A Practical Guide to Your Healthcare Process Automation Strategy
Build a successful healthcare process automation strategy with our guide. Learn to justify ROI, prioritize use cases, and implement a phased roadmap.
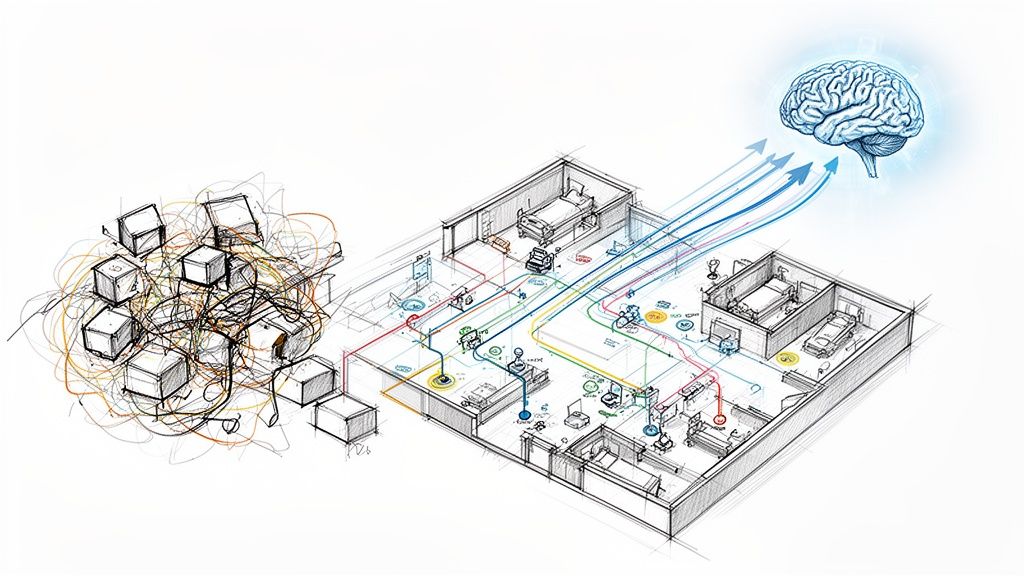
A healthcare process automation strategy isn't just about buying software. It’s a complete game plan for overhauling how your organization works, from the front desk to the back office. The real goal is to use technology to solve the big problems: improving patient care, easing the burden on your staff, and getting a handle on rising operational costs.
Think of it as creating an intelligent, connected system for your entire organization, rather than just implementing a few scattered AI tools for business.
Defining Your Healthcare Automation Strategy
A modern healthcare process automation strategy leaves behind the old approach of putting a bandage on process problems. Instead of deploying a single bot for one repetitive task, it’s about building a unified system that connects clinical, financial, and administrative functions.
It's like building a central nervous system for your hospital or clinic. Information flows where it's needed automatically, instead of relying on slow, manual "reflexes." This integrated approach is what it takes to tackle the immense pressures facing the industry today.
This shift demands that every technology investment is directly tied to your organization's most important goals. We're not automating for the sake of automation; we're automating to see real, measurable improvements in care quality and operational health. At Ekipa, we specialize in building these foundations through our expert Healthcare AI Services.
