Healthcare Digital Transformation Strategy: A Practical Roadmap for Hospitals
Discover a practical healthcare digital transformation strategy that blends AI, data architecture, and proven change management into a clear actionable roadmap.

A healthcare digital transformation strategy isn't some futuristic nice-to-have anymore. It's a matter of survival. It means taking a hard look at how your health system actually runs and rebuilding it with smart technology to make patient care better, workflows smoother, and costs lower. This isn't just about new software; it's a direct response to creaking legacy systems, patients who expect more, and a workforce on the brink of burnout.
Why Going Digital Is No Longer Optional in Healthcare
For too long, the healthcare industry has lived a double life. We've seen incredible medical breakthroughs happen in the same buildings that still rely on fax machines and paper charts. That contradiction just isn't sustainable. People are used to managing their banking, shopping, and travel with a few taps on their phone, and they're starting to wonder why their healthcare experience feels stuck in the past.
The pressure isn't just coming from patients, either. Internally, health systems are getting crushed by rising operational costs and scary levels of clinician burnout. When doctors and nurses spend hours on repetitive administrative work, they're not spending that time with patients. It’s a massive drain on both the budget and morale.
The Urgency Has Reached a Tipping Point
Leaders across the industry see the writing on the wall. Digital initiatives are now the top priority for health systems worldwide, and it’s easy to see why. About 90% of C-suite executives believe the push for digital tech will only speed up in 2025.
The urgency is real because healthcare has been playing catch-up for years. To get a handle on the foundational tech needed for modern care delivery, this IT Services Healthcare Transformation Guide is an excellent primer. It's no wonder that around 70% of leaders are saying that investing in digital platforms is essential for their organization’s survival. This isn't just about updating servers; it's about redesigning the entire business to be more resilient, efficient, and focused on the patient.
A solid digital strategy is built on several core components that work together. From enhancing patient engagement to optimizing back-end operations, each pillar plays a critical role.
Table: Core Pillars of a Modern Healthcare Digital Strategy
| Pillar | Objective | Key Technologies |
|---|---|---|
| Patient Engagement | Empower patients with self-service tools and personalized communication. | Patient Portals, Telehealth, Mobile Apps, Wearables |
| Clinical Workflow | Free up clinicians from administrative tasks to focus on high-value patient care. | EHR/EMR Optimization, AI Scribes, Clinical AI |
| Operational Efficency | Automate repetitive back-office processes to reduce costs and errors. | Robotic Process Automation (RPA), AI-powered Billing |
| Data & Analytics | Turn raw data into actionable insights for better decision-making. | Cloud Data Warehouses, BI Dashboards, Predictive AI |
| Interoperability | Ensure seamless and secure data exchange between different systems. | APIs, FHIR Standards, Health Information Exchanges |
Ultimately, a truly effective strategy integrates these pillars into a cohesive whole, creating a system that's more than the sum of its parts.
The Strategic Power of Automation
At its heart, a smart digital transformation strategy is about one thing: automating the low-value, repetitive work so your highly skilled people can focus on the high-value, human work. Labor is almost always the biggest line item on a hospital's budget, which makes fixing inefficient workflows the biggest opportunity.
With intelligent automation, health systems can:
- Slash the Administrative Burden: Think about automating appointment scheduling, billing, and prior authorizations. The hours saved go directly back to patient-facing activities.
- Boost Clinical Efficiency: Give your clinicians tools that provide immediate access to patient data and simplify collaboration. This not only improves outcomes but also makes their jobs less frustrating.
- Create a Better Patient Experience: When patients can use digital tools to schedule appointments, talk to their care team, and see their own health records, they feel more in control and engaged.
- Unlock Insights from Data: A connected digital system generates a massive amount of data. Analyzing it reveals patterns that can improve population health and lead to more effective treatments.
Key Takeaway: Stop thinking of digital transformation as an IT project. It’s a core business strategy to overhaul operations, empower your staff, and meet the expectations of today’s patients. It's what will keep your organization viable for the long haul.
