Improving Patient Experience with AI Solutions: A Practical Guide for Clinics
Explore how improving patient experience with AI solutions can elevate care, efficiency, and satisfaction—practical steps you can implement today.
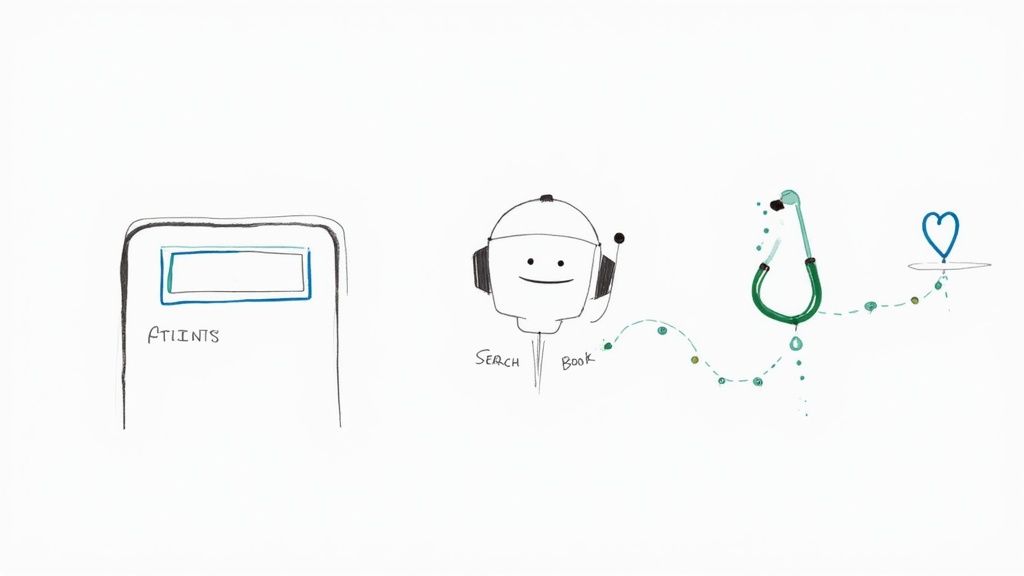
Using AI to improve the patient experience isn't some far-off idea anymore. It's a real, on-the-ground necessity. Patients today expect their healthcare to be as responsive, personal, and easy to access as everything else in their lives. This means bringing in smart tools like AI-powered chatbots for scheduling appointments or automated reminders that help people stick to their treatment plans. These first digital interactions are where you start building trust and getting better results.
The Digital Shift in Modern Patient Care
Think about it: the modern patient's journey almost never begins in a waiting room. It starts with a Google search. That simple fact changes everything. It positions AI not as a futuristic accessory but as the core operating system for a healthcare system that actually listens to and responds to patients. People now expect the same on-demand convenience from their doctor that they get from their bank.
This means instant access to information, personalized messages, and proactive communication are the new baseline. A simple phone call to book an appointment feels clunky and slow when we’re all used to 24/7 digital services.
Meeting Modern Patient Expectations
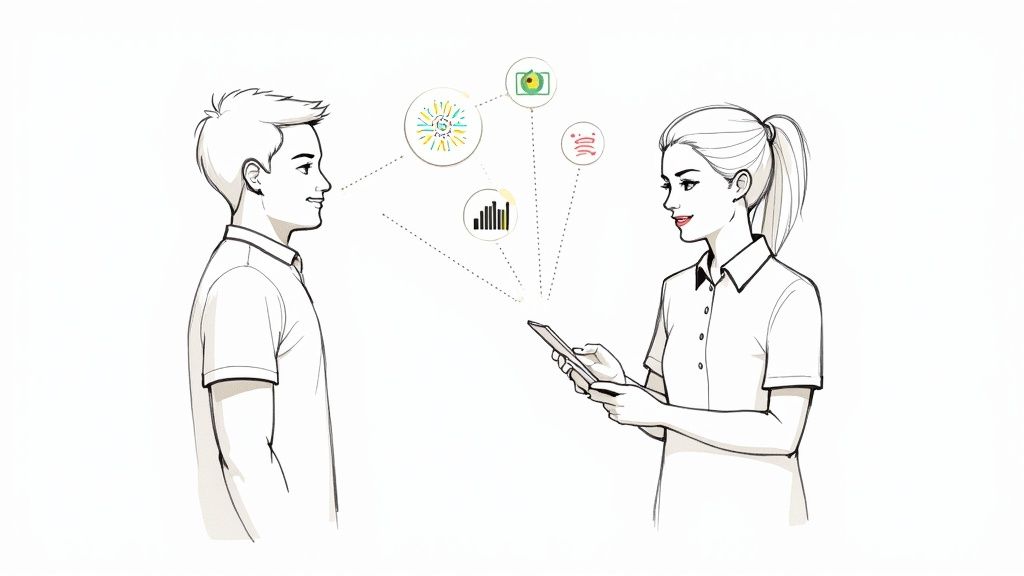
AI makes its biggest, most immediate impact right in that gap between what patients expect and what traditional healthcare can deliver. The very first interactions a person has with your clinic or hospital are critical. They set the tone for the entire relationship.
