A Guide to Healthcare Data Stewardship in the Age of AI
Unlock AI's potential in healthcare with our guide to healthcare data stewardship. Learn to build a framework that turns health data into a strategic asset.

Think of all the patient data your organization holds—every chart, lab result, and doctor's note. It's not just a collection of files; it's a vast library filled with deeply personal stories. Healthcare data stewardship is the essential practice of acting as the responsible guardian for that library.
This isn't a simple IT checklist. It's the very foundation of patient trust and the engine for modern medical breakthroughs.
Why Data Stewardship Suddenly Matters More Than Ever
Good stewardship builds the bridge between raw health information and the life-saving insights technology promises. We're seeing an explosion of data from digital health records, wearable devices, and advanced imaging. For leaders, championing stewardship is no longer optional—it's the only way to safely harness powerful technologies and genuinely improve patient care. This is the groundwork that allows advanced AI solutions to redefine what's possible in medicine.

This goes far beyond just storing data. It’s about guaranteeing its quality, security, and ethical use from the moment it’s collected to the moment it’s archived. A data steward is like a master librarian for a hospital's most sensitive information. They don't just put books on a shelf; they verify their accuracy, control who gets to read them, and ensure they're preserved for the future.
The Sheer Scale of the Data Challenge
The need for this kind of structured oversight is growing more urgent by the day. The sheer volume of global healthcare data is mind-boggling, and it's expanding at a pace that demands smart management strategies. This growth is fueled by everything from the universal adoption of electronic health records (EHRs) to the stream of data coming from our own smartwatches.
Just look at the numbers in the U.S. As of 2021, a staggering 96% of non-federal acute care hospitals had adopted certified EHRs. That’s a huge jump from just 28% in 2011. It's no surprise that the big data in healthcare market, valued at $68.56 billion in 2023, is expected to skyrocket to $283.43 billion by 2032, according to research from SNS Insider.
This data deluge makes stewardship non-negotiable for a few key reasons:
- Fuel for Advanced Analytics: High-quality, well-governed data is the essential ingredient for building accurate predictive models and AI-powered diagnostics.
- The Currency of Patient Trust: Proper stewardship is a clear signal to patients that you're committed to protecting their most sensitive information.
- Staying on the Right Side of the Law: It creates the necessary framework to comply with strict regulations like HIPAA, helping you avoid massive fines and legal headaches.
To truly grasp how these elements work together, it helps to think of stewardship as resting on several core pillars. Each one supports the entire structure, ensuring data is not just managed, but managed with purpose.
The Pillars of Modern Healthcare Data Stewardship
This table breaks down the core components of healthcare data stewardship into actionable pillars, showing their strategic importance.
| Pillar | Description | Business Impact |
|---|---|---|
| Data Governance | Establishes the rules of the road: who can access data, what they can do with it, and how decisions are made. | Creates clear accountability, reduces risk, and ensures consistent data handling across the organization. |
| Data Quality | Ensures data is accurate, complete, and reliable. This involves cleaning, validating, and standardizing information. | Prevents clinical errors, improves the accuracy of analytics and AI models, and boosts operational efficiency. |
| Data Security | Protects data from unauthorized access, breaches, and cyber threats through encryption, access controls, and monitoring. | Safeguards patient privacy, maintains regulatory compliance (HIPAA), and protects the organization's reputation. |
| Ethical Use & Privacy | Goes beyond legal requirements to ensure data is used responsibly, fairly, and with patient consent at the forefront. | Builds and maintains patient trust, fosters a culture of ethical innovation, and mitigates long-term reputational risk. |
| Data Lifecycle Management | Manages data from its creation to its eventual archival or deletion, ensuring it's handled properly at every stage. | Optimizes storage costs, ensures data relevance, and helps meet data retention and compliance requirements. |
These pillars aren't just theoretical concepts; they are the practical building blocks for creating a trustworthy and effective data ecosystem.
Stewardship is no longer a back-office function. It is a strategic imperative that directly impacts patient outcomes, operational efficiency, and the successful implementation of modern medical technologies.
