Clinical Decision Intelligence: Transforming Healthcare with AI-Driven Insights
Learn how clinical decision intelligence uses AI to boost patient outcomes, ROI, and practical implementation.
Imagine a healthcare system that can see a patient's health crisis coming, long before it actually arrives. That’s the core promise of Clinical Decision Intelligence (CDI). It’s a huge leap beyond the basic alerts doctors are used to, blending massive amounts of patient data with smart AI and the invaluable wisdom of clinical experts—all to support better decisions right at the point of care.
The Dawn of a Proactive Healthcare Era
Today's healthcare system is under enormous strain. We're facing a rising tide of chronic diseases, clinician burnout, and the sobering reality that diagnostic errors contribute to tens of thousands of deaths every year. The old, reactive way of doing things just isn't cutting it anymore.
This is where Clinical Decision Intelligence steps in, not as some far-off concept, but as a real, practical solution for today. It’s all about making a fundamental shift—moving from a system that just reacts to sickness to one that proactively keeps people well.
This guide isn't about buzzwords. It’s about digging into the "why" behind CDI. Think of it as the answer to ballooning operational costs, overwhelmed doctors, and the growing expectation for medicine that’s truly personal. By weaving intelligence into every clinical decision, healthcare organizations can start tackling these deep-rooted problems head-on.
Beyond Basic Alerts
Clinicians have had Clinical Decision Support Systems (CDSS) for years. These are the rule-based tools that, for instance, flag a potential drug interaction. They're helpful, but limited.
Clinical Decision Intelligence is the next generation. It doesn't just flag problems; it predicts them.
Clinical Decision Intelligence turns data into foresight. It helps clinicians see around the corner, giving them the chance to step in before a patient's health takes a turn for the worse. It's the difference between a smoke alarm and a system that prevents the fire from ever starting.
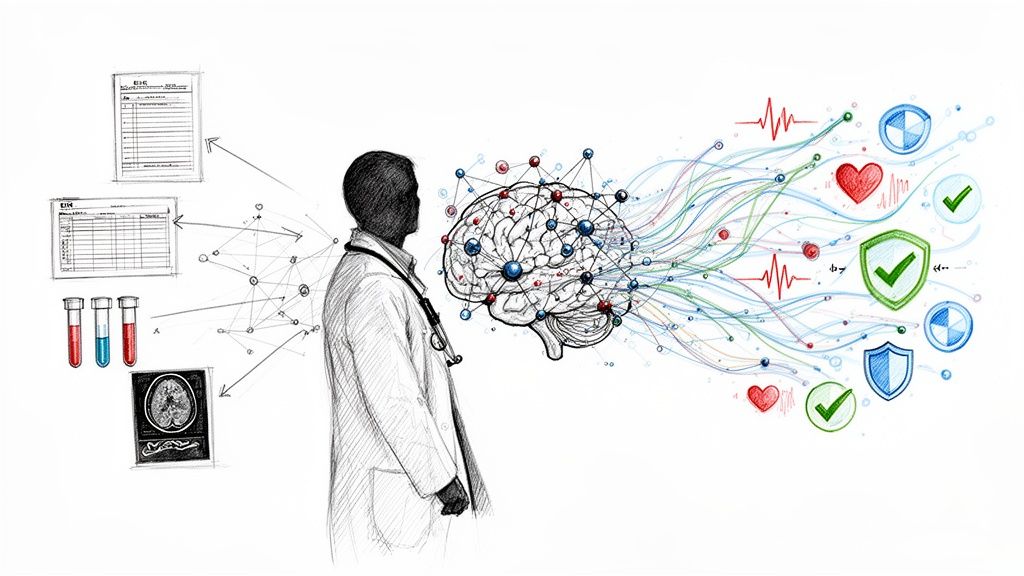
This more advanced approach uses sophisticated AI models to sift through incredibly complex data—everything from electronic health records (EHRs) and lab results to genomic data and real-time patient monitoring. The whole point is to deliver subtle, context-aware insights directly into a doctor's natural workflow. To really understand how big of a deal this is, it's worth exploring how AI clinical decision support is making healthcare smarter.
