Evidence-Based Care Automation: How AI Improves Clinical Outcomes
Discover how evidence-based care automation with AI boosts patient outcomes and efficiency, with practical steps and real-world benefits.
Evidence-based care automation is about weaving AI-powered intelligence directly into the fabric of clinical workflows. Think of it as an intelligent co-pilot for clinicians. It's designed to close the gap between the latest groundbreaking research and the practical, day-to-day decisions made at a patient's bedside. This approach gives healthcare professionals the tools to deliver the highest standard of care, with every decision reinforced by data and driven by smart technology.
What Is Evidence-Based Care Automation?
Let's paint a picture. A doctor is managing a patient with a rare, complex condition. Instead of spending precious time manually digging through medical journals or relying solely on personal experience, an automated system instantly digests the patient's unique data. It then cross-references this profile against a vast library of clinical trials and established guidelines, presenting treatment recommendations that align perfectly with proven best practices. That's evidence-based care automation in a nutshell.
This goes far beyond just having digital records. It’s about building a living, breathing system where patient care becomes more consistent, safer, and incredibly effective. By embedding this intelligence right into the clinical workflow, we can smooth out the inconsistencies in treatment approaches, drastically cut down on human error, and make sure every single patient benefits from the entire medical community's collective knowledge. The goal is to shift from being reactive to being proactive and data-informed.
The Driving Force Behind Modern Healthcare
The move toward automation isn't just a fleeting trend; it’s a powerful market shift with serious money behind it. The global healthcare automation market, valued at USD 46.85 billion in 2025, is on track to explode to USD 119.19 billion by 2035. This incredible growth is being powered by the adoption of sophisticated AI solutions designed to automate clinical decision-making. Right now, North America is leading the pack with a 42% revenue share, thanks to its rapid embrace of new technology, as detailed in market analysis from Precedence Research.
This financial momentum points to a fundamental need in the healthcare industry. As we've discussed in our AI adoption guide, healthcare providers are under constant pressure to deliver better outcomes while keeping costs in check. Evidence-based care automation tackles this challenge head-on by:
- Standardizing Care: Making sure treatment plans are built on the most current and effective research available.
- Improving Efficiency: Automating tedious data analysis and administrative work, which frees up clinicians to spend more quality time with patients.
- Personalizing Treatment: Using a patient's specific data to fine-tune recommendations and move away from a one-size-fits-all mentality.
From Theory to Practical Application
Bringing these systems to life requires a smart blend of deep clinical knowledge and top-tier technical skill. It all kicks off with a thorough AI requirements analysis to pinpoint the areas where automation can make the biggest splash. From there, the process moves into building advanced models capable of understanding complex medical data, from electronic health records to intricate genomic information.
At its core, evidence-based care automation is about augmenting human expertise, not replacing it. It provides clinicians with the tools to make better, faster, and more informed decisions at the point of care.
Successfully rolling out these tools is a central pillar of our Healthcare AI Services. By integrating intelligent automation, healthcare organizations can truly transform how they operate, enhance patient safety, and establish a new benchmark for quality. This strategic move ensures that every clinical action is backed by a world of evidence, instantly accessible, and applied with surgical precision.
The Real-World Benefits for Patients and Providers
When you bring evidence-based care automation into a healthcare setting, you set off a powerful chain reaction. The benefits ripple out, touching everyone from the patient in the exam room to the administrator managing the budget. This isn't just about bolting on new technology; it’s a genuine shift in how healthcare works, measured, and gets better. Think of it as a force multiplier for a hospital's clinical know-how and operational muscle.