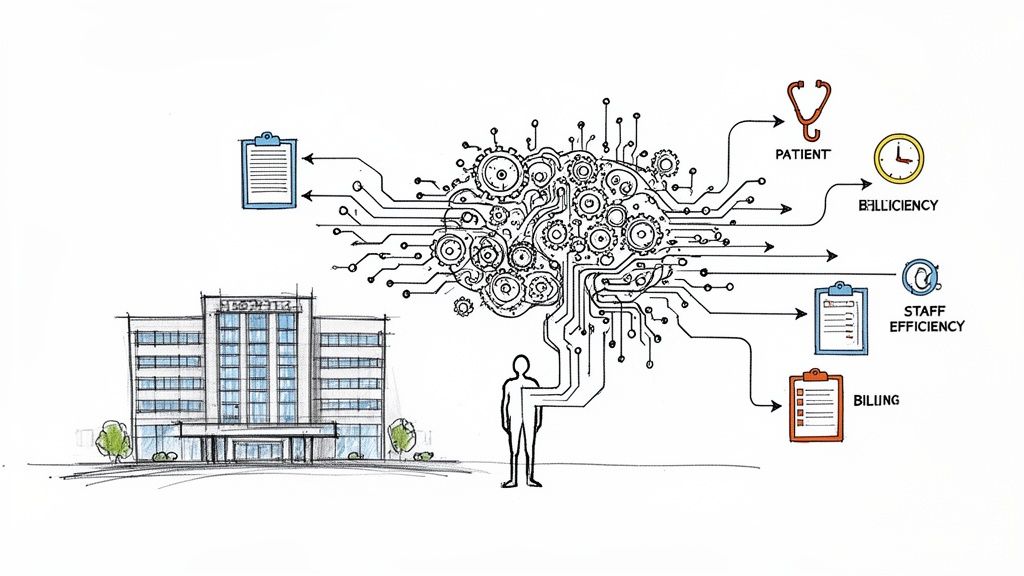
Core Components of a Modern Strategy
A solid strategy is built on a few essential, interconnected pillars. Each one supports a different part of the healthcare ecosystem, from how patients are managed to how the bills get paid. Getting a handle on these components is the first step to creating a plan that actually works.
The table below breaks down the essential pillars of a successful strategy, showing how they fit together to drive improvements across the entire organization.
Core Components of a Modern Healthcare Automation Strategy
| Pillar | Objective | Key Technologies | Primary Business Impact |
|---|---|---|---|
| Process Optimization | Redesign inefficient workflows before automating them. | Process Mining, Task Mining, Business Process Management (BPM) | Reduces waste, eliminates bottlenecks, and creates a solid foundation for automation. |
| Technology Integration | Ensure new tools work seamlessly with existing systems (EHR, billing). | APIs, Integration Platforms (iPaaS), Robotic Process Automation (RPA) | Creates a single source of truth, avoids data silos, and improves data flow. |
| Data Governance & Security | Protect patient data and maintain strict compliance. | Data Encryption, Access Control Systems, AI-powered Threat Detection | Ensures HIPAA compliance, builds patient trust, and prevents costly data breaches. |
| Change Management | Prepare and support staff for new, technology-enabled ways of working. | Training Platforms, Communication Tools, User Adoption Monitoring | Increases ROI, boosts staff morale, and ensures the technology is actually used. |
By building a strategy on these core components, you ensure that every automation project, no matter how small, contributes to the bigger picture.
Moving Beyond Isolated Tasks
The real magic of a healthcare process automation strategy happens when you connect functions that used to operate in silos.
For instance, automating patient intake can do a lot more than just speed up form-filling. When it’s integrated properly, that single action can instantly trigger an insurance eligibility check, update the patient’s clinical record in the EHR, and notify the right care team that the patient has arrived—all at once. That kind of seamless coordination is simply impossible with disconnected tools.
By looking at entire end-to-end processes, healthcare organizations can find massive opportunities for improvement. To see how these principles translate into real-world results, it’s helpful to explore practical guides on healthcare workflow automation that show tangible benefits.
Ultimately, a well-executed strategy changes how work gets done across every department, freeing up your team to focus on what matters most: the patient.
Moving From Siloed Tools to Integrated Platforms
For years, the go-to approach for automation in healthcare was to find a single tool to fix a single problem. The billing department would get its own software, patient scheduling would use something else, and clinical teams operated in yet another system. This created a bunch of digital islands, or data silos, where critical information was trapped. The result? No real, system-wide efficiency gains.
A modern healthcare process automation strategy demands a complete pivot from this disjointed model. The real goal is to build a cohesive, connected ecosystem where data flows freely and securely between all your systems. It's like ditching a bunch of disconnected walkie-talkies for a fully integrated communications network that covers the entire organization.
This kind of deep connection is what makes true end-to-end automation possible. Imagine a patient rescheduling an appointment. In an integrated system, that one action can automatically trigger insurance verification, update the Electronic Health Record (EHR), and notify the right clinical team—all without a single person having to lift a finger. That level of orchestration is simply impossible when your tools can't talk to each other. This is often achieved through custom healthcare software development that prioritizes integration.