This predictive power is the engine behind modern Healthcare AI Services, which are designed to build these intelligent systems. The goal is to transform overwhelming floods of data into simple, actionable advice that directly improves patient outcomes and makes hospitals run more smoothly.
In the end, CDI helps build a healthcare system that's more resilient, efficient, and truly focused on the patient. We're finally moving toward a reality where technology isn't just a tool, but a true partner in delivering care.
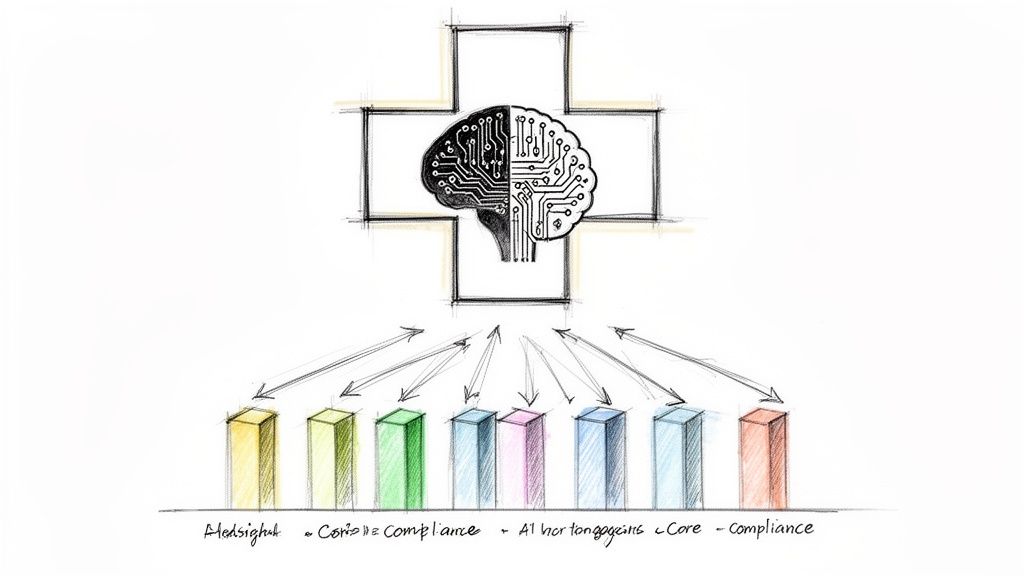
A Look Inside a Modern Clinical Decision Intelligence Ecosystem
Think of a modern clinical decision intelligence ecosystem as the central nervous system of a hospital. It’s designed to connect all the disparate pieces of information, process them with powerful analytics, and deliver critical insights to clinicians right when they need them most. This complex architecture really comes down to four key pillars working in concert.
This diagram shows how it all fits together—not as a straight line, but as a continuous loop where raw data is refined into expert-level clinical actions.
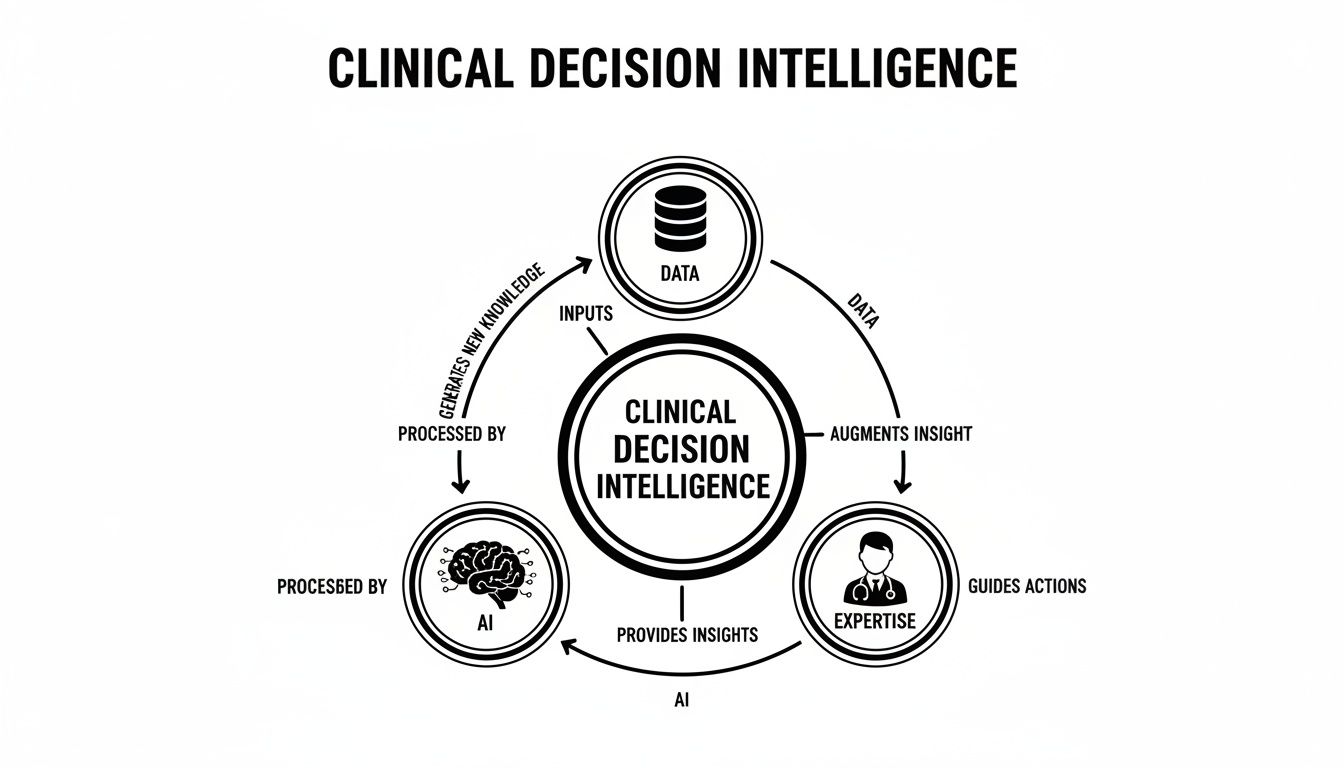
What this really highlights is that CDI isn't just a one-and-done tool. It's a living system of learning and improvement, where data, AI, and human expertise are constantly feeding and refining one another.
Data Integration and Interoperability
The entire system is built on its ability to pull in and make sense of data from dozens of different sources. As anyone in healthcare knows, patient information is often scattered everywhere—stuck in electronic health records (EHRs), lab systems, imaging archives (PACS), and even data from wearable devices.
True interoperability is about smashing those silos. It means using modern standards like FHIR (Fast Healthcare Interoperability Resources) to create a single, unified view of a patient's journey. Without this complete picture, even the most sophisticated AI models are essentially flying blind. A solid CDI system needs a well-thought-out foundation, and exploring concepts in Business Intelligence Architecture can shed light on how to build these data frameworks to scale.
