Healthcare Systems Integration Strategy: A Future-Proof Guide
Discover how the healthcare systems integration strategy aligns data standards like FHIR, automates workflows with AI, and ensures compliance.

Having a solid healthcare systems integration strategy isn't just a nice-to-have anymore; it's essential for staying competitive and delivering quality care. Think of it as the blueprint for connecting all your different software, data streams, and daily workflows into a single, cohesive ecosystem. The entire point is to finally break down those frustrating data silos, smooth out operations, and give your teams the tools they need to improve patient outcomes. From foundational AI solutions to advanced automation, a connected system is the starting point for true innovation.
Why Modern Healthcare Demands Integrated Systems
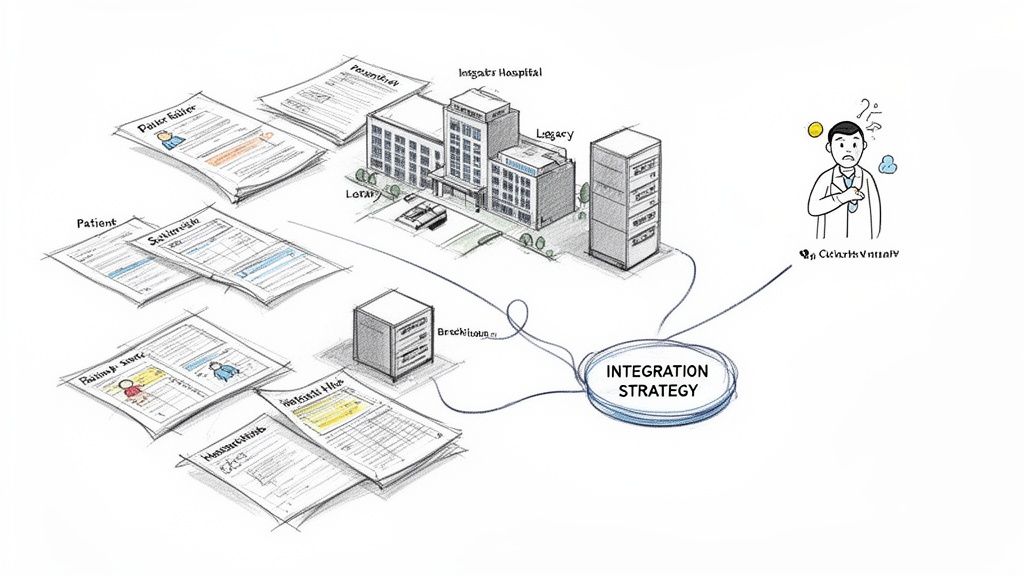
Let's be honest. Disconnected patient data, creaky legacy systems, and clunky manual processes aren't just minor headaches. They're real threats to patient safety, operational efficiency, and your ability to innovate. The ground is shifting in healthcare, and organizations are realizing that a thoughtful healthcare systems integration strategy is a core business function, not just an IT project. As we explored in our AI adoption guide, having a solid data foundation