Here are a few key areas where https://www.ekipa.ai/industries/healthcare can really move the needle:
-
Effortless Scheduling: AI chatbots can book and reschedule appointments and answer frequently asked questions anytime, day or night. This frees up your admin staff to focus on patients with more complex needs.
-
Proactive Communication: Smart, automated reminders for appointments, medications, and follow-ups are a game-changer. They directly improve patient compliance and can slash no-show rates, which can hit as high as 30% in some specialties.
-
Personalized Information: Instead of generic pamphlets, AI can send patients relevant articles and videos based on their specific diagnosis or an upcoming procedure. This helps them become more engaged and informed partners in their own health.
A solid strategy is everything when it comes to improving the patient experience with AI. You're not just buying new software; you're fundamentally redesigning how you deliver care, and you have to see it through the patient's eyes.
This isn't just about plugging in technology; it takes real strategic thinking. As healthcare continues its digital evolution, it's worth exploring the practical strategies for improving patient experience that can work for your practice.
By focusing on these initial digital touchpoints, healthcare organizations can build a stronger, more trusting relationship with patients from their very first click.
Pinpointing Where AI Can Make the Biggest Impact
Before you even think about specific AI tools, you have to get a brutally honest look at your current patient experience. Jumping into a new technology without knowing exactly what problem you're trying to solve is a fast track to a failed project and wasted budget. The real goal here is to find the moments of friction—the genuine pain points—that both your patients and your staff run into day after day.
This all starts with a deep dive into the entire patient journey. I mean every single step. You need to trace their path from the moment they first search for a new doctor online, through scheduling, the visit itself, and all the way to post-visit follow-ups and that dreaded billing cycle. Each of these touchpoints is a hidden opportunity for a smarter, AI-driven improvement.
Mapping the Patient Journey
The key is to gather a mix of hard data and human stories. Pull your operational metrics—things like appointment wait times, no-show rates (a big one!), and how long people are on hold with your call center. That gives you one part of the picture.
But then you need the qualitative side. Dig into patient feedback from surveys, read your online reviews (yes, even the ugly ones), and have actual conversations. This is where you uncover the real frustration.
When you put these two datasets together, the problem areas jump out. Are your phone lines constantly jammed, making it nearly impossible to book an appointment? Do patients call repeatedly, confused by a billing statement that looks like it's written in a different language? Are your clinicians spending more time staring at a screen, clicking boxes in the EHR, than looking their patients in the eye? These are the exact spots where a well-placed AI solution can be a game-changer.
A data-driven approach takes the guesswork and internal politics out of the equation. It lets you zero in on the problems that truly matter, ensuring your tech investments solve real needs, not just perceived ones.
To make this process stick, you have to formalize it. A structured AI requirements analysis is non-negotiable. It creates a foundational document that gets all your stakeholders on the same page and clarifies the real technical and operational needs for any project you're considering. This is the first, most critical step in building a solid business case, a process we guide our clients through with our expert AI strategy consulting.
Prioritizing High-Impact AI Opportunities
Okay, so you’ve mapped the journey and have a list of pain points. Now what? The temptation is to try and fix everything at once, but that’s a classic recipe for disaster. You have to be strategic. This is where a simple prioritization matrix becomes your best friend.
This framework is all about evaluating potential projects against a consistent set of criteria. It forces you and your team to think critically about the real-world impact versus the practical difficulty of each idea.
