Boosting Clinical Operations Efficiency with AI
A practical guide for healthcare leaders on improving clinical operations efficiency with AI. Explore key bottlenecks, KPIs, and a clear implementation roadmap.
Improving clinical operations efficiency is so much more than a simple cost-cutting exercise. It's a strategic necessity for survival and growth in a healthcare system that's being stretched to its absolute limits. When you get this right, you're not just saving money; you're building a foundation for better patient outcomes, creating financial resilience, and, critically, holding onto your best clinical talent.
The Strategic Importance of Operational Excellence
Whether we're talking about clinical development or direct patient care, efficiency is the engine that drives quality. Think of it as the art of making the most of your time, your people, and your technology to deliver the best possible results. When operations are running smoothly, clinicians can spend less time on administrative tasks and more time focused on patients. Researchers can push discoveries forward faster. And the entire organization can finally achieve financial stability.
The pressure from all sides is immense. Hospital leaders are constantly juggling the need to reduce patient wait times and improve bed turnover, all without ever compromising the quality of care. At the same time, pharmaceutical executives are trying to manage increasingly complex clinical trials while being pushed to slash development timelines. In this kind of environment, small tweaks just won't cut it anymore. What's needed is a complete overhaul.
Navigating Rising Complexity
This challenge is only getting bigger, especially in the world of clinical development. Between 2010 and the early 2020s, the complexity of clinical trials skyrocketed. According to IQVIA’s Clinical Productivity Index, which measures trial output against input, the score dropped from over 15 before the pandemic to just 10.9 by 2023. This decline is a stark reminder of how longer cycle times and complicated protocols are eating away at efficiency, forcing sponsors to design smarter, leaner trials from the ground up.
This data really drives home a critical point: efficiency isn't about doing less; it's about working smarter. The real solution lies in bringing in intelligent systems and processes that can manage complexity without burning out your staff. This is exactly where targeted Healthcare AI Services can make a huge difference, giving you the tools to leapfrog from small adjustments to major gains.
"Embedding quality and safety within clinical operations is not just a goal; it's a strategic imperative. A resilient health system is built on a foundation of safety, effectiveness, timeliness, and equity—all of which are direct outcomes of operational efficiency."
The Pillars of a Modern Health System
Achieving this level of operational excellence demands a holistic approach that goes far beyond just digital tools. The physical infrastructure—the very space where care happens—is just as important.

For instance, something as seemingly simple as the right furniture can have a huge impact. Following a comprehensive guide to choosing healthcare furniture helps facilities create environments that are both ergonomic and infection-controlled, directly supporting better workflows and staff well-being. By thoughtfully combining smart technology with a well-designed physical space, healthcare organizations can build a truly efficient and safe ecosystem where every single element contributes to better outcomes.
Uncovering the Real Bottlenecks in Your Operations
If you want to improve your clinical operations efficiency, you first need to diagnose exactly where things are breaking down. This isn't about chasing the latest trend; it's about finding the specific points of friction that drain time, money, and morale. Often, these hidden drags are so baked into daily routines that they're just accepted as "the way things are."
Think about a skilled clinician spending nearly half their day fighting with a clunky EHR instead of focusing on patients. Or a critical clinical trial that grinds to a halt for months because patient recruitment is painfully slow. These aren't just abstract problems—they are expensive, everyday realities that get in the way of patient care and scientific progress.
Pinpointing these issues is the crucial first step. It's how you build a solid business case for making smart, targeted changes.
To put this in context, let's look at the most common culprits that slow down clinical teams and what they actually cost the business.
Common Clinical Operations Bottlenecks and Their Business Impact
| Bottleneck Area | Specific Challenge | Impact on Efficiency | Financial Consequence |
|---|---|---|---|
| Administrative Tasks | Manual data entry, scheduling, billing, prior authorizations. | Diverts skilled staff to low-value work, leading to burnout and high turnover. | Increases operational costs; staff turnover can cost 1.5-2x an employee's salary. |
| Data Management | Disconnected EMRs, lab systems, and trial software creating data silos. | Incomplete patient views, redundant data entry, and high risk of clinical errors. | Leads to poor decision-making, repeat tests, and potential compliance penalties. |
| Patient Recruitment | Outdated, manual processes for identifying and enrolling trial participants. | Drags out trial timelines, delaying time-to-market for new therapies. | Every day a blockbuster drug is delayed can mean over $1 million in lost revenue. |
| Regulatory Compliance | Cumbersome documentation and reporting for FDA, HIPAA, etc. | Consumes significant time and resources, pulling focus from core research activities. | Non-compliance can result in hefty fines, legal fees, and reputational damage. |
As the table shows, these aren't minor inconveniences. They are significant operational and financial liabilities that directly impact your bottom line and your ability to deliver care.
