A Strategic Guide to Enterprise Healthcare Modernization
Discover a strategic roadmap for enterprise healthcare modernization. Learn how to leverage AI, cloud, and data to drive better outcomes and efficiency.

When we talk about enterprise healthcare modernization, we're not just talking about a simple tech refresh. It's a fundamental reinvention of a health system's technology, daily processes, and core infrastructure to meet the demands of today's world. This means moving away from clunky, isolated systems and building a connected, data-smart ecosystem that genuinely improves patient outcomes, boosts efficiency, and strengthens the bottom line.
This isn't just about upgrading software; it's about survival and relevance.
Why Modernization Is No Longer Optional for Healthcare
For years, the healthcare industry has lagged behind other sectors in embracing digital tools. While banking and retail were busy transforming, many health systems were stuck with fragmented data, frustrating manual workflows, and ancient software. That's simply not sustainable anymore. Enterprise healthcare modernization has gone from a "nice-to-have" idea to a critical business imperative.
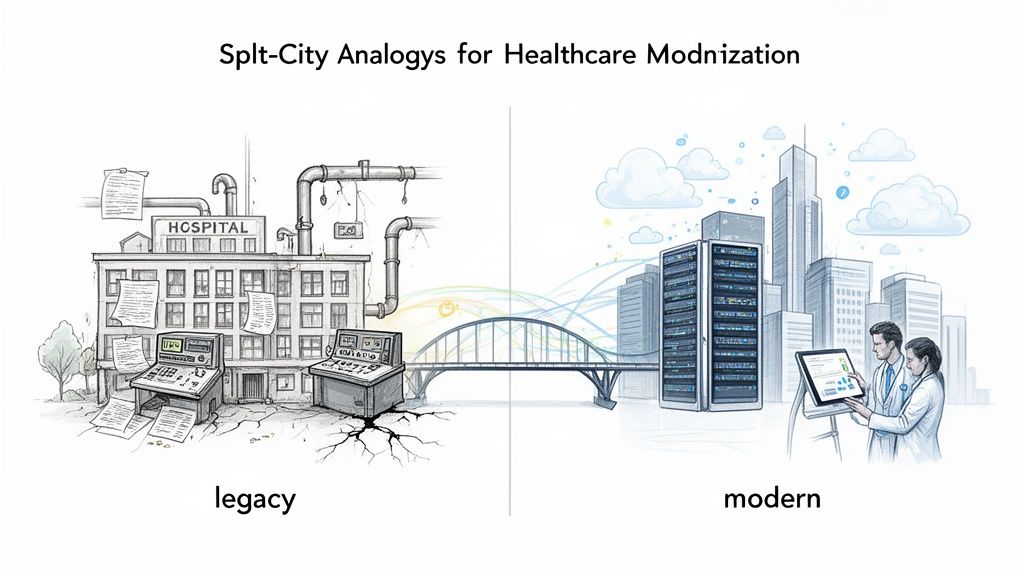
Think of it this way: you can't run a modern city on crumbling roads, an unreliable power grid, and a patchwork of disconnected communication lines. It just won't support growth. In the same vein, a healthcare organization propped up by disconnected systems and manual processes can't possibly deliver the high-quality, efficient care that patients now expect and absolutely deserve.
The Driving Forces Behind the Shift
This urgency is being driven by a perfect storm of pressures. Patients have completely different expectations now—they want seamless digital experiences and direct access to their own health information. At the same time, operational costs are skyrocketing, and clinician burnout is at an all-time high, often made worse by clunky, inefficient technology that gets in the way of patient care.
The market statistics tell the same story. The global healthcare information systems market is projected to explode from $519.23 billion in 2024 to over $1.77 trillion by 2034. That’s nearly a threefold increase in just a decade. This massive growth is a direct signal that the industry is scrambling to catch up, with many organizations still inexplicably relying on fax machines and paper charts.
Modernization isn't about chasing the latest shiny tech. It's about building a strong, flexible foundation that can support the future of medicine—from highly personalized patient care to AI-powered diagnostics.
