AI in Physician Decision Support Systems for Better ROI
Discover how AI-powered physician decision support systems improve patient care, streamline workflows, and deliver a measurable return on investment.

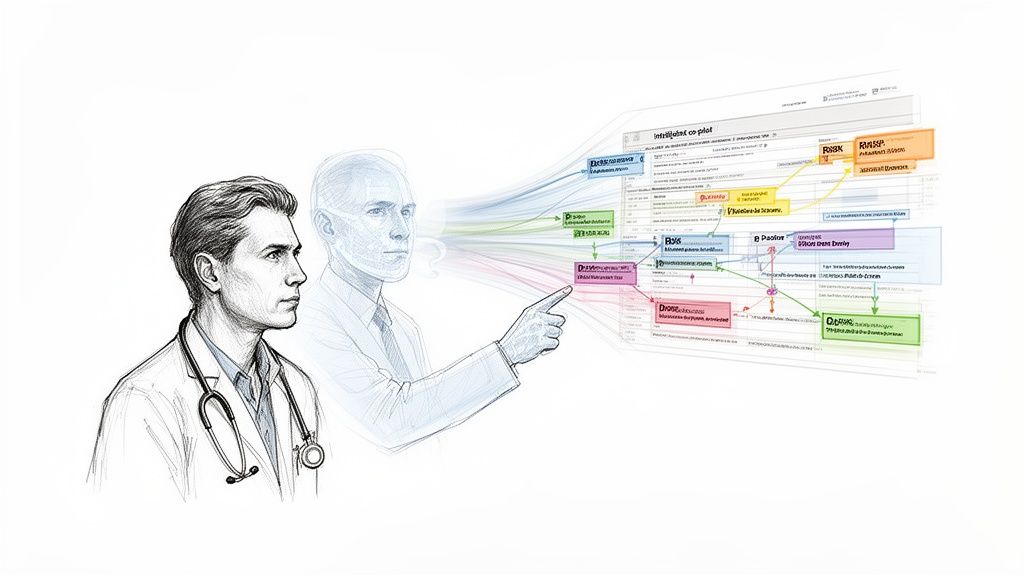
Imagine having a seasoned medical expert looking over the shoulder of every physician, instantly crunching patient data to flag critical risks and suggest proven treatment paths. That’s the reality of modern physician decision support systems (PDSS). Think of them as an intelligent co-pilot, helping to navigate the vast sea of medical data to provide clear, actionable recommendations right at the point of care.
From Medical Records To Actionable Insights
In any given clinical setting, doctors are flooded with information from electronic health records (EHRs), lab results, and imaging scans. A physician decision support system acts as an intelligent filter, cutting through that noise by analyzing massive datasets in real time to offer timely, context-aware suggestions.
This is a huge leap from the basic, rule-based alert systems of the past. Today's advanced platforms are sophisticated AI engines that personalize patient care and help clinicians sidestep diagnostic errors. For healthcare leaders and CTOs, this shift is a strategic move toward operational excellence. It’s about giving clinicians better tools, not replacing their expertise.
The Core Purpose of a PDSS
The fundamental goal here is to enhance clinical judgment, not automate it. These systems are built to help with complex decisions by providing a second set of eyes, one that’s backed by enormous amounts of data and evidence-based guidelines. At its heart, a PDSS is all about enabling data driven decision making in a clinical setting, pushing practice beyond intuition toward reproducible, evidence-based care.
By plugging directly into clinical workflows, a well-designed PDSS can flag potential drug interactions, suggest differential diagnoses based on reported symptoms, or recommend care pathways that align with the latest medical research.
The real magic happens when raw data becomes a practical insight. These systems don't just show you information; they interpret it. For instance, a system might analyze a patient's genetic markers alongside their current medications to predict the risk of an adverse reaction—a calculation that’s nearly impossible for a human to make on the fly. You can see how our own AI-powered data extraction engine helps turn this kind of unstructured data into valuable insights.
