Solving Clinical Data Integration Challenges in Healthcare
Discover proven strategies to solve clinical data integration challenges. Learn how to break down data silos and unlock AI-driven healthcare innovation.
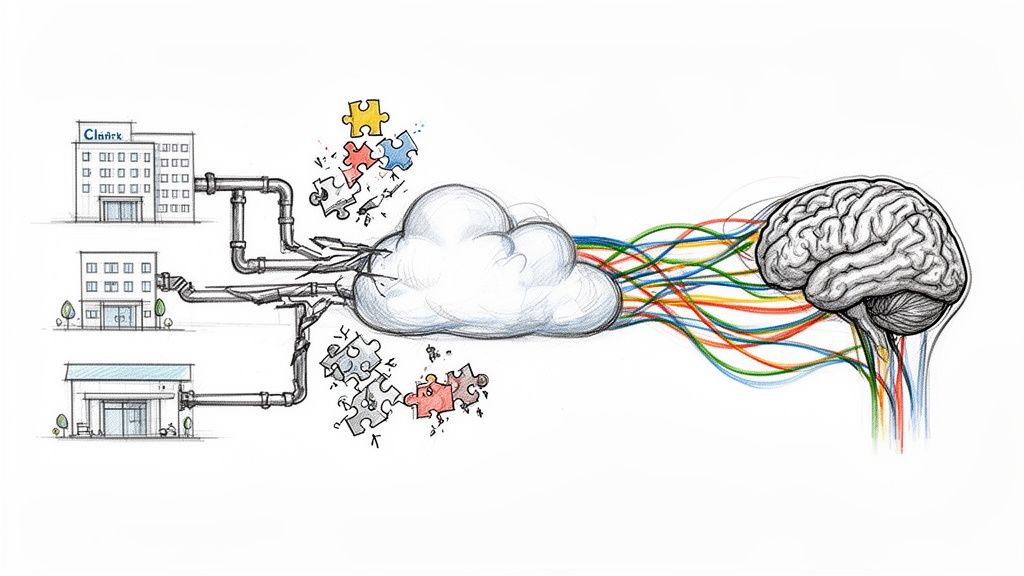
Healthcare organizations are absolutely swimming in data. But here's the problem: that data is almost never in one place. It's locked away in separate, disconnected systems, creating what we call clinical data integration challenges. Think of the fragmented records spread across different EHRs, lab systems, and imaging databases. This isn't just an IT nuisance; it's a direct threat to patient safety, a major drag on hospital operations, and a roadblock to genuine innovation.
The Real-World Cost of Disconnected Health Data
If you ask any clinician, they'll tell you that having a patient's complete medical history at their fingertips is non-negotiable for providing good care. But the day-to-day reality is a messy patchwork of incompatible systems that simply refuse to talk to each other. This digital disconnect forces doctors and nurses to act like detectives, trying to piece together a coherent patient story from scattered clues.
The gap between what's needed and what's possible is stark. The statistics below paint a clear picture of a system-wide problem that needs immediate attention.
The Disconnect Between Need and Reality in Data Integration
This table summarizes the critical gap between the acknowledged importance of data integration in healthcare and the practical challenges organizations face in achieving it.
| Metric | Finding | Implication for Healthcare Leaders |
|---|---|---|
| Provider Acknowledgment | Nearly 90% of healthcare providers believe seamless access to patient records is crucial for quality care. | The demand for integrated data is nearly universal among front-line staff. |
| Integration Hurdles | A staggering 40% of providers report facing major hurdles in integrating their IT systems. | Despite the clear need, nearly half of the workforce is hamstrung by technology barriers. |
| Patient Safety Impact | A lack of data interoperability is linked to medical errors, redundant testing, and delays in care. | The cost of inaction is measured not just in dollars, but in negative patient outcomes. |
These numbers tell a story of good intentions clashing with technological reality, a challenge that leaders must address to move their organizations forward.
Why a Single Source of Truth Is So Critical
Imagine a patient's health story is a book. The primary care EHR is one chapter, the hospital's lab system is another, and the specialist’s imaging archive is a third. Without integration, providers are forced to read just one chapter at a time, completely missing the context that connects them.