By bringing in technologies that solve these very real, everyday problems, you can start making meaningful change. Specialized Healthcare AI Services are a huge part of this, offering powerful ways to automate complex tasks and surface insights you could never see before. This is how technology stops being a cost center and starts driving better, more sustainable healthcare.
Building Your Strategic Framework for Maximum Impact
A solid digital transformation strategy in healthcare starts with a brutally honest look at where to focus your efforts. Vague goals like "improving efficiency" are useless. You need to zero in on specific, high-impact opportunities that deliver real results and build momentum for the long haul. That means getting your hands dirty and digging into your current processes to find the real pain points.
Kick things off with a deep dive into your clinical and operational workflows. I mean, map out everything—from the moment a patient first calls for an appointment to the final bill and follow-up. This exercise will shine a bright light on the bottlenecks: the chaotic scheduling systems, the mind-numbing billing cycles, the endless manual data entry. These aren't just minor headaches; they're huge drains on your resources and your team's morale.
The shift from these old, creaky systems to a new strategic approach is often driven by intense pressure, as this visual shows.
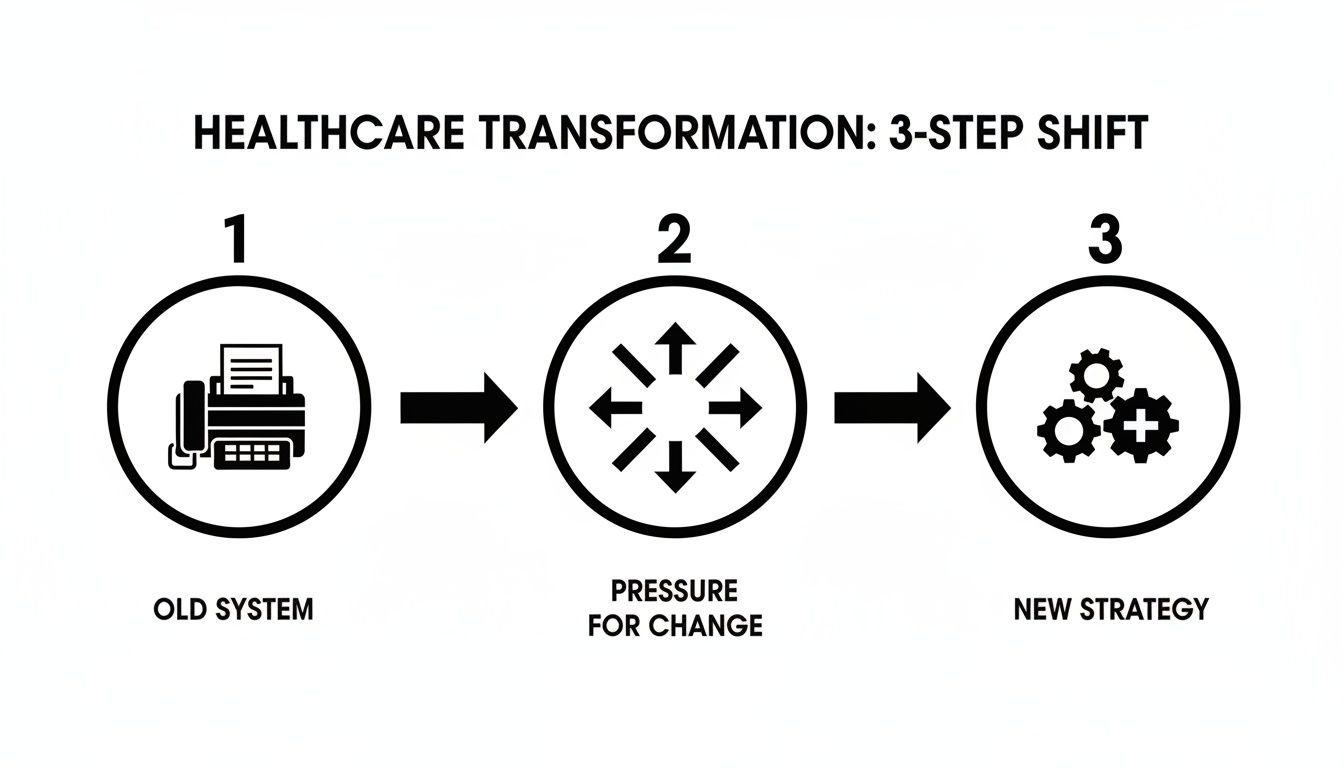
This diagram really gets to the heart of it. External pressures and internal breakdowns force a move away from legacy systems. To survive and grow, you have to adopt a structured, tech-forward strategy.
