A C-Suite Guide to Care Pathway Optimization with AI
Discover how care pathway optimization drives real results. Learn to map workflows, leverage AI, and scale solutions for better patient outcomes and efficiency.

Optimizing a care pathway is all about strategically redesigning how you deliver care to get better patient outcomes, make your operations run smoother, and bring down costs. This isn't about small, isolated fixes. It's about creating a single, seamless, evidence-based journey for a patient, from the moment they're diagnosed all the way through recovery. For any health system trying to get a handle on rising costs and patient expectations, this has become a top priority.
Why We Have to Modernize Patient Journeys
In healthcare right now, standing still is one of the biggest risks an organization can take. The old ways of delivering care—often siloed and reactive—are simply breaking down under the pressure. We're facing a perfect storm of rising operational costs, a worldwide shortage of clinicians, and an aging population with more complex chronic diseases than ever before. The way we've always done things just isn't cutting it anymore.
This is exactly why care pathway optimization is no longer just a "nice-to-have" project. It's a core strategic move. It forces us to fundamentally rethink how we deliver care, not just inside the hospital but across the entire patient experience. The whole point is to build standardized, predictable, and high-quality journeys that produce better results for patients, clinicians, and the organization itself.
From Patchwork Processes to a Cohesive System
I see it all the time with healthcare leaders. Their current workflows have often grown organically over decades, leading to a patchwork of processes filled with variability and hidden waste. A patient's journey for something as common as a knee replacement can look completely different based on which doctor they see, which department they're in, or even what day of the week it is. This kind of inconsistency is what drives up costs and, frankly, can hurt patient outcomes.
A solid optimization plan replaces that guesswork with a structured, data-driven approach. When you get it right, it pays off for everyone involved:
- For Patients: They get the right care at the right time. This leads to better health outcomes and a far less confusing, more positive experience.
- For Clinicians: They get clear, evidence-based protocols. This cuts down on administrative headaches and lets them focus on the clinical work that truly matters.
- For the Organization: Operations become more efficient, waste is reduced, readmission rates drop, and the bottom line gets stronger. It builds a more resilient and competitive health system.
The Financial and Clinical Stakes
The need for this is written in the numbers. Look at Germany, where it was found that roughly 80% of health system costs were being spent on just 20% of citizens—a glaring sign of inefficiency. The industry is waking up to this. While only about 15% of healthcare organizations are actively implementing optimization strategies today, another 30% are planning to jump in within the next two years. That's a huge shift. You can explore more data on the growth of care pathway optimization to see just how fast this is moving.
By standardizing care, health systems can systematically cut out unnecessary steps, reduce expensive complications, and make sure their resources are actually being used where they can make the biggest difference. This isn't just about saving money; it's about saving lives.
Before diving into the tactical details, it's helpful to frame the work around a few core pillars. These are the foundational elements that hold a successful optimization strategy together.
Table: Core Pillars of a Successful Optimization Strategy
| Pillar | Description | Key Objective |
|---|---|---|
| Data-Driven Analysis | Grounding all decisions in real-world performance data, not assumptions or anecdotal evidence. | To uncover hidden bottlenecks, variations in care, and opportunities for improvement. |
| Clinical Leadership | Ensuring that physicians, nurses, and other frontline staff are central to the redesign process. | To build evidence-based protocols that are practical, trusted, and widely adopted. |
| Patient-Centric Design | Mapping the journey from the patient's perspective to address their needs, fears, and pain points. | To create a seamless, supportive, and less stressful experience that improves outcomes. |
| Technology Enablement | Using tools like AI and automation to support clinicians, streamline workflows, and personalize care. | To enhance human capabilities, reduce administrative burden, and enable new care models. |
Ultimately, a strategy that balances these four pillars is one that is built to last, driving both immediate wins and long-term, sustainable transformation.
The Growing Role of AI and Data
True optimization requires more than a new flowchart on the wall. You have to get deep into the data, and that's where artificial intelligence is a game-changer. Modern AI solutions can tear through massive datasets from EHRs, patient monitors, and billing systems to find patterns and problems that are completely invisible to the human eye.