This capability is essential for any organization committed to delivering superior patient outcomes. By putting powerful Healthcare AI Services to work, hospitals and clinics can transform their patient data from a passive archive into an active tool for improving both care quality and operational efficiency. The result is a healthcare environment that is safer, more consistent, and ready to tackle the complexities of modern medicine.
The Two Brains Behind Clinical AI Systems
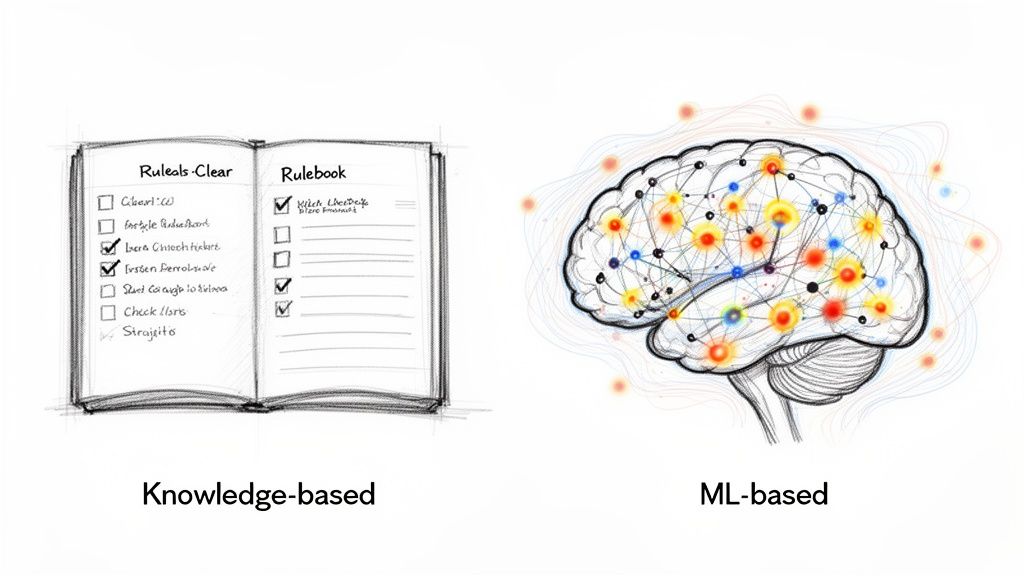
Not all physician decision support systems "think" alike. Under the hood, they generally run on one of two very different engines, each with its own set of strengths. Figuring out which approach is right for your organization is the first step toward successful implementation.
At a high level, the two models are knowledge-based systems and machine learning-based systems. One operates like a digital encyclopedia, strictly following pre-set rules. The other acts more like a seasoned detective, sifting through mountains of data to uncover hidden patterns.
Knowledge-Based Systems: The Digital Rulebook
The classic and most common form of clinical decision support is the knowledge-based system. Think of it as an enormous, interactive medical textbook that's been programmed with a clear set of “if-then” logic. These rules aren’t just made up; they come directly from established clinical guidelines, medical literature, and expert consensus.
Their logic is straightforward and easy to follow. For instance, if a patient’s lab work shows critically low potassium (the “if”), the system flags it and might suggest a specific supplement protocol (the “then”). Because every recommendation is tied to a specific, pre-defined rule, clinicians can immediately understand why the system made its suggestion. This transparency is a huge reason for their widespread adoption and trust.
This model is the workhorse of the industry, currently holding a 60-70.1% market share. Hospitals love them because they deliver reliable, evidence-based recommendations that help standardize care. In fact, studies show these systems can slash clinical practice variability by as much as 35%—a major win for any leader focused on reducing preventable errors. You can dig into more of this data in the full clinical decision support systems market report.
Machine Learning-Based Systems: The Data Detective
If knowledge-based systems are the established veterans, then machine learning (ML)-based systems are the forward-thinking newcomers. They represent the next generation of AI solutions in healthcare. Instead of relying on hand-coded rules, these systems learn directly from historical data—and lots of it.
They analyze millions of anonymized patient records, lab results, and even medical images to spot complex patterns that a human might miss. This makes them incredibly good at prediction.