AI and Machine Learning Models
Once all that data is brought together, the AI and machine learning models get to work. These algorithms are the analytical brains of the operation, trained to spot subtle patterns that are often completely invisible to the human eye. This is where predictive and prescriptive analytics really shine.
For example, these models can:
Predict Risk: Flag patients who are at a high risk for developing sepsis or being readmitted to the hospital.
Augment Diagnosis: Analyze medical images to help radiologists spot the earliest signs of disease.
Personalize Treatment: Suggest therapies tailored to a patient's specific genetic makeup and clinical history.
Tools like our own Clinic AI Assistant are built on these exact principles, using advanced models to give clinicians an analytical edge.
Clinical Workflow Integration
Here’s the reality: technology is only useful if people actually use it. For CDI to make a real impact, it has to fit seamlessly into the way clinicians already work. They’re already buried under alerts and administrative tasks, so the last thing they need is another clunky tool to learn.
The goal of CDI isn’t to add another screen or another login. It's about embedding intelligence directly into the EHR, offering context-aware suggestions that feel like a natural extension of a doctor's own thought process.
This smooth integration is absolutely critical for adoption. The market data backs this up, with integrated platforms expected to capture 58.23% of revenue in 2025. Even stand-alone modules are seeing huge growth (a projected 15.7% CAGR through 2031), but only when they’re designed to be embedded within the EHR. With medical knowledge now doubling every 73 days, the move toward these adaptive, machine learning-based systems—which already command a 61.55% market share—is only getting faster.