Here’s a simple way to lay it out:
AI Opportunity Prioritization Matrix
This matrix is designed to help you cut through the noise and compare potential AI initiatives on an even playing field. By scoring each opportunity based on patient impact, implementation difficulty, and potential return, you can quickly identify the low-hanging fruit and the longer-term strategic bets.
| Patient Journey Stage | Identified Pain Point | Potential AI Solution | Patient Impact (1-5) | Implementation Complexity (1-5) | Estimated ROI (Low/Med/High) |
|---|---|---|---|---|---|
| Appointment Scheduling | Long phone hold times, limited office hours for booking | AI-powered web chatbot for 24/7 scheduling | 5 | 2 | High |
| Clinical Visit | Physician burnout from extensive EHR documentation | Ambient clinical scribe for automated note-taking | 4 | 4 | High |
| Post-Visit Follow-Up | Poor medication adherence, patient confusion | Automated, personalized follow-up messages & education | 4 | 3 | Medium |
| Billing & Payments | Confusion over statements, surprise bills | AI tool for real-time cost estimation and clear summaries | 3 | 3 | Medium |
This kind of visual guide makes your best starting points obvious. Look at that scheduling chatbot—high patient impact and low complexity. That’s a perfect pilot project. It delivers a quick, visible win that builds momentum and proves the value of AI to the rest of the organization.
For a much more granular breakdown, a Custom AI Strategy report can provide an analysis tailored to your specific clinical workflows and business goals. By systematically finding and prioritizing your opportunities like this, you ensure your AI journey is strategic, focused, and set up for success right from the start.
Giving Clinicians Time to Focus on Patients
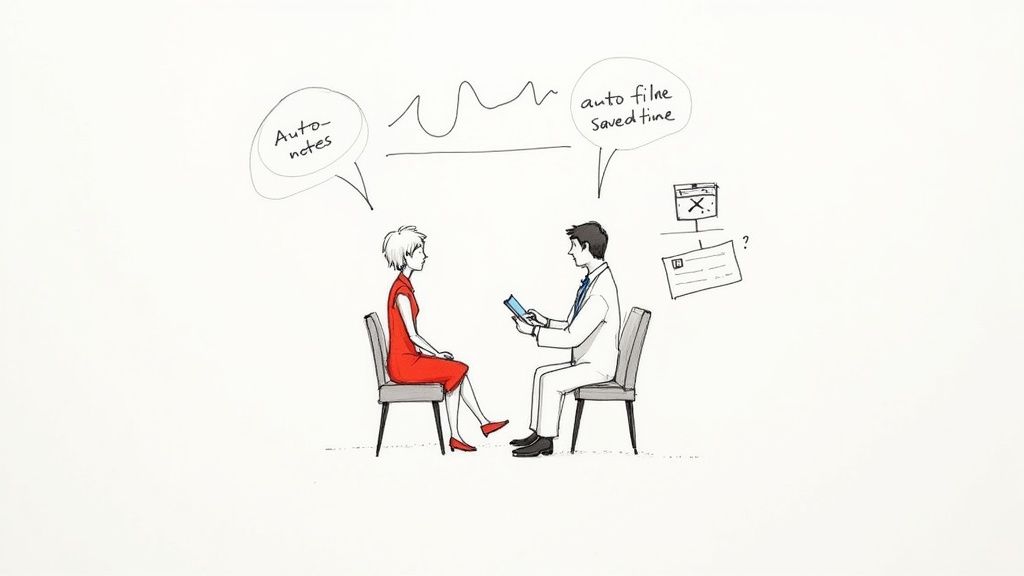
You can't deliver a truly positive patient experience when your clinicians are drowning in administrative work. It's just not possible. One of the most powerful—and often overlooked—ways AI can help is by directly tackling physician burnout at its source: the documentation burden. This isn't just about operational efficiency; it’s a fundamental shift that puts the human connection back at the heart of healthcare.
The link between a clinician's well-being and a patient's satisfaction is crystal clear. When doctors and nurses are less stressed and more present, they listen better, show more empathy, and build stronger relationships. This is the real secret to improving patient experience with AI solutions.
The End of "Pajama Time"
For years, clinicians have been wrestling with the mountain of administrative tasks tied to electronic health records (EHRs). This has created a phenomenon known as "pajama time," where doctors spend hours after their shifts—at home, late into the night—just to catch up on notes. This isn't just an inconvenience; it erodes their personal lives, fuels exhaustion, and pulls their focus away from patients.
AI-powered ambient scribing is the most promising solution to this problem I've seen. These tools work quietly in the background during a patient visit, listening to the natural conversation. The AI then intelligently transcribes, structures, and summarizes the entire interaction, creating a clinical note that’s nearly ready for the EHR.