Prioritizing Your Transformation Initiatives
Once you've got a list of potential projects, you have to decide what to tackle first. Not all opportunities are created equal. A simple portal update might be an easy win, but will it have the same game-changing impact as an AI tool that helps slash diagnostic errors? You need a structured way to weigh each initiative to make smart decisions.
A prioritization matrix is perfect for this. It’s a simple but powerful tool that helps you score potential projects against what really matters to the business, ensuring you put your money and people where they’ll make the biggest difference.
Here are the kinds of criteria you should be evaluating each initiative against:
- Clinical Impact: Does it directly improve patient outcomes, enhance safety, or boost the quality of care?
- Efficiency Gains: How many hours will this save our clinicians and administrative staff every week?
- Financial ROI: What’s the real potential for cost savings or new revenue?
- Implementation Difficulty: What are the technical, financial, and cultural hurdles we'd have to clear?
This methodical approach stops you from getting distracted by low-impact "quick wins" and keeps the focus on advancements that truly move the needle.
Real-World Scenario: A hospital is weighing two projects: a cosmetic update to its patient portal versus implementing an AI-powered diagnostic tool for radiologists. The portal update is straightforward, but the AI tool scores off the charts on clinical impact and long-term ROI by helping spot early-stage cancers. The matrix makes the strategic choice obvious.
Creating a Targeted and Actionable Plan
With this framework in place, you can build a roadmap that's both ambitious and actually achievable. The goal is to sequence your projects to deliver tangible value fast. This proves the concept, silences the skeptics, and builds the buy-in you need from key stakeholders.
This is exactly where a well-defined strategy can be a game-changer, offering targeted solutions for your most pressing challenges. Instead of grabbing off-the-shelf software, you can pinpoint the exact features that will solve your unique problems—whether that’s automating prior authorizations or finally optimizing operating room schedules.
Your healthcare digital transformation strategy can't just be a document that gathers dust. It needs to be a living, practical blueprint for success.
Putting AI at the Heart of Your Healthcare Strategy
Artificial intelligence isn't some far-off concept for healthcare anymore; it’s the engine powering the most significant advancements happening today. When we talk about placing AI at the center of your healthcare digital transformation strategy, we’re not just talking about software updates. We’re talking about fundamentally rethinking how care is delivered—using smart technology to make everything from clinical diagnoses to back-office tasks faster, more accurate, and deeply interconnected.
AI, particularly generative AI, is changing the game on both sides of the healthcare coin. Administratively, it's about crushing the repetitive work that drains your staff's time, like sifting through billing codes or juggling appointment schedules. On the clinical side, it’s about giving doctors and nurses intelligent tools that serve up evidence-based insights right when they need them, helping them make quicker, more confident decisions at the point of care.
This shift is more than just an upgrade; it's a necessary evolution. AI is now a core component of healthcare's digital future, and generative AI is proving to be an especially powerful force. I've seen organizations move from simply automating isolated tasks to integrating AI across their entire ecosystem. The potential impact is staggering, with some projections showing up to a 40% improvement in healthcare outcomes from these kinds of interventions. And it's not just about patient care—AI is reshaping everything from how clinical trials are run to the way regulatory submissions are handled in pharma.
From Simple Automation to Intelligent Orchestration
The real magic of AI in healthcare happens when it connects disconnected processes and begins to orchestrate the entire patient journey. It’s no longer about using a single tool to fix a single problem. It's about building an intelligent, interconnected web that supports both patients and clinicians at every single touchpoint.