A unified data source—what we call a "single source of truth"—binds all those chapters together into one complete, coherent story. When every provider has the full picture, great things happen:
- Improved Patient Safety: Critical details like allergies or a history of adverse drug reactions are front and center, helping to prevent dangerous medical mistakes.
- Better Operational Efficiency: Your staff can stop wasting time chasing down records, faxes, and lab results and focus their energy back on caring for patients.
- More Accurate Diagnostics: With a complete longitudinal health record, clinicians can spot trends, connect dots, and make far more informed decisions.
Building the Foundation for Healthcare's Future
The pressure on healthcare leaders to get this right is mounting, because clean, integrated data is the bedrock of all future progress. Without it, even the most advanced tools are basically useless.
Fragmented data is the single biggest bottleneck holding back truly transformative technologies. You can't run predictive analytics or AI-powered diagnostics on messy, incomplete information. They need a reliable, consolidated data ecosystem to work.
This is why solving clinical data integration challenges has evolved from an IT project into a core business strategy. For any organization looking to adopt advanced Healthcare AI Services, building this solid data foundation is the essential first step. It's the only way to turn data chaos into a powerful strategic asset that drives better outcomes for everyone.
Breaking Down the Core Integration Barriers
Once you get past the big-picture idea of data silos, you start to see the real, on-the-ground hurdles that bring a modern healthcare data strategy to a screeching halt. These aren't just abstract IT problems. They are operational roadblocks with very real consequences for patient care and the bottom line. To get this right, you have to take a hard, honest look at the technical, semantic, and organizational mess you're dealing with.
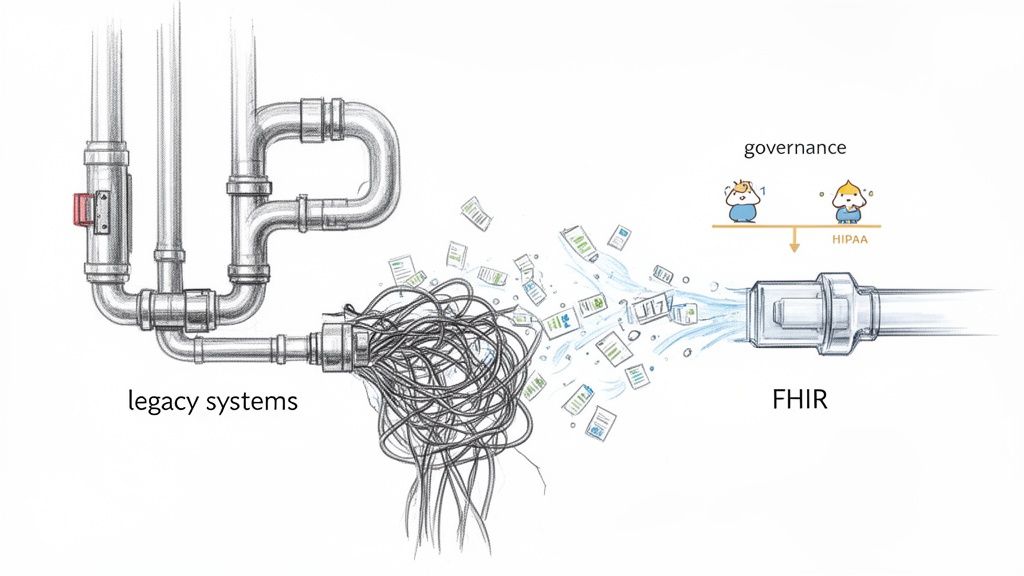
Think of your legacy systems like the old, corroded plumbing in a historic building. They were installed decades ago using different materials and standards. If you try to connect a modern, high-pressure fixture to that old network, it’s not just difficult—it’s a recipe for disaster. Each custom patch and workaround just adds to your technical debt, making future upgrades a bigger and more expensive nightmare.
The 'Tower of Babel' Problem of Semantic Interoperability
Even if you get the pipes connected, a deeper challenge emerges: semantic interoperability. This is all about making sure different systems can not only swap data but actually understand what it means. It’s healthcare's very own 'Tower of Babel' scenario.