This isn't a small adjustment. It's a complete overhaul of a broken workflow, handing back precious minutes from every single appointment.
Reclaiming the Doctor-Patient Relationship
By automating the soul-crushing process of note-taking, ambient AI scribes let physicians finally put down the keyboard and make eye contact. They can be fully present in the conversation, actively listening to their patient's concerns without the constant distraction of typing and clicking.
The impact is immediate and profound:
-
Deeper Engagement: Clinicians can pick up on subtle, non-verbal cues they would have otherwise missed while staring at a screen.
-
Improved Accuracy: The AI captures the full conversation, dramatically reducing the risk of manual data entry errors or forgetting key details.
-
Greater Patient Trust: Patients feel heard and valued when they have their doctor's undivided attention. That connection is the foundation of a strong therapeutic relationship.
Freeing clinicians from administrative overload is one of the most direct ways to improve the quality of patient interactions. When doctors are less burdened by paperwork, they can be more present, empathetic, and focused on delivering exceptional care.
This isn't just wishful thinking; the numbers tell a compelling story. Ambient scribing has quickly become one of the most successful clinical AI applications out there, generating $600 million in annual revenue and showing a staggering 2.4x year-over-year growth rate.
Consider that doctors spend roughly one hour on documentation for every five hours of patient care. A recent 10-week pilot study found AI scribes slashed documentation time during appointments while still producing high-quality notes. Unsurprisingly, primary care providers reported a significant drop in both administrative burden and cognitive load. You can learn more about these findings on the state of AI in healthcare for a deeper dive.
A Strategic Investment in Internal Tooling
Implementing a tool like an ambient scribe is a perfect example of a smart investment in internal tooling. While the clinician is the direct user, the patient is the ultimate beneficiary. When you cut documentation from hours down to minutes per day, the positive effects ripple across the entire organization.
You’ll see higher staff morale, reduced turnover, and a clinical environment where providers have the mental and emotional space to truly connect with patients. That is the very essence of patient-centric care. For organizations ready to make this leap, a solution like our Clinic AI Assistant offers a great starting point for automating these critical administrative tasks.
By strategically deploying these kinds of AI solutions, you aren't just buying software. You're investing in your most valuable asset—your clinical team—and, by extension, the quality of care every single patient receives.
Extending Care Beyond the Clinic Walls
Let's be honest: modern healthcare can't just be about what happens during a 15-minute appointment. The real work of managing health, especially for chronic conditions, happens every single day in a patient's home. This is where AI-driven Remote Patient Monitoring (RPM) completely changes the game, moving care from a reactive "wait-and-see" model to a proactive, continuous partnership.
This shift is a cornerstone of improving the patient experience with AI. Instead of waiting for a crisis, RPM systems use smart technology to get ahead of risks. This proactive approach gives patients a real sense of control over their health, which is incredibly powerful.
From Raw Data to Proactive Insights
At its core, RPM is a simple idea supercharged by AI. You have wearable sensors, smart scales, blood pressure cuffs, and glucose monitors constantly collecting vital health data. But data by itself is just noise. The real magic begins when machine learning algorithms start analyzing these data streams in real time.
These AI models are trained to spot subtle patterns and deviations that are nearly impossible for a human to catch. They can flag when a patient's metrics are trending in a dangerous direction, often long before the patient even feels any symptoms. This predictive power is what turns RPM from a simple monitoring tool into a potentially life-saving system.
This is a perfect example of how AI Automation as a Service can deliver tangible, positive outcomes. It’s all about building intelligent workflows that extend your clinical team's reach far beyond the clinic's physical walls.
The Real-World Impact of Remote Monitoring
When you get an RPM program right, the benefits are significant and easy to measure. You'll see improvements in everything from patient outcomes to your organization's bottom line.
-
Empowered Patients: When people can see their own health data and connect it to their daily actions, they become much more engaged and motivated in their own care.
-
Fewer Hospitalizations: By catching problems early, you can stop minor issues from turning into full-blown emergencies that demand a costly hospital stay.
-
Smarter Chronic Disease Management: RPM helps clinical teams manage large populations of patients with conditions like diabetes, hypertension, and heart failure far more effectively, letting them focus their time on those who need it most.