Just look at what’s already happening out in the field:
- Predictive Analytics for Proactive Care: AI algorithms are now sophisticated enough to scan thousands of electronic health records to flag patients at high risk for conditions like sepsis or heart failure. This gives care teams a crucial head-start, allowing them to intervene before a patient even shows obvious symptoms.
- AI-Powered Diagnostic Support: In radiology, AI has become an invaluable "second set of eyes." These tools can review medical images, highlighting potential abnormalities that a radiologist might miss during a long shift. It’s a powerful way to reduce human error and get diagnoses back faster.
- Optimized Hospital Operations: Forget guesswork. AI can accurately predict patient admission rates, which helps hospitals get ahead of bed capacity issues and staff scheduling. The result is shorter wait times and smarter allocation of your most valuable resources.
Key Insight: Let's be clear: the goal isn't to replace clinicians. It's to augment their expertise. AI does the heavy lifting with data, freeing up your human experts to focus on what they do best: complex decision-making, patient communication, and delivering compassionate care.
Demystifying AI and Making It Practical
Bringing AI into your organization doesn't have to be a massive, intimidating overhaul. The key is to start small by targeting specific, high-value problems and building momentum from there. The first step is to demystify the technology and show its practical power in solving real-world challenges. For healthcare leaders putting AI front and center, understanding how AI-powered software development can speed up the delivery of these new tools is a critical piece of the puzzle.
This is exactly where a model like AI Automation as a Service proves its worth. It gives you access to sophisticated AI capabilities without having to build a massive in-house data science team from the ground up. By zeroing in on practical applications that deliver immediate value—whether that’s reducing medical errors or fine-tuning supply chains—you start building the foundation for a smarter, more patient-centric system.
Laying the Right Technology and Data Foundation for the Future
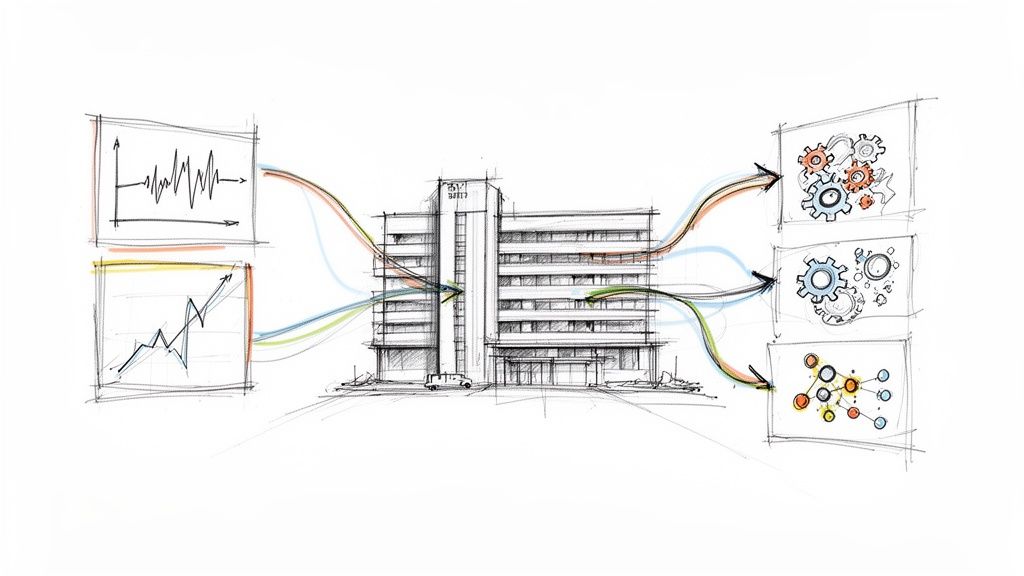
Your digital transformation strategy is only as good as the technology it runs on. You can have the most brilliant AI initiatives planned, but they will fall flat without a modern, scalable, and secure architecture underneath. The real goal here is to build a tech and data ecosystem that doesn't just solve today's problems but is flexible enough to handle whatever comes next.