For example, an ML model could analyze a patient's vitals, medical history, and demographics to forecast their risk of developing sepsis in the next 12 hours. It learns the subtle combination of factors that preceded sepsis in thousands of past cases, allowing it to flag at-risk patients long before they show obvious symptoms. For complex challenges like this, specialized AI strategy consulting can help map out the most effective ML approach.
A key difference with machine learning is that the models get smarter over time. As they process more data, their algorithms become more accurate and refined, continuously improving their predictive power. This is a core advantage of modern AI tools for business.
Comparing The Two Approaches
To decide between a knowledge-based or machine learning-based system, you have to ask what you’re trying to achieve. Is your main goal to standardize care based on established best practices? Or are you aiming to unearth new clinical insights from your own patient data?
The table below breaks down the key differences to help guide that conversation.
Knowledge-Based vs Machine Learning-Based PDSS
This comparison highlights the two primary types of physician decision support systems, detailing their technology, characteristics, and ideal use cases.
| Feature | Knowledge-Based Systems | Machine Learning-Based Systems |
|---|---|---|
| Foundation | Explicitly programmed "if-then" rules | Algorithms that learn from data patterns |
| Transparency | High: Logic is clear and traceable ("white box") | Often Low: Can be a "black box," making it hard to explain predictions |
| Best For | Standardizing care, enforcing protocols, and avoiding known errors | Predictive analytics, risk stratification, and personalized medicine |
| Data Needs | A curated knowledge base of clinical guidelines | Large, high-quality historical datasets for training |
| Example | Alerting a physician about a potential drug-allergy interaction. | Predicting the likelihood of hospital readmission based on patient history. |
In the end, the path forward isn't always about choosing one over the other. Many healthcare organizations are now exploring hybrid models that pair the reliability of knowledge-based rules with the predictive insights of machine learning. This combination often creates the most powerful and versatile physician decision support systems.
Tying Better Medicine to a Healthier Bottom Line
Bringing a physician decision support system into your hospital isn't just about upgrading your tech stack; it’s a core business move that directly strengthens your organization's financial footing. These systems forge a clear, powerful link between top-tier patient care and a much healthier bottom line. It's time to stop seeing them as a cost center and start recognizing them as a critical engine for efficiency and growth.
The value really breaks down into two main buckets: measurable wins on the clinical side and significant returns on the operational side. By improving patient outcomes while streamlining how your teams work, a PDSS is the key to unlocking the kind of value-based care that defines modern healthcare.
Enhancing Clinical Outcomes
From a clinical perspective, the benefits are immediate and profound. Think of a PDSS as an intelligent safety net, catching potential problems long before they turn into emergencies. This proactive approach dramatically cuts down on preventable medical errors—a huge source of patient harm and a massive financial drain.
For example, an AI-powered system can instantly spot a dangerous drug interaction by checking a patient's full medication list against their latest lab results and even genetic markers. A single, timely alert can prevent a life-threatening reaction, saving not only a life but also the tens of thousands of dollars tied to emergency interventions and prolonged hospital stays.
These systems also foster consistency. By embedding evidence-based treatment protocols directly into the workflow, they ensure every patient receives standardized, high-quality care. That consistency is the bedrock of patient safety and satisfaction.
Driving Financial ROI
All those clinical improvements translate directly into real, tangible financial gains. Every medical error avoided, every treatment plan optimized, and every day shaved off a hospital stay has a clear dollar value.
The global market for these systems is exploding, projected to jump from roughly $3 billion in 2026 to over $15.32 billion by 2033. This surge is fueled by hospitals determined to slash diagnostic errors by up to 35% with AI-driven, evidence-based tools. You can dig deeper into these market trends and their impact on healthcare.
Some of the most common financial benefits include:
- Reduced Readmission Rates: When patients get the right, guideline-based care the first time, their chances of a costly and penalized readmission plummet.
- Shorter Lengths of Stay: Quicker, more accurate diagnoses and fine-tuned treatment paths mean patients can go home sooner. This frees up beds and lets you serve more people.