Of course, to do any of this, you have to nail the fundamentals of data security and patient privacy. That means using tools like secure HIPAA compliant online forms for any sensitive information. Building that trust is non-negotiable. With that foundation in place, a clear plan, like a Custom AI Strategy report, can show you exactly how to apply these powerful tools to get real, measurable results—turning your biggest system-wide challenges into a major competitive advantage.
Mapping Your Workflows to Uncover Hidden Inefficiencies
You can't fix a process you don't truly understand. Before you can optimize anything, you need to get an honest, granular look at your current care pathways. This isn't about drawing a few boxes on a whiteboard; it’s about creating a detailed, evidence-based picture of how care actually happens on the ground, day in and day out.
The only way to get this picture is to talk to the people on the front lines. I’m talking about in-depth interviews with your physicians, nurses, discharge planners, and even the administrative staff who manage the paperwork. Their firsthand accounts will expose the informal workarounds, communication gaps, and persistent bottlenecks that formal protocols always miss. This is where you find the real story.
Of course, you need the hard data to back it up. Digging into your EHR and billing systems will give you the quantitative proof you need to pinpoint systemic problems. You’ll be able to see exactly where costly variations in care are happening, where treatment is being delayed, and what’s driving up your operational costs. This foundational discovery work is also the first critical step in a comprehensive AI requirements analysis, ensuring you apply technology with surgical precision instead of as a blunt instrument.
This whole process is about turning external pressures into a clear, measurable strategy for improvement.
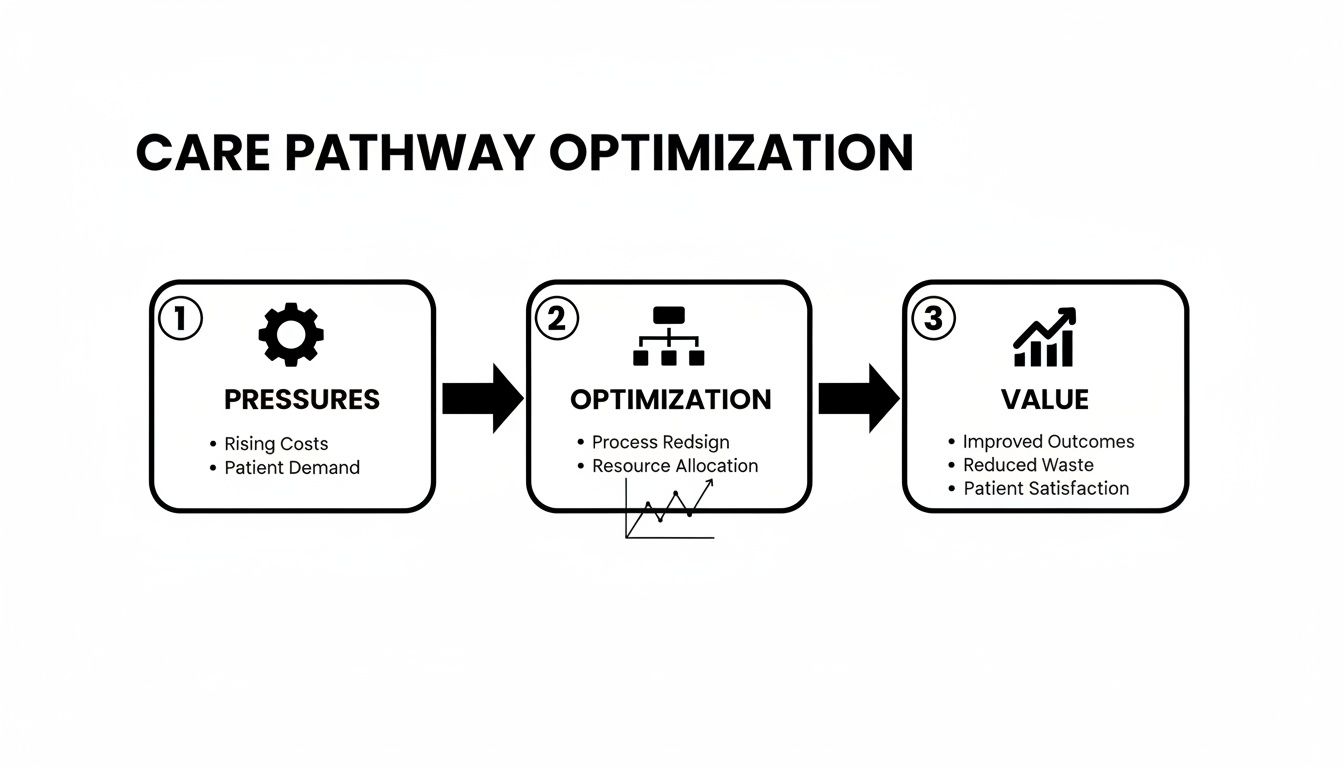
As the chart shows, mapping and improving your workflows is a direct response to the challenges you're facing, leading to concrete organizational value.