One of the biggest hurdles I see holding health systems back is the mess of data silos. Over decades, we've bolted on countless systems—EMRs, lab software, billing platforms, and now data from wearables. This has created a fragmented nightmare where critical information is locked away, making it impossible to see a full patient journey or get any real value from analytics and AI solutions.

The only way forward is to create a unified data platform. Think of it as the central hub, the single source of truth that pulls all those different data streams together. This unified view is the absolute bedrock for the powerful analytics and AI applications you want to build.
Core Principles for an Agile Architecture
You don’t want to build something that becomes another legacy headache in five years. To avoid that, you have to bake modern architectural principles into the very foundation of your strategy.
- Go Modular: Instead of a single, massive system, think in terms of smaller, independent services that talk to each other. This makes it infinitely easier to update, replace, or scale one piece without taking the whole system down.
- Embrace an API-First Design: This just means you design your systems with the primary goal of making them easy to connect to. It’s absolutely essential for interoperability, allowing you to plug in new tools, share data securely with partners, and build new apps on top of what you already have. It’s also the secret to effective internal tooling.
- Build on Cloud-Native Infrastructure: The cloud gives you the power to handle huge datasets and unpredictable workloads without buying and managing racks of servers. This frees up your IT team from maintenance duty so they can focus on work that actually drives the business forward.
A well-designed, API-first architecture turns your health system from a closed-off fortress into an open platform for innovation. It's how you future-proof your technology investments, period.
For some, this means building from the ground up with custom healthcare software development. For others who need to move faster, an AI Automation as a Service partner can bring the right infrastructure and expertise to the table quickly.
Deciding on Your Data Architecture
A key decision is how you'll structure your data platform. The two main schools of thought are centralized (like a data warehouse) and decentralized (like a data mesh). Each has its trade-offs, and the right choice depends entirely on your organization's scale, culture, and long-term goals.
Here’s a quick rundown to help you weigh the options:
Comparing Data Architecture Models
| Architecture Model | Pros | Cons | Best For |
|---|---|---|---|
| Centralized (e.g., Data Warehouse) | High data consistency; Simplified governance; Stronger security controls | Can create bottlenecks; Slower to adapt to new data sources; Can be complex to scale | Organizations with standardized data needs and a strong central IT team that can manage a single source of truth. |
| Decentralized (e.g., Data Mesh) | Highly scalable; Greater team autonomy and speed; Fosters domain-specific expertise | More complex governance; Potential for data duplication; Requires a significant cultural shift | Large, complex organizations with diverse data domains where agility and team ownership are critical for innovation. |
Ultimately, there's no single "right" answer. A centralized model offers control, which can be ideal for smaller systems or those just starting to unify their data. A decentralized mesh, on the other hand, provides the agility large, innovative systems need to move fast.
Data Governance and Security Are Non-Negotiable
In healthcare, we’re not just dealing with data; we’re stewards of highly sensitive, personal, and regulated information. Robust governance and security can't be an afterthought—they have to be designed in from day one. It’s foundational to earning patient trust and staying compliant.
Your governance framework needs to have ironclad policies for:
- Data Access: Who gets to see what, and when? Implement role-based access controls so clinicians and staff only see the specific information required for their jobs.
- Data Quality: You need processes to ensure the data feeding your system is accurate, complete, and consistent. Remember: garbage in, garbage out. Bad data leads to bad analytics and AI models you can't trust.
- Data Privacy and HIPAA Compliance: Every single component of your architecture must be built to protect patient privacy and meet HIPAA rules. This means encryption (both at rest and in transit), secure storage, and regular security audits.
A strong governance policy is the rulebook that keeps everyone safe and ensures your data is a reliable asset. We bake this thinking directly into our AI Product Development Workflow so that compliance is a given, not a scramble at the end.
The Human Side of Change: Getting Your Team on Board
Let's be honest: the most brilliant technology in the world is useless if your people don't use it. You can have a state-of-the-art AI platform and a perfectly designed data architecture, but if your clinicians and staff see it as just another hurdle, it will fail. This is the part of the journey where change management becomes your most important tool—it’s all about the people.
