthcare today, if you're standing still, you're already falling behind. Adopting hospital operational intelligence (OI) isn't some futuristic, nice-to-have project anymore—it's a fundamental requirement for staying competitive. Hospitals that get this right shift from a constant state of putting out fires to one of proactive, data-informed control. That's a massive advantage, not just for patient care but for financial survival.
This is about moving beyond guesswork and gut feelings to make decisions that deliver real, measurable returns. When you have a unified, real-time view of everything happening in your facility, you can finally make smarter calls that directly impact the bottom line. It's about turning a flood of data into real dollars by systematically plugging the leaks that drain your resources and drive up costs.
Strengthen Your Financial Health
The first and most obvious win from operational intelligence is on your balance sheet. Think of OI as a high-powered lens that reveals hidden opportunities to save money and find new revenue that were completely buried in disconnected data systems.
Here’s where you’ll see the financial gains:
- Slash Operational Waste: By truly understanding patient flow and how your resources are being used, you can pinpoint and fix the bottlenecks that cause expensive equipment and skilled staff to sit idle.
- Maximize High-Value Assets: OI ensures that critical resources—like your operating rooms and MRI machines—are running at peak capacity, which directly boosts revenue.
- Fine-Tune Revenue Cycle Management: With real-time monitoring of billing and claims, you can catch errors before they turn into costly denials. This means faster reimbursement cycles and much healthier cash flow.
These aren't just abstract ideas. Recent data shows hospitals using AI-driven operational workflows are seeing a return on investment of $3.20 for every $1 spent, often getting there in just 14 months. It's no wonder that 80% of hospitals are now turning to AI to make their operations more efficient and improve care.
Elevate Patient Care and Staff Satisfaction
Beyond the numbers, operational intelligence dramatically improves the day-to-day experience for both patients and staff. Let's be honest: a hospital that runs like a well-oiled machine is a much better place to receive care and a far less stressful place to work. As hospitals adopt these advanced systems, navigating complex regulations becomes even more critical. A good HIPAA Compliance Guide for Healthcare Providers is essential for protecting patient data in this new environment.
By transforming raw data into predictive insights, OI allows hospitals to anticipate patient needs rather than just reacting to them. This proactive stance is the cornerstone of modern, high-quality healthcare delivery.
This shift translates into real-world improvements everyone can feel:
- Shorter Wait Times: Predictive models can forecast patient arrivals, helping you staff the emergency department appropriately and create a much smoother admissions process.
- Faster Bed Turnover: OI systems know when a patient is about to be discharged and can automatically coordinate housekeeping and transport, getting that bed ready for the next person in record time.
- More Balanced Workloads: By automating tedious administrative tasks and helping create more predictable schedules, OI is a powerful tool in the fight against the staff burnout that causes high turnover.
Ultimately, facilities driven by operational intelligence are simply more resilient, agile, and ready for whatever comes their way. Our Healthcare AI Services are designed to help you achieve these very real returns, turning your operational data from a headache into your greatest strategic asset.
Peeking Under the Hood: How an OI System Actually Works
To really grasp the power of hospital operational intelligence, you have to look under the hood. The architecture might seem complex at first, but it's really just a highly organized data pipeline, built to turn a chaotic flood of raw information into crystal-clear insights for decision-makers.
Think of it like a city's water supply. You have countless small streams and reservoirs (your data sources) all feeding into a central processing plant (the data hub). There, the water is filtered and purified (the data is processed and analyzed). Finally, it’s delivered through a network of pipes (dashboards and alerts) right to the homes where it's needed. An OI system does the very same thing, but with hospital data.