Ultimately, healthcare data stewardship is the disciplined practice that turns chaotic information into a reliable, actionable resource. It’s the essential groundwork for any organization looking to innovate responsibly with specialized Healthcare AI Services and build a data-driven future. Without it, even the most powerful technologies will fail to deliver on their promise.
Navigating the Legal and Ethical Maze of Health Data
When you're handling sensitive patient data, you're not just managing information—you're managing trust. This puts you smack in the middle of a complex web of regulations designed to protect people. Laws like the Health Insurance Portability and Accountability Act (HIPAA) in the U.S. and the General Data Protection Regulation (GDPR) in Europe aren't just red tape; they're the legal foundation of patient confidence.
These laws set firm ground rules for how patient information can be collected, stored, and shared. HIPAA, for example, is the American standard for safeguarding health information, demanding that organizations build strong security measures to keep data out of the wrong hands. It's why using a verified HIPAA compliant platform for things like secure digital transactions isn't just a good idea—it's essential.
The stakes are incredibly high. A misstep can lead to massive fines, but even worse, it can instantly destroy the trust you've worked so hard to build. But make no mistake: just staying compliant is the bare minimum. True stewardship starts where the rulebook ends.
The Ever-Shifting Regulatory Ground
The world of data regulation is anything but static. New frameworks are popping up all the time, putting more pressure on how we handle health data. Take the EU's European Health Data Space (EHDS) and Data Governance Act. These initiatives are fundamentally changing analytics by requiring unified, privacy-first data access across borders.
Meanwhile, in the U.S., HIPAA's tough security standards are running up against the sheer volume of data we're now generating, making things tricky for adopting cloud and AI technologies. For business leaders and CTOs, this constant churn isn't just noise—it’s a clear signal to build compliant AI solutions from the ground up and actively work to root out bias in predictive models.
This isn't a "set it and forget it" situation. You have to stay ahead of the curve, anticipating tomorrow's regulations today. This is where getting expert guidance from an AI Strategy consulting tool can be a game-changer, helping you create flexible systems that adapt to new laws without stifling innovation.
Going Beyond the Law: Tackling the Tough Ethical Questions
Legal compliance is non-negotiable, but our ethical duties run much deeper. Real healthcare data stewardship means wrestling with the tough moral questions that laws can't always answer. Right now, the biggest ethical challenge on the table is making sure data bias doesn't lead to discriminatory AI.
An algorithm trained on data from a single demographic might perform poorly for other groups, leading to misdiagnoses and perpetuating health disparities. Ethical stewardship means actively working to identify and correct these biases before they cause harm.
Think about it this way: a hospital creates a predictive model to flag patients at high risk for a new preventative care program. If the data used to train that model historically underrepresented a specific minority community, the AI might completely miss at-risk individuals from that group. This isn't necessarily a legal breach, but it's a massive ethical failure—one with life-or-death consequences.
Transparency Isn't Optional
To find your way through these ethical minefields, you have to be transparent. It's that simple. Patients have a fundamental right to know how their data is being used, especially when it's feeding an algorithm that makes decisions about their health. This comes down to a few key actions:
- Talk like a human. Give patients clear, easy-to-understand information about your data policies. No legalese.
- Get real consent. Make sure your consent process is explicit and straightforward, not buried on page 37 of a legal document.
- Be ready to explain yourself. You need to be able to show how and why an AI model arrived at a specific conclusion.
Ethical slip-ups, even accidental ones, can shatter patient trust in an instant. By making both legal compliance and ethical integrity your top priorities, you build a foundation strong enough to support the responsible use of data to truly improve healthcare for everyone.