- Smarter Resource Use: The system helps clinicians avoid redundant or low-value tests, saving a significant amount of money on labs, imaging, and other diagnostic procedures.
This is where integrating something like AI Automation as a Service can really multiply the financial benefits. By automating how critical data is analyzed and presented, these services make sure the insights from your PDSS land in front of the right people at the right time, maximizing their impact on your operational costs.
A Smart Investment in Value-Based Care
At the end of the day, a PDSS is what aligns great clinical work with long-term financial stability. It empowers healthcare organizations to confidently embrace value-based care models, where you get paid for delivering excellent outcomes, not just for the volume of services you provide.
Investing in a PDSS is an investment in a safer, more efficient, and financially resilient future. It gives your clinical teams the tools they need to do their best work while simultaneously shoring up the organization's operational health. By connecting the quality of care directly to cost savings, these systems prove that what’s best for the patient is also what's best for business. Keeping an eye on these returns is simple with tools that give you a clear view, much like our Financial Insights Dashboard.
Your Practical PDSS Implementation Roadmap
Getting a physician decision support system up and running is a journey, not a simple plug-and-play installation. It demands a clear-eyed plan that marries the technical side of things with the very human, day-to-day realities of clinical practice. A good roadmap ensures the tech doesn't just work on paper but is actually embraced by the clinicians it’s meant to help.
This journey starts long before you ever see a vendor demo. It begins with a deep, honest look at your own clinical and operational world. The goal is to find the exact pain points where a PDSS can do the most good. Nailing this first step is absolutely critical for building a solid business case and getting everyone on board.
Phase 1: The Strategic Blueprint
Before a single dollar is spent or a contract is signed, you have to define what a "win" looks like for your organization. This first phase is all about strategy and making sure everyone is pulling in the same direction. It involves zeroing in on specific clinical areas—like slashing medication errors in the ICU or getting better at spotting sepsis in the emergency department—where a decision support tool can make a real impact.
This is where a detailed AI requirements analysis comes into play. You have to set clear, measurable goals. Forget vague objectives like "improve patient care." Instead, aim for concrete targets, such as "reduce adverse drug events by 15% within 12 months." A specific target gives the project a clear direction and a benchmark for actually measuring your return on investment. Crafting this initial strategy is a core part of what we do through a Custom AI Strategy report, which helps organizations connect their needs to real, tangible outcomes.
Phase 2: The Technical Foundation
Once your strategy is locked in, the focus shifts to the nuts and bolts. The single most important piece of the puzzle here is making sure the PDSS integrates seamlessly with your existing Electronic Health Record (EHR) system. If it feels like a clunky add-on or forces clinicians to juggle multiple windows, you can bet adoption rates will tank.
Data is the fuel for any PDSS, so quality and security are just as important. The system needs a steady diet of clean, standardized, and complete patient data to do its job well. You'll also have a big decision to make on the deployment model:
- On-Premise: Gives you more direct control over your data but comes with a hefty upfront investment in hardware and the IT team to manage it.
- Cloud-Based: Offers much more flexibility and lower initial costs, but it means you have to be extremely thorough in vetting your vendor’s security practices.
This is also the phase where you figure out the specific tools you'll need, which could be anything from a sophisticated analytics platform to custom internal tooling built to fit your unique clinical workflows.
This graphic shows how the technical groundwork you lay directly connects to clinical improvements and, eventually, a solid financial return.