From Vague Goals to Meaningful KPIs
Once you have that clear map of your current state, you have to define what "better" actually looks like. Setting meaningful Key Performance Indicators (KPIs) is non-negotiable. These aren't just metrics for a dashboard; they are the yardsticks you’ll use to measure the real-world impact of your changes.
Forget generic goals like "improve efficiency." Get specific. Your KPIs should be a direct reflection of the problems you just uncovered.
- Are total knee replacement patients staying too long? Your KPI is reducing average length of stay (LOS) for that specific cohort.
- Are certain patient groups coming back too soon? Your goal is to minimize 30-day readmission rates for them.
- Is the ED backed up? Focus on decreasing patient wait times from door to disposition.
- Are HCAHPS scores for discharge flagging? Aim to boost scores related to communication and discharge planning.
- Seeing too much variation between clinicians? The target is improving adherence to evidence-based protocols.
These sharp, focused KPIs give you a clear baseline. They turn a well-intentioned initiative into a measurable, results-driven strategy.
Identifying the True Sources of Inefficiency
With your map and your metrics, you can finally start pinpointing the real problems. More often than not, the issues aren't isolated incidents but systemic flaws baked into the workflow. For example, a high readmission rate for heart failure patients probably isn't a clinical failing—it’s more likely a breakdown in the discharge process.
A deep dive might show that patients aren't getting clear medication instructions or, more commonly, that follow-up appointments simply aren't being scheduled before they walk out the door. These are the high-impact intervention points where a small, targeted change can deliver dramatic results.
This is also where you'll start to see clear opportunities for smart technology. Maybe manual appointment scheduling is creating endless delays—a perfect use case for AI Automation as a Service. Or perhaps your clinicians don't have a reliable way to predict which patients are at the highest risk of decline, a problem easily solved with the right AI tools for business.
Ultimately, this mapping phase isn't just about documenting what's broken. It's about building a rock-solid business case for change. It gives you the data-backed evidence needed to get buy-in from leadership and clinicians, setting the stage for everything that comes next. By understanding precisely where the friction is, you can be sure you're solving the right problems.
Pinpointing High-Impact AI Intervention Opportunities
Once you have a clear, data-backed map of your current care pathways, the real work begins. You shift from diagnosis to action, and this is where the potential of care pathway optimization truly comes alive. It's time to pinpoint the specific moments in the patient journey where intelligent automation and predictive analytics can deliver the biggest wins.
This isn't about chasing the shiniest new toy. It’s about a deliberate, strategic application of AI solutions to solve the exact problems you’ve already uncovered. The goal is to find those high-leverage points—the spots where a single, targeted intervention can create a positive ripple effect across the entire pathway, improving both clinical outcomes and your bottom line.
From Bottlenecks to Breakthroughs
Your workflow map is now a treasure map. It’s pointing directly to the friction points, delays, and frustrating variations in care. These are your prime candidates for an AI-driven solution.