Governance and Explainability
Finally, none of this works without trust. A CDI system has to operate under a strict governance framework that guarantees patient privacy, keeps data secure, and complies with regulations like HIPAA.
But it goes beyond just checking boxes. Explainability is a non-negotiable part of the equation. Clinicians have to understand why an AI model is recommending a certain course of action. This "explainable AI" (XAI) is essential for building confidence, allowing doctors to sanity-check the AI's logic, and making sure the final decision always stays in human hands. Without that transparency and a strong ethical backbone, even the most accurate AI will never earn the trust it needs to truly change patient care.
Calculating the ROI of Clinical Decision Intelligence
For any healthcare leader, bringing in new technology like clinical decision intelligence isn't just a tech upgrade. It's a fundamental business decision. The real goal is to build a more resilient, efficient, and financially sound organization. Beyond the obvious clinical wins, the return on investment (ROI) from CDI is concrete, measurable, and frankly, too compelling to ignore. It’s about turning sophisticated data analytics into a healthier bottom line.
The business case for CDI really stands on three pillars: making operations smoother, strengthening financial performance, and elevating patient outcomes. When you get these three things working in harmony, you create a powerful cycle where each success feeds the next. This isn't just an abstract concept; it's a practical blueprint for sustainable growth.
The market's explosive growth tells the story. The global market for clinical decision support systems (CDSS), which is a core part of CDI, was pegged at USD 3.65 billion in 2024 and is expected to soar to USD 8.10 billion by 2034. That 8.30% compound annual growth rate isn't happening by accident. It's fueled by the clear financial and operational wins these systems deliver. With cloud-based solutions now dominating 65% of the market, this tech is more accessible than ever. Integrating these systems into a wider AI strategy can yield staggering results, like cutting diagnostic errors by up to 50% in some studies. You can dig into the numbers in this clinical decision support systems market report.
Driving Operational Efficiency
Think of CDI as an efficiency engine. Its primary job is to attack the bottlenecks, administrative headaches, and manual processes that clog up care delivery and drive up costs. By automating routine analysis and embedding predictive insights right into the existing workflow, CDI frees up clinicians from tedious, time-draining tasks.
What does that look like in practice? Imagine a system that automatically flags a patient as high-risk the moment they're admitted. Right away, the care team can channel resources proactively instead of scrambling to react to a crisis later. This simple step can optimize everything from bed management to diagnostic testing, all while giving clinicians more time for what they do best: caring for patients. This is exactly what our "AI Automation as a Service" is designed to do—turn smart insights into automated actions that remove operational friction.
Boosting Financial Performance
The financial upside of clinical decision intelligence is both direct and substantial. By making clinical decisions more accurate and timely, these systems go after some of the biggest and most stubborn cost centers in healthcare.
Just look at the financial wins you can unlock:
Fewer Readmissions: CDI can pinpoint which patients are most likely to be readmitted and suggest specific interventions before they even go home, helping you avoid steep penalties.
Reduced Medical Errors: Adverse drug events and misdiagnoses come with enormous financial and human costs. AI-powered alerts and diagnostic aids can stop many of these events from ever happening.
Better Billing Accuracy: By helping clinicians ensure documentation is complete and correct at the point of care, CDI strengthens the entire revenue cycle and drastically cuts down on denied claims.
Building a rock-solid business case starts with quantifying this potential ROI. Our AI strategy consulting services are built to help organizations map out these financial gains from day one.
Mapping CDI Implementation to Tangible ROI
It's one thing to talk about benefits, but it's another to see the direct line between an investment and its financial return. This table breaks down how specific CDI features translate into measurable business outcomes.
| CDI Investment Area | Operational Impact | Financial ROI |
|---|---|---|
| Predictive Readmission Models | Proactive discharge planning and targeted follow-ups for high-risk patients. | Lower readmission penalties, reduced cost-per-patient episode. |
| Real-Time Clinical Alerts | Prevents adverse drug events and flags potential diagnostic errors instantly. | Reduced costs from medical errors, lower malpractice insurance premiums. |
| AI-Powered Documentation Assistance | Ensures accurate and complete clinical notes at the point of care. | Fewer claim denials, accelerated revenue cycle, optimized reimbursements. |
| Workflow Automation Tools | Automates routine administrative tasks like data entry and patient scheduling. | Increased clinician capacity, reduced staff burnout, lower overhead costs. |
As you can see, each investment is designed not just to improve care, but to create a clear and defensible financial return.