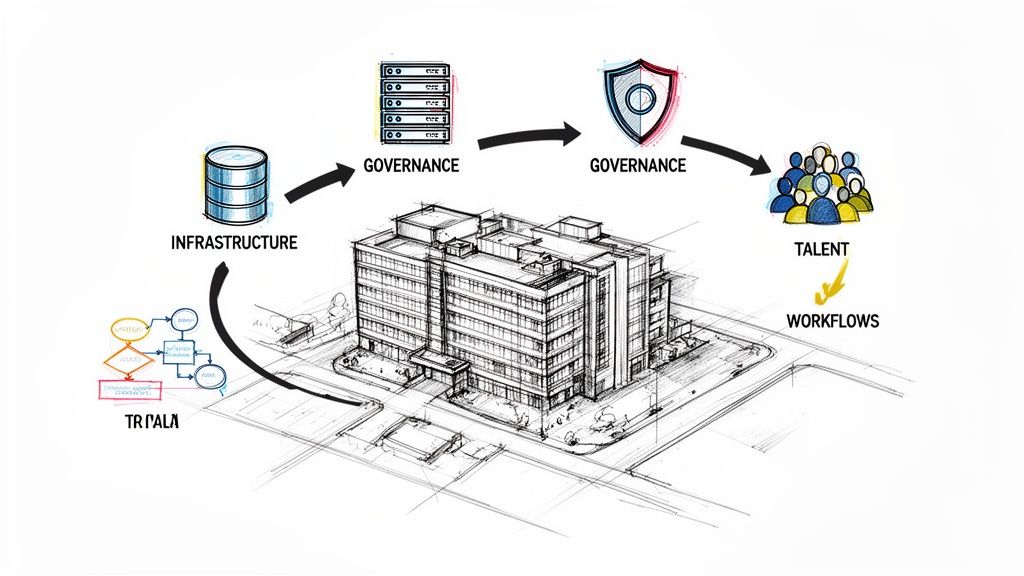
Building Your Data Stewardship Governance Framework
A solid governance framework is the blueprint that transforms good intentions about data into reliable, everyday practice. It’s what takes your organization from simply having data to strategically managing it as a core asset. Without this structure, even the most dedicated data stewardship efforts can fall flat, becoming inconsistent and ineffective.
This isn't about creating red tape or locking data away. Quite the opposite. It’s about establishing clear, secure, and efficient pathways for data to be used responsibly. A well-defined governance structure is the bedrock for scaling operations, enabling powerful AI Automation as a Service, and building the kind of internal tooling that actually makes a difference.
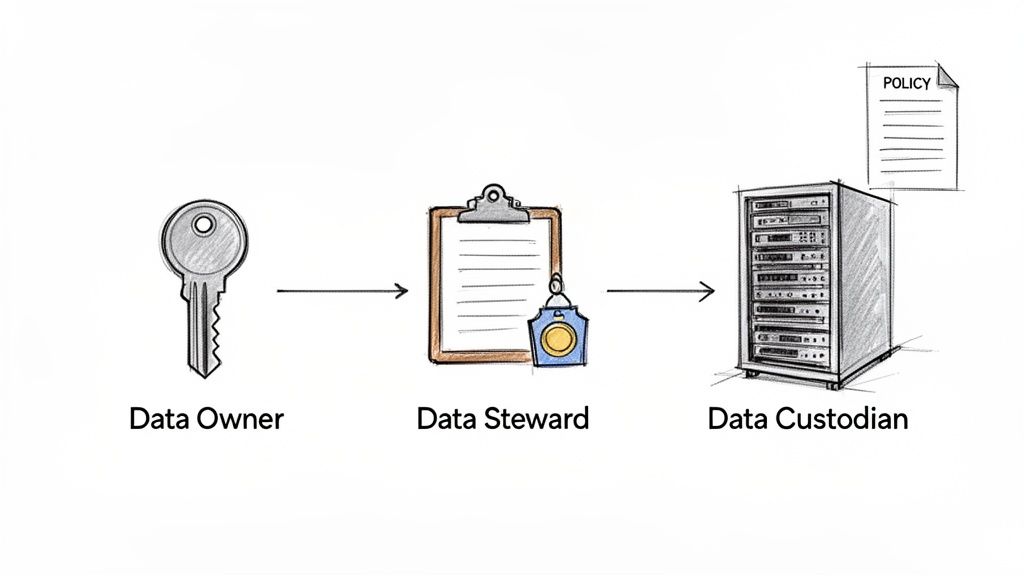
Defining the Core Roles and Responsibilities
The very first step in building your framework is assigning clear accountability. In healthcare data stewardship, there are three roles that form the backbone of any effective governance team. When you clearly define who does what, you eliminate confusion and ensure every piece of data has a designated guardian.