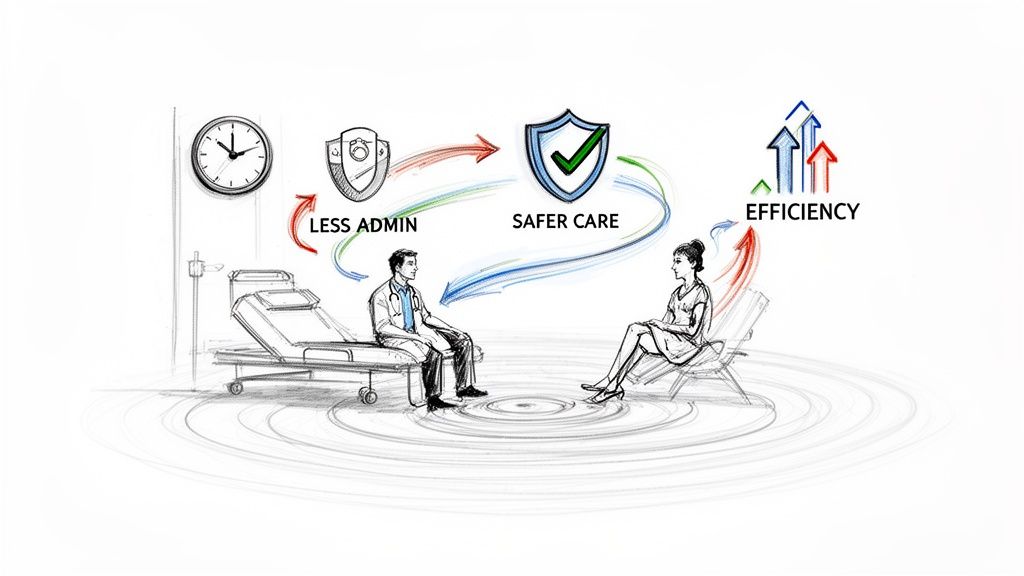
For clinicians, the most immediate and welcome change is getting their time back. By handing off tedious tasks like writing progress notes or running compliance checks to automated systems, they can put their energy where it belongs: with their patients. This is a game-changer for morale and well-being. In fact, a recent study showed that 90% of providers using AI-enhanced tools reported feeling less stress on the job.
Raising the Bar for Clinical Outcomes and Patient Safety
One of the biggest wins with evidence-based care automation is how it standardizes treatment protocols. When the latest medical evidence is baked directly into the daily workflow, it’s much easier to provide consistent, high-quality care and dramatically lower the risk of medical errors.
This directly translates to better care for patients:
- Sharper Diagnostic Accuracy: AI models can sift through mountains of patient data, spotting subtle patterns that are easy for the human eye to miss. This helps clinicians make more precise diagnoses, faster.
- Truly Personalized Treatment: Automation helps us move past one-size-fits-all medicine. It allows for care plans tailored to a patient’s unique genetics, lifestyle, and clinical history.
- Fewer Adverse Events: These systems act as a digital safety net, flagging potential drug interactions or other risks in real time, adding a critical layer of protection to every clinical decision.
By making sure every decision is grounded in solid data, evidence-based care automation makes a high standard of care the new normal, not just an occasional goal. It chips away at the clinical variability that so often leads to medical errors.
This commitment to precision and safety is what effective Healthcare AI Services are all about—turning sophisticated technology into real, measurable improvements for patients. You end up creating a system where quality isn’t just an aspiration; it's the default setting.
Driving Operational Efficiency and Financial Strength
The impact of automation extends far beyond the clinic walls. On the operational side, it smooths out countless processes that used to eat up time and money. This efficiency boost strengthens the organization's bottom line and makes it more nimble.
Here are some of the key operational victories:
- Quicker Patient Throughput: Automating things like patient intake, initial screenings, and data entry frees up staff and resources, which means shorter wait times for everyone.
- Lower Administrative Costs: AI-powered tools can manage scheduling, billing, and claims with incredible speed and accuracy, slashing the number of costly human errors.
- Smarter Resource Allocation: Data-driven insights give administrators a clearer picture of where to assign staff and equipment, ensuring resources are always where they'll do the most good.
- Reduced Staff Burnout: Taking the administrative weight off clinicians’ shoulders improves job satisfaction and helps retain top talent—a massive win for both the budget and workplace culture.
In the end, evidence-based care automation creates a virtuous cycle. Clinicians who are supported by smart tools and freed from paperwork deliver better care. Better care leads to better patient outcomes, which in turn improves operational efficiency and financial stability. It’s a clear win for the quality of care and the long-term health of the entire organization.
The Technology Driving Intelligent Healthcare
Behind every automated clinical recommendation and streamlined workflow, there’s a powerful suite of interconnected technologies. These are the engines that turn massive amounts of data into actionable, evidence-based insights, and understanding how they work is key to grasping the full potential of evidence-based care automation.
Think of it like a highly specialized medical team. Each member has a distinct role, but their combined expertise creates an outcome far greater than what any single person could achieve. This is exactly how modern AI tools are reshaping healthcare from the ground up.