Linking Better Outcomes to Business Value
At the end of the day, improving patient outcomes isn't just a clinical mission—it's a powerful driver of long-term business value. We're living in an era of value-based care, where payments are increasingly tied to results. Better outcomes now lead directly to better financial performance.
CDI forges a direct link between high-quality care and financial sustainability. When patients recover faster and have fewer complications, the hospital’s reputation grows, patient loyalty increases, and the organization thrives under new payment models.
This reputational lift is priceless. A hospital known for excellence becomes a magnet for top medical talent and a pillar of trust in the community. This perfect alignment between patient well-being and organizational health is the ultimate ROI of clinical decision intelligence. The journey starts with a clear vision, and a Custom AI Strategy report can provide the roadmap to get you there.
Clinical Decision Intelligence in Action
This is where the rubber meets the road. Abstract ideas like "predictive models" and "workflow integration" are interesting, but their real value becomes clear when you see them saving lives and solving real-world medical problems. The true power of CDI isn't in the theory; it's in the practical applications that are already changing how we approach diagnostics, treatment, and medical research.
These aren't hypothetical, futuristic scenarios. They are happening right now. Let’s look at a few specific real-world use cases to see how weaving deep data analysis into the fabric of clinical practice leads to better outcomes.
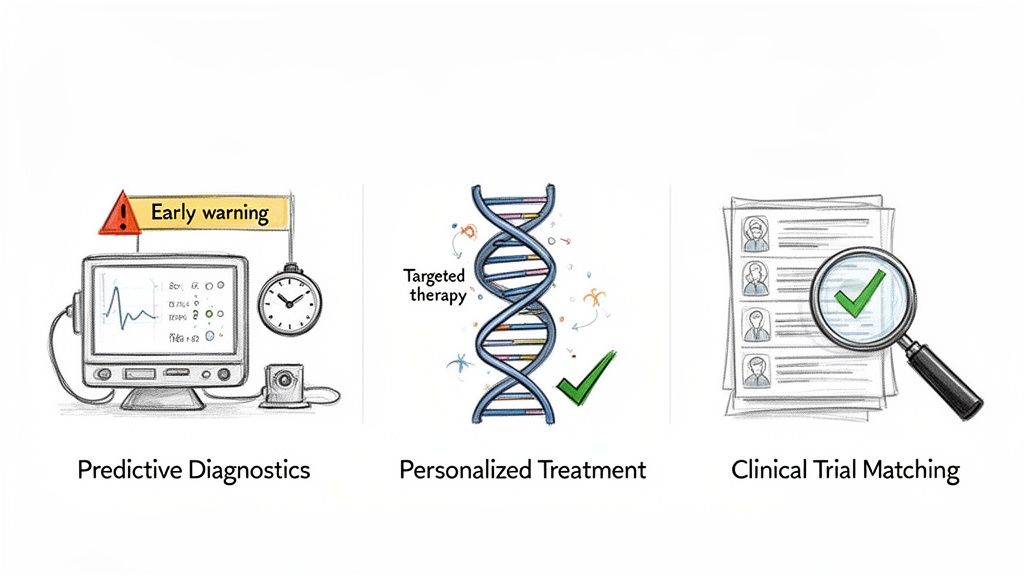
Predictive Diagnostics: Catching Sepsis Early
Sepsis is a medical emergency that can escalate with terrifying speed, making early detection the absolute key to survival. The problem is that its early symptoms—fever, a high heart rate, confusion—are incredibly common and easily mistaken for less serious issues, especially in a chaotic hospital setting. By the time the signs become unmistakable, the window for the most effective treatment may have already closed.
This is exactly the kind of challenge that clinical decision intelligence was built to solve. A CDI system can act as a tireless digital watchman, continuously monitoring dozens of data streams from a patient’s Electronic Health Record (EHR). It sifts through real-time vital signs, lab results, and even unstructured nursing notes, looking for the subtle, combined patterns that are the faint, early whispers of sepsis—often hours before a human clinician could possibly spot them.