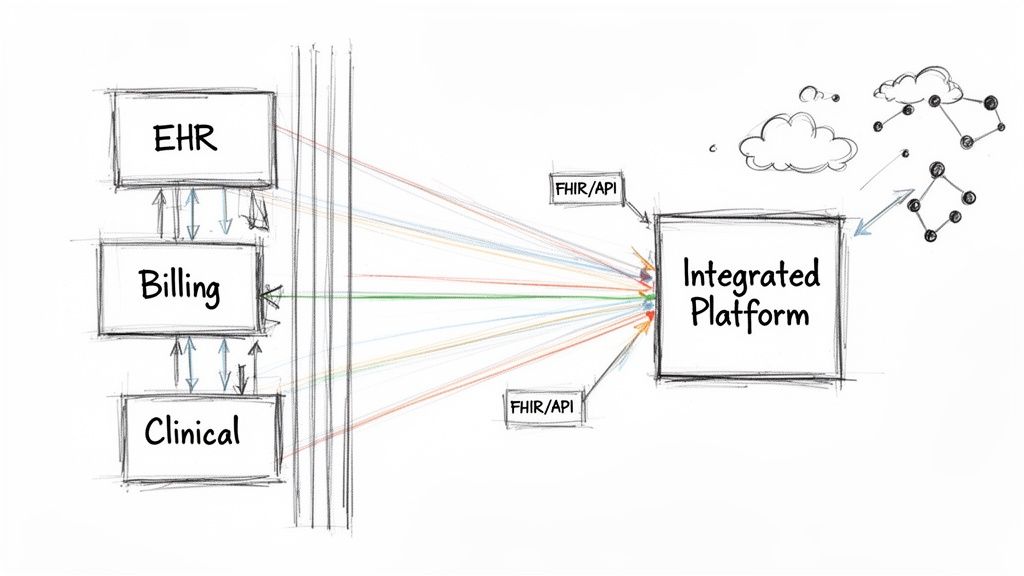
The Central Role of Interoperability
At the very core of this integrated vision is interoperability—the ability for different software and IT systems to communicate, swap data, and actually use the information they've exchanged. If you don't have it, your automation efforts will always be stuck in first gear, limited in both scope and impact.
This is where a few non-negotiable technical standards come into play.
- Fast Healthcare Interoperability Resources (FHIR): Think of FHIR as the universal translator for healthcare data. It standardizes data formats and provides an Application Programming Interface (API) for exchanging electronic health records.
- Application Programming Interfaces (APIs): These are the digital handshakes that let different systems connect and share information securely in real time.
When you build your strategy on these standards, you create what's known as "data liquidity." It means patient info, billing codes, and clinical notes can move from one system to the next without a hitch. This is the bedrock of any automation plan that's built to last.
A New Standard for Technology Procurement
This shift toward integration is completely changing how healthcare organizations buy new technology. A recent global survey drove this point home, revealing that 84% of healthcare organizations are done digitizing "one department at a time." Instead, they're standardizing on end-to-end architectures that connect everything.
The same study found that a staggering 92% of leaders now rank FHIR/API interoperability as a top-three criterion when buying new platforms. Why? Because effective automation now depends entirely on data liquidity across scheduling, clinical, financial, and even supply chain processes.
This isn't just a trend; it's a fundamental change. Deep integration is no longer a "nice-to-have" feature—it's a core requirement for survival and growth. As organizations make this transition, exploring tools like no-code automation platforms can give teams the power to build and connect workflows without needing a deep bench of developers. The focus has moved from flashy standalone features to one simple question: how well does this new tool plug into everything else we already have? It’s about making sure every new piece of tech strengthens the entire ecosystem, rather than just creating another data silo.
Building a Business Case That Gets the Green Light
Getting executives to sign off on your healthcare process automation strategy means you have to speak their language. This isn't just another IT project; it's a financial move. Your job is to draw a straight line from the investment to the bottom line with a business case that’s packed with hard data.