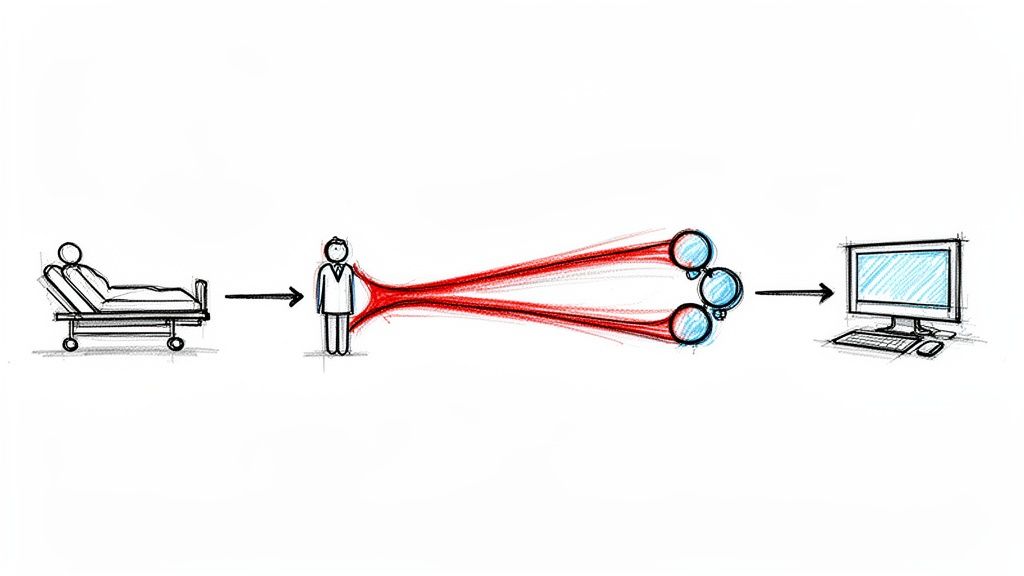
The Foundation: Pulling All Your Data Together
An effective OI system starts by collecting data from every single corner of the hospital. These different sources are the lifeblood of operational intelligence; without bringing them together, you're always looking at an incomplete picture.
Here are the usual suspects:
- Electronic Health Records (EHRs): The core of all clinical information, holding patient histories, diagnoses, and treatment plans.
- Admission, Discharge, Transfer (ADT) Systems: Live feeds that track every patient's journey through the hospital, which is absolutely critical for managing bed capacity.
- Pharmacy and Lab Systems: Crucial data on medication administration and test results that directly impact patient flow and resource planning.
- Financial and Billing Platforms: The money side of things—information on claims, payments, and the entire revenue cycle.
- IoT Sensors: Real-time data streaming from medical equipment like infusion pumps or ventilators, helping you monitor usage and predict maintenance needs.
This mix of data gets pulled together in two main ways. Real-time data streaming grabs information the second it’s created, which is essential for immediate alerts—like notifying a team that ICU capacity just hit 95%. At the same time, ETL (Extract, Transform, Load) processes work in the background, gathering historical data for deeper analysis to spot those long-term trends. All of this unified data lands in a central data warehouse, creating a single, reliable source of truth.
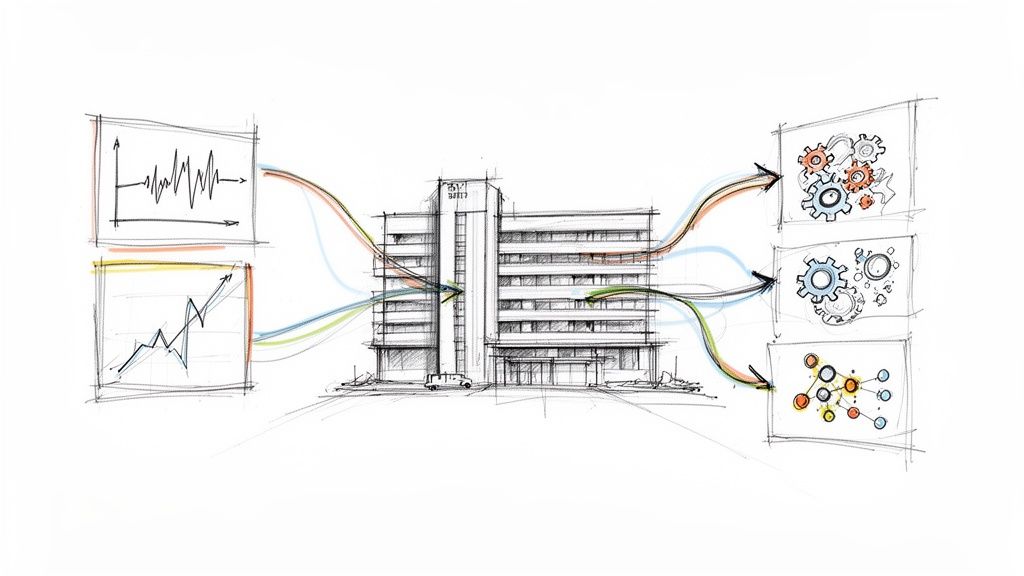
This diagram shows how operational intelligence creates a positive feedback loop for finances, patient care, and staff.