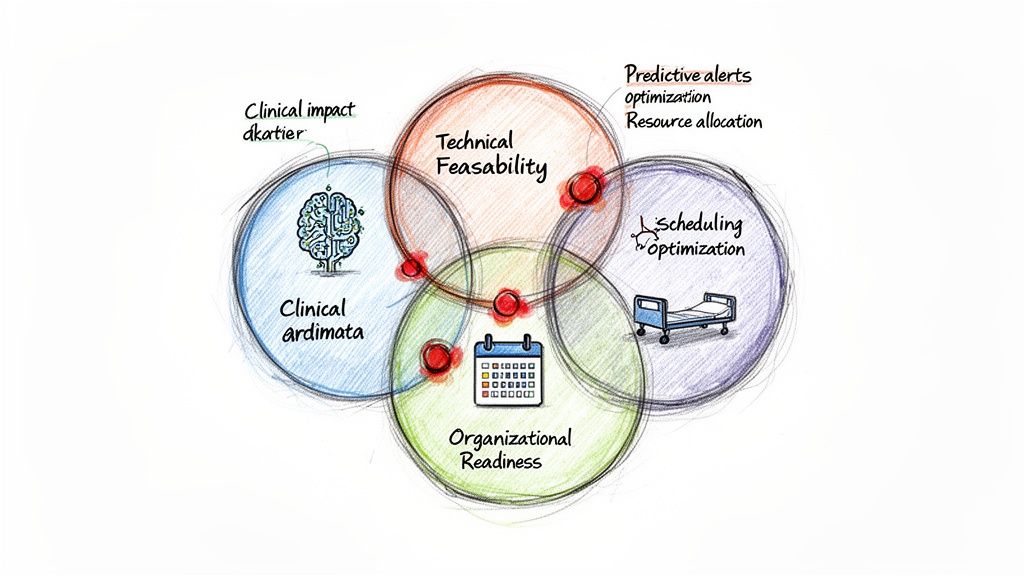
Let’s get practical. Think about a surgical pathway for knee replacements. Your analysis might show that last-minute cancellations and scheduling snafus are a massive headache, driving up costs and frustrating everyone involved. This is a perfect place for a machine learning model to step in and optimize surgical scheduling, predicting conflicts before they happen and allocating OR time with far greater precision.
Or what about managing patients with chronic heart failure? A huge challenge is preventing those costly, and often avoidable, hospital readmissions. Here, predictive analytics can be a game-changer. By analyzing real-time data from wearables and EHRs, an AI model can flag at-risk patients before their condition spirals, allowing your care teams to intervene proactively with a simple telehealth check-in or a quick medication adjustment. This often involves custom healthcare software development to integrate these new data sources securely.
A Triple-Threat Framework for Evaluating Opportunities
Not all opportunities are created equal. To build a solid business case and secure some early wins, you need a structured way to evaluate and prioritize potential AI projects. From my experience, a robust evaluation has to balance three critical factors:
- Clinical Impact: Does this actually move the needle on patient outcomes or safety? Will it help clinicians stick to evidence-based protocols and deliver better care?
- Technical Feasibility: Do we have the data we need? Is the technology mature enough to solve this specific problem reliably? A clear AI Product Development Workflow is essential for assessing this without guesswork.
- Organizational Readiness: Do we have clinical champions and operational leaders who will back this? Does it align with our bigger strategic goals and, frankly, our budget?
The sweet spot for any new initiative is right at the intersection of high clinical impact, strong technical feasibility, and solid organizational readiness. You can have the most brilliant tech in the world, but if your frontline staff won't use it, it's dead on arrival.
Learning from Real-World Use Cases
Seeing these ideas in action is what makes it all click. We’ve seen countless real-world use cases where targeted AI delivers tangible results.
For instance, AI-powered diagnostic tools are helping radiologists spot subtle signs of disease earlier and more accurately, directly improving a patient’s prognosis.