For instance, one EHR might log a myocardial infarction with the code "MI," while a connected lab system uses a different code for "heart attack." They’re describing the exact same clinical event, but without a common language, the systems see them as two different things. This kind of miscommunication leads directly to fragmented patient histories and deeply flawed analytics.
At its core, semantic interoperability is about ensuring that data retains its context and meaning as it moves between systems. Without it, you’re just moving digital noise from one database to another.
This is exactly why standards like HL7v2 and the more modern FHIR (Fast Healthcare Interoperability Resources) were created. The problem is, adoption is all over the place. Many organizations are stuck trying to translate data from ancient, proprietary formats, which creates a massive amount of friction. It often takes a focused AI strategy consulting engagement just to map out these different data dialects and build a coherent translation layer.
The Quality Trap of 'Garbage In, Garbage Out'
Let's say you've managed to solve the technical and semantic issues. You're still left with the quality of the data itself, which is often a huge hurdle. The old adage of "garbage in, garbage out" is especially brutal in healthcare. Incomplete patient records, typos in medication names, or inconsistent data entry habits can make an entire dataset dangerously unreliable.
This problem gets amplified when you start prepping data for advanced analytics or machine learning. Bad data doesn't just give you inaccurate reports; it can lead to clinical conclusions that put patients at risk. This is why investing in something like AI Automation as a Service to automatically cleanse, standardize, and validate data streams is no longer a luxury—it’s a necessity before you can do anything meaningful with it.
Navigating Governance and Compliance Tightropes
Finally, a complex web of data governance and regulatory compliance is draped over this entire process. Simply establishing clear rules for who owns the data, who can access it, and how it’s secured is a monumental task. Every single decision has to be viewed through the lens of regulations like HIPAA.
Ensuring compliance, particularly when handling Protected Health Information (PHI), is a make-or-break integration barrier. The technical requirements for security and privacy have to be designed into the integration architecture from the very beginning. This can get incredibly complicated during projects like a HIPAA SharePoint migration or any other major system overhaul.
This isn’t just about ticking boxes for auditors. It's about building and maintaining trust with your patients and avoiding crippling legal and financial penalties. The sheer volume of data makes this even more intimidating. Healthcare providers generate roughly 30 petabytes of data every year, yet some studies suggest that nearly 47% of it is never used because of integration and compliance roadblocks.
Each of these barriers directly impacts daily operations and can easily derail ambitious AI initiatives. It really underscores why a comprehensive strategy, built by an expert team who has done this before, is the only way to build a solid, compliant data foundation.
How Poor Integration Sabotages AI and Operations
Disconnected data isn’t some abstract IT headache. It’s an active saboteur, undermining your most important strategic goals right now. When clinical data is scattered across different, non-communicating systems, the consequences are very real, impacting everything from patient safety to your bottom line.
These data gaps create dangerous blind spots.
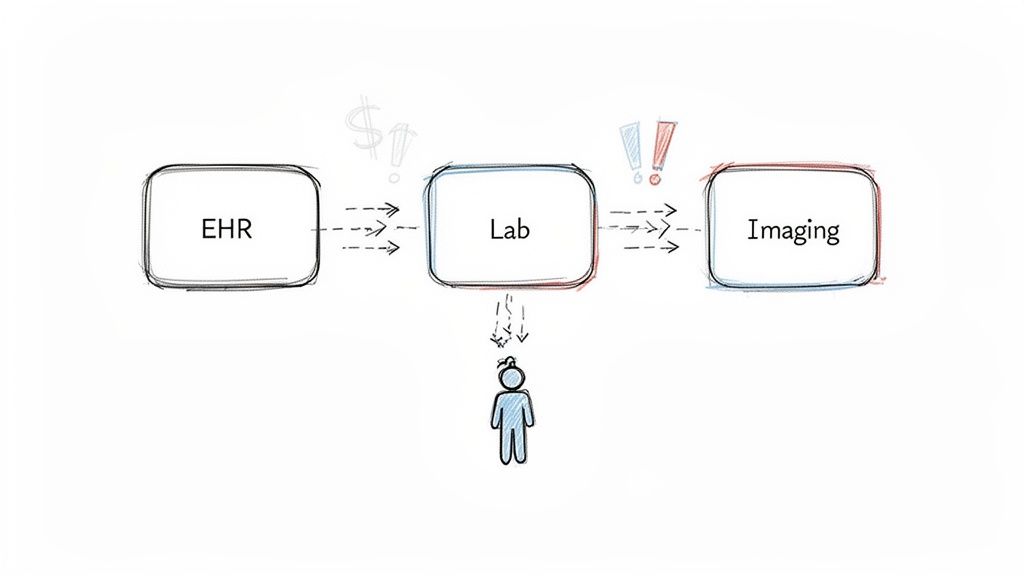
Imagine a patient with a severe penicillin allergy documented in their primary care doctor's EHR. That same patient is rushed to the hospital for emergency surgery. If the hospital’s system can’t see the data from the primary care clinic, that critical allergy information is invisible to the surgical team. This isn't just a hypothetical; it's a preventable risk that happens every single day because of data silos.