To make sense of these roles, let's break them down.
Key Roles in a Healthcare Data Stewardship Team
| Role | Primary Responsibility | Key Focus |
|---|---|---|
| Data Owner | Strategic accountability for a specific data domain. | Business strategy, policy approval, ultimate accountability. |
| Data Steward | Day-to-day management and implementation of data policies. | Data quality, metadata, business rules, tactical execution. |
| Data Custodian | Technical management and security of data assets. | Infrastructure, security controls, backup, technical implementation. |
Each role is distinct, yet they must work together seamlessly for the system to function. Let's dig a bit deeper into what that looks like in practice.
A Closer Look at the Team
1. Data Owners
Think of a Data Owner as the ultimate decision-maker for a specific area of data. These are usually senior leaders or department heads. For example, the Director of Clinical Operations might "own" all patient admissions data. They are strategically accountable for that data's quality, security, and ethical use, but they aren't bogged down in the day-to-day, hands-on management.
Their job is to:
- Set the rules: They give the final green light on policies for data access and use within their domain.
- Carry final accountability: The buck stops with them if something goes wrong with the data under their watch.
- Approve high-level access: They have the final say on major data access requests.
2. Data Stewards
The Data Stewards are your hands-on managers and subject matter experts. They are the people responsible for putting the Data Owner's policies into practice every single day. A clinical data steward, for instance, might be a nurse informaticist who truly understands the nuances of patient charting and works to ensure data entry standards are actually being met on the floor.
Their daily tasks involve:
- Defining data quality: They establish the specific rules for what makes data accurate and complete.
- Managing metadata: They document what the data means, where it came from, and how it’s supposed to be used.
- Resolving issues: They're the go-to person for any questions about data quality or definitions.
3. Data Custodians
Finally, we have the Data Custodians. These are the technical guardians of the data, almost always coming from the IT department. They are responsible for the "how"—the technical environment where data is stored, moved, and secured. They are the ones who implement the security controls and access rights that the Owners and Stewards have defined.
Their focus is purely technical:
- Technical implementation: They manage the databases, servers, and security infrastructure.
- Access control: They are the ones physically granting or revoking user access based on approved policies.
- Backup and recovery: They make sure data is safely backed up and can be restored if disaster strikes.
A common mistake is to view data governance as solely an IT responsibility. It's not. It is fundamentally a business function that is supported by IT. The most successful frameworks are built on a strong partnership between business leaders (Owners), subject matter experts (Stewards), and technical teams (Custodians).
Crafting Essential Governance Policies
Once the roles are clear, the next step is to create simple, direct policies that govern the entire data lifecycle. These policies are the guardrails for your team, ensuring consistency and compliance across the board.
Your framework should include policies covering three critical areas:
- Data Access and Use: This policy dictates who can see, create, or change data and under what circumstances. It should always be based on the principle of least privilege, a fancy term for a simple idea: users only get access to the data they absolutely need to do their jobs, and nothing more.
- Data Quality Standards: This is where you define what "good" data actually looks like for your organization. The policy should spell out specific metrics for accuracy, completeness, and timeliness, along with a clear process for finding and fixing errors.
- Data Lifecycle Management: This policy governs data from the moment it's created to its eventual archival or deletion. It defines retention periods based on clinical needs and legal requirements, ensuring you don't hold onto sensitive data longer than necessary.
Building this framework is a huge step in your organization's data maturity. It creates the accountability and structure needed to truly trust your data, which is non-negotiable before you can even think about more advanced initiatives like implementing sophisticated Healthcare AI Services.