Similarly, natural language processing (NLP) models are taking on the soul-crushing work of clinical documentation. This frees up physicians from administrative overload and helps chip away at burnout. These aren't futuristic concepts; they are practical solutions delivering real value in hospitals today. For a deeper look, our guide on how Pathwise AI helps optimize care pathways has more specific examples.
By systematically identifying and evaluating these high-impact opportunities, you move from a theoretical understanding of care pathways to a concrete, actionable roadmap. This ensures that when you invest in technology, it isn’t just innovative—it’s truly impactful.
Designing and Running a Pilot That Actually Works
It's tempting to take a great plan and immediately push it across the entire organization. That’s a mistake. Jumping from the drawing board to a full-scale rollout is a high-risk gamble that rarely pays off.
A much savvier move is to run a controlled pilot program first. This is your chance to test your proposed changes in a real-world setting, learn from what happens on the ground, and build the evidence and momentum you need for a broader launch. A well-run pilot is the single best way to de-risk your entire care pathway optimization strategy.
This isn’t just a small, informal experiment. Think of it as a disciplined, structured process designed to prove your intervention works and gather the hard data needed to justify a larger investment. The first step? Be incredibly selective about where and how you run it. You need a tightly defined scope to get clean, actionable results.
Start by choosing the right patient group. Don't try to boil the ocean. Pick a specific, well-defined cohort—say, uncomplicated primary knee replacement patients—where you have a clear theory about how your changes will move the needle. Just as important is finding an engaged clinical team. You need champions who are open to new ideas and willing to help drive the process.
What Does a "Win" Look Like?
With your scope locked in, you have to define success with razor-sharp clarity. Your KPIs from the mapping phase are the foundation, but now you need to attach specific, measurable targets to them for the pilot.
- Goal: Cut the average length of stay for the pilot cohort by 15%.
- Goal: Boost adherence to the new discharge protocol to over 90%.
- Goal: See a 10-point jump in patient satisfaction scores tied to care coordination.
These numbers tell you what happened. But to understand why it happened, you need to talk to your frontline staff. Their qualitative feedback is gold. It reveals the practical friction points and gives you the insights needed to refine the workflow before you even think about scaling up.
We’ve found that a structured methodology, like our own AI Product Development Workflow, is crucial here. It brings the same project management discipline to the pilot that you’d apply to any other mission-critical initiative, ensuring it stays on track and delivers meaningful data.
Don't Forget the People
Even the most brilliant pilot will fall flat if you ignore the human element. Your frontline staff are juggling a dozen things at once, and any change—even a good one—can feel like just another burden. Getting their buy-in isn't a "nice-to-have"; it's a prerequisite for success.
Start by explaining the "why." Connect the pilot directly to the problems they face every single day. Frame this not as a top-down mandate, but as a collaborative effort to make their jobs easier and, most importantly, improve patient outcomes.
The impact of getting this right is huge. One comparative analysis of coronary heart disease pathways found a shocking disparity: one region had a 3.7% in-hospital mortality rate, while another, despite spending more, had an 11.4% mortality rate. This isn't just a statistic; it's a powerful reminder that a well-designed, well-implemented pathway saves lives and resources. You can dive into the full analysis on care pathway disparities to see the data for yourself.
Your pilot is where you build your own success story. By starting small, proving the value, and gathering a coalition of supporters, you create an undeniable case for change. This is how a promising idea becomes a validated, scalable solution that's ready for the rest of the organization.
Scaling Success Across Your Organization
A successful pilot is a launchpad, not the finish line. It gives you the proof you need and the momentum to tackle the next, much harder challenge: scaling your optimized pathway across the entire health system.
This phase is less about the tech and more about people, process, and culture. I’ve seen countless promising transformation projects die on the vine right here—not because the solution was wrong, but because the rollout lacked discipline.