The Brains of the Operation: Machine Learning
At the very core of this shift is Machine Learning (ML), a subset of Artificial Intelligence. Imagine ML models as brilliant, tireless researchers who can sift through millions of patient records, clinical trials, and research papers in seconds. They don't just read the data; they learn from it, identifying subtle patterns and correlations that are often invisible to the human eye.
These models are trained on vast datasets to predict outcomes, flag at-risk patients, and suggest personalized treatment pathways. For instance, an ML algorithm might analyze a patient's lab results, genetic markers, and lifestyle factors to recommend the most effective treatment, all based on the documented outcomes of thousands of similar cases.
The Universal Translator: Natural Language Processing
So much of the world's most valuable medical information is locked away in unstructured text—think of doctors' notes, dense research articles, and patient journals. This is where Natural Language Processing (NLP) comes in, acting as a universal translator. Simply put, NLP gives computers the ability to read, understand, and interpret human language.
NLP algorithms can scan a physician's dictated notes and automatically pull out key information like symptoms, diagnoses, and prescribed medications. This not only saves clinicians countless hours of manual data entry but also turns messy, narrative-based notes into structured data that ML models can actually use. It’s the critical link that makes sense of the complex, human side of healthcare data. To see how far this is going, you can even explore the impact of AI-driven augmented reality for a look at how these fields are converging.
The Efficiency Engine: Robotic Process Automation
While ML and NLP handle the heavy lifting of complex analysis, Robotic Process Automation (RPA) is the workhorse focused on streamlining everything on the backend. RPA uses software "bots" to automate the repetitive, rules-based tasks that are essential but incredibly time-consuming.
Think about tasks like:
- Processing insurance claims
- Managing patient billing
- Scheduling appointments and sending reminders
- Moving data between different, disconnected systems
RPA bots handle these jobs with perfect accuracy, 24/7. This dramatically cuts down on administrative overhead and frees up human staff to focus on more complex, patient-facing responsibilities. It’s no surprise the digital health automation market is set for major growth, with RPA being the fastest-growing piece of the puzzle. It’s been shown to boost efficiency by up to 50% and reduce patient wait times by 25-30%.
When you combine these technologies, you get a powerful ecosystem for evidence-based care automation. ML provides the predictive intelligence, NLP unlocks insights from text, and RPA makes sure the entire operational framework runs like a well-oiled machine. This synergy is what allows healthcare organizations to deliver smarter, faster, and more effective care. A great example of this in action is our Clinic AI Assistant.
Your Strategic Roadmap to Implementation
Bringing evidence-based care automation into your organization is a journey, not a simple flick of a switch. It takes careful planning, getting everyone on the same page, and a step-by-step approach that shows its worth along the way. Think of this as a practical guide for healthcare leaders aiming to turn a powerful idea into a working reality.
The whole thing kicks off with a focused analysis to figure out which clinical and operational spots would benefit most from automation. Not every workflow is a good candidate; the goal is to find high-volume, repetitive tasks or critical decision points where data-driven support can genuinely move the needle on outcomes and efficiency.
Building the Business Case and Assembling Your Team
Once you’ve zeroed in on the best opportunities, it’s time to build a solid business case. This isn't just about the tech—it's about tying the investment directly to what the organization cares about, like improving patient safety, cutting operational costs, or making clinicians' lives easier. Your business case needs to spell out the expected ROI, backed by solid data.
Getting buy-in from the right people is make-or-break. You'll need to talk to stakeholders from every corner of the organization, from the doctors and nurses on the floor to the IT, finance, and compliance teams. The key is to show them how this technology will help them do their jobs better, not replace them.
With everyone on board, you can put together your implementation team. This isn't a job for one department. You'll need a mix of talent:
- Clinical Champions: Respected physicians or nurses who can be advocates and guide the clinical side.
- IT and Data Experts: The technical wizards who will handle system integration, data security, and governance.
- Project Managers: The organizers who keep everything on track, on time, and on budget.
- End-Users: The people who will actually use the system every day. Their feedback is pure gold.
This simple diagram shows how these intelligent systems work—taking in data, analyzing it, and producing insights that guide better decisions.