Connecting Stewardship to Successful Healthcare AI
You can't build a powerful AI solution on a shaky data foundation. It’s that simple. High-quality, ethically sourced data is the fuel for any successful artificial intelligence initiative, and data stewardship is the rigorous process of refining that fuel. Without it, even the most sophisticated AI engine will sputter, stall, or worse, produce dangerous clinical outcomes.
There’s a direct and unbreakable line between how well you manage your data and how well your AI models perform. When stewardship is just an afterthought, you're practically inviting critical AI failures. Algorithms trained on incomplete or messy data churn out unreliable predictions. Models built on biased datasets don't just reflect existing health disparities—they amplify them. These aren't just technical glitches; they are massive risks in a live healthcare environment.
The Dangers of Poor Stewardship in AI
Bad data practices can quietly poison your AI investments before they ever have a chance to deliver value. The old adage of "garbage in, garbage out" is especially brutal in healthcare, where the stakes are quite literally life and death.
Poor stewardship almost always leads to one of these major failures:
- Biased Algorithms: If your historical data doesn't properly represent certain patient groups, the AI you build on it will inevitably fail those same groups. This can lead to anything from misdiagnoses to completely ineffective treatment plans.
- Unreliable Predictions: Data riddled with errors or inconsistencies destroys a model's ability to see patterns and make accurate predictions. This renders tools meant to forecast disease outbreaks or flag high-risk patients completely useless.
- Compliance Nightmares: Launching an AI initiative with poorly governed data is a fast track to violating privacy regulations like HIPAA. The fallout? Crippling financial penalties and a catastrophic loss of patient trust.
As we explore how data stewardship fuels AI, it's also worth thinking about the bigger picture, like the ethical implications of AI giving professional advice.
Unlocking Opportunities with a Solid Data Foundation
Now, let's flip the script. When you get data stewardship right, the possibilities are incredible. A solid foundation of clean, well-managed, and ethically sourced data turns AI from a potential liability into a game-changing asset for improving patient care.
The need has never been greater. An estimated 4.5 billion people still lack full access to essential health services, a gap that modern, data-driven health systems can help close. This urgency is reflected in the market; the healthcare analytics sector, valued at $52.98 billion in 2024, is expected to soar to $198.79 billion by 2033. This growth is largely fueled by regulations demanding better privacy and interoperability—the very pillars of good stewardship.
With a strong stewardship framework in place, you can confidently build advanced solutions:
- Predictive Analytics: Reliably forecast disease outbreaks, identify at-risk populations, and optimize hospital staffing with models built on data you can actually trust.
- Personalized Medicine: Move beyond one-size-fits-all care by developing AI that helps tailor treatment plans to an individual’s unique genetic and health profile.
- Operational Efficiency: Automate routine administrative work with tools like our Clinic AI Assistant, which helps free up your clinical staff to focus on what matters most—their patients.
Stewardship isn't a final checkbox; it's woven into every single stage of a successful AI project. It starts the moment you begin analyzing requirements and continues all the way through data preparation, model training, and deployment. Think of it as the essential first step, not an afterthought.
At the end of the day, treating data stewardship as a non-negotiable prerequisite for AI is the only way to build technology that is safe, effective, and ethical. It's the commitment that transforms a promising idea into a reliable tool that genuinely improves patient care.
Your Roadmap for Implementing Data Stewardship
Moving from the theory of data stewardship to a real, working program can feel like trying to boil the ocean. It's a huge undertaking. The secret is to break it down into smaller, more manageable steps. This roadmap gives you a clear path to follow, whether you're starting from scratch or trying to mature an existing program. It makes the whole process feel achievable, not overwhelming.
The idea is to build momentum phase by phase, proving the value of your work as you go. As you can see below, strong data stewardship isn't just a compliance task—it's the bedrock for any successful AI initiative in healthcare.