To better understand the "why," let's look at the specific problems that modernization solves.
Core Healthcare Challenges Addressed by Modernization
The table below breaks down the common pain points in legacy healthcare systems and shows exactly how a modernized approach provides a direct solution.
| Challenge | Impact of Outdated Systems | Modernization Solution |
|---|---|---|
| Data Silos | Clinicians lack a complete patient view, leading to duplicate tests, medical errors, and care gaps. | Interoperability creates a unified patient record by connecting disparate systems like EMRs, labs, and pharmacies. |
| Operational Inefficiency | Manual processes for scheduling, billing, and records management cause delays, high administrative costs, and staff burnout. | Automation and AI handle repetitive tasks, optimize workflows, and reduce administrative overhead. |
| Poor Patient Experience | Patients struggle with disconnected portals, lack of communication, and inconvenient access to care. | Digital front-door technologies (e.g., patient portals, telehealth) provide a seamless, consumer-grade experience. |
| Reactive Care Models | Healthcare is delivered only after a patient is sick, leading to higher costs and poorer long-term outcomes. | Predictive analytics and remote monitoring enable proactive interventions and preventive care strategies. |
| Security Vulnerabilities | Legacy systems are often difficult to secure, leaving sensitive patient data exposed to cyber threats. | Cloud-native security and compliance frameworks provide robust, multi-layered protection against modern threats. |
By tackling these core issues head-on, modernization directly improves both the quality of care and the financial health of the organization.
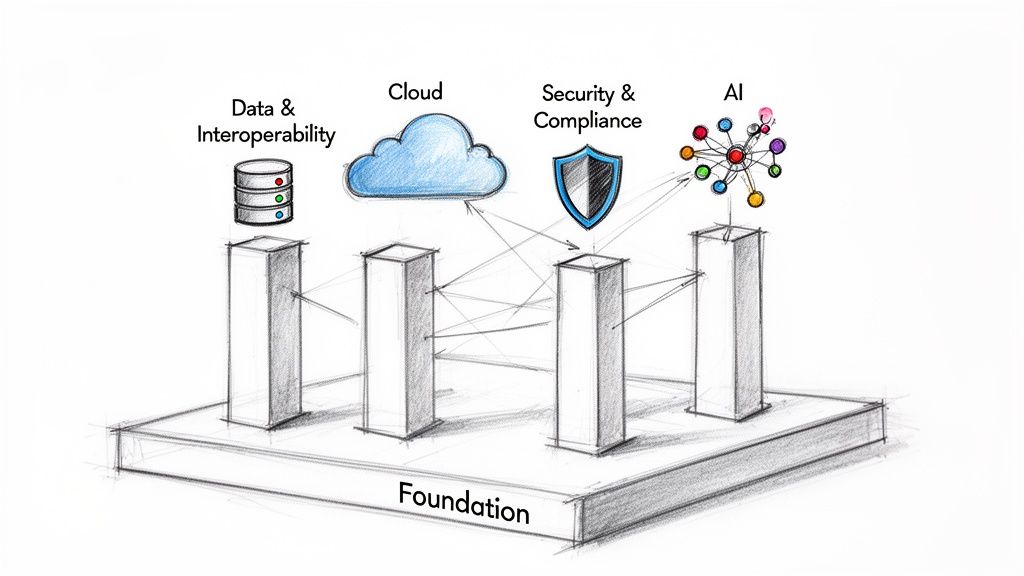
The Foundational Pillars of Transformation
A successful modernization strategy is built on four interconnected pillars. These aren't separate projects but a unified framework for creating a healthcare system that's ready for the future.
- Data and Interoperability: The goal here is to unlock and connect all that siloed patient data. This creates a single, comprehensive view that helps inform clinical decisions and make operations run smoother.
- Scalable Cloud Infrastructure: This involves moving away from rigid, on-premise servers to flexible cloud environments. The cloud can easily scale up or down as needed and provides the power for advanced analytics.