This failure to share information is one of the most glaring consequences of poor clinical data integration. Each system holds a vital piece of the patient puzzle. Without a way to put those pieces together, clinicians are forced to make high-stakes decisions with an incomplete picture.
Crippling Predictive Models and AI Initiatives
If you’re looking to bring in advanced Healthcare AI Services, a fragmented data foundation is your biggest roadblock. AI and machine learning models can do amazing things, but their power comes directly from the quality and completeness of the data they learn from.
Think about an AI model built to predict sepsis risk. To work properly, it needs a constant, comprehensive flow of data—vital signs, lab results, medication history, and clinical notes. If that data is stuck in different systems and arrives late, or not at all, the model's predictions become unreliable.
An AI model trained on incomplete or fragmented data is worse than no model at all. It creates a false sense of security while delivering inaccurate predictions, potentially leading clinicians to miss critical warning signs or intervene incorrectly.
This is the classic "garbage in, garbage out" problem, but with much higher stakes. Any investment in sophisticated AI solutions is built on quicksand without a unified data stream. An algorithm simply can't see what the data doesn't show it, turning a promising tool into a new source of risk. As our real-world use cases make clear, a solid data foundation is non-negotiable for success.
Undermining Population Health and Driving Waste
Beyond the immediate bedside, poor integration throws a wrench into bigger strategic efforts like population health management. The whole point is to spot at-risk groups and intervene before they get sick, but how can you do that without seeing the complete health journey of your community? You can't manage chronic disease across a population when you only have scattered fragments of each patient's story.
And then there's the operational waste. The cost of these data gaps is staggering. Staff waste countless hours manually piecing together records, chasing down faxes, and re-entering information that already exists somewhere else. This isn't just inefficient—it's a massive driver of administrative overhead and employee burnout.
Every minute a nurse spends on the phone tracking down a lab result from another clinic is a minute they can't spend with a patient. Tackling these clinical data integration challenges isn't just about getting ready for AI. It's about fixing the expensive and dangerous problems plaguing healthcare operations today. A smart integration strategy transforms that fragmented data from a liability into a powerful asset that fuels better care and a healthier bottom line.
Your Strategic Roadmap for Data Unification
We've talked about the problems, but recognizing them is the easy part. Building the solution—that takes a real plan. It’s time to stop discussing clinical data integration challenges and start fixing them.
A winning strategy isn’t some massive, one-and-done project. Think of it as a methodical journey, one that transforms your data from a frustrating liability into your most valuable asset. This roadmap breaks that journey down into clear, manageable steps. Trying to fix everything at once is a recipe for disaster, leading to stalled projects and wasted money.
The stakes are high. When you let data stay fragmented, the consequences cascade, leading directly to operational failures and, ultimately, sabotaging your AI initiatives before they even get off the ground.