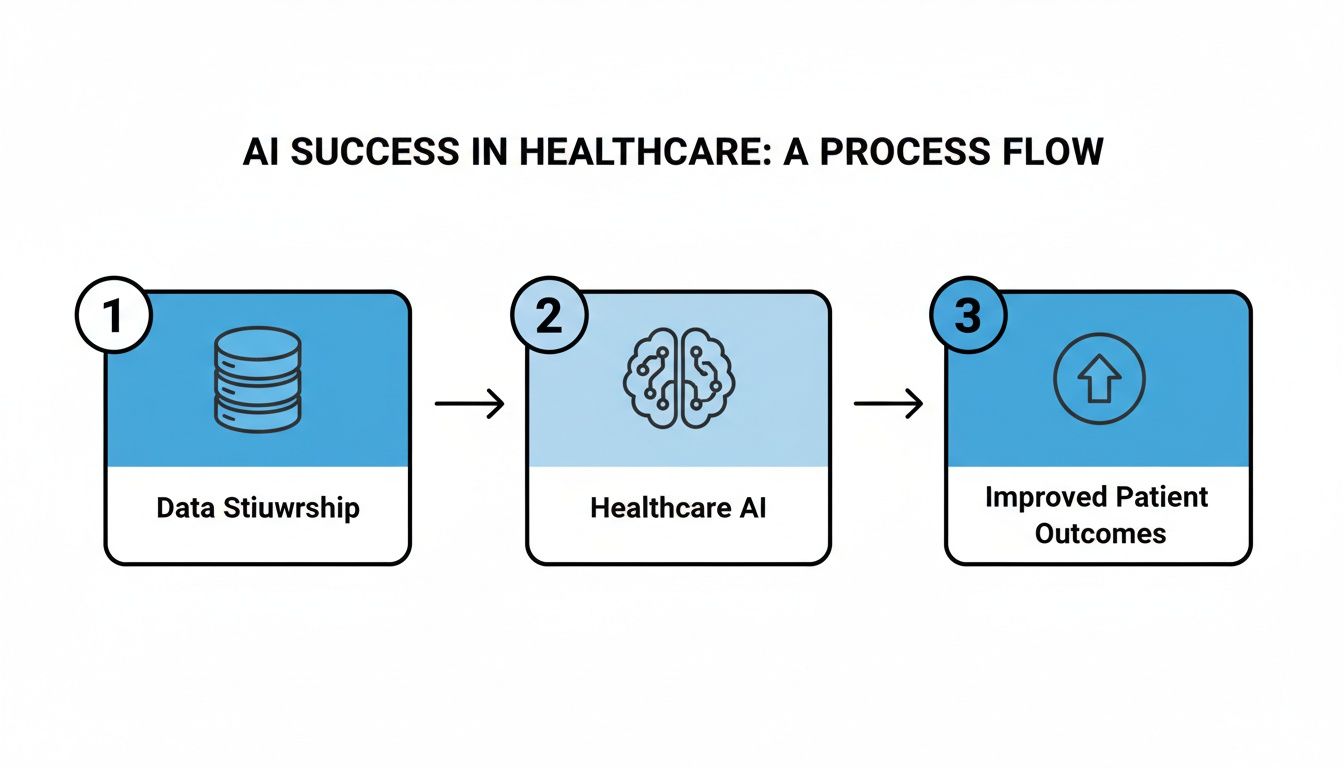
This really drives home the point that stewardship is the essential first step. It's what allows you to generate the kind of reliable, AI-driven insights that can genuinely improve patient care.
Phase 1: Assessment and Discovery
Before you can build anything, you need to know the lay of the land. This first phase is all about discovery—creating a complete inventory of your entire data landscape. You can't govern what you don't know you have.
The main goal here is to identify every single data source. We're talking EHRs, billing systems, lab results, imaging archives, and everything in between. You'll need to map out data flows to understand how information moves through your organization and classify data based on its sensitivity (like Protected Health Information, or PHI). One of the biggest hurdles you'll face is uncovering "shadow IT"—all that data living in unofficial spreadsheets or departmental databases that can pose a massive risk.
Phase 2: Framework Design
Once you have a clear picture of your data, you can start designing the governance framework. This is where you put pen to paper and define the rules, roles, and responsibilities we talked about earlier. It is absolutely critical to get executive buy-in at this stage; their support will be the backbone of enforcement later on.