Real transformation doesn't happen when technology is forced upon a team. It happens when they feel it's a tool that works for them, not something being done to them. To get to that point, you have to earn genuine buy-in. That starts with a vision that answers the one question everyone is thinking: "What's in this for me?"
Crafting a Vision That Actually Connects
A vision statement filled with buzzwords about ROI and operational efficiency isn't going to inspire the nurse on the night shift. Your messaging has to connect directly to the realities of their work and their core mission of caring for patients. The entire goal is to show them, in no uncertain terms, how these new tools will make their lives better.
Frame the changes around benefits they'll feel personally:
- Less Time on Paperwork: "This AI scribe will take care of clinical notes, giving you back an hour every day to actually be with your patients."
- A Real Impact on Patient Health: "This new analytics tool will flag high-risk patients sooner, so we can step in and prevent a crisis before it happens."
- More Meaningful Work: "By automating inventory, you can stop chasing down supplies and focus on the complex clinical work you were trained for."
When the "why" is crystal clear, you'll find that resistance starts to fade. People are far more willing to climb a learning curve when they believe it leads to a less frustrating, more fulfilling workday. This is something we focus on heavily in our AI strategy consulting—making sure the technology serves the human from day one.
Building Trust with Honesty and Real Training
Once you've shared the vision, you can't just go silent. You need a rock-solid, transparent communication plan to keep everyone in the loop. Nobody likes surprises, especially when their job is on the line. Consistent updates, town halls, and open Q&A sessions build trust and stop the rumor mill from churning.
Training is just as crucial, and I don't mean a one-off webinar. Effective training builds confidence, not just competence. A program that actually works needs to be:
- Tailored to the Role: A radiologist and a scheduler need completely different training.
- Hands-On: Let people play with the new tools in a sandbox environment where they can't break anything.
- Continuous: Offer support long after the system goes live.
My Two Cents: Don't confuse "implementation" with "adoption." Implementation is just flipping the switch. Adoption is when the new technology becomes so ingrained in the daily workflow that your team can't imagine going back. You only get there by putting people first.
Finding and Empowering Your Champions
One of the most effective things you can do is find your internal "digital champions." These are the people on the front lines who are naturally curious about technology and respected by their peers. They aren't just power users; they're the informal leaders everyone turns to for advice.
Give these champions a seat at the table. Involve them in the AI requirements analysis and beta testing. Equip them with the knowledge to answer questions, calm fears, and share early wins. A simple "Hey, this new tool just saved me 20 minutes" from a trusted colleague is worth more than a dozen emails from management.
This approach turns pockets of resistance into a groundswell of support. It ensures your new tools aren't just installed, but woven into the very fabric of how your organization operates. Navigating this human element is what our expert team does best, because we know that true success is always a partnership between great people and great technology.
Showing the Payoff: Measuring Success and Proving the ROI of Your Digital Strategy
To keep the C-suite bought in and the funding flowing for your healthcare digital transformation strategy, you have to prove it’s working. And I don’t mean with vanity metrics. We're talking about showing clear, undeniable value through key performance indicators (KPIs) that map directly to better clinical, operational, and financial results. This isn't just a box you check at the end of a project; it's how you continuously validate the investment and make smarter decisions down the road.
The entire goal is to draw a straight line from every digital initiative to a tangible outcome. Don't just report on system uptime. Instead, show how your new tools are cutting patient readmission rates, boosting diagnostic accuracy with better AI tools for business, or shaving minutes off the average patient wait time. These are the numbers that make executives sit up and listen because they represent real-world impact.
Defining KPIs That Actually Mean Something
You need a balanced view. If you only focus on financial returns, you'll miss the bigger picture of clinical quality and patient satisfaction. A balanced scorecard approach is perfect for this, giving you a holistic look at how your strategy is performing across the board.
Your scorecard should be a mix of metrics like these:
- Clinical Outcomes: Are hospital-acquired infections down? Are medication adherence rates up? Are we getting diagnostic results back to physicians faster?
- Operational Efficiency: We need to see a drop in administrative busywork, better utilization of our operating rooms, and fewer staff overtime hours. For instance, are new internal tooling systems actually reducing manual data entry?