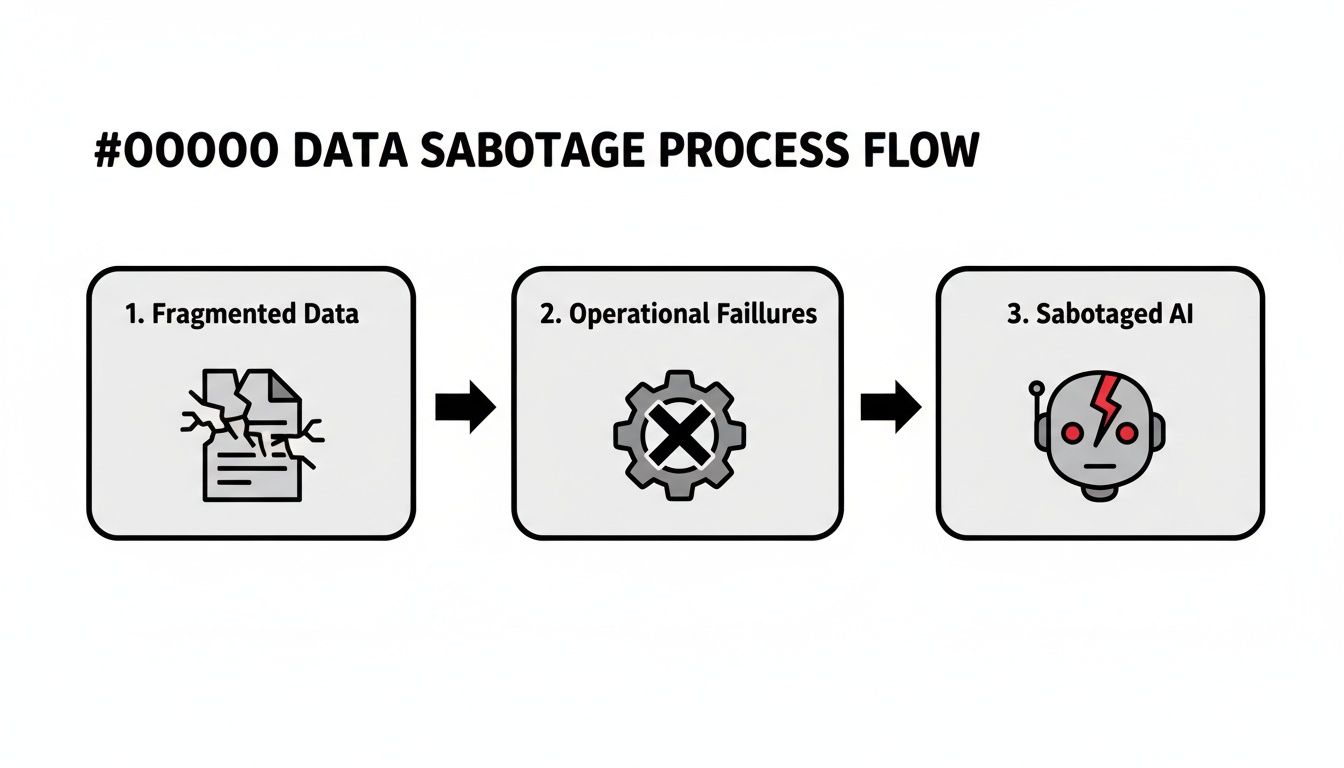
This is the reality of inaction. Siloed information doesn't just create headaches; it actively undermines your most important technology investments. That's why we have to start at the foundation.
Phase 1: Audit and Assess Your Data Ecosystem
You can't build bridges until you know where the islands are. The very first step is a thorough audit of your entire data world. This means getting your hands dirty and identifying every single system that holds clinical information—from your main EHR and lab systems all the way down to those forgotten departmental spreadsheets and ancient databases.
This phase is all about achieving total clarity. The goal here is to document every data format, map out how information currently moves (or doesn't), and pinpoint the most critical bottlenecks and quality nightmares. It’s this deep-dive analysis that provides the raw intelligence needed to build a smart, effective integration strategy.
Phase 2: Standardize and Modernize Your Architecture
With a clear map of your current state, you can start building the modern infrastructure needed to let data flow freely. This isn't about a "rip and replace" strategy that disrupts everything overnight. It's about a smarter, strategic adoption of modern standards and a more flexible architecture.
The old way of connecting systems one-by-one is fragile and expensive. A modern approach, however, builds a resilient foundation for the future. The table below contrasts these outdated tactics with the strategic solutions needed today.