When the algorithm flags a high risk of sepsis, it doesn’t just sound a generic alarm. It sends a specific, targeted alert directly to the right care team. This is a data-backed heads-up that cuts through the noise, prompting immediate action, leading to faster treatment and dramatically improved patient survival rates.
Personalized Treatment Planning in Oncology
Treating cancer is never a one-size-fits-all proposition. Today, the most effective therapies are often precisely matched to a patient's unique genetic code. But figuring out that perfect match requires an oncologist to analyze staggering amounts of genomic data and cross-reference it with the latest research and clinical trial results—a nearly impossible task for any single person.
This is where CDI platforms shine. They can ingest a patient's entire genomic profile and, in minutes, compare it against massive databases of clinical trial data, established treatment guidelines, and emerging research. The system can pinpoint specific genetic mutations and recommend the targeted therapies or immunotherapies that have the highest probability of success for that specific individual. This slashes the time it takes to get a patient on the right treatment, helping them avoid a painful trial-and-error process where every day counts.
Our own diagnostic tool, Diagnoo, is built on this very principle—using advanced AI to pull clear, precise insights from incredibly complex medical data.
Accelerating Clinical Trial Matching
Clinical trials are the engine of medical progress, but one of their biggest bottlenecks is simply finding the right patients. The traditional process of manually screening thousands of patient records against a long list of complex trial criteria is incredibly slow, expensive, and riddled with potential for human error. This bottleneck means that many patients who could benefit from an experimental treatment never even hear about it, and promising new therapies are delayed.
CDI completely streamlines this process. AI-powered algorithms can scan an entire health system's patient database almost instantly, matching individuals to relevant clinical trials based on their specific diagnosis, medical history, lab values, and even genetic markers.
The benefits here are twofold:
For Patients: It opens the door to potentially life-saving treatments they might never have found otherwise.
For Researchers: It drastically shortens patient recruitment timelines, which can shave months or even years off the development cycle for new drugs and therapies.
These examples show that clinical decision intelligence is much more than just a background support tool. It’s an active, intelligent partner in patient care. By transforming raw data into clear, actionable insights right at the point of care, it empowers clinicians to make faster, more confident, and more precise decisions that directly improve and save lives.
Your Roadmap to Implementing Clinical Decision Intelligence
Getting started with clinical decision intelligence isn't about flipping a switch overnight. It’s a deliberate journey, one that requires a clear, methodical roadmap to ensure each step builds on the last. For healthcare leaders, this means moving from initial curiosity to a full-scale, impactful system with purpose and precision.
The process begins with a simple question: what’s the right problem to solve? From there, you prepare your data foundation, choose the right technology, and finally, prove the concept before expanding it across the organization. This structured approach is the key to managing complexity and delivering real value at every stage.
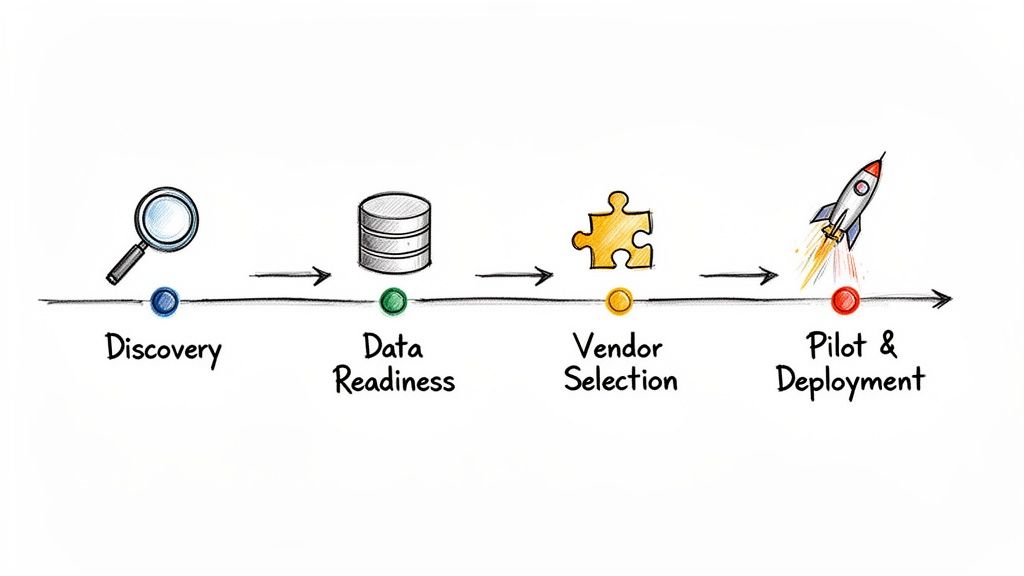
Stage 1: Discovery and Use Case Identification
The first phase—discovery—is arguably the most critical. Instead of trying to boil the ocean, the goal is to pinpoint a single, high-impact use case that has a clear path to success. The best projects to start with are those that tackle a significant clinical or operational pain point where the potential ROI is easy to define.