Remote patient monitoring is one of the most direct ways to deliver on the promise of value-based care. It shifts the focus from just treating sickness to actively maintaining wellness, which is simply better for patients and more sustainable for the entire healthcare system.
The numbers really drive this point home. One three-month study on RPM implementation found that emergency department visits dropped by a staggering 68%, and hospitalizations fell by 35%. The cost savings were just as impressive, with average hospitalization costs plummeting from $3,842 to $1,399. You can dive into the full research on RPM's impact to see the detailed outcomes.
Getting Started with Your RPM Strategy
For organizations ready to jump in, there are two main paths forward. You can partner with an established vendor that offers a comprehensive RPM platform—this is often the quickest way to get a pilot program up and running. The other option, especially for those with unique needs or a desire for more control, is to invest in custom healthcare software development. This allows you to build a proprietary system that fits your existing workflows perfectly.
No matter which path you choose, the goal is the same: use powerful AI tools for business to deliver more responsive, personalized, and effective care. As we've covered before, choosing the right tech is all about aligning its capabilities with your core strategic goals. It’s worth exploring these real-world use cases to see how other organizations have made it work. This proactive model doesn't just improve health outcomes—it builds the kind of lasting trust and loyalty that shows patients you're truly committed to their well-being, both inside and outside the clinic.
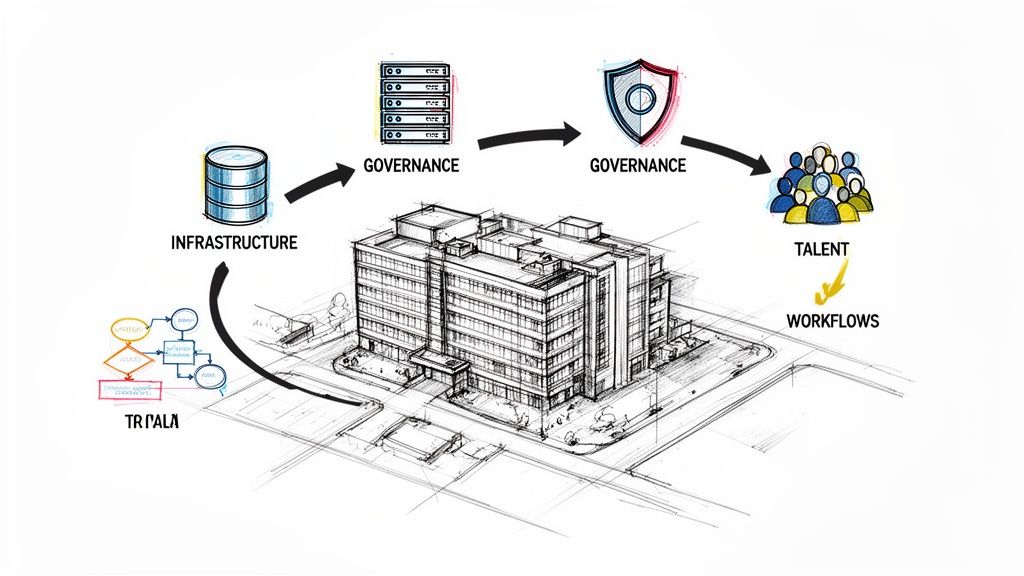
Your 180-Day AI Implementation Roadmap
An idea without a solid plan is just a wish, especially when it comes to healthcare technology. I’ve seen too many promising AI projects fizzle out because they lacked a clear, phased approach. To really move the needle on patient experience, you need a structured journey from initial discovery to measurable, scalable impact.
This 180-day roadmap is a practical blueprint I've seen work time and again. It’s designed to guide your team, manage expectations, and turn that initial investment into results you can actually see and feel. Breaking the process down prevents scope creep and builds momentum through a series of small, strategic wins.
Days 1-60: Discovery and Pilot Selection
The first two months are all about laying the groundwork. You’re moving from a general desire for "improvement" to a specific, actionable plan. The goal here is to get your key players on the same page, dig into your operational data, and pick a high-impact pilot project that has a real shot at success.
Here’s what to focus on first:
-
Align Your Stakeholders: Get a cross-functional team in a room—clinical leaders, IT staff, administrative heads, and patient advocates. Getting everyone’s perspective from the start is non-negotiable for buy-in.
-
Drill Down on the Data: Use the prioritization matrix we talked about earlier to analyze patient journey pain points. You're looking for a problem that's both a major headache for patients and something current AI can genuinely solve.