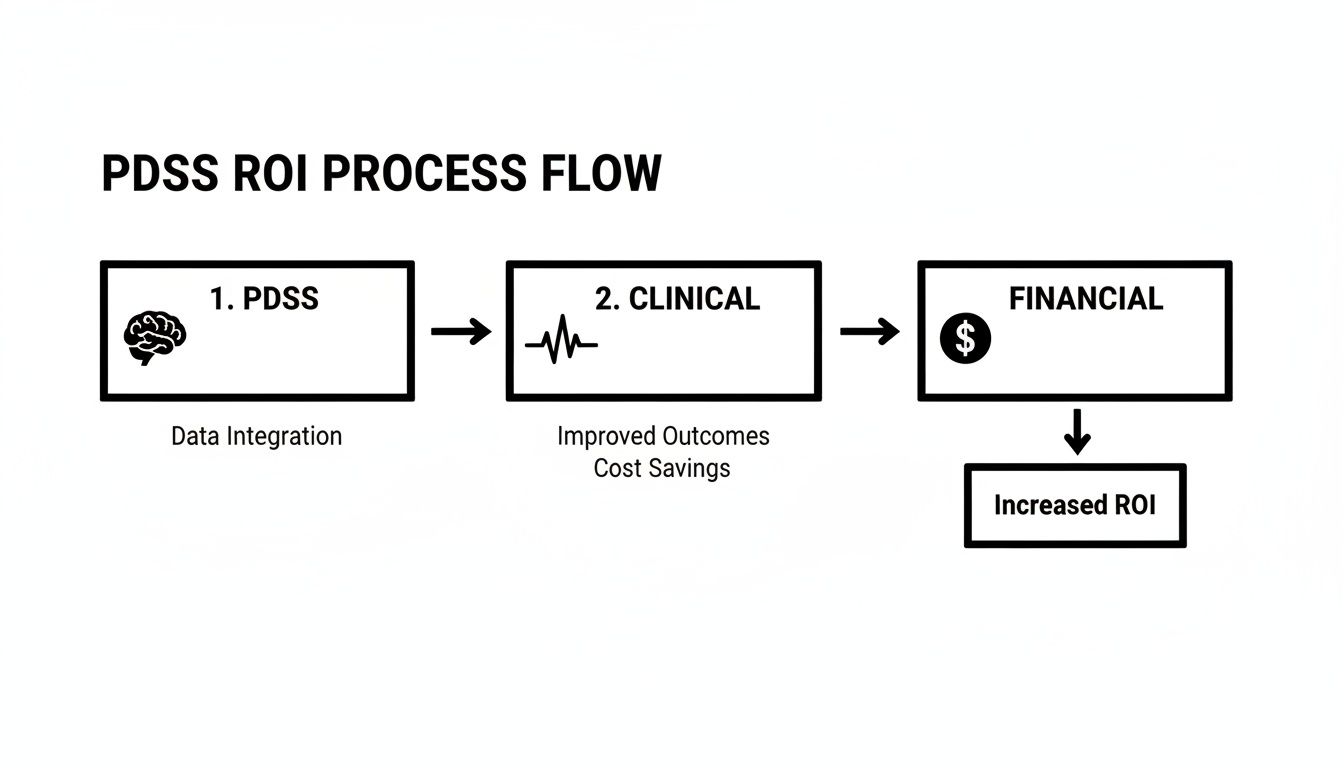
As you can see, a well-integrated system uses clinical data to drive better health outcomes, which in turn brings down costs and boosts the bottom line.
Phase 3: The Human Element
Let's be clear: the technology is only half the battle. The number one reason physician decision support systems fail is a lack of adoption by the people they're designed for. This is why managing the change process isn't just some item to check off a list—it's a central part of the entire plan. Getting physicians to buy in isn't optional; it's everything.
The key is to position the PDSS as a supportive co-pilot that enhances clinical judgment, not a backseat driver that dictates it. Involve clinicians from the very beginning—in the selection, the design, all of it—to make sure the system solves their real-world problems.
Minimizing disruption to their workflow is just as important. The system should feel like a natural extension of how they already work. This means configuring alerts to be genuinely helpful and actionable, which is the only way to avoid "alert fatigue"—that point where clinicians start tuning out notifications because they’re either too frequent or irrelevant. A smart, ongoing approach to training and gathering feedback is what separates a successful implementation from a forgotten one.
For organizations looking for an experienced guide, our battle-tested AI Product Development Workflow offers a structured way to navigate these tricky human and technical challenges.