The real goal is to bake the new workflow so deeply into your organization’s DNA that it becomes the new standard of care. That means shifting from a small, dedicated pilot team to an enterprise-wide operational model. To pull that off, you need a strong governance structure to steer the ship, manage resources, and keep everything tied to your bigger strategic goals. This is also where services like our implementation support can transition from a pilot tool to a core part of your operational infrastructure.
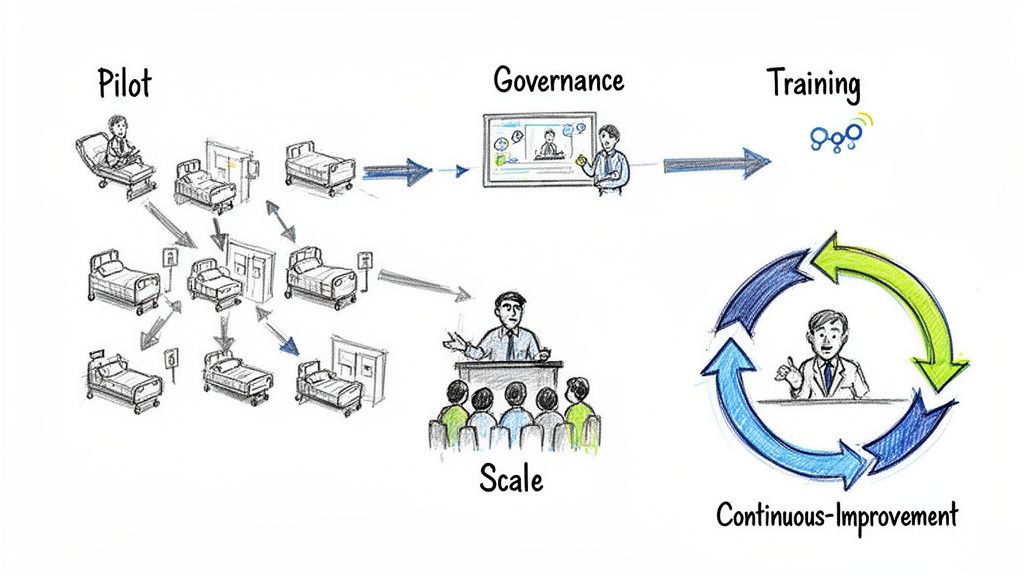
Establishing a Robust Governance Framework
To scale without chaos, you need a central team calling the shots. This governance body, often a cross-functional steering committee, is responsible for prioritizing rollouts, allocating budget, and knocking down organizational roadblocks. Their main job is to ensure the scaled-up version stays true to the principles you proved in the pilot, while still being flexible enough for different departments or facilities.
Who should be on this committee? Make sure you have the right people in the room:
- Clinical Leadership: They'll champion the changes and protect clinical integrity.
- Operational Managers: These are the folks who will handle the real-world logistics of implementation.
- IT and Data Specialists: They manage the technical backbone and keep the data flowing.
- Finance Representatives: They need to be there to track performance against your financial targets.
Think of this group as the central nervous system for the rollout. They’re there to make data-driven decisions and keep everyone on the same page.
Mastering the Art of Change Management
Honestly, the technology is the easy part. Changing human behavior? That’s the real mountain to climb.
Effective change management is the single most critical factor in a successful scaling effort. You can't just send out a memo with a new protocol and expect everyone to fall in line. It never works.
The heart of change management is communication. You have to constantly explain the "why" behind the new pathway, connecting it directly to better patient outcomes and a less frustrating work environment for your staff. Use the data from your successful pilot—it's your most powerful tool for building credibility and getting people excited.
A solid communication plan is proactive, not reactive. It anticipates the tough questions and addresses concerns before they fester. This means town halls, departmental huddles, and clear, consistent messaging from every leader. You’re trying to create a story of positive evolution, not one of disruptive chaos.
Training Your Teams for the New Reality
Training can't be a box-checking exercise tacked on at the end. It has to be practical, role-specific, and ongoing.