Leave the technical jargon at the door. The conversation needs to be about value—clear, tangible outcomes like cutting costs, getting more from your team, and boosting revenue. It’s all about proving how smart automation builds a stronger, more profitable healthcare organization.
Pinpointing What the C-Suite Actually Cares About
When you're making your pitch, you need to focus on the metrics that keep leadership up at night. Vague promises about "improved efficiency" are dead on arrival. Instead, build your case around solid, measurable gains in three key areas.
-
Slash Costs by Standardizing Work: Think about all the repetitive, manual work that happens every day—data entry, claims processing, patient scheduling. Automating these tasks creates a standard, predictable workflow. Not only does this cut down on human error, but it also drastically reduces the labor hours spent on administrative grunt work.
-
Optimize Your Workforce with Smart Analytics: Automation frees your highly skilled people from mind-numbing tasks so they can focus on what they do best: patient care. You can also use predictive analytics to get staffing levels right based on patient demand, which helps you avoid both costly overstaffing and staff burnout.
-
Boost Revenue Through Better Patient Engagement: Simple tech tools can have a huge impact. Automated appointment reminders, remote patient monitoring, and easy digital payment options all make for a better patient experience. This translates directly to fewer no-shows, better patient retention, and getting paid faster.
This isn't just a theory; it's where the industry is headed. Deloitte's 2026 Global Health Care Outlook found that 64% of leaders see AI as a way to cut costs by automating workflows, and 55% see savings in workforce optimization. With leaders planning to pour nearly 19% of their tech budgets into AI, the pressure is on to show real results.
Calculating Your ROI and Defining Success
A solid business case needs credible financial projections. You don't need to predict the future, but you do need a clear method for estimating the return. A great place to start is by calculating the "cost of doing nothing"—the money you're losing every single day because of slow, manual processes.
The most compelling business cases don’t just talk about future gains; they expose current losses. When you frame the problem as a daily financial leak, you create a powerful sense of urgency to fix it.
Next, you need to define exactly how you'll measure success. These are your Key Performance Indicators (KPIs), and they must be specific, measurable, and tied directly to the value you promised.
Sample KPIs for Healthcare Automation
| Value Driver | Key Performance Indicator (KPI) | How to Measure It |
|---|---|---|
| Cost Reduction | Claim Denial Rate | The percentage of claims rejected by payers each month. |
| Average Cost per Claim | Total cost of your billing department divided by the number of claims processed. | |
| Workforce Optimization | Staff Overtime Hours | The number of overtime hours your administrative staff logs per pay period. |
| Employee Turnover Rate | The percentage of administrative staff who leave the organization each year. | |
| Revenue Enhancement | Days in Accounts Receivable (A/R) | The average time it takes to collect on payments owed to you. |
| Patient No-Show Rate | The percentage of appointments where the patient doesn't show up. |
To keep an eye on these numbers, you need the right tools. For example, a financial insights dashboard is crucial for tracking your revenue cycle in real time. When you can present this kind of clear, undeniable data, your business case practically makes itself.
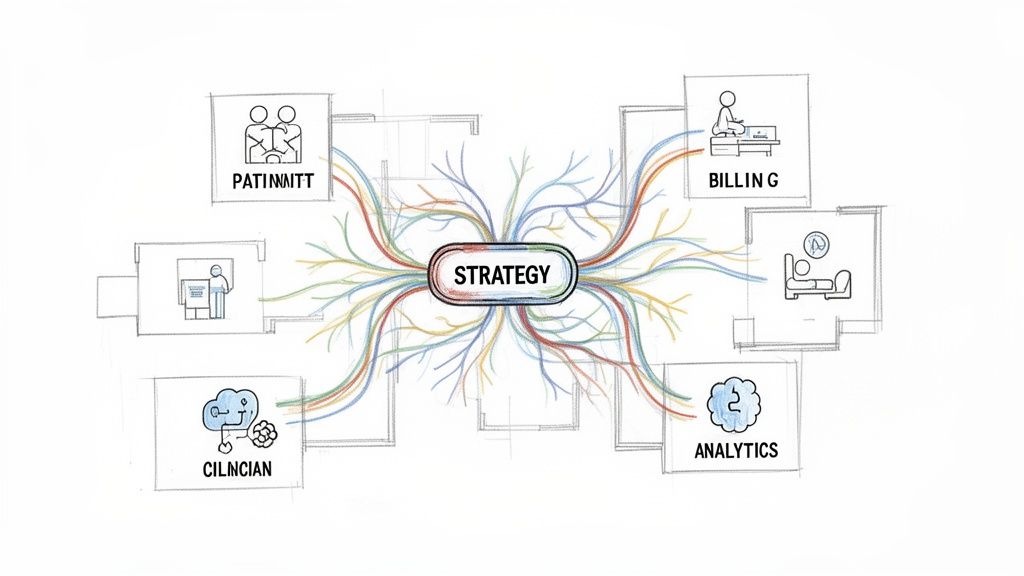
Alright, you've decided to move forward with a healthcare process automation strategy. That's a huge step. But now comes the million-dollar question: where do you actually begin?