- Advanced Security and Compliance: Security can't be an afterthought. It has to be woven into the very fabric of the digital ecosystem to protect sensitive patient data and stay on the right side of regulations.
- Artificial Intelligence (AI): Think of AI as the intelligence layer. It can automate tedious tasks, help predict patient risks, and pull real, actionable insights from the mountains of data you already have.
These pillars provide the blueprint for truly reinventing how you deliver care and run your operations. Our specialized Healthcare AI Services are designed to help organizations build and integrate these powerful capabilities. Once you understand the 'why' behind this shift, the path forward becomes much clearer.
The Four Pillars of a Modern Healthcare Ecosystem
Rethinking enterprise healthcare isn't a single project; it's about building a completely new digital foundation. Think of it like constructing a building—you need strong pillars to support the entire structure. A modern healthcare system is no different, relying on four core components that must work in concert.
If you neglect one, the whole system becomes unstable. These pillars aren't just tech upgrades. They represent a fundamental change in how healthcare organizations handle information, protect data, scale their operations, and uncover critical insights. Let's dig into each one.
Pillar 1: Data and Interoperability
For years, patient data has been stuck in digital silos. It’s fragmented across countless separate systems—EHRs, lab software, billing platforms—that simply don't talk to each other. This is one of the biggest roadblocks to providing efficient, high-quality care.
The answer is interoperability. It's about getting these disconnected systems to speak a common language so they can share information fluidly and securely. When data flows without friction, doctors get a complete, real-time picture of a patient's health history, which means fewer redundant tests, a lower risk of medical errors, and better diagnoses. It's like finally replacing a chaotic pile of paper folders with a single, searchable digital record that's always up to date.
Pillar 2: Scalable Cloud Infrastructure
Relying on traditional on-premise servers is like being stuck with a physical file room—it's expensive, impossible to expand quickly, and incredibly rigid. A scalable cloud infrastructure throws that old model out the window, replacing it with a dynamic, secure, and resilient digital backbone.
Moving to the cloud isn't just about storage; it's about agility. The benefits are immediate:
- Elasticity: Hospitals can instantly scale their computing power up or down to handle fluctuating needs, like during a public health emergency, and only pay for what they actually use.
- Accessibility: Authorized staff can securely access patient information from anywhere, on any device. This is what makes effective telehealth and remote care possible.
- Innovation: The cloud delivers the massive processing power needed for advanced analytics and AI—something that’s just not practical with legacy on-site hardware.
Ultimately, this move creates an agile environment ready for future growth and new technologies, all without the massive upfront cost of buying more physical servers.
Pillar 3: Advanced Security and Compliance
In healthcare, data security isn't just a feature; it's an absolute necessity. With cyber threats becoming more sophisticated by the day, protecting sensitive patient health information (PHI) is a constant battle. A modern approach demands that security is built into the very fabric of the ecosystem from day one, not bolted on as an afterthought.
A modern security posture involves a multi-layered defense strategy. This includes end-to-end encryption for data both at rest and in transit, strict identity and access management protocols to ensure only authorized personnel can view sensitive information, and continuous threat monitoring to detect and neutralize potential breaches in real time.
This pillar also ensures you stay on the right side of regulations like HIPAA. By embedding compliance controls directly into the infrastructure, you can automate much of the reporting and auditing process, drastically reducing the risk of a costly violation. Building these secure, compliant systems often requires deep expertise in areas like custom healthcare software development.