Choosing The Right Partner And Staying Compliant
Bringing a physician decision support system into your clinical environment is about much more than just plugging in new software. The real work—and where many initiatives stumble—lies in navigating regulatory hurdles and picking the right long-term partner. Get these two things right, and you’re building a system that’s not only effective but also secure, trusted, and sustainable.
Healthcare operates under a microscope of regulations designed to protect patient information. Any PDSS you adopt must be airtight when it comes to rules like the Health Insurance Portability and Accountability Act (HIPAA) in the U.S. and the General Data Protection Regulation (GDPR) in Europe. The consequences of non-compliance aren’t just steep financial penalties; they’re a breach of patient trust that can be incredibly difficult to repair.
Navigating The Regulatory Maze
Think of compliance as the foundation of the entire project. When you're handling the most sensitive data imaginable, security and privacy aren't just features—they're absolute necessities. This is why a vendor's commitment to data governance should be at the top of your evaluation list.
But today, compliance goes beyond HIPAA and GDPR. With machine learning driving many of these systems, a new standard has emerged: explainable AI (XAI). It’s simply not enough for an algorithm to spit out a recommendation. Clinicians, quite rightly, won't trust a "black box" that can’t show its work.
An explainable system peels back the curtain, revealing the "why" behind its suggestions. This transparency is crucial for building clinical trust, as it allows physicians to validate the logic and act on insights with confidence.
This isn't just about trust, either. Explainability is quickly becoming a core component of meeting the legal and ethical standards for AI in medicine.
Your Vendor Vetting Checklist
Choosing a technology partner is a marriage, not a first date. You need a collaborator who gets the clinical world inside and out, not just a company pushing a product. A thorough vetting process is your best defense against a bad fit. When you're assessing potential PDSS partners, you have to dig deep into their approach to data privacy and regulatory adherence. A solid guide can help with secure vendor onboarding and compliance with regulations like GDPR and CCPA.
Here are the key questions to build your evaluation around:
- Proven Clinical Validation: Ask for the proof. Can the vendor show you hard evidence—case studies, peer-reviewed research—that their system actually improves outcomes in a real-world setting?
- Seamless Interoperability: How cleanly will it play with your existing tech stack? The system absolutely must integrate with your EHR and other tools using modern standards like FHIR (Fast Healthcare Interoperability Resources). Anything less creates frustrating workflow friction for your team.
- Robust Data Security and Compliance: This is non-negotiable. The vendor must be able to demonstrate an ironclad commitment to data security, with clear protocols for protecting patient information and meeting every single regulatory requirement.
- Dedicated Support and Training: What happens after you sign the contract? A real partner will have a comprehensive plan for implementation, training, and ongoing support to ensure your clinicians get the most out of the system.
- A Clear Future Roadmap: Where is this technology going? A forward-thinking vendor has a clear vision and can speak to how they plan to incorporate new advancements and adapt to the ever-changing needs of healthcare.
For organizations whose needs are too specific for an off-the-shelf solution, a custom-built system can be a game-changer. For this you can seek a reliable custom healthcare software development partner. This path lets you create a tool that is perfectly molded to your clinical workflows and strategic goals.
Deciding whether to buy or build is a major decision. Our experts can help you make that call, and our AI Product Development Workflow provides a structured framework to guide you through the entire process, from initial idea to final rollout.
So, you've made the strategic decision to invest in a physician decision support system. That's a huge step. But how do you actually prove it's working?
To justify the investment and make a solid case for future projects, you need a straightforward, data-backed way to measure its impact on the ground. Success isn't just about having the latest tech; it's about seeing real, measurable improvements in patient care, the daily workflow, and the hospital's bottom line.
The trick is to track a balanced mix of key performance indicators (KPIs) that paint the complete picture. You’ll want to define these metrics before you go live. This gives you a clear baseline to measure against, providing the hard evidence needed to show value to everyone from the C-suite to the clinicians on the floor.
How to Define Your Core Metrics
The best way to see if your physician decision support system is delivering is to group your KPIs into three core areas: clinical, operational, and financial. Each one gives you a different, but equally important, perspective on the system's value.