Strategic Approaches to Key Integration Challenges
| Challenge | Traditional (and Flawed) Approach | Modern Strategic Solution |
|---|---|---|
| Data Silos | Building brittle, point-to-point connections for every new need. | Implementing a unified data fabric or hub that acts as a central access point for all systems. |
| Inconsistent Standards | Forcing outdated formats like HL7v2 to work with modern tools. | Adopting FHIR as the "lingua franca" for data exchange, using its flexible API-based structure. |
| Lack of Oversight | Letting each department manage its own data rules (or lack thereof). | Establishing a central governance framework with clear rules for data ownership, access, and quality. |
| Poor Data Quality | Relying on manual cleanup projects that are slow and never-ending. | Deploying AI-powered automation to clean, validate, and standardize data at scale. |
By moving from reactive fixes to a proactive, architectural strategy, you build a system that's not just integrated but also scalable and secure for the long haul.
Phase 3: Automate and Optimize With AI
This final phase is where you really start to accelerate. Let's be honest: manually cleaning, mapping, and validating massive volumes of clinical data is painfully slow, expensive, and riddled with human error. This is where AI-driven automation changes the entire equation.
By injecting intelligent automation into your integration workflow, you can slash the manual effort and dramatically improve data quality at scale. This transforms a resource-draining chore into a fast, repeatable process.
This is where you can bring in tools to do the heavy lifting. For instance, sophisticated machine learning algorithms can be trained to spot and correct inconsistencies across thousands of patient records in minutes. Natural language processing (NLP) can pull structured, usable data from unstructured physician notes—a task that would take a human team months to complete. This is the key to making the entire journey not just achievable but also cost-effective and sustainable, setting the stage for the powerful analytics and AI models you want to build.
One of the most effective ways to do this is with a purpose-built AI-powered data extraction engine that is designed to handle the unique complexities of healthcare information.
How a Strategic Partner Accelerates Integration
Trying to untangle the web of technical, semantic, and organizational knots in clinical data integration is not a solo mission. When organizations try to navigate this complex terrain with only their internal teams, they often hit dead ends, blow their budgets, and get stuck in a cycle of frustration. A strategic partner brings the specialized expertise, proven methods, and technical muscle needed to turn a daunting challenge into a successful, manageable project.
Bringing in outside help can dramatically speed up the process. The benefits are similar to what you might see with outsourced IT support, where deep experience drives real progress. This isn’t just about handing off a task; it’s about collaborating with a team that has already cleared these specific minefields and can show you the most direct path forward.
From Ambiguity to a Clear Roadmap
The first thing a good partner does is cut through the noise to create a precise, actionable strategy. Many organizations know they have a data problem but can't quite put their finger on its full scope or figure out where to begin. This is where a structured, methodical approach changes everything.
An expert partner starts with a deep discovery process. They map out your entire data ecosystem, pinpoint the most critical pain points, and make sure your integration goals line up with what the business is trying to achieve. The result isn't some generic template; it's a customized plan that details the specific steps, technologies, and milestones needed to get you where you need to go.
A strategic partner doesn't just offer solutions; they first help you ask the right questions. By bringing an outside perspective, they can challenge internal assumptions and uncover hidden opportunities, ensuring the integration strategy is built on a solid foundation of business reality.
This initial planning is essential for getting executive buy-in and setting expectations everyone can agree on. It turns an overwhelming idea into a series of achievable projects. The urgency here is real—the healthcare data integration market, valued at USD 23.48 billion in 2025, is projected to hit USD 43.66 billion by 2034, pushed by massive EHR adoption and the growing demand for data-driven insights.
Building the Right Infrastructure and Tools
Once the strategy is locked in, it's time to build. A partner brings the technical horsepower to construct the infrastructure needed for data to flow smoothly and reliably. This often means designing and implementing the right tools to manage complex data pipelines, from pulling data in and transforming it to validating its quality and keeping it secure.
This is where specialized skills become invaluable. For instance, a partner can:
- Develop custom connectors to finally pull data from those stubborn legacy systems that don't have modern APIs. This is a key part of custom healthcare software development.
- Implement a solid data governance framework from the very beginning to ensure quality and compliance.
- Deploy AI-powered automation to handle the tedious work of data cleansing and standardization at a massive scale.