Your chief objective is to establish clear accountability. Formally assign your Data Owners, Stewards, and Custodians. Then, draft your core policies for things like data quality, access control, and data lifecycle management. Just remember, these policies need to be practical. They should be designed to enable secure data use, not just to lock it down.
Phase 3: Technology Selection
Policies are great, but technology is what brings your framework to life. The right tools can turn your rules into automated, enforceable actions, making stewardship tasks much simpler while giving you a clear view into your data ecosystem.
The goal is to pick tools that actually fit your specific needs. This might include:
- Data Catalogs: These create a searchable, Google-like inventory of all your data assets.
- Master Data Management (MDM) Platforms: Essential for creating a single source of truth for critical data, like your master patient or provider index.
- Data Quality Tools: These can automatically monitor, clean, and validate your data, saving countless hours of manual work.
When you're looking at vendors, prioritize solutions that play nicely with your existing systems (especially your EHR) and support healthcare-specific standards like HL7 or FHIR. These are key elements of any successful custom healthcare software development project.
Phase 4: The Pilot Program
Don't try to roll this out across the entire organization all at once. That's a recipe for disaster. Instead, start small with a focused pilot program. This lets you test-drive your framework and technology on a smaller scale, learn some valuable lessons, and score some early wins to build momentum.
Pick a single, high-impact data domain for your pilot—something like patient admissions or medication administration data. Your goal is to implement your new roles, policies, and tools within this limited scope. This controlled environment lets you work out the kinks in your process and get direct feedback from your new data stewards. A successful pilot becomes a powerful case study you can use to get support for a wider rollout.
Phase 5: Continuous Improvement
Data stewardship isn't a project you finish. It’s a discipline you practice. The final phase is about creating a cycle of continuous monitoring, measurement, and refinement. This is how you ensure your program stays effective and can adapt to new regulations, technologies, and challenges.
Establish key performance indicators (KPIs) to track things like data quality scores, how often you pass compliance audits, or how long it takes for researchers to get access to the data they need. You'll want to review these metrics regularly and use them to fine-tune your policies and retrain your teams. This iterative approach ensures your data foundation gets stronger over time and is a cornerstone of any successful AI Product Development Workflow.
By following this roadmap, you can systematically build a robust data stewardship program that not only protects patient information but also unlocks incredible new opportunities for innovation.
How Do You Know If Your Stewardship Program Is Actually Working?
It's one thing to launch a data stewardship program; it's another thing entirely to prove it's making a difference. To get buy-in and justify the investment, you need to show real, measurable results. We're not talking about fuzzy goals here, but hard numbers that connect your stewardship efforts directly to business value and better patient outcomes.
Success isn't about how many policies you've written. It's about the tangible impact those policies have on data quality, compliance, the speed of your operations, and even the accuracy of your AI models.
The Four Pillars of Measuring Stewardship Success
To get a complete picture, you can't just look at one area. A great way to track progress is to use a balanced approach, focusing on metrics across four key domains. This ensures you're making well-rounded improvements, not just shifting a problem from one department to another.
1. Data Quality Metrics
This is ground zero for your stewardship program. If the data isn't getting better, something is wrong. Clean, trustworthy data is the bedrock of everything you do, from making sound clinical decisions to building next-generation AI solutions.
- Accuracy Rate: What percentage of your data is actually correct? For critical patient information, you should be aiming for 98% or higher.
- Completeness Score: Are all the essential fields filled out in your EHRs, billing systems, and other core datasets? Track the percentage of complete records.
- Duplicate Reduction: A classic sign of data chaos is duplicate records. A steady decrease in duplicate patient or provider files shows your governance and master data management are taking hold.
2. Compliance and Risk Reduction Metrics
Let’s be honest: strong stewardship is your best line of defense against eye-watering fines and reputational damage. These metrics show stakeholders that you're actively protecting the organization.
- Audit Success Rate: How are you faring in internal and external audits? The goal should be 100% compliance with major regulations like HIPAA, with no major findings.
- Data Breach Incidents: A falling number of security incidents or unauthorized access attempts is a direct reflection of better data handling and security controls.