Clinical KPIs: These get right to the heart of the matter—patient outcomes. They are the ultimate proof that the system is improving the quality of care. You'll want to watch for things like reduced patient mortality rates, fewer adverse drug events, and better adherence to evidence-based clinical guidelines.
Operational KPIs: This is all about workflow and efficiency. A win here means your teams can work smarter, not just harder. Keep an eye on metrics like a reduced average length of hospital stay, less time physicians spend charting, and more appropriate use of diagnostic tests.
Financial KPIs: This is where you connect the dots between better care and a healthier budget. Look for direct cost savings from avoiding unnecessary tests, lower costs associated with treating medical errors, and reduced penalties for things like hospital readmissions.
By tracking these interconnected metrics, you build a powerful story. For example, you can show how better adherence to a sepsis protocol (a clinical KPI) led to shorter ICU stays (an operational KPI), which directly resulted in major cost savings (a financial KPI).
Success in Action: A Sepsis Alert Case Study
To see just how powerful these systems can be, let's look at one of the most common real-world use cases: an AI-powered sepsis alert. One hospital integrated a PDSS that constantly scanned patient EHR data—vitals, lab results, clinical notes—looking for the earliest, most subtle signs of sepsis.
Before this system was in place, clinicians often couldn't confirm sepsis until a patient was already showing obvious, late-stage symptoms, making treatment much more difficult. The new PDSS flagged high-risk patients hours earlier, giving care teams a critical head start on antibiotics and fluids.
The results were stunning. Within the first year, the hospital saw a 20% reduction in sepsis-related mortality. Operationally, the average hospital stay for septic patients fell by two full days. Financially, this added up to millions of dollars in cost savings each year. This is a perfect example of how a well-designed PDSS delivers a clear, measurable return across the board. Our expert team helps organizations define and monitor these critical metrics to ensure a clear return on investment.
Frequently Asked Questions
What’s the real difference between a PDSS and an EHR?
Think of it this way: the Electronic Health Record (EHR) is the patient’s detailed digital file. It’s a comprehensive library holding everything from lab results and imaging scans to physician notes and medication history. It’s essential, but it's fundamentally a storage system. A PDSS, on the other hand, is the expert consultant that reads everything in that file and offers real-time advice. While the EHR passively holds the data, the PDSS actively analyzes it to flag potential drug interactions, suggest a differential diagnosis, or recommend a treatment protocol based on the latest clinical guidelines. The EHR tells you what happened; the PDSS helps you figure out what to do next.
How do we get our doctors to actually use it?
Adoption is everything. If a PDSS feels like another clunky system bolted onto the side of the EHR, physicians will ignore it. The secret is making it an invisible, indispensable part of their daily routine. First and foremost, the system has to integrate seamlessly into their existing workflow. Second, bring clinicians into the conversation from the very beginning. When they help choose and configure the system to solve problems they face every day, they become champions for it. And finally, you have to tackle alert fatigue head-on by customizing notifications so that only the truly important ones get through. As we explored in our AI adoption guide, a user-first design is critical. This philosophy is central to our Healthcare AI Services.
What’s the right way to get started with a PDSS?
Hold off on the vendor demos. The most critical first step is to pinpoint a specific, high-stakes problem you want to solve. Sit down with your clinical teams and identify the top 2-3 challenges where better, faster decisions could make a huge difference. This initial AI requirements analysis is where the real work happens. It shifts the project from "Which new tool should we buy?" to "What's the most important problem we can solve?" This focus ties your investment directly to a clear, measurable goal from the start. A Custom AI Strategy report can provide this foundational roadmap, making sure your project aligns with your organization's most important goals.
Ready to unlock the full potential of AI in your healthcare organization? Ekipa AI provides the strategic clarity and technical expertise needed to turn your vision into reality. From initial strategy to seamless implementation, our expert team helps you build physician decision support systems that deliver real clinical and financial value.
Discover how our AI strategy consulting can accelerate your transformation.