Pillar 4: Artificial Intelligence
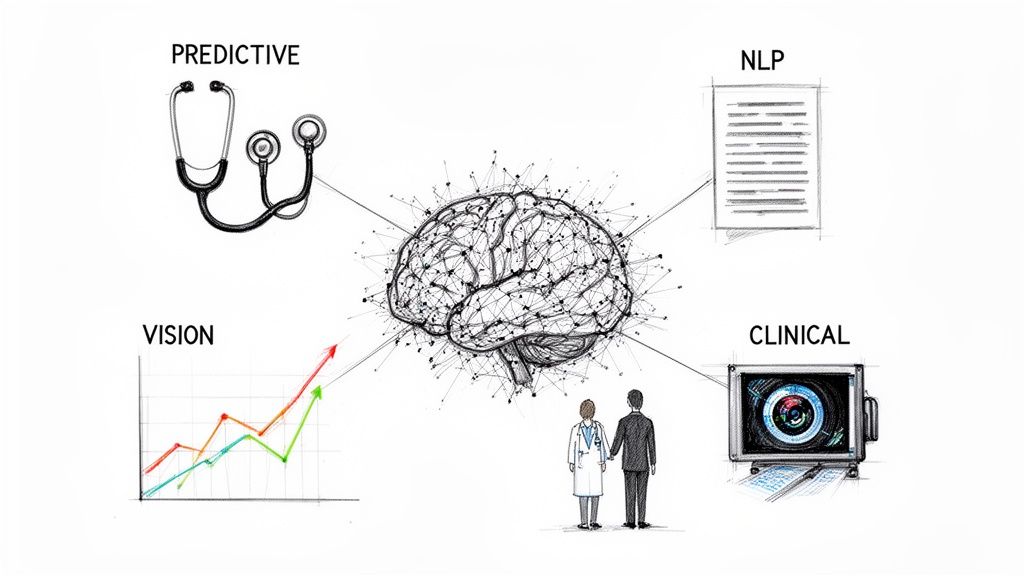
If data is the fuel and the cloud is the engine, then Artificial Intelligence (AI) is the smart navigation system telling you where to go. AI is what turns enormous volumes of raw data into genuinely useful insights that can improve both clinical outcomes and operational efficiency.
Powerful AI solutions can analyze complex datasets to spot patterns and predict outcomes in ways no human could. The applications are real and they make a difference right now. For instance, specialized Healthcare AI Services can power predictive models that flag patients at high risk for certain conditions, allowing for early intervention.
Similarly, AI Automation as a Service can take over repetitive administrative tasks, which helps reduce clinician burnout and gives them more time to focus on patients. To see how this works in practice, you can explore real-world use cases that show tangible results.
Putting Intelligence into Practice with AI
If clean data is the fuel and the cloud is the engine, then Artificial Intelligence (AI) is the intelligent navigation system guiding your modernized healthcare enterprise. AI isn't some far-off concept anymore. It's the critical layer that activates all that data you've organized, turning massive, complex streams of information into real-world insights that improve how you care for patients and run your operations.
The industry is voting with its dollars. Investment in healthcare AI is exploding, with AI-focused companies projected to grab 55% of all health tech funding by 2025. That’s a huge leap from just 29% in 2022. This isn't just hype; it’s a clear signal that enterprises see AI as the key to accelerating diagnoses, cutting down on errors, and automating cumbersome workflows.
Of course, just buying AI tools for business won't get you there. Real success hinges on a clear vision for what you want to achieve and a solid strategy to make it happen.
From Data Overload to Actionable Intelligence
Where AI truly shines is in its ability to spot patterns that are simply invisible to the human eye. This is where you start seeing the tangible rewards of modernization. With clean, interoperable data flowing smoothly through your cloud infrastructure, AI algorithms can finally get to work.
The applications aren't science fiction; they're practical and have an immediate impact:
- Predictive Analytics: Imagine AI models combing through EHR data to flag patients at high risk for sepsis or readmission before they crash. This allows clinical teams to step in early and change the outcome.
- Natural Language Processing (NLP): These tools can read through unstructured clinician notes and automatically pull out the important details. This slashes the administrative burden on doctors and nurses and helps minimize documentation mistakes.
- Computer Vision: In radiology, AI-powered image analysis can help spot subtle anomalies on X-rays or MRIs faster and more accurately, acting as an invaluable second set of eyes for the radiologist.
These aren't just efficiency gains. They directly tackle some of the biggest headaches in healthcare, like clinician burnout and preventable medical errors. By taking routine tasks off their plates and sharpening their decision-making, AI helps professionals focus on what truly matters: patient care.