As you can see, when the hospital's finances improve, it directly enables better patient care, which in turn leads to a more sustainable and satisfied workforce.
The Engine: Analytics and Actionable Outputs
Once all the data is in one clean, central place, the real magic begins. This is the analytics layer, where advanced tools—including AI and machine learning—go to work. These algorithms sift through terabytes of data, uncovering patterns and connections that would be completely invisible to the human eye. This is where modern AI solutions can make a massive difference, turning past performance into predictive power.
For instance, an AI model could analyze years of ADT data to accurately forecast emergency department admissions for the coming weekend, letting you adjust staffing levels before the rush hits. Building these kinds of predictive tools often involves creating specialized internal tooling that integrates smoothly with your existing hospital systems. Thinking ahead like this is a core part of any good AI strategy consulting.
The final step is the output layer, which is all about getting these valuable insights to the right people at the right moment. We're not talking about emailing dense spreadsheets here. It’s about delivering clear, intuitive information that triggers immediate action.
The goal of an OI system's output is not just to inform, but to empower. It translates complex analytics into simple directives that frontline staff and administrators can act on instantly.
This typically happens in two ways:
- Interactive Dashboards: These are the visual command centers for administrators and department heads, displaying key performance indicators (KPIs) in real-time. A manager can see operating room utilization, wait times, and staffing levels all in one glance.
- Automated Alerts: These are instant notifications sent directly to clinical staff. A nurse might get a ping on their mobile device that a patient’s vital signs are trending downward, giving them a critical head-start on intervention.
This complete architecture—from raw data collection to actionable output—is what makes hospital operational intelligence such a powerful force for change.
Tracking Success with the Right KPIs
So, you've invested in hospital operational intelligence. Now what? The real test isn't just implementing the technology; it's proving its worth. To do that, you need to track the right Key Performance Indicators (KPIs). Think of these metrics as the vital signs of your hospital's operational health, turning a whirlwind of daily activities into clear, hard numbers.
Without a solid KPI framework, you’re essentially flying blind. You might have a gut feeling that things are improving, but you won't be able to prove it to the board or pinpoint exactly which changes are making a difference. The goal is to get past anecdotes and anchor your success story in undeniable data.
A well-defined set of metrics gives leaders the evidence they need to show real value from their OI initiatives. More importantly, it creates a shared language for success, getting clinical, administrative, and financial teams all pulling in the same direction.