-
Pick Your Pilot Project: Zero in on one single, high-impact use case. An ideal pilot delivers a visible win without being overly complex. Think about an AI scheduling chatbot for a busy department or an ambient scribe for a few physicians.
Your initial pilot project sets the tone for everything that follows. A quick, decisive win builds confidence and makes it much easier to get the resources you need for more ambitious projects down the road.
By the end of day 60, you should have a rock-solid project charter. This document needs to spell out the problem you’re solving, the pilot's scope, the key success metrics (KPIs), and a detailed budget. This is the bedrock of your entire implementation.
Days 61-120: Development and Initial Deployment
With a clear plan in your back pocket, the next 60 days are all about execution. This is where the technical work really begins as you prepare data, select the right partners, and start rolling out your chosen solution. Sticking to a proven structure here is the key to keeping things on track.
This is exactly where a structured AI Product Development Workflow becomes indispensable. It gives you a repeatable framework for managing everything from data prep to vendor evaluation and integration, ensuring nothing critical falls through the cracks. It’s simply a systematic way to reduce risk and move faster.
Take remote patient monitoring, for example. The core logic is straightforward but powerful: collect data, analyze it for insights, and trigger the right alerts.
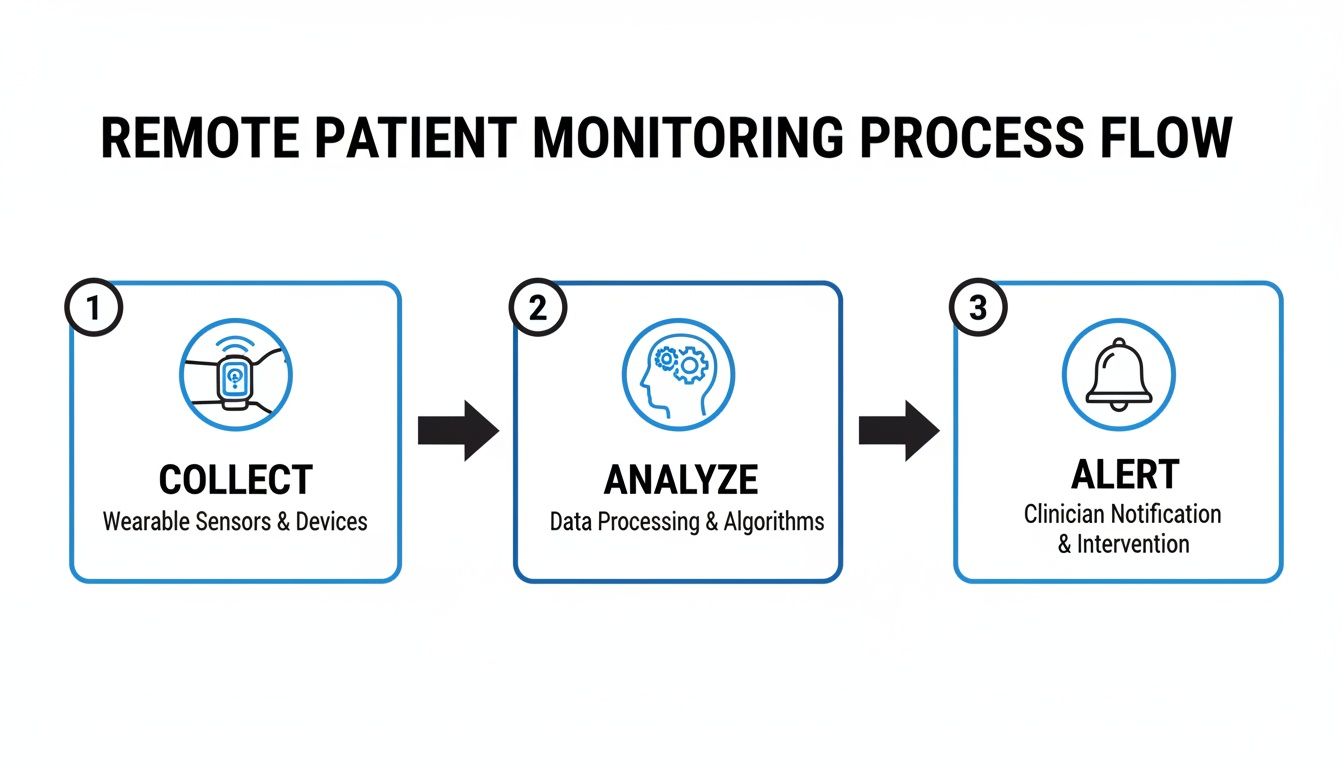
This simple "collect, analyze, alert" sequence is the foundation of so many proactive healthcare AI systems. It's a great illustration of how a clear process delivers results.