The list of potential projects can feel endless, stretching from the moment a patient checks in to the day their final payment is collected. It's tempting to chase after quick, easy wins, but that's a recipe for scattered results. The real key is a disciplined selection process that puts high-impact use cases at the front of the line.
A structured approach keeps you from spreading your resources too thin. It ensures your first automation projects deliver clear, measurable value—the kind of value that builds excitement and momentum for the entire program. Think of it like building an investment portfolio; you want to start with the "blue-chip" opportunities that promise the most reliable returns.
This is where a solid AI requirements analysis is worth its weight in gold. It helps you sift through that long list of possibilities and zero in on a handful of top priorities by measuring each potential project against your core business goals. To make this easier, I find it helps to group automation opportunities into three main areas.
Revenue Cycle Management (RCM)
For most healthcare organizations, this is the best place to start. Why? Because the ROI is incredibly direct and easy to measure. The entire revenue cycle is packed with repetitive, rules-based tasks that are practically begging to be automated. Every inefficiency here hits your cash flow directly, which makes any improvement a top priority.
Analysts estimate that automating key RCM functions like claims management, prior authorizations, and coding could free up as much as $360 billion in annual savings across the U.S. health system. It’s no surprise that revenue cycle leaders now rank automation as their number-one investment. You can dig into some of the latest RCM trends to see just how big this opportunity is.
High-impact RCM use cases include:
- Automated Prior Authorization: Using AI to automatically submit requests and check their status. This dramatically cuts down on the frustrating delays and endless manual follow-up.
- Intelligent Claim Scrubbing: Deploying AI to check claims for errors against payer rules before they're even submitted, which is a game-changer for reducing denial rates.
- Automated Payment Posting: Instantly posting payments from Electronic Remittance Advice (ERA) files to speed up reconciliation and improve cash flow.
Clinical Operations
While the financial returns in clinical operations might not be as black-and-white, the impact on care quality and staff morale is enormous. Automating clinical tasks frees up doctors and nurses from soul-crushing administrative work, letting them focus on what they do best: taking care of patients.
Automation in a clinical setting isn't about replacing clinicians. It's about removing the friction that leads to burnout and giving them better tools to do their jobs.
Consider these powerful opportunities:
- Simplified Clinical Documentation: Using ambient AI scribes that listen to and automatically summarize patient conversations. This can slash the time spent on EHR data entry.
- Automated Patient Triage: Implementing intelligent chatbots to handle initial patient questions, gather symptoms, and guide them to the right level of care.
- Lab Result Routing: Automatically sending test results to the correct physician and flagging critical values that need immediate attention.
Back-Office Administration
Don't forget the administrative functions that keep your organization running—HR, finance, and IT. These departments are often buried in standardized, high-volume work, making them perfect candidates for intelligent systems that can run 24/7 without making mistakes. As we explored in our AI adoption guide, improving these internal workflows is a critical step in building a more agile organization.
A few high-value back-office examples:
- HR Onboarding and Credentialing: Automating the entire process of bringing on a new clinician, from background checks and credential verification to getting them system access.
- Automated Invoice Processing: Using AI to read, categorize, and approve invoices, making sure vendors are paid on time while cutting down on manual work for the finance team.