Deploying AI with a Clear Purpose
Bringing AI into your organization is much more than a tech project—it's a fundamental business initiative that needs careful planning. A successful rollout starts by pinpointing the specific, real-world problems you need to solve. This crucial first step ensures your investment is directly tied to goals you can actually measure, as we explored in our AI adoption guide.
For instance, a hospital battling long ER wait times could deploy an AI-powered triage system to sort patients more effectively. An organization focused on better patient engagement might use an NLP-driven chatbot to handle post-discharge follow-ups. When looking at different solutions, it's vital to know how to compare AI models effectively based on their cost, speed, and accuracy for your specific use case.
The goal of AI in healthcare is not to replace clinicians. It’s to empower them. Think of it as a tireless, data-savvy assistant that surfaces insights and automates processes, allowing healthcare professionals to work at the absolute top of their game.
Effectively deploying these systems requires a methodical approach, from the initial concept all the way through to full-scale rollout and ongoing optimization. For more specific challenges, like improving interactions with providers, specialized tools like an HCP Engagement Co-pilot can deliver targeted, measurable improvements.
By turning raw data into predictive, actionable intelligence, AI becomes the force that truly drives a modern healthcare organization forward.
Your Phased Roadmap to Healthcare Modernization
Trying to figure out where to start with enterprise healthcare modernization can feel like boiling the ocean. It’s a massive undertaking. The key is to break it down into a structured, phased approach, turning one monumental task into a series of manageable, value-driven steps.
This roadmap isn't a rigid, one-size-fits-all prescription. Think of it more as a flexible guide. Its purpose is to de-risk the process, get all your key people on the same page, and ensure every investment logically builds on the last. Let's walk through the four phases that make this happen.
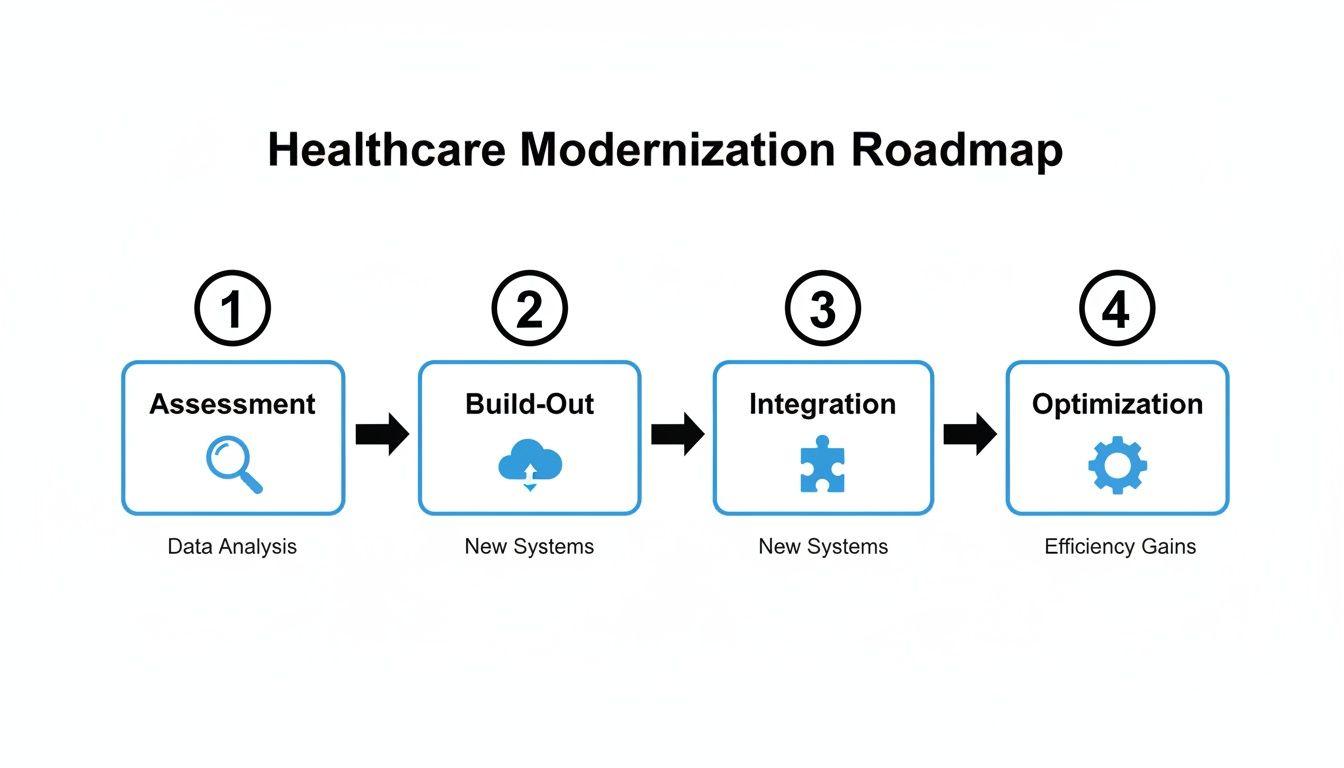
Phase 1: Assessment and Strategy Definition
Before you lay a single digital brick, you have to understand the ground you're building on. This first phase is all about a deep, honest look at your current systems, processes, and—most importantly—your pain points. It means mapping out your tech stack, finding where the data is trapped in silos, and pinpointing the biggest operational bottlenecks holding you back.
But a technical audit alone isn't enough. The real heart of this phase is defining what success actually looks like in plain business terms. What problems are you really trying to solve?
- Are you trying to slash patient wait times by 20%?
- Is the goal to cut administrative waste in the billing department?