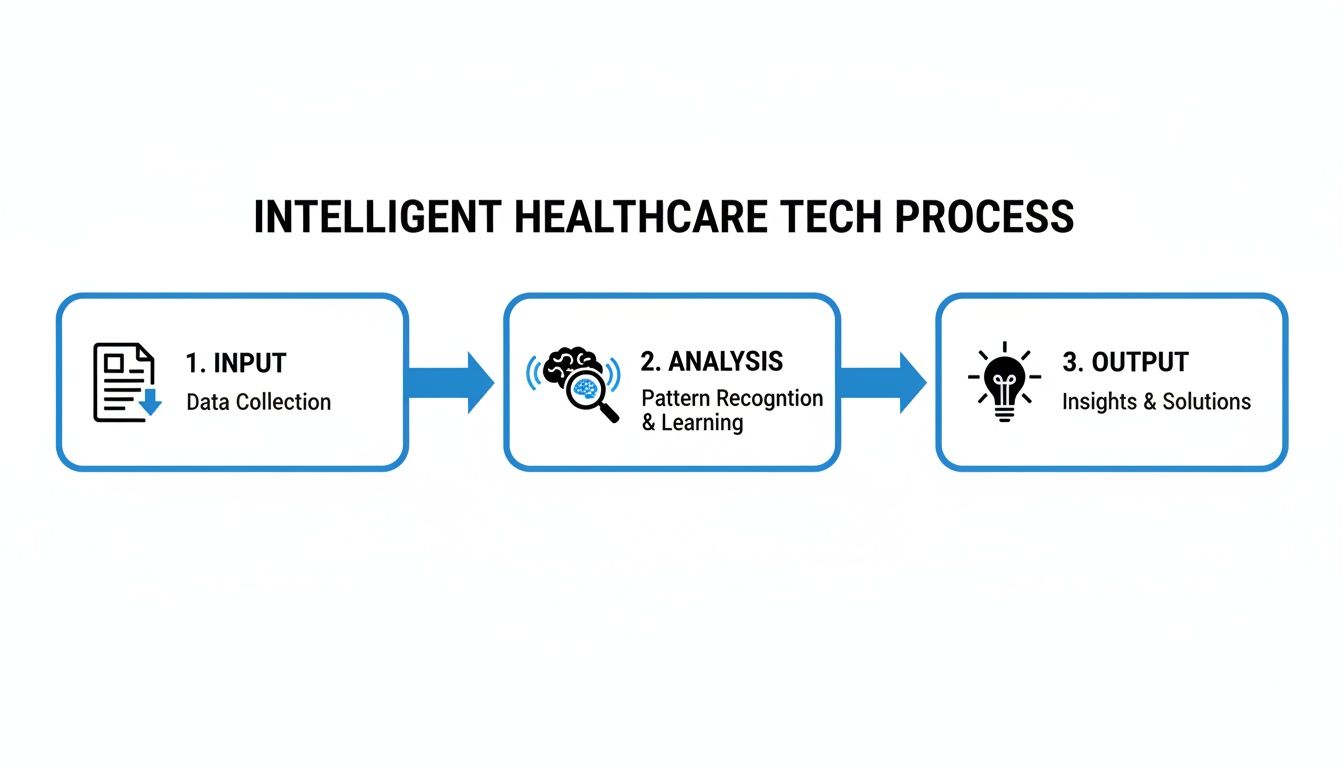
It’s a straightforward flow: raw data (Input) gets processed by smart algorithms (Analysis) to create actionable guidance (Output) that supports clinical care.
A Phased Rollout and Managing the Human Side
A big-bang launch is a recipe for disaster. Instead, go with a phased rollout. Start small with a pilot program in a single, well-defined department or workflow. This gives you a safe space to test the technology, see how users react, and score some early wins before you even think about scaling up.
The following table breaks down a typical phased approach, outlining the critical steps at each stage to ensure a smooth and successful deployment.