Your frontline staff—the nurses, therapists, and schedulers—need more than a 30-minute webinar. They need hands-on training that simulates the new workflow, letting them build muscle memory and confidence before the system goes live.
I’m a big fan of the "train-the-trainer" model. Empower the clinical champions from your pilot to become super-users and mentors for their peers. This approach doesn't just scale well; it uses the credibility of colleagues who have already seen the benefits firsthand. It’s how you turn skeptics into your biggest advocates.
What's Next? Building a Future-Ready Healthcare System
We’ve walked through a practical playbook for transforming patient care, and if there's one key takeaway, it's this: care pathway optimization isn't a one-and-done project. Think of it as a continuous journey toward building a healthcare system that's truly more efficient, effective, and centered on the patient.
The potential here is enormous, especially with AI, but it all comes down to having a clear vision and a solid plan to make it happen. You've seen the opportunities, from untangling complex workflows with AI Automation as a Service to simply improving how you connect with patients. For example, many forward-thinking organizations are seeing real success by implementing a chatbot for healthcare to give patients instant answers and better access to care.
It's time to shift from talking about change to actively building it. The gap between a good healthcare system and a great one is closed by a relentless commitment to data-driven improvement.
This kind of journey needs a map. To help you get started on the right foot, our team can put together a Custom AI Strategy report that digs into your specific challenges and goals. As we’ve seen time and again, and as we explored in our AI adoption guide, a well-defined plan is what separates successful initiatives from stalled ones.
A thorough AI requirements analysis is the first real step to lighting the path forward. It ensures that every investment you make and every change you implement delivers real, measurable value from day one.
When you're ready to start that conversation, I encourage you to connect with our expert team. Let's talk about what it will take to build your future-ready organization, together.
Common Questions Answered
We get a lot of questions about optimizing care pathways and bringing AI into the clinical mix. Here are a few of the most common ones we hear from leaders like you.
What’s the Most Important First Step?
Before you do anything else, you have to get a crystal-clear, honest picture of where you are right now. This means mapping your current care pathways in minute detail.
I'm not talking about a simple flowchart. You need to dig in and gather real numbers on performance and, just as importantly, talk to your frontline staff and patients. Their firsthand experience is gold.
Without this baseline—a map that shows you exactly where the bottlenecks are and why care varies from one physician to another—you’re just guessing. This deep-dive discovery phase, which includes a thorough AI requirements analysis, is the only way to find the opportunities that will actually make a difference.
How Do We Measure the ROI of Investing in AI?
Measuring the return on an AI investment isn't a single number; it's a blend of financial, operational, and clinical wins.
On the financial side, you can directly track cost savings from things like shorter lengths of stay, lower readmission rates, and smarter use of resources.
Operationally, look at metrics like patient throughput, how much time your staff gets back from tedious admin work, and shorter wait times. And clinically, it’s all about better patient outcomes, improved adherence to best practices, and higher patient satisfaction scores.
The trick is to define these metrics before you even start a pilot. That’s how you build a rock-solid business case for expanding your investment in Healthcare AI Services.
How Can We Get Clinical Staff to Actually Adopt New Pathways?
Getting your clinical teams on board is everything, and it has to start on day one. You absolutely must involve your doctors, nurses, and other providers in the mapping and redesign process from the very beginning. They’re the ones on the ground, and their insights are what will make any new pathway practical instead of purely theoretical.
Don’t position this as another mandate from the top. Frame it as a team effort to make their jobs easier and, most importantly, improve patient care.
Use the data from your pilots to show them the proof. Demonstrate real benefits, like less time spent on paperwork or tangible improvements in patient health. Great communication, solid training, and celebrating those early victories are all key to managing the change.
When they have a hand in building it, it becomes their process. That buy-in is what makes the new pathway stick. This kind of collaborative approach is at the heart of effective AI strategy consulting.
Ready to put these ideas to work? The Ekipa AI platform is designed to help you quickly pinpoint and act on the AI opportunities that will drive real results, turning your biggest challenges into measurable wins. Start building your AI roadmap today.