- Do you need to improve clinician morale by giving them back time spent on documentation?
Answering these questions first ensures your modernization efforts are tied directly to tangible results. A comprehensive Custom AI Strategy report can give you a major head start here, providing a clear blueprint that connects your tech needs to your strategic goals right from day one. This process involves a detailed AI requirements analysis to ensure alignment.
Phase 2: Foundational Build-Out
With a clear strategy in hand, it’s time to start building the digital infrastructure that will support everything else you want to do. This is where you pour the concrete and put up the steel beams for your modern healthcare ecosystem. The focus is squarely on two areas: migrating to the cloud and achieving true data interoperability.
This phase is less about flashy new apps and more about getting the plumbing right. It involves moving key workloads to a secure, scalable cloud environment. That gives you the agility and raw computing power needed for advanced analytics. At the same time, you'll start the critical work of breaking down those data silos by implementing modern interoperability standards like FHIR (Fast Healthcare Interoperability Resources).
This stage is the digital equivalent of laying the foundation and framing for a new hospital. It’s not the most visible work, but without it, nothing else can be built securely or sustainably. Getting this right makes every subsequent phase smoother and more impactful.
Phase 3: AI and Advanced Capabilities Integration
Once your foundation is solid, it's time to bring your data to life with intelligent solutions. This is the phase where clinicians, administrators, and even patients start to see and feel the real power of modernization. Now you can begin layering advanced capabilities on top of your newly connected and scalable platform.
The focus here shifts to deploying targeted solutions that solve the specific problems you identified back in Phase 1. This could look like:
- Automating Workflows: Implementing internal tooling to handle the tedious, repetitive tasks that burn out staff, like patient scheduling or claims processing.
- Predictive Analytics: Using AI models that analyze EHR data to flag patients at high risk for readmission or spot the earliest signs of disease.
- Enhanced Diagnostics: Integrating computer vision tools that help radiologists interpret medical images with greater speed and accuracy.
Following a proven AI Product Development Workflow is critical here. It ensures these complex projects are managed effectively, moving from a small pilot to a full-scale deployment without blowing up your timeline or budget. As we’ve seen time and again, starting with well-defined, high-impact use cases is the key to building early momentum and showing a clear return on your investment.