- Financial Impact: This is the classic ROI. Show me the direct cost savings from automation, the reduction in denied claims, and a healthier revenue cycle.
- Patient & Staff Experience: We can't forget the human element. Use surveys and feedback channels to track patient satisfaction scores and, just as importantly, keep a pulse on clinician burnout rates.
This comprehensive view is what tells the full, compelling story of your transformation.
Proving Your Value with Real-World Wins
The best healthcare organizations don't just use data to track what happened—they use it to constantly refine what they do next. Look at a leader like Novant Health. They achieved a Level 9 out of 10 in the 2025 Digital Health Most Wired Survey, putting them in the top 1% of 50,000 healthcare organizations globally. That's not just a fancy award; it's a reflection of their proven excellence in clinical quality, analytics, patient engagement, and innovation. You can read more about their healthcare technology leadership on NovantHealth.org.
This kind of achievement isn't an accident. It’s proof that a well-designed and flawlessly executed strategy delivers validated, impressive outcomes that benefit both patients and the clinicians who care for them.
Getting this right requires a clear plan and the right expertise. By defining the right KPIs from the get-go and consistently measuring your progress against them, you can build an airtight case for the ROI of your digital initiatives. This data-driven approach doesn't just justify past investments; it builds the confidence you need to secure resources for the next wave of innovation. Let our expert team help you build a strategy that delivers results you can measure.
Frequently Asked Questions
Where’s the Best Place to Start with Digital Transformation in a Healthcare Setting?
It’s tempting to try and fix everything at once, but that's a recipe for disaster. The smartest move is to find the most acute pain point in your organization and start there. Look at your existing clinical or administrative workflows—where are the biggest bottlenecks?
Maybe it's the patient intake process, which is notoriously manual, or perhaps it's the revenue cycle management, where delays directly hit your bottom line. Pick one high-impact area where technology can deliver a clear, measurable win. This gives you a quick victory that builds momentum and gets people on board for bigger changes down the road. A thorough AI requirements analysis can really help you zero in on that perfect first project.
How Do We Actually Get Clinicians to Use New Digital Tools?
This is the million-dollar question, isn't it? The key is to stop pushing technology on them and start pulling them into the process. Adoption lives and dies by clinician involvement.
Bring them into the conversation from day one. Let them help choose and design the tools. If a new system doesn't solve a real problem they face every day—like cutting down on charting time or giving them faster access to patient histories—they simply won't use it. You have to frame the benefits in their language: less admin work, better information, and ultimately, better outcomes for their patients. When you co-create the solution with them, as we explored in our AI adoption guide, you turn your biggest skeptics into your most powerful advocates.
What's the Single Biggest Mistake to Avoid in This Process?
Thinking of it as just an IT project. That’s the classic pitfall.
A successful digital transformation is a fundamental business strategy, not a tech upgrade. It requires rock-solid leadership, a compelling vision that everyone understands, and a relentless focus on managing the human side of change. If you don't address the ingrained habits, fears, and daily workflows of your staff, you can have the best technology in the world, and it will still fall flat. It’s this kind of strategic blind spot that our AI strategy consulting is specifically designed to help organizations avoid.
Can AI help with both administrative and clinical tasks?
Absolutely, and that’s one of its biggest advantages. AI is incredibly versatile. It can streamline back-office headaches like billing and coding just as effectively as it can provide clinical decision support at the bedside. A truly effective strategy tackles both sides of the house to maximize efficiency and elevate care quality across the entire organization.
How do you calculate the ROI for a digital health initiative?
It's about more than just cost savings. A true ROI calculation quantifies the "soft" benefits, too. Think about the long-term cost reduction from improved patient outcomes, the value of increased staff productivity, and the financial impact of higher patient retention. A solid analysis puts a dollar value on all of it, showcasing the comprehensive value of real-world use cases.
Ready to build a future-proof healthcare strategy? Ekipa AI delivers a Custom AI Strategy report in 24 hours, turning your transformation goals into a clear, actionable roadmap. Our approach is backed by our expert team dedicated to navigating the complexities of healthcare innovation.