Implementation Roadmap Stages and Key Actions
| Phase | Key Actions | Primary Objective |
|---|---|---|
| 1. Discovery & Planning | Identify high-impact use cases, build the business case, secure stakeholder buy-in, and assemble the project team. | Establish a clear vision, justify the investment, and build foundational support for the project. |
| 2. Pilot Program | Select a limited scope, configure the system, train a small user group, and deploy in a controlled environment. | Validate the technology, gather real-world user feedback, and demonstrate tangible value with minimal risk. |
| 3. Evaluation & Refinement | Analyze pilot KPIs, collect user feedback, identify issues, and refine the system and workflows accordingly. | Learn from the initial rollout, make necessary adjustments, and prepare for a broader implementation. |
| 4. Scaled Deployment | Develop a full rollout plan, conduct organization-wide training, and deploy the system across targeted departments. | Expand the proven solution to achieve wider organizational impact and maximize ROI. |
| 5. Continuous Improvement | Monitor system performance, track long-term outcomes, and identify new opportunities for automation and optimization. | Ensure the system evolves with organizational needs and continues to deliver value over time. |
By moving through these stages deliberately, you build momentum and ensure each step is built on a solid foundation.
The success of any technology project depends far less on the software itself and far more on how well you manage the human side of change. This is non-negotiable.
Training is obviously a huge piece of this. Your staff needs to learn more than just which buttons to click; they need to understand why this change is happening. Showing them how automation can free them from tedious paperwork and let them focus on what they do best—caring for patients—is a game-changer. For a structured approach to this process, check out our guide on implementation support.
Finally, picking the right technology partner is critical. Whether you're building something from scratch or bringing in an existing platform, you need a partner who gets healthcare and has the experience to prove it. A strategic, people-focused roadmap is your best bet for making sure your evidence-based care automation initiative succeeds for the long haul.
So, you’ve decided to bring evidence-based care automation into your organization. That’s a big move. But how do you actually prove it's working?
Measuring the success of this kind of strategic shift isn't just about checking technical boxes. You need a solid way to track Key Performance Indicators (KPIs) and a clear-eyed view of your Return on Investment (ROI). This is all about connecting the dots between your investment and real, tangible improvements—clinically, operationally, and financially.
The whole point is to show that your investment is paying off where it counts. Forget simple metrics like system uptime. We need to focus on what matters to your clinicians, administrators, and the C-suite.
What Should You Actually Be Measuring?
Success with evidence-based care automation isn't a single number on a dashboard. It’s a combination of different metrics that, together, paint a full picture of the impact. The best way to start is by sorting your metrics into a few key buckets.
Here’s a practical breakdown of KPIs you should consider tracking:
- Clinical KPIs: This is where the rubber meets the road. These metrics show the direct impact on patient care. Keep an eye on adherence rates to clinical guidelines, a drop in medical errors, and better patient outcomes for specific conditions, like lower readmission rates.
- Operational KPIs: These are all about efficiency. You'll want to track things like reduced time spent on administrative tasks for your clinical staff, faster patient throughput from admission to discharge, and an overall boost in staff productivity or capacity.
- Financial KPIs: This is how you tie it all back to the bottom line. Measure cost savings from fewer administrative errors, more efficient use of resources, and the total cost per patient episode.
Nailing down a measurement strategy from the very beginning is crucial. Our AI strategy consulting can help you set these benchmarks, and a Custom AI Strategy report can even help forecast what's possible, giving you realistic goals before a single line of code is written.
Showing the Real Return on Your Investment
Once you have your KPIs, you can start building a compelling ROI case. The basic formula is straightforward—(Financial Gain - Investment Cost) / Investment Cost—but the tricky part is accounting for all the gains. You’ll find value in both direct cost savings and the more subtle (but powerful) efficiency benefits.
For instance, our AI Automation as a Service can automate billing and claims, which creates a direct, easy-to-calculate ROI. But what about the value of keeping your best nurses and doctors because they're less burned out? That's just as important, even if it's harder to put a precise dollar figure on it. A powerful business case includes both.
The most convincing arguments for evidence-based care automation are built on clear, quantifiable data. When you can tie every KPI back to either saving money or improving care, you create a story that stakeholders can't ignore.
The market is already telling this story. The adoption of AI in healthcare is growing by double digits year after year. In fact, 81% of executives expect generative AI to have a major impact on their productivity by 2025. And with an 82% ROI realization reported for AI projects, the financial argument is getting stronger every day.
This isn't just a trend; it's a response to a global shortage of healthcare workers that makes automation essential for long-term survival. You can learn more about the broader shift by exploring these healthcare automation market trends.
Navigating the Challenges of AI in Healthcare
While the promise of evidence-based care automation is huge, the road to getting there isn't always smooth. Let's be honest—adopting these powerful tools means wrestling with some very real challenges around data security, ethics, and system integration. If you want to build a strategy that works, you have to tackle these issues head-on.