Following a well-defined AI Product Development Workflow keeps the project on track, managing everything from the initial concept to deployment and ongoing improvements. This structured approach prevents scope creep and guarantees the final solution actually solves the problems identified at the start. By combining strategic oversight with deep technical execution, a partner truly accelerates your journey toward a unified, intelligent healthcare ecosystem.
Your Path to a Unified Healthcare Ecosystem
Let’s be honest: tackling clinical data integration is a massive undertaking. It’s complex, it’s messy, but it’s absolutely solvable. In fact, it's the non-negotiable foundation for the future of healthcare. The only way to succeed where so many others have stalled is with a smart, phased approach.
The path from siloed data to a truly intelligent healthcare ecosystem isn't just a tech project; it's a strategic necessity. For too long, disconnected information has dictated the quality of care, operational efficiency, and the pace of innovation. A solid integration strategy is what finally unlocks the real-world potential of analytics and AI.
The real goal here is to build a seamless data environment where information flows freely and securely. Imagine empowering every clinician with the complete patient story, right when they need it most. This isn't some far-off dream anymore—it's an achievable reality.
It's time to stop reacting to data problems and start proactively building a solution that lasts. If you're ready for a clear, actionable plan to transform your data infrastructure and finally see what AI-driven healthcare can do, connect with our expert team.
Frequently Asked Questions
It’s natural to have questions when you’re staring down a complex clinical data integration project. Let’s tackle some of the most common ones we hear from healthcare leaders so you can move forward with clarity.
Where Do We Even Begin?
The best first step is always a thorough data ecosystem audit. Before you can connect anything, you have to know what you have. Think of it like mapping out all your separate islands of data before you can even think about building bridges between them.
This means identifying every system that holds clinical information, figuring out its format, tracing how data moves (or doesn't move), and finding the biggest logjams. This discovery phase, which is a core part of our AI requirements analysis, gives you the blueprint for an integration strategy that actually works. It helps you focus your efforts on the problems that matter most, instead of trying to fix everything at once.
How Do We Choose Between Standards Like HL7 and FHIR?
This is a big one. While a lot of your older, trusted systems probably still run on standards like HL7v2, the future is undeniably FHIR (Fast Healthcare Interoperability Resources). FHIR was built for the modern web. It uses APIs that are much more flexible and easier for developers to work with, making it the clear choice for new projects.
So what do you do in the meantime? For most organizations, a hybrid approach makes the most sense. You can use integration engines that act as translators, converting data from your legacy HL7 systems into the standardized FHIR format. This clever strategy lets you build a modern, unified data layer without having to rip and replace everything you already have.
This Sounds Expensive. How Can We Justify the Cost?
You need to build a business case that focuses on two things: reducing risk and creating new value.
First, the risk. Fragmented data isn't just an inconvenience; it’s a direct cause of clinical errors, a nightmare for compliance, and a source of huge operational waste. These are real costs that are already hitting your bottom line every single day.
Then, there’s the value. A unified data ecosystem is the launchpad for the projects that truly move the needle—things like predictive analytics to improve patient outcomes, streamlined clinical workflows, and the promise of personalized medicine. A well-structured AI strategy consulting process can help you model the financial upside of these initiatives, making it much easier to get the green light from your leadership team.
Can AI Actually Help with the Integration Work Itself?
Yes, absolutely. This is where things get really interesting. AI and machine learning are fantastic tools for accelerating the heavy lifting of data integration.
Modern AI tools for business can automate some of the most painful, manual tasks, like mapping data fields between systems, cleaning up messy data, and enforcing standards. For example, natural language processing (NLP) can pull structured data out of unstructured sources like doctors' notes, a task that would take a human team ages to complete.
Using AI Automation as a Service can drastically cut down the time and cost of an integration project. It frees up your best people to work on strategy instead of getting bogged down in manual data wrangling. As we explored in our AI adoption guide, this is how you make integration achievable at scale.
Ready to turn your scattered data into your most powerful asset? Ekipa AI can deliver a Custom AI Strategy report in just 24 hours, giving you a clear, actionable roadmap to solve your clinical data integration challenges. Our work is backed by our expert team, ready to guide you at every step.