Days 121-180: Evaluation and Scaling Strategy
The final phase is all about measurement and looking ahead. Once your pilot has been up and running for a bit, it’s time to get rigorous about evaluating its performance against the KPIs you set back in phase one. This data-driven assessment is how you prove the value of your investment and build the case for expansion.
Your final stretch should include these activities:
-
Measure Against KPIs: Collect and analyze the performance data. Did you actually reduce patient wait times? Did clinician satisfaction scores go up? You have to quantify the impact.
-
Gather Human Feedback: Don't just look at the numbers. Conduct surveys and interviews with the staff and patients who used the new system. Their real-world experiences are just as valuable.
-
Map Out the Scaling Plan: If the pilot was a success, it's time to draft a detailed plan for a broader rollout. This plan needs to address the budget, training, and technical requirements to take the solution to other departments or even other facilities.
This structured roadmap ensures your AI investment truly improves patient care. By moving methodically from discovery to deployment and evaluation, you can navigate the common hurdles like data governance and change management, setting your organization up for lasting success.
Forging a More Human Path in Healthcare
Ultimately, weaving AI into the fabric of patient care isn't a one-and-done project. It's an ongoing commitment. It all starts by truly listening to your patients, figuring out where their journey is most frustrating, and then pinpointing the high-impact solutions that will make a real difference—not just for them, but for your clinicians, too.
When you get this right, you’re not just implementing technology; you're building a healthcare system that feels more personal, runs more smoothly, and is fundamentally more human.
Of course, the technology is just one piece of the puzzle. To really move the needle on patient happiness, your AI initiatives should support broader strategies to improve patient satisfaction scores. This big-picture view ensures that every tool you adopt serves the core mission: delivering better, more compassionate care.
You don't have to figure all this out on your own. Bringing in experts who have been down this road before can help you move faster and avoid common pitfalls, ensuring the AI solutions you build are designed to last. A clear vision combined with the right expertise is what creates a meaningful, positive impact on every life you touch.
If you're ready to talk through your organization's unique challenges and see how a focused approach can deliver real results, connect with our expert team today.
Frequently Asked Questions (FAQ)
What is the best way for a clinic to start implementing AI for patient experience?
Start small and targeted. Instead of a massive overhaul, identify a single, high-impact pain point in the patient journey. For many, this is appointment scheduling. Implementing an AI-powered chatbot for 24/7 scheduling can provide a quick, visible win, freeing up administrative staff and improving patient convenience. This success builds momentum for more complex projects. As we explored in our guide to scaling AI across your organization, a successful pilot is crucial for long-term buy-in.
How can we measure the ROI of AI solutions for patient experience?
Measuring ROI requires a two-pronged approach. Quantitatively, track metrics like reduced patient wait times, lower appointment no-show rates, and decreased administrative costs. Qualitatively, measure patient satisfaction scores (e.g., Net Promoter Score) and clinician burnout rates before and after implementation. A strong business case combines hard financial savings with clear improvements in patient and staff well-being.
What are the biggest challenges in implementing healthcare AI?
The primary challenges are typically data, integration, and people. Ensuring robust data privacy and HIPAA compliance is non-negotiable. Integrating new AI tools for business with existing systems, especially legacy EHRs, can be technically complex. Finally, managing change is critical; staff must see AI as a supportive tool, not a threat. Clear communication and training are essential to show how AI reduces administrative burdens and enables better patient care.
Can AI help reduce physician burnout?
Absolutely. This is one of AI's most powerful applications in healthcare. Tools like ambient AI scribes can automatically listen to and document patient encounters, drastically cutting down on "pajama time"—the hours clinicians spend on paperwork after their shifts. By automating these administrative tasks, AI gives clinicians more time for direct patient interaction, leading to reduced stress, higher job satisfaction, and more empathetic care. This investment in internal tooling directly benefits the patient experience.
Ready to build a smarter, more patient-centric healthcare experience? At Ekipa AI, we specialize in turning your strategic goals into reality with a clear, actionable plan. Discover how our AI Strategy consulting tool can help you identify and execute the right AI opportunities for your organization.