The Crushing Weight of Administrative Overload
One of the biggest drags on any clinical operation is administrative waste. We're not just talking about paperwork. It’s the endless stream of low-value, repetitive tasks that eats up the time of your most highly trained professionals.
Inside provider organizations, this friction adds up to a massive financial hit. In the US, administrative spending makes up 15% to 30% of all healthcare costs, with wasteful spending estimated between $285 billion and $570 billion every year. This burden falls right on clinical operations—from scheduling and care coordination to documentation and billing. It's why over 35% of healthcare organizations are now using automation to fix these workflows, giving clinicians their time back. You can read more about this trend and what's expected by 2025 at csicompanies.com.
This is where a solution like AI Automation as a Service provides a direct path forward, handling the manual work so your team can focus on what they do best.
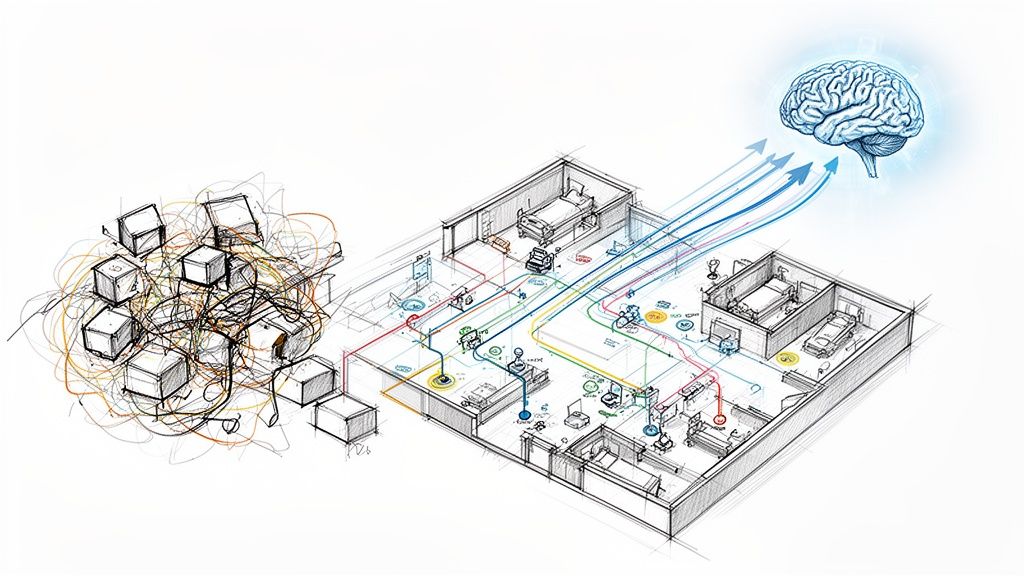
Disconnected Data and Workflow Friction
Another huge bottleneck is disconnected data. When your information systems can't talk to each other, critical data gets trapped in silos. This leads to people doing the same work twice, delayed decisions, and messy handoffs between departments.
A truly efficient clinical operation should run like a symphony orchestra—every section has to be in perfect harmony. When data is siloed, it's like the string section can't hear the woodwinds. The result is a chaotic, ineffective performance.
This data fragmentation shows up in a few key ways:
- Manual Data Re-entry: Staff waste hours copying information from one system to another, which is a recipe for errors.
- Incomplete Patient Views: Clinicians have to make decisions without the full story, which can compromise the quality of care.
- Delayed Reporting: Pulling together data for performance reviews or regulatory reports becomes a massive, time-sucking chore.
The fix is to create integrated systems that let data flow securely and freely to where it's needed. Building better internal tooling can bridge these gaps, creating a single source of truth that powers smarter and faster operations.
By tackling these two core bottlenecks—administrative overload and fragmented data—organizations can achieve major gains in their clinical operations efficiency.
How to Measure What Truly Matters
You can't fix what you can't see. In the intricate world of healthcare, the journey to better clinical operations efficiency begins with a simple, age-old principle: tracking the right metrics. These Key Performance Indicators (KPIs) aren't just numbers on a dashboard; they are the vital signs of your organization's health, telling you exactly where you’re thriving and where you need to intervene.
Without a solid baseline, any new initiative is just a shot in the dark. Whether you're overhauling a process or investing in new technology, establishing and monitoring the right KPIs gives you the hard evidence needed to justify strategic decisions and, ultimately, prove your return on investment. It's how you turn guesswork into a clear, actionable strategy.
Let’s dig into the essential metrics for both sides of the clinical coin: drug development and patient care. These are the numbers that tell the real story of your operational performance.
Key Metrics for Clinical Development
In the high-stakes, high-cost world of clinical trials, time is the most critical resource. Every delay can cost millions and, more importantly, keep life-changing therapies from the patients who need them. The following KPIs are non-negotiable for anyone serious about trial efficiency.
Trial Cycle Time: Think of this as the total time on the clock, from the moment a protocol is finalized to the second the database is locked. A shorter cycle time is a direct reflection of sharp project management, seamless site coordination, and clean data collection.
Patient Recruitment Rate: This is your enrollment speedometer—how many patients are you enrolling per month versus your target? Slow recruitment is the most notorious trial killer, and this metric tells you just how much of a problem it is, right now.
Protocol Amendment Rate: How often do you have to go back and change the trial's rulebook after it’s been set? A high number of amendments is a massive red flag, often pointing to a flawed initial design that will cause downstream delays, budget overruns, and data headaches.
These metrics give you a real-time, ground-level view of how your trials are actually performing. They help you spot friction points early, allowing your team to pivot before a small hiccup becomes a catastrophic failure.
Essential KPIs for Care Delivery
For hospitals and clinics, efficiency isn't just about the bottom line; it's about patient experience, safety, and access to care. The challenge is always to get the most out of your resources without ever cutting corners on quality. The right metrics help you walk that tightrope.
A clinician uses vital signs to assess a patient’s health. A healthcare leader must use operational KPIs to diagnose the health of their organization. A rising Average Length of Stay is like a fever—it's a clear signal that something is wrong and requires immediate investigation.
Here are the core metrics every care delivery leader should have their eyes on:
Bed Occupancy Rate: This is the percentage of your available beds that are currently filled. While a high number looks good on paper, consistently pushing 100% capacity is a sign of strain that leads to ER overcrowding and postponed surgeries.
Average Length of Stay (ALOS): This tracks how many days, on average, a patient stays in the hospital. When ALOS is low for a given condition, it’s often a sign of highly efficient care pathways, effective treatment plans, and well-oiled discharge processes.
Patient Wait Times: Simply put, how long does a patient have to wait between walking in the door and seeing a clinician? Long waits are a primary driver of patient dissatisfaction and can, in some cases, lead to worse outcomes.
Tracking these KPIs is the first step, but the real magic happens when you define them within the context of your organization’s unique goals and challenges. A Custom AI Strategy report can help you pinpoint, define, and build a framework to monitor these metrics, turning raw data into your most powerful tool for driving meaningful operational change.
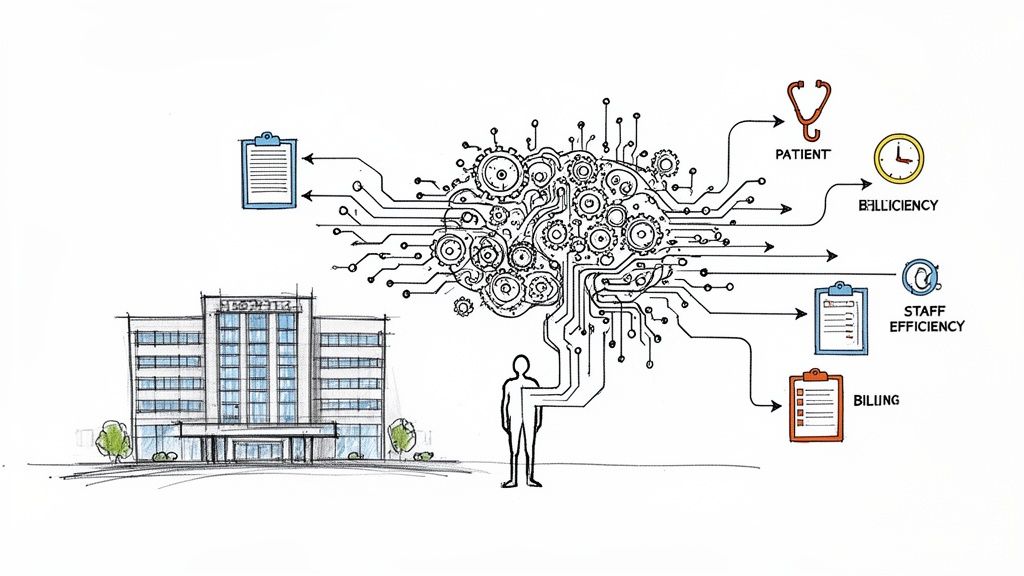
Putting AI to Work in Clinical Operations
Once you've mapped out the operational bottlenecks and know which KPIs signal success, it's time to connect those problems to real-world solutions. This is where artificial intelligence stops being an abstract idea and becomes a practical, powerful tool for improving clinical operations efficiency. It’s about being deliberate—applying the right AI technology to the specific challenges that bog down patient care and drug development.
Think of predictive analytics not as some complex algorithm, but as a crystal ball that shows you future demand in the emergency room. It allows hospitals to staff up before a surge hits, not after, dramatically cutting down patient wait times. Or picture Natural Language Processing (NLP) as a highly-trained scribe who automates clinical notes, giving doctors back the precious hours they currently spend on paperwork. These aren't far-off possibilities; they're happening right now.
The trick is to match the technology to the task. Machine learning can pinpoint the perfect patient profiles for a clinical trial, and intelligent automation can take over the mind-numbing, repetitive tasks that cause good people to burn out. By deploying targeted AI solutions, you can transform operational headaches into sources of genuine strength.
High-Impact AI Applications
Let's get specific. Here’s how different AI applications can tackle the exact operational challenges we’ve been discussing. Each one creates a direct line to improving the KPIs that matter most, from shrinking trial timelines to reducing a patient's average length of stay.
Predictive Analytics for Patient Flow: Hospitals can feed historical admissions data, local health trends, and even weather forecasts into a machine learning model to get an accurate read on upcoming patient surges. This foresight allows them to allocate resources proactively, preventing ER overcrowding and ensuring beds are ready when needed. The result is a direct, positive impact on Bed Occupancy Rate and Patient Wait Times.
NLP for Documentation Automation: A huge chunk of any clinician's day is eaten up by documentation. NLP-powered tools can actually listen to a conversation between a doctor and patient and automatically draft the structured clinical notes. This frees up clinicians to be fully present with their patients, cuts down on the administrative load, and leads to more accurate data. A great example of this in action is the Clinic AI Assistant, a tool designed to do exactly that.
Machine Learning for Trial Recruitment: One of the biggest drags on clinical development is finding the right patients. AI algorithms can sift through millions of electronic health records in minutes to find eligible candidates—a job that would take a human team months. This massively speeds up the Patient Recruitment Rate and gets trials off the ground faster.
These are just a handful of the many compelling real-world use cases where AI is delivering tangible, measurable results.
From Theory to Operational Reality
Putting these technologies into practice requires a smart combination of technical skill and a gut-level understanding of how a clinic or hospital actually works. Building effective internal tooling isn’t just about programming; it's about designing systems that clinicians find so useful they can't imagine going back. The goal is simple: create intuitive tools that enhance human expertise, not try to replace it.
To see the direct impact, let’s compare the old way with the new.
The table below gives a snapshot of how specific AI technologies solve some of the most stubborn challenges in clinical operations.
AI Solutions for Top Clinical Operations Challenges
| Operational Challenge | Traditional Approach | AI-Powered Solution | Expected KPI Improvement |
|---|---|---|---|
| ER Overcrowding | Reactive staffing based on current volume; manual bed management. | Predictive analytics forecasts patient arrivals, optimizing staff and bed allocation. | 15-20% reduction in Patient Wait Times; improved Bed Occupancy Rate. |
| Slow Trial Recruitment | Manual chart review and site-based outreach to find eligible patients. | Machine learning scans EHRs to identify ideal candidates in real-time. | Up to 50% faster Patient Recruitment Rate; shorter Trial Cycle Time. |
| Clinical Burnout | Hiring more administrative staff; accepting documentation as a necessary burden. | NLP automates note-taking and administrative tasks, freeing up clinician time. | Increased clinician satisfaction; improved data accuracy and completeness. |
It's clear that AI provides a much smarter, more proactive way of working.
The true value of AI in clinical operations isn't just automation; it's augmentation. It empowers highly skilled professionals by removing friction, providing intelligent insights, and allowing them to operate at the absolute top of their license.
Ultimately, putting AI to work is all about building a more intelligent, responsive healthcare system. It requires a thoughtful selection of AI tools for business that are suited to the unique needs of your organization. When you get it right, these systems do more than just improve numbers on a spreadsheet—they lead to better patient outcomes and create a more sustainable, rewarding environment for the people on the front lines.
Your Step-by-Step AI Implementation Roadmap
Bringing AI into your clinical operations to boost efficiency can feel like a huge undertaking. But you don't have to boil the ocean. A smart, structured approach breaks the journey down into smaller, more manageable steps. The trick is to start small, show a clear win, and then scale up intelligently, as we explored in our AI adoption guide.
This five-step process is a practical guide for healthcare leaders. It's designed to make sure every move you make is strategic, measurable, and tied directly to what matters most to your organization. It turns the big, scary idea of "AI adoption" into a real, achievable project.
Step 1: Strategic Assessment and Goal Setting
First things first: what problem are you actually trying to solve? This isn't about chasing shiny new tech. It's about fixing specific, costly issues that are holding you back. Start by taking a hard look at your operations to find the biggest bottlenecks we've discussed. Are patient wait times killing your satisfaction scores? Is paperwork burying your clinicians?
Once you've zeroed in on the core challenges, set goals you can actually measure. For example, a great goal isn't "improve scheduling," but "reduce patient no-show rates by 15% within six months." Or, "cut down time spent on clinical documentation by 30% by the end of the year." This clarity gets everyone on the same page and gives you a clear finish line to aim for.
Step 2: Prioritizing High-Impact Pilot Projects
With your goals locked in, resist the temptation to fix everything at once. Pick one or two projects that offer the biggest bang for your buck with the lowest initial complexity. A perfect pilot project tackles a problem everyone recognizes, has a simple metric for success, and can deliver a quick, visible win.
A great example is using an AI-powered tool for patient scheduling, such as an AI Strategy consulting tool. It’s a common headache, the return on investment is easy to see (fewer no-shows, fuller schedules), and it quickly shows both your staff and leadership what this technology can do. These early wins are absolutely essential for getting the buy-in you'll need for bigger, more ambitious projects down the road.
Step 3: Ensuring Data Infrastructure Readiness
AI runs on data. Simple as that. Before you can even think about deploying a solution, you have to get your data house in order. This means your data must be clean, easy to access, and secure. I've seen too many AI projects hit a wall, not because the algorithm was wrong, but because the data was a complete mess—stuck in different systems, full of errors, or just plain incomplete.
This stage is all about:
- Data Auditing: Figure out where your most important data lives and get an honest assessment of its quality.
- Integration: Build secure bridges so data can flow smoothly between your EHR, billing systems, and scheduling platforms.
- Governance: Establish crystal-clear rules for data privacy and security, making sure you’re staying compliant with HIPAA and other regulations.
This groundwork isn't glamorous, but it's non-negotiable. It's like putting high-octane fuel in a race car—it ensures your AI tools have what they need to perform at their peak.
Step 4: Running a Pilot Program to Prove Value
Now it's time for the test drive. Run your chosen solution in a controlled environment, like with a single department or clinical team, for a set period—maybe 90 days. The entire focus here is on collecting hard data and real-world feedback.
This simple flow is the heart of any AI problem-solving effort: you spot a challenge, apply a targeted AI solution, and measure how your key metrics improve.
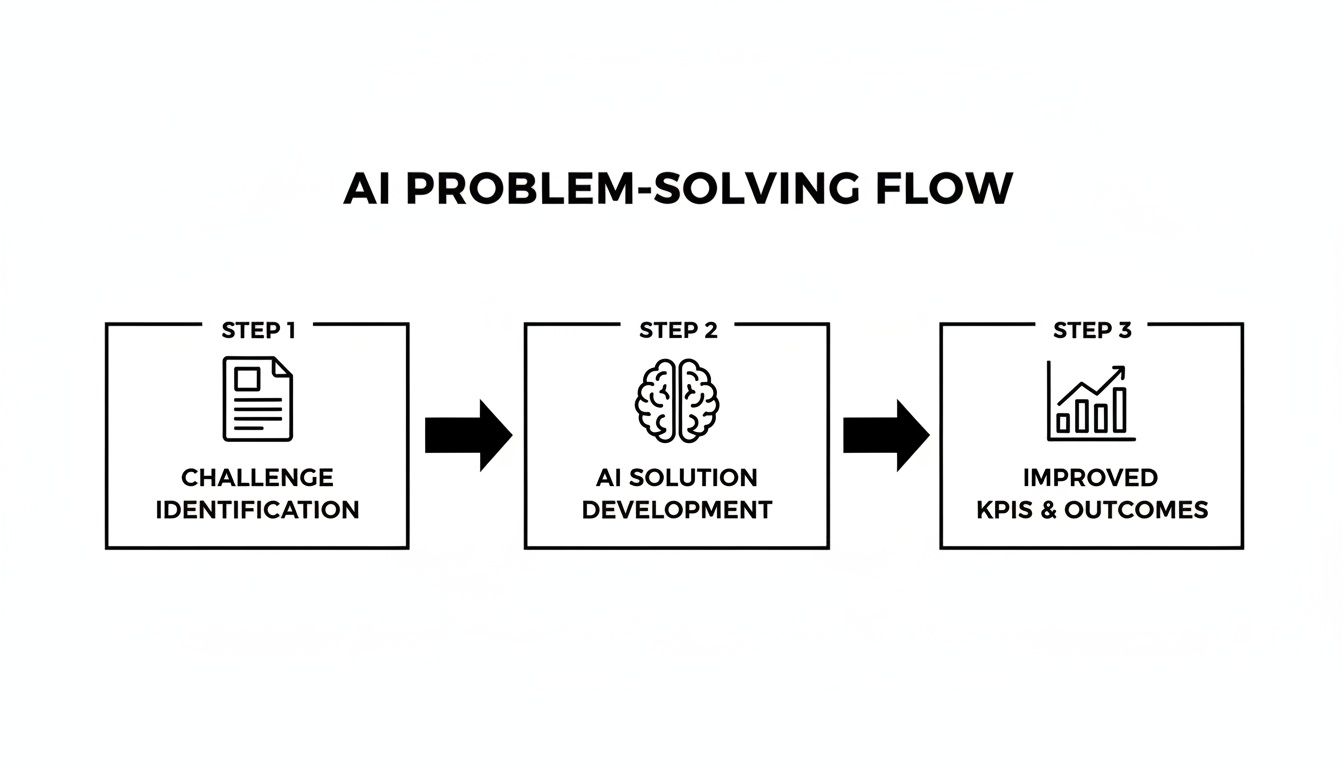
Keep a close eye on the KPIs you defined back in Step 1. But just as important, talk to the staff using the new tool. Is it easy to use? Does it actually make their day better? This feedback is pure gold. It helps you tweak the solution and your entire implementation plan. To make sure your pilot is set up for success, it can be helpful to work with partners who offer specialized AI consulting services.
Step 5: Scaling Successful Initiatives
Once your pilot delivers clear, positive results, you've got a success story on your hands. Now it’s time to take what works and scale it across the organization. This isn't just a technical rollout; it requires a smart change management plan.
Use the great results and glowing reviews from your pilot team to build excitement and calm any nerves in other departments. Following a structured AI Product Development Workflow ensures the process is repeatable and causes minimal disruption. Invest in great training and be there with ongoing support so your staff feels confident, not threatened, by the new tools. This roadmap helps you de-risk your investment and build a true culture of improvement.
The Real-World Payoff of Operational Excellence
Improving clinical operations efficiency isn't just about tweaking processes on a whiteboard. It delivers powerful, tangible results that matter to everyone, from the nurses on the floor to the executives in the boardroom. A smart strategy doesn't just save a few dollars; it leads directly to better, safer care for patients and builds a stronger, more resilient healthcare organization. This is where operational tweaks save lives.
When you iron out the wrinkles in your clinical processes, the whole system just works better. You see fewer medical errors, patient safety scores go up, and most importantly, more people survive. It proves that efficiency and clinical excellence are two sides of the same coin. For the C-suite, the financial wins are undeniable—lower operating costs, less waste, and the ability to care for more patients create a compelling reason to invest.
From Cost Savings to Better Patient Outcomes
The true test of operational excellence in healthcare is its effect on people's lives. The latest data paints a pretty clear picture. Initiatives aimed at improving safety and efficiency between April 2024 and March 2025 are on track to have saved over 300,000 additional lives.
At the same time, hospitals handled a 4% jump in patient volume and a 5% increase in how complex those cases were. This shows they're doing more with what they have. By the second quarter of 2025, patients in hospitals were nearly 30% more likely to survive than experts predicted, directly linking these operational gains to saving lives. You can read more about these performance improvements from Vizient.
These aren't just numbers on a page; they're real wins driven by systematic changes. Organizations that truly commit to this are doing more than just tidying up their workflows—they are fundamentally getting better at delivering top-notch care, even when things get tough.
The Financial Case for Making the Investment
While saving lives is always the primary goal, the financial benefits are what get these projects the green light from leadership and fund the next wave of improvements. A highly efficient clinical operation is, without fail, a financially healthy one.
Here’s where the money part really clicks:
- Slashed Operational Costs: Automating tasks and optimizing how work gets done cuts down on administrative bloat and eliminates redundant steps.
- Increased Patient Capacity: When patient flow is smooth and stays are shorter, hospitals can treat more people without adding more beds.
- Lower Staff Turnover: Taking the administrative weight off your clinical team reduces burnout, which in turn cuts the massive costs tied to recruiting and training new staff.
These financial gains create a positive feedback loop. The money saved can be plowed back into better technology, upgraded facilities, and new patient care programs. This is where investing in tools like custom healthcare software development becomes so critical. It lets organizations build solutions that zero in on their specific bottlenecks, making sure every dollar spent on tech delivers a real, measurable return.
Frequently Asked Questions
Where Do We Even Begin with AI in Our Clinic?
The best place to start is small. Before you get tangled up in complex technology, take a hard look at your daily operations and find the single biggest headache. Is it the endless back-and-forth of patient scheduling? Or maybe the time sink of manual documentation?
Pick one high-impact, low-complexity problem and run a pilot project. A focused AI requirements analysis can help you pinpoint that perfect starting point. This approach is all about getting a quick win, which builds the confidence and momentum you'll need for bigger projects down the road.
How Can We Actually Measure the Return on Investment for AI?
Measuring ROI is about looking at both the numbers you can count and the improvements you can feel.
On one hand, you have the "hard" metrics:
- Direct cost savings from automating administrative tasks.
- Reduced length of stay for patients.
- Increased number of patients you can see each day.
On the other, you have the "soft" metrics, which are just as important:
- Higher staff morale and lower turnover.
- Fewer preventable medical errors.
- Better patient health outcomes and satisfaction.
The key is to track these KPIs before and after you introduce any new technology. A Custom AI Strategy report can give you a clear framework for defining what to measure and how to track it.
Do My Doctors and Nurses Need to Become Tech Experts to Use AI?
Absolutely not. The goal of great AI is to feel invisible. The best AI tools for business are designed to fit right into the workflows your team already uses, with simple, intuitive interfaces.
Think of it as giving your staff a smart assistant that handles the tedious, repetitive work. This frees up your highly skilled professionals to focus on what truly matters: making critical decisions and providing excellent patient care. The right AI solutions should empower your team, not burden them. If you're curious about how this works in practice, feel free to connect with our expert team.
At Ekipa AI, we see operational challenges not as problems, but as opportunities for real growth and efficiency. Our AI strategy consulting services are designed to give you a clear, practical roadmap for transforming your clinical operations. Learn more about the people behind our innovations by meeting our expert team.