- IT Help Desk Support: Deploying AI-powered chatbots to handle common IT requests like password resets. This frees up your IT staff for more complex problems.
By sorting and evaluating opportunities within these three domains, you can build a balanced, strategic roadmap. It's always helpful to explore real-world use cases to see how these ideas are already delivering tangible results for other organizations. This structured thinking ensures your healthcare process automation strategy gets off to a strong start and delivers value for years to come.
Designing Your Phased Implementation Roadmap
A successful healthcare process automation strategy isn't a massive, one-time project. It’s a journey. Trying to automate everything at once is a surefire way to overwhelm your teams and grind everything to a halt. Instead, a phased implementation roadmap is your best bet for building momentum, managing risk, and making sure every step delivers real, tangible value.
This approach lets you score early wins, learn from what’s working (and what’s not), and build a solid foundation for wider adoption. It breaks a daunting initiative down into a series of manageable, value-driven milestones.
This infographic breaks down the typical four-phase flow of a strategic automation roadmap.
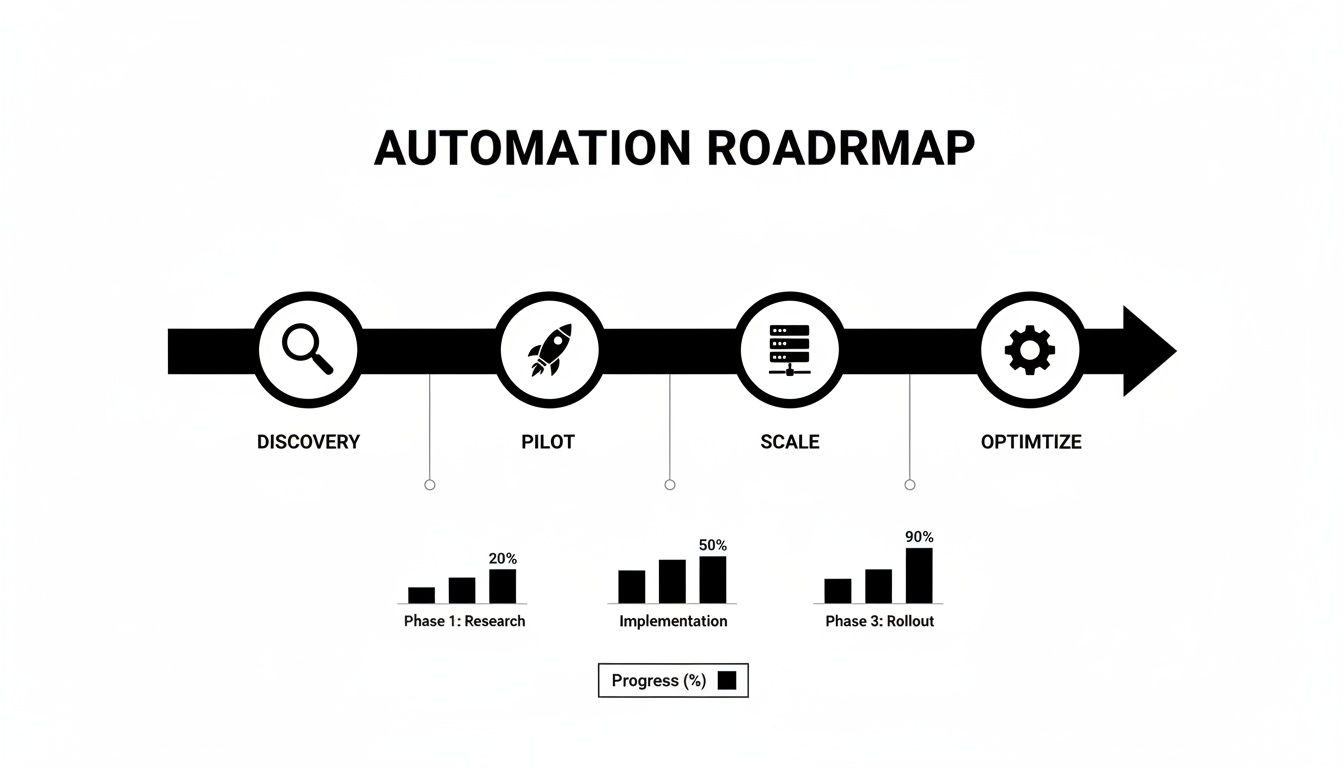
As you can see, it’s a progressive path, starting with deep analysis in the discovery phase and moving toward constant improvement in the optimization stage.