Phase 4: Continuous Optimization and Scaling
Modernization isn’t a one-and-done project. It’s an ongoing cycle of improvement and adaptation. In this final, continuous phase, the goal is to monitor how your new systems are performing, measure their impact against the KPIs you set in Phase 1, and use those insights to refine and improve.
This is where you dig into what’s working, what isn't, and gather direct feedback from the people using the tools every day. Successes in one department can now be scaled across the entire enterprise, creating a flywheel effect where each improvement makes the next one easier. This constant optimization loop ensures your health system doesn't just catch up to the present—it stays resilient and ready for whatever comes next.
Navigating Common Modernization Hurdles
Embarking on a full-scale healthcare modernization effort is a serious commitment to change. And like any massive overhaul, it’s going to have its fair share of obstacles. Knowing what these challenges are ahead of time is the first step to actually overcoming them. We're not just talking about technical glitches; this is about untangling a complex web of regulations, stubborn legacy systems, data security risks, and good old human resistance.
Getting through this requires a proactive strategy, not a reactive one. A phased rollout can keep disruption to a minimum, and transparent communication is absolutely essential for getting your teams on board. This is where having real-world, battle-tested experience makes all the difference.
The Legacy System Tangle
One of the biggest headaches is trying to make shiny new technology play nicely with the old, reliable systems that have been running your operations for decades. These legacy platforms might be clunky, but they hold years of critical patient data and business logic. A "rip and replace" strategy is almost never practical or affordable.
The real solution is smart integration, not a wholesale replacement. This means using modern APIs to build bridges between your old and new systems, letting data flow where it needs to. It’s a delicate process, often demanding specialized skills in areas like custom healthcare software development to add new capabilities without torpedoing existing workflows.
Ensuring Ironclad Data Security and Compliance
In healthcare, data security isn't just a good idea; it's the law. Trying to meet the stringent demands of regulations like HIPAA while moving to new cloud and AI platforms is a high-stakes balancing act. One wrong move can lead to massive penalties and, even worse, a complete loss of patient trust.
Security can't be an afterthought bolted onto your new systems. It has to be woven into the fabric of your modernization strategy from day one. That means everything from data encryption and access controls to continuous threat monitoring.
This requires a deep understanding of both the technology and the intricate regulatory landscape. Partnering with a team that has a proven track record in building secure, compliant healthcare solutions isn't just a good idea—it's non-negotiable.
Managing Organizational Change
Maybe the most overlooked hurdle is the human one: resistance to change. Your clinicians and administrative staff are used to their workflows. Introducing new tools can feel disruptive, even threatening. If you don't get buy-in from the people who will actually use these systems every day, even the most brilliant technology will fall flat.
This is where effective change management comes in. It’s all about:
- Clear Communication: You have to explain the "why" behind the changes and show people how the new tools will make their jobs easier, not harder.
- Comprehensive Training: Provide hands-on training so everyone feels confident and competent with the new systems. Don't just throw them a manual.
- Involving End-Users: Bring clinicians and staff into the design and selection process. When they have a say, they develop a sense of ownership.
Getting past these obstacles demands a mix of technical skill, strategic planning, and a genuine understanding of the human element. By anticipating these roadblocks, you can build a far more resilient and successful modernization plan. If you need expert guidance on this complex journey, connect with our expert team to see how specialized AI solutions can help you tackle these challenges head-on.
Measuring What Actually Matters: The Real-World Impact of Modernization
So, how do you prove all this work is actually moving the needle? It’s a fair question, and one every executive will ask. The key is to stop talking about IT metrics and start talking about business results.
A successful modernization effort isn't just a line item on the IT budget; it's a strategic investment that pays dividends across the entire organization. We need to shift the conversation from server uptime and processing speeds to things like better patient outcomes and a more agile, responsive operation.
This is about building a rock-solid business case, and that starts with tracking the right Key Performance Indicators (KPIs) that connect your technology spend to tangible value.
Key Performance Indicators to Keep Your Eye On
To really show the ROI, you have to focus on metrics that tell a story about efficiency, cost, and the quality of care. These are the numbers that prove you’re making a real difference.