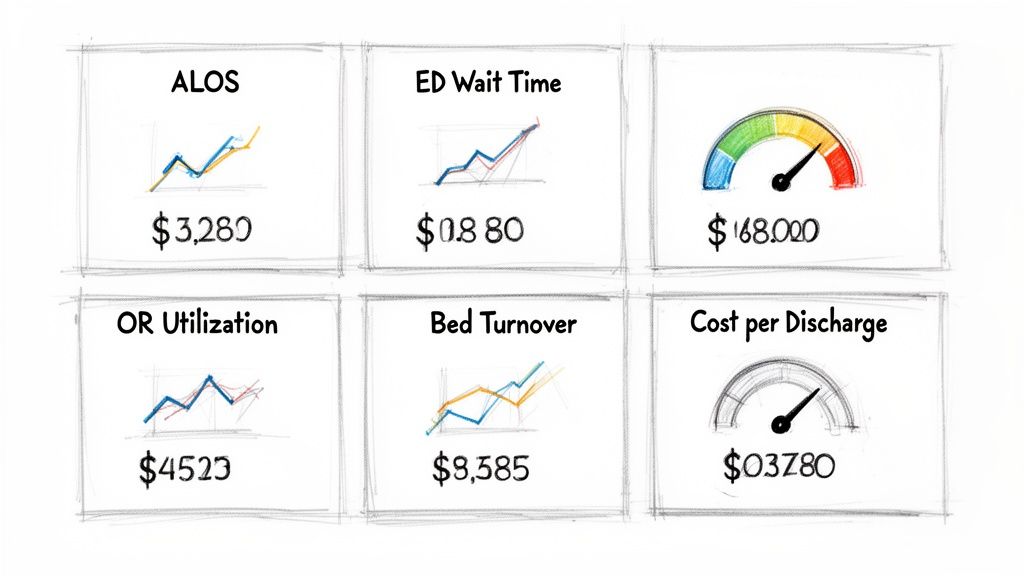
To get a clear picture of performance, it's helpful to group KPIs by the area of the hospital they measure. This table breaks down some of the most critical metrics you should be watching.
Essential KPIs for Hospital Operational Intelligence
| Category | Key Performance Indicator (KPI) | What It Measures |
|---|---|---|
| Patient Flow & Throughput | Average Length of Stay (ALOS) | The average number of days a patient is in the hospital. Shorter stays (when safe) mean more efficient care. |
| Patient Flow & Throughput | Emergency Department (ED) Wait Times | The time from a patient's arrival to being seen by a clinician, a key indicator of front-door efficiency. |
| Patient Flow & Throughput | Bed Turnover Rate | How quickly a bed is ready for the next patient after discharge. High rates show great team coordination. |
| Resource Management | Operating Room (OR) Utilization | The percentage of available OR time used for surgeries. Higher utilization directly boosts revenue. |
| Resource Management | Medical Equipment Uptime | The percentage of time critical equipment (e.g., MRI) is operational and available for patient care. |
| Resource Management | Staff-to-Patient Ratios | Real-time monitoring of staffing levels per unit to ensure patient safety and prevent staff burnout. |
| Financial Health | Claim Denial Rate | The percentage of insurance claims rejected by payers. A low rate means accurate billing and better cash flow. |
| Financial Health | Cost Per Discharge | The average total cost of caring for a patient from admission to discharge. OI helps find cost-saving opportunities. |
| Financial Health | Revenue Cycle Length | The time it takes to get paid after providing a service. A shorter cycle is crucial for financial stability. |
Tracking these KPIs provides a balanced view, ensuring that improvements in one area—like speeding up discharges—don't negatively impact another, such as patient safety or staff workload.
Patient Flow And Throughput Metrics
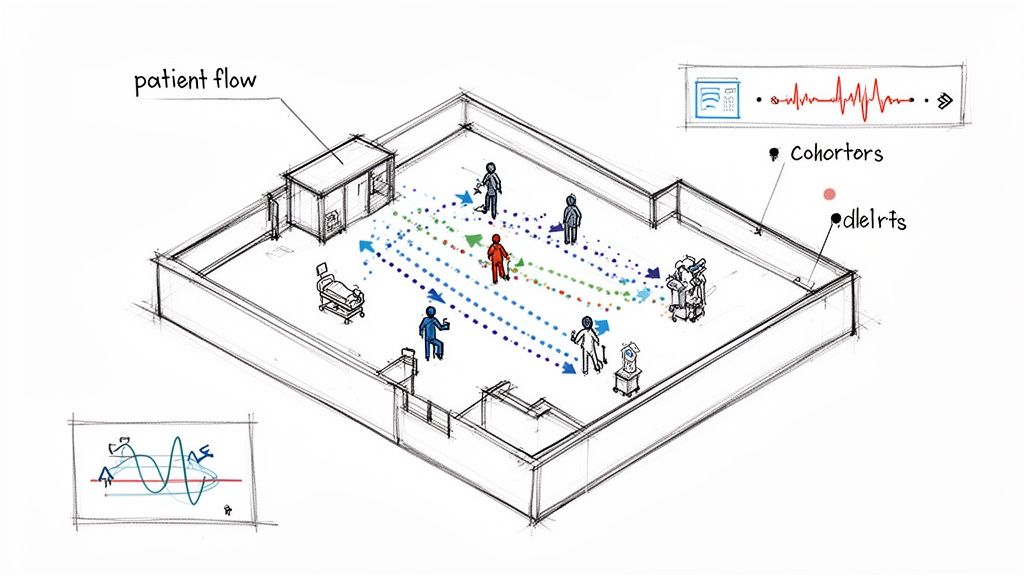
The patient journey is the very heart of your hospital's operations. When that journey is smooth and efficient, care gets better, satisfaction climbs, and you make the most of your facility's capacity. Any slowdown or bottleneck here creates a ripple effect that touches every other department.