Ask yourself questions like:
Where are our biggest bottlenecks in patient care?
Which condition contributes most to our readmissions or highest costs?
Is there a specific diagnostic challenge where our clinicians desperately need more support?
Choosing the right starting point, as we explored in our AI adoption guide, builds crucial momentum. A well-defined AI requirements analysis will bring clarity to the scope, success metrics, and technical needs, setting you up for a successful pilot that wins over key stakeholders.
Stage 2: Data Readiness Assessment
With a use case in hand, the focus shifts to the fuel that powers all AI: data. Any clinical decision intelligence tool is only as reliable as the information it’s built on. This stage involves a thorough assessment to make sure your data is clean, accessible, standardized, and ready for complex analysis.
Key activities here include:
Data Auditing: Identifying and cataloging all relevant data sources, from the EHR to lab systems and beyond.
Quality Control: Putting processes in place to clean the data, handle missing values, and correct inconsistencies.
Interoperability: Making sure data can flow seamlessly between different systems using standards like FHIR.
This foundational work is completely non-negotiable. Without a solid data pipeline, even the most sophisticated algorithms will fail to produce accurate or trustworthy insights. Investing time here prevents massive headaches down the road.
Stage 3: Technology and Vendor Selection
Next up is the classic build-versus-buy decision. Developing a CDI platform from the ground up requires a huge investment in specialized talent and custom healthcare software development. On the other hand, partnering with an experienced vendor can fast-track the process and give you access to proven technology.
When you’re evaluating partners, look for deep expertise in both AI and healthcare. The right partner will inherently understand the unique regulatory and workflow challenges of a clinical environment. This is where tailored AI solutions and a comprehensive AI Product Development Workflow become invaluable, guiding you through the tricky parts of integration and deployment. Whether you need simple internal tooling or a full-scale platform, the right choice must align with your organization's long-term vision.
Stage 4: Pilot Program and Scalable Deployment
The final stage is where your strategy becomes a reality. A pilot program lets you test the CDI solution in a controlled, real-world setting. This is your chance to gather honest feedback from clinicians, measure performance against your KPIs, and fine-tune the system before a big rollout.
A successful pilot is your proof point. It demonstrates tangible value, builds trust among clinical staff, and creates the strong business case needed to secure resources for wider deployment.
Once the pilot proves itself, the focus shifts to scalability. This involves mapping out a plan to introduce the CDI solution to other departments or facilities, ensuring the technical architecture can handle the increased demand while maintaining performance. The journey from a single use case to an enterprise-wide capability is guided by a clear Custom AI Strategy report, which outlines the steps for sustainable growth. By following this roadmap, your organization can turn CDI from a promising concept into a core part of modern patient care.
Finding the Right Partner for Your CDI Journey
Bringing clinical decision intelligence into your organization isn't just another IT project. It’s a fundamental change in how your teams work, and that kind of shift requires a true strategic partner, not just a vendor.
You’re wading into a complex world of clinical workflows, tangled data architectures, sophisticated AI models, and a web of regulatory rules. The path from a good idea on a whiteboard to a scalable, impactful CDI system is rarely a straight line.
Common roadblocks pop up everywhere. You might struggle to pinpoint the best starting use case, wrestle with integrating new tech into legacy EHRs, or face pressure to prove tangible ROI from day one. This is exactly where a collaborative partner makes all the difference—someone who can cut through the noise of traditional, slow-moving consulting and give you a clear, fast track to real results.