The first and most immediate hurdle is HIPAA compliance and data security. We're talking about some of the most sensitive data on the planet. Any automation system has to be built like a fortress, with security that is absolutely unbreachable. This goes way beyond standard encryption; it requires strict access controls, frequent security audits, and a clear data governance plan that spells out exactly how patient information is handled, stored, and used by AI. Building the right internal tooling ensures these processes are robust and secure from the start.
Addressing Algorithmic Bias and Ethical Concerns
Next up is the very real risk of algorithmic bias. AI models are only as good as the data they learn from. If that data contains existing health disparities—and most historical data does—the AI can easily end up perpetuating or even worsening those biases. Think about a diagnostic tool trained mostly on data from one demographic; it could be dangerously inaccurate for others.
Fighting this requires a conscious, ongoing effort:
- Diverse Data Sets: You have to intentionally seek out and use training data that truly reflects your entire patient population.
- Transparency and Explainability: This is where "explainable AI" (XAI) comes in. These techniques let you see why an AI made a certain recommendation, giving clinicians the power to question and override a bad call.
- Continuous Auditing: Algorithms aren't "set it and forget it." They need regular testing to check for biased results and require constant fine-tuning.
At the end of the day, the guiding principle has to be this: technology should enhance, not replace, a clinician's judgment and empathy. These tools are powerful assistants, but the final decision must always belong to a human expert.
Integrating with Legacy Systems and Fostering Adoption
Let’s talk tech. Many hospitals and clinics run on a maze of older IT systems that weren't built to talk to each other. Trying to plug modern AI tools for business into this kind of environment without causing chaos is a massive technical lift. It often demands specialized skills to build custom APIs and data pipelines, which is a big piece of any custom healthcare software development project.
But the technical side is only half the battle. You also have to win over the people who will actually use the tools. Clinicians are, and should be, skeptical of new technology that affects patient care. Getting them on board means proving the value, offering solid training, and making them part of the process from the very beginning. As we’ve explored in our AI adoption guide, managing the human side of change is every bit as critical as the technology itself.
Getting through these complexities isn't easy, and it takes real experience. Our expert team partners with organizations to create automation strategies that are not only powerful but also compliant and trusted. We're here to make sure your move into evidence-based care automation is both successful and responsible.
Frequently Asked Questions (FAQ)
We get it—adopting new technology in a clinical setting brings up a lot of questions. Here are straightforward answers to some of the most common ones we hear from healthcare leaders.
Where’s The Best Place To Start?
Before you even think about software, start with a focused assessment. The first step isn't buying a tool; it's pinpointing the exact clinical and operational headaches where automation can make the biggest difference.
A thorough AI requirements analysis will help you identify those high-impact areas. From there, you can define clear goals and honestly evaluate your organization's data readiness. Our AI Strategy consulting tool is designed to help you build a practical roadmap, ensuring your first project is a clear win that aligns with your bigger vision.
How Does This Fit With Our Existing EHR System?
It has to be seamless—otherwise, it's just another login for your team to juggle. Modern care automation platforms are built from the ground up to integrate with major Electronic Health Record (EHR) systems.
Think of it as a smart layer that works on top of your current setup. It uses secure APIs to pull necessary patient data in real-time, run its analysis, and then push valuable insights or automated notes right back into the patient's chart. This integration is a core part of our AI Product Development Workflow, because avoiding data silos and making life easier for clinicians is non-negotiable.
Are We Trying To Replace Our Healthcare Professionals?
Not a chance. This is about augmentation, not replacement. The entire point is to empower your skilled professionals, not sideline them.
These AI tools for business are designed to be expert assistants, taking on the heavy lifting of data analysis and repetitive administrative tasks. This frees up your doctors, nurses, and specialists to focus on what they do best: complex decision-making, direct patient interaction, and providing empathetic, high-quality care.
By automating the routine, you allow your team to operate at the top of their license, which is a proven way to reduce burnout and improve patient outcomes. You can see this principle in action in several real-world use cases where technology amplifies human expertise.
Ready to see how evidence-based care automation can work for your organization? Ekipa AI can help. We specialize in turning your biggest operational challenges into scalable, impactful solutions.
Let our expert team show you what's possible and help guide your first steps.