- Time to Fulfill Data Subject Requests: When patients ask for their data under regulations like GDPR, how fast can you deliver? Tracking this shows your process is becoming more efficient and compliant.
A successful stewardship program transforms compliance from a reactive fire drill into a predictable, well-managed process. You're building a defensible position that protects both your patients and the organization's future.
3. Operational Efficiency Metrics
Good stewardship isn't just about rules; it’s about making everyone's job easier. By removing data-related roadblocks, you save a ton of time and money. These KPIs demonstrate that impact.
- Time-to-Data Access: How long do your analysts, researchers, or clinicians have to wait for the data they need to do their jobs? A 50% reduction in that wait time is a massive win.
- Reduced Manual Rework: Think about all the hours your team spends manually cleaning data before it can be used for a report. Tracking a decrease here shows a direct return on your stewardship investment.
4. AI Enablement Metrics
At the end of the day, great data stewardship is what fuels real innovation. If your organization is investing in Healthcare AI Services, the link between data quality and AI performance is direct and undeniable.
- Improved Model Accuracy: Are your predictive models getting smarter? As the quality of your input data goes up, the accuracy of your models should follow, leading to more reliable clinical predictions.
- Faster Model Development: How long does it take your data science team to build and deploy a new model? Well-governed, analysis-ready data can dramatically slash the time spent on data preparation.
By consistently tracking these KPIs, you can build a powerful story that connects your stewardship program to tangible business outcomes. This data-driven narrative helps leadership see the program's true value, making it much easier to secure ongoing support and showcase its role in successful real-world use cases. These are the kinds of results that speak to the dedication and skill of our expert team.
Frequently Asked Questions (FAQ)
Where do you even begin with a data stewardship program?
The first, non-negotiable step is a comprehensive data discovery audit. It's a simple truth: you can't protect and manage what you don't know you have. This means mapping out every data source—from EHRs and lab systems to billing platforms—and classifying data based on sensitivity, with a laser focus on identifying all Protected Health Information (PHI). This initial audit gives you the blueprint for everything that comes next, including conducting a thorough AI requirements analysis for future projects.
Isn't a data steward just another name for a data owner?
That's a common mix-up, but the roles are actually quite different, working hand-in-hand. Think of a Data Owner as the high-level executive with ultimate accountability for a specific data domain (e.g., the Chief Medical Officer owning all clinical trial data). The Data Steward is the on-the-ground expert who brings that strategy to life, managing data quality, defining business rules, and ensuring the data is usable and trustworthy. One is the general, the other is the field commander.
How can AI actually help with data stewardship?
This is where things get really interesting. AI acts as a massive force multiplier for your stewardship efforts. Modern AI tools for business can do the heavy lifting that would take a human team ages to complete. Imagine AI algorithms that automatically scan petabytes of data to classify sensitive information, proactively flag quality errors, or detect unusual access patterns that could signal a security threat. As we explored in our AI adoption guide, this operational efficiency frees up your human experts to focus on the strategic side of governance.
What is the biggest challenge in healthcare data stewardship?
The biggest challenge is often cultural, not technical. It's about shifting the organizational mindset to view data as a shared, strategic asset rather than a departmental silo. Getting buy-in from clinical staff, IT teams, and executive leadership is crucial. Overcoming this requires clear communication, demonstrating the direct benefits of good stewardship (like reduced errors and better patient outcomes), and establishing a governance framework with clear accountability.
How does data stewardship impact patient trust?
Directly and profoundly. In an era of constant data breaches, patients are more concerned than ever about their privacy. A robust data stewardship program is a clear signal that your organization takes the protection of their sensitive health information seriously. By being transparent about how data is used, ensuring its security, and using it ethically to improve care, you build a foundation of trust that is essential for long-term patient relationships.
Ready to build a robust data stewardship framework that fuels your AI ambitions? Ekipa AI can help. Our AI strategy consulting services and expert team provide the guidance needed to turn your data into a strategic asset. Get a Custom AI Strategy report to start your journey.