Look closely at these numbers:
- Average Length of Stay (ALOS): This tracks the average time a patient spends in a hospital bed. When you can safely reduce ALOS, it's a clear sign of efficient care delivery and helps free up beds much faster.
- Emergency Department (ED) Wait Times: Measuring the time from when a patient walks in the door to when they see a provider is a raw, honest look at your front-door efficiency and the patient experience.
- Bed Turnover Rate: This KPI reveals how quickly a bed is cleaned, prepped, and made available after a patient is discharged. A fast turnover is a testament to incredible coordination between your clinical, transport, and housekeeping teams.
Boosting these metrics doesn't just look good on a report; it directly improves the patient experience and allows your hospital to care for more people without needing to build new wings.
Resource Management And Utilization Metrics
Hospitals are packed with incredibly expensive, life-saving resources—from state-of-the-art surgical suites to your highly trained specialists. Making sure these assets are used effectively is non-negotiable for both your bottom line and the quality of care you provide. Operational intelligence finally gives you the visibility to squeeze every drop of value from them.
Key metrics to watch in this area include:
- Operating Room (OR) Utilization: This calculates the percentage of scheduled OR time that is actually used for procedures. Every percentage point increase here is a direct line to more revenue.
- Medical Equipment Uptime: For critical gear like MRI scanners and ventilators, this tracks the time they are up and running versus down for maintenance. High uptime ensures these tools are always ready when a patient needs them.
- Staff-to-Patient Ratios: With OI systems, you can monitor these ratios in real time across every unit. This helps managers deploy staff to maintain safe levels and prevent burnout by balancing the workload.
Financial Health And Revenue Cycle Metrics
At the end of the day, a hospital has to stay financially healthy to continue its mission. Operational intelligence is a powerful ally in monitoring and improving financial performance by untangling the notoriously complex revenue cycle. A dedicated tool, like a financial insights dashboard, can bring all these numbers into one place for a clear, immediate view.
Keep a sharp eye on these financial KPIs:
- Claim Denial Rate: This is the percentage of claims that payers reject. A low denial rate is a huge win, indicating your billing and coding are accurate and your cash flow is strong.
- Cost Per Discharge: This metric averages out the total cost to care for one patient, from admission all the way to discharge. OI is brilliant at helping you spot the hidden inefficiencies that quietly drive this number up.
- Revenue Cycle Length: This measures the time between providing a service and actually getting paid for it. The shorter that cycle, the faster cash comes in, which is vital for the hospital's liquidity.
Building Your Implementation Roadmap
Putting a hospital operational intelligence (OI) system in place isn't like flipping a switch. It's a strategic journey, one you take in deliberate, well-planned phases. A solid roadmap is your best friend here—it helps you navigate the tangled web of data integration, new technology, and cultural shifts. It's the key to making sure this initiative delivers real, lasting value instead of ending up as another project collecting dust on a shelf.
Your first move is to build a strong foundation. This means getting your data governance policies in order from the get-go to ensure every piece of information feeding the system is accurate, secure, and reliable. At the same time, you'll need to pull together a cross-functional team. Get leaders from IT, clinical departments, finance, and administration in the same room. You need their perspectives and their support to champion the project across the entire organization.