Your Partner in Transformation
At Ekipa AI, we’ve built our entire approach around solving these very problems. We believe in getting to the heart of the matter quickly, starting with a tailored Custom AI Strategy report that provides a clear roadmap right from the beginning. Our goal is to empower your team, not create a long-term dependency.
We offer a full spectrum of support for your CDI journey:
Rapid Strategy: Our AI strategy consulting helps you quickly zero in on the highest-value CDI opportunities within your specific clinical environment.
Efficient Execution: We provide specialized Healthcare AI Services and hands-on guidance using our proven AI Product Development Workflow.
Scalable Solutions: Whether it's through AI Automation as a Service or building powerful AI tools for business, we make sure your CDI capabilities can grow and adapt as your needs evolve.
We don't just build technology. We build the strategic foundation that turns your CDI vision into a sustainable, high-impact reality. We help you connect the dots between powerful AI solutions and measurable improvements in patient outcomes and operational efficiency.
The journey to transform patient care with clinical decision intelligence is a team sport. We invite you to connect with our expert team—the specialists who can guide your organization from the first strategic conversation all the way through implementation and beyond.
FAQ: Clinical Decision Intelligence
Here are answers to some of the most common questions we hear from healthcare leaders and innovators about putting clinical decision intelligence into practice.
How is CDI different from the CDSS we already have?
Think of your traditional Clinical Decision Support System (CDSS) as a set of guardrails. It's built on rules. It'll throw up an alert if you prescribe a drug that interacts with another, which is incredibly useful, but it's fundamentally reactive.
Clinical Decision Intelligence (CDI) is more like having an entire air traffic control system. It's proactive. It sifts through massive, messy datasets in real-time to spot patterns, predict which patients are at risk, and suggest personalized next steps. A CDSS is a feature; CDI is the whole intelligent strategy that weaves this kind of predictive power into everything a clinician does.
How do we keep AI models from being biased or unfair?
Building fair AI isn't just a technical challenge; it's a moral imperative. You can't just hope for fairness; you have to design for it from the ground up. This is a non-negotiable part of building trust with both clinicians and patients.
A solid approach requires a few key commitments:
Start with Representative Data: The model is only as good as the data it learns from. You have to ensure your training data reflects the true diversity of the patient population you serve, not just a slice of it.
Conduct Bias Audits: We use specific algorithms designed to detect and correct for bias, then regularly audit the model's performance across different patient groups to make sure it's working equitably for everyone.
Keep a Human in Control: This is critical. Clinicians must always have the final say. An AI recommendation is just that—a recommendation. The system must be designed so a human expert can easily review, question, and ultimately override the AI’s suggestion.
This kind of ethical governance is the foundation of any CDI strategy we help build, and it's a central pillar of our AI strategy consulting.
We're interested, but where do we even begin?
The best way to get started is to think small to win big. Don't try to boil the ocean. Instead, kick things off with a focused discovery phase to pinpoint a single, high-impact clinical problem where you can draw a straight line to a successful outcome.
Maybe it's a project to bring down sepsis mortality rates by 15% or one aimed at improving diagnostic accuracy for a specific type of cancer. A targeted AI requirements analysis helps you nail down what success looks like and build a rock-solid business case. This approach gets you a measurable win early on, which builds the confidence and momentum you need to scale CDI across the organization.
How does this actually work with our existing EHR?
If it doesn't fit into a clinician's daily routine, it won't get used. It's that simple. Modern CDI platforms are built to work with the Electronic Health Record (EHR) systems your teams rely on, not force them to jump to yet another screen.
The magic happens through modern APIs and interoperability standards like HL7 FHIR. These act as universal translators, allowing CDI tools to securely connect to major EHRs from vendors like Epic and Oracle Cerner. The result? AI-powered insights and recommendations appear right inside the patient chart, exactly where and when the doctor needs them. It feels less like a separate tool and more like the EHR just got a whole lot smarter. This seamless integration ensures the intelligence from our AI solutions becomes a natural part of the care process.
Ready to move from theory to action? Ekipa AI can help you build a clear, actionable plan. Our Custom AI Strategy report is designed to accelerate your journey into clinical decision intelligence. If you have more questions, our expert team is ready to help.