Phase 1: Discovery and Strategy (1-2 Months)
This first phase is all about understanding the lay of the land before you start building. Your main goal here is to find and prioritize the automation opportunities that actually line up with your organization's big-picture goals. This is where a deep AI requirements analysis is worth its weight in gold.
Key activities in this phase include:
- Stakeholder Workshops: Get clinical, administrative, and IT leaders in the same room to define what success looks like and agree on the goals.
- Process Mining: Use specialized tools to map out your current workflows—from patient intake to billing—and pinpoint the real bottlenecks and inefficiencies.
- Use Case Prioritization: Evaluate potential automation projects based on their potential impact, how feasible they are to implement, and their likely ROI. This gives you a clear, data-backed shortlist to start with.
The main takeaway from this phase is a strategic roadmap document. This plan, often developed with the help of AI strategy consulting, will outline your first pilot project and give you a high-level view of the phases to come.
Phase 2: Pilot and Proof-of-Concept (2-4 Months)
Once you’ve picked a high-impact use case, it’s time to prove its value on a small, controlled scale. A pilot project is essential for showing the technology works and building confidence among everyone involved. You’re looking for a quick, decisive win.
Think of the pilot as a clinical trial for your automation strategy. It’s a low-risk environment where you can test your hypothesis, gather data, and prove the solution works as intended before you prescribe it to the entire organization.
Success here is all about hitting clear, predefined KPIs. For a pilot focused on revenue cycle management, that might mean achieving a 15% reduction in claim denials for one department or posting payments 20% faster. Our AI Product Development Workflow provides a structured framework to get these critical pilot projects across the finish line.
Phase 3: Scaled Implementation (6-12+ Months)
With a successful pilot under your belt, it's time to expand. This phase is all about taking the lessons you learned from the proof-of-concept and applying them to broader departments or processes. This could mean rolling out automated prior authorizations across all your specialty clinics or deploying internal tooling for HR onboarding across the entire hospital system.
A few key things to keep in mind here:
- Technical Scalability: You have to be sure your IT infrastructure can handle the increased volume of transactions and data.
- Comprehensive Training: Develop and deliver solid training programs so your staff feels comfortable and proficient with the new tools and workflows.
- Change Management: Be transparent about the changes, listen to and address employee concerns, and consistently highlight how these new systems will make their daily work better.
Phase 4: Continuous Optimization (Ongoing)
Automation isn't something you just "set and forget." This final, ongoing phase is all about continuous improvement. Healthcare regulations change, new technologies pop up, and your organization's needs will evolve. Your strategy has to adapt, too. This is where a model like AI Automation as a Service can be incredibly helpful.
Activities in this phase include keeping an eye on performance dashboards, regularly gathering user feedback, and always looking for new opportunities to automate. By creating a cycle of evaluation and refinement, you ensure your healthcare process automation strategy stays effective and keeps delivering value long after the initial rollout.
Partnering for Success on Your Automation Journey
Think of your healthcare process automation strategy not as a destination you arrive at, but as a continuous journey of improvement. It all starts with building a rock-solid business case, then moves into picking the right high-impact processes to automate, and finally comes to life through a carefully planned, phased roadmap.
But let's be honest—this path is littered with challenges unique to healthcare.
You're not just plugging in new software. You're navigating a maze of data integration, iron-clad regulatory compliance, and significant organizational change. This requires more than just good technology; it demands real-world industry expertise from a partner who truly understands what’s at stake. In a field where patient outcomes and data security are everything, the right guidance isn't a luxury, it's a critical factor for success.
Why an Expert Partner Is Essential
Going it alone on a major automation initiative can be a recipe for costly mistakes. You might pick the wrong technology stack or, just as damaging, fail to get your staff to embrace the new way of working. A strategic partner is like a guide and a co-pilot, helping you sidestep these pitfalls.