-
Operational Efficiency: Are patients spending less time in the waiting room? Are you processing claims faster? How much less time are clinicians spending on paperwork? These aren't just small wins; they show that automation and smarter workflows are making the entire system run smoother.
-
Cost Reduction: This is where the numbers get really compelling. Track the direct financial gains, like lower administrative overhead, slashed IT maintenance costs from moving to the cloud, and a measurable drop in expensive medical errors.
-
Clinical Outcomes: This is the ultimate goal, right? You can track this by looking at things like lower hospital readmission rates or better patient adherence to treatment plans. This is how you prove that better data is leading to better medicine.
-
Patient Satisfaction: Don't forget the human element. Patient surveys and engagement data can show you if the experience is improving. Are people finding it easier to book appointments? Do they feel more connected to their care teams?
The Business Case for a Modern Future
Across the globe, the people on the front lines of healthcare are already seeing the benefits. In fact, 80% of European healthcare professionals believe digital health technology has led to better care, and 76% are optimistic about what's next.
We’re seeing real-world examples of organizations crushing their administrative backlogs, delivering stroke treatments faster than national averages, and using virtual clinics to bring specialist care to underserved communities. You can read more about how trust is essential for healthcare's digital evolution.
When it comes down to it, modernizing your healthcare enterprise isn't just an IT project—it's a core business strategy. Having the right partner can make or break your success. At Ekipa, our tailored AI solutions and hands-on guidance give you the roadmap to build a truly resilient, future-proof healthcare organization.
Ready to start your journey and see measurable results? Let's connect with our expert team and talk about what's possible.
Frequently Asked Questions about Enterprise Healthcare Modernization
Thinking about a major modernization project brings up a lot of questions. It’s a big undertaking, after all. Here are some of the most common ones we hear from healthcare leaders, along with some straightforward answers to help you see the path forward.
What’s the very first step in a healthcare modernization project?
Before you even think about new technology, you have to start with a serious, honest look at where you are right now. The best first step is always a deep-dive assessment of your current systems, technology, and day-to-day workflows. You need to pinpoint exactly what's causing friction, figure out what your legacy systems can (and can't) do, and get crystal clear on what you want to achieve. A modernization project built on a solid strategy succeeds; one built on a shopping list of new tech usually doesn't. Getting help from a team that provides AI strategy consulting can be invaluable here to build a roadmap that ties every investment back to a real-world goal.
How do we modernize without putting patient data at risk?
Security can't be a box you check at the end of the project. It has to be baked in from the very beginning. This means building a security strategy with multiple layers: end-to-end encryption, strict access controls, constant threat monitoring, and unwavering compliance with regulations like HIPAA. This is non-negotiable. Working with partners who live and breathe secure custom healthcare software development is the only way to ensure every piece of your new system is built to protect your patients' trust.
Do we have to completely rip out our existing EHR system?
Thankfully, no. That "rip and replace" strategy is incredibly disruptive, expensive, and often unnecessary. A smarter approach is to build on top of what you already have. Your Electronic Health Record (EHR) system is the core, but it doesn't have to be the limit. By using modern APIs and focusing on interoperability, you can add powerful new tools—like AI-driven diagnostics or automated administrative bots—that talk to your existing systems. It's about enhancing your current investment, not throwing it away.
How can we measure the ROI on a modernization initiative?
Proving the value of modernization comes down to tracking the right metrics across the board—financially, operationally, and clinically. You have to define these KPIs before you start. This includes financial wins (reduced overhead), operational gains (faster check-in times, less paperwork for clinicians), and clinical impact (improved diagnostic accuracy, better patient adherence). Tracking these KPIs is how you show stakeholders that this isn't just a cost center—it's a critical investment in the future of your organization.
Ready to build a clear, actionable strategy for your healthcare organization? Ekipa AI specializes in creating AI roadmaps that solve your most pressing challenges. Connect with our expert team to start designing a future-proof healthcare ecosystem today.