Phase 1: Launching a Strategic Pilot Project
With your governance and team ready, it's time to launch a pilot project. The whole point here is to show value fast and get people excited. Forget about a massive, hospital-wide overhaul right away. Instead, pick one specific, high-impact area where you know there are inefficiencies and where you can show measurable improvement.
Good candidates for a pilot project usually include:
- Optimizing Surgical Scheduling: Zero in on getting the most out of your operating rooms. Focus on cutting down idle time between procedures and making the pre-op workflow as smooth as possible.
- Streamlining Patient Discharges: Tackle the communication breakdowns between doctors, the pharmacy, transport, and housekeeping. The goal is to lower the average length of stay and get beds ready for the next patient faster.
- Improving Emergency Department Flow: Concentrate on slicing down wait times and fine-tuning patient triage. This is a win for both patient satisfaction and the quality of care.
A successful pilot is your ticket to getting everyone else on board. It gives you a real success story to share, proving that hospital OI isn't just a buzzword—it works.
Phase 2: System Integration and Change Management
Once your pilot has proven its worth, you can shift your focus to the bigger picture: integrating more systems and, crucially, managing the human side of this change. This is when you start connecting the OI platform to a wider array of data sources—think legacy EHRs, financial systems, and software from other departments.
But remember, the best tech on the planet is useless if your staff won't use it. This is where change management comes in. It's the art of getting your people ready for a new way of working.
An implementation roadmap isn't just about technology milestones. It’s a blueprint for cultural evolution, guiding your teams from their current state to a future where data-driven decisions are second nature.
Great change management boils down to a few practical steps:
- Develop Targeted Training Programs: Don't do generic training. Create role-specific sessions that show clinicians, administrators, and support staff exactly how these OI tools will make their jobs easier and more effective.
- Foster a Data-Driven Culture: Leaders have to walk the walk. When they consistently use OI dashboards in meetings and to make decisions, it sends a clear message: this is how we operate now.
- Communicate Early and Often: Keep everyone in the loop. Share progress, celebrate the small wins from the pilot, and be honest about the challenges and the rewards.
Phase 3: Scaling to an Enterprise-Wide Solution
The final phase is all about taking your successful pilot and scaling it into a full-blown, enterprise-wide system. You'll start rolling out the OI platform to other departments, plugging in new data sources, and finding new problems to solve. Following a proven AI Product Development Workflow ensures this expansion is organized and built to last.
The adoption of predictive AI in hospital operations has taken off, with 71% of nonfederal acute care hospitals in the US using it by 2024. But the growth isn't even. System-affiliated hospitals have hit 86% adoption, while independent facilities are trailing at just 37%. This gap really drives home the need for a smart scaling strategy, particularly in areas like billing automation, which saw a massive 25-point jump in just one year.
As you scale, you’ll see your system evolve. It will move beyond just descriptive analytics (what happened) and into predictive and prescriptive analytics (what will happen and what should we do about it). This is the moment your hospital stops just reacting to operational issues and starts proactively shaping them with genuine foresight. That’s when you know your hospital operational intelligence initiative has truly succeeded.
Navigating the Bumps in the Road to Implementation
Let’s be honest: while the promise of hospital operational intelligence is exciting, getting there isn't always a straight line. The path is often littered with predictable—and preventable—hurdles. We're talking about everything from tangled, messy data to the simple, powerful force of human habit.
The key is to see these roadblocks coming. Hospitals that anticipate the challenges are the ones that sail through implementation, avoiding painful delays and proving the value of their investment much faster.
Wrestling with Data and Tech Headaches
The biggest technical headache is almost always data silos. For decades, hospitals have stored clinical, financial, and operational information in completely separate systems that don’t talk to each other. Trying to get a clear, complete picture of what's happening is like assembling a puzzle with pieces from ten different boxes.
On top of that, you have the problem of poor data quality. Incomplete records, inconsistent terms, and duplicate entries can poison your OI system from the start. After all, your insights are only as good as the data you feed the system.
The antidote is a solid data governance plan. This isn't just about rules; it's about clarity. It means you need to:
- Assign ownership: Someone needs to be officially responsible for the quality of each data set.
- Standardize the language: Make sure "patient discharge" means the same thing in every department and every system.
- Scrub your data clean: Set up automated checks to catch and fix errors before the information hits your OI platform.
Then there’s the challenge of old technology. Many hospitals are running on legacy systems that were never built to share data in real-time. The thought of a massive "rip and replace" project is enough to scare off any executive. A much smarter approach is to start small. Pick one area with a clear potential for a big win—like reducing ER wait times—and launch a pilot project. A quick, visible success makes it much easier to get the support and budget for a wider rollout.
Overcoming the "We've Always Done It This Way" Mindset
Here’s the thing: technology is often the easy part. The real work is in changing how people think and work. Your clinicians and staff have routines they've relied on for years. A new system, no matter how great, can feel like just one more thing added to an already overwhelming workload, or even a threat to their professional judgment.
This kind of cultural resistance can sink a project before it ever gets going. You have to be strategic about managing the human side of this change.
- Explain the "Why," over and over: Don’t just talk about efficiency. Show a nurse how it means less time charting and more time with patients. Explain to a surgeon how it prevents scheduling conflicts.
- Bring people in from the start: Involve the doctors, nurses, and schedulers who will actually use the system in the design and selection process. When people feel like they’ve helped build the solution, they become its biggest advocates.
- Shout about the wins: When your pilot project successfully cuts wait times or smooths out the surgical schedule, make sure everyone knows about it. Success stories are the best way to turn skeptics into believers.
A Custom AI Strategy report can be a huge help here. It acts as a roadmap, identifying potential resistance points and helping you craft a communication plan that speaks directly to the concerns of each group. This turns the process into a team effort, not a top-down mandate.
Don't forget that where a hospital is—both geographically and organizationally—matters. There are real gaps in adoption. For example, AI use is at 43.9% in metro-area hospitals but drops to just 17.7% in rural ones. Independent hospitals also face an uphill battle, with only 37% using predictive AI compared to 86% of those in large health systems. Knowing where you stand helps you build a realistic plan. You can read more about these AI adoption trends in U.S. healthcare.
FAQs About Hospital Operational Intelligence
Here are some of the most frequently asked questions we receive from healthcare leaders about implementing operational intelligence.
What is hospital operational intelligence?
Hospital operational intelligence (OI) is a data-driven approach that uses real-time analytics, AI, and integrated data from across the hospital to provide a live, comprehensive view of operations. This allows leaders to monitor performance, predict bottlenecks, and make proactive decisions to improve patient flow, resource management, and financial health.
How does operational intelligence differ from traditional hospital reporting?
Traditional reporting is retrospective; it tells you what happened last week or last month. Operational intelligence is real-time and predictive. It shows you what's happening right now and uses AI to forecast what is likely to happen next, enabling proactive intervention rather than reactive problem-solving.
What are the biggest benefits of implementing an OI system?
The primary benefits include:
- Improved Patient Flow: Shorter wait times, reduced length of stay, and faster bed turnover.
- Enhanced Resource Utilization: Maximizing the use of expensive assets like operating rooms and MRI machines.
- Stronger Financial Performance: Reduced operational waste, improved revenue cycle management, and lower claim denial rates.
- Increased Staff Satisfaction: More balanced workloads and less time spent on administrative tasks, which helps reduce burnout.
Is operational intelligence only for large hospital systems?
No, OI is scalable and beneficial for healthcare facilities of all sizes. While large systems have complex operations, smaller hospitals and clinics can gain significant efficiencies by focusing on specific high-impact areas, such as surgical scheduling or inventory management, through a targeted pilot project.
What is the first step to implementing hospital operational intelligence?
The first step is a thorough assessment of your current state. This involves identifying your biggest operational pain points and conducting an inventory of your existing data sources and systems. A detailed AI requirements analysis is crucial for creating a clear roadmap that aligns with your specific goals and challenges.
Ready to build a smarter, more efficient hospital? Ekipa AI provides the strategic foundation you need. We deliver expert AI strategy consulting that helps healthcare organizations like yours turn complex data into a powerful operational advantage. Contact our expert team today to learn more.