Here’s what they bring to the table:
- Accelerate Time-to-Value: Why reinvent the wheel? A good partner brings proven frameworks and even pre-built solutions to the table, meaning you see a return on your investment much faster.
- Mitigate Compliance Risks: They ensure every automated workflow is built from the ground up with HIPAA and other critical regulations baked right in. No afterthoughts, no expensive fixes down the line.
- Drive User Adoption: They know how to implement change management that actually works, getting your clinical and administrative teams not just to use the new tools, but to champion them.
This is about more than just efficiency; it's about fundamentally changing how care is delivered and how your organization functions. The right partner doesn’t just hand you powerful AI solutions; they provide the strategic wisdom to make sure that change is successful and sustainable.
We do more than just sell software. We deliver the deep expertise and hands-on implementation support you need to turn your vision into a scalable, compliant, and genuinely impactful reality. Our proven AI Product Development Workflow is designed to manage your projects effectively, from the first pilot program all the way to a full-scale rollout.
Your automation journey is a unique reflection of your organization's specific goals and challenges. Let's talk about how we can build a strategy that fits you perfectly. Connect with our expert team today to start the conversation.
Frequently Asked Questions (FAQ)
Diving into a healthcare process automation strategy always kicks up a few questions. Let's tackle some of the most common ones we hear from healthcare leaders just like you.
Where Do We Even Begin? What’s the First Step?
Before you automate anything, you have to know exactly what’s broken. The very first step is to take a hard, honest look at your current workflows.
Pinpoint the real bottlenecks. Where are things getting stuck? Think about patient intake, the billing cycle, or even how clinical notes are managed. Find those repetitive, soul-crushing tasks that burn out your staff and create delays. This discovery phase is everything—it shows you precisely where automation will give you the biggest and fastest win.
Getting an outside perspective can be a game-changer here. Expert AI strategy consulting helps you cut through the noise and build a roadmap based on solid data, not just gut feelings.
How Do We Actually Measure if This is Working?
Measuring the success of your healthcare process automation strategy isn't just about dollars and cents. You need to look at both the hard numbers and the human impact to get the full story.
-
The Hard Numbers (Quantitative KPIs): These are the metrics your CFO will love. Track direct cost savings from less manual work, watch your claim denial rate drop, and measure how quickly you’re getting paid (a shorter revenue cycle).
-
The Human Impact (Qualitative KPIs): These are just as crucial. Are your patient satisfaction scores climbing? Is employee burnout decreasing? Is your data finally accurate and reliable across different systems?
The key is to define what success looks like before you start. Set your benchmarks on day one, so you know exactly what you're aiming for.
What Are the Biggest Roadblocks We’re Likely to Face?
The toughest challenges usually pop up in three areas: wrestling with data, managing people, and navigating compliance.
First, healthcare data is notoriously messy and locked away in old, stubborn systems. Getting these different platforms to talk to each other is often the biggest technical headache.
Next, you have the human element. People are creatures of habit, and you can’t just drop a new tool on their desk and expect them to love it. A solid change management plan is non-negotiable if you want people to actually use the new system. And finally, every single thing you do with AI solutions must be HIPAA compliant. Protecting patient data has to be baked into the design from the very beginning.
Should We Build This Ourselves or Find a Partner?
This is the classic "build vs. buy" debate. The right answer really comes down to your organization's internal skills, budget, and long-term vision.
Building your own custom solutions or internal tooling gives you total control, but it's a massive undertaking. It demands a huge investment in specialized talent, time, and money—resources most healthcare providers would rather dedicate to patient care.
For the vast majority of organizations, partnering with a specialized vendor is the smarter, faster path forward. You get instant access to proven technology and deep industry expertise. Models like AI Automation as a Service let you tap into that expertise immediately, so you can focus on what you do best: taking care of patients.
Ready to turn your automation strategy from an idea into a reality? Ekipa AI delivers the expertise and tools to help you identify high-impact opportunities and execute them with confidence. Get your Custom AI Strategy report in 24 hours and speak with our expert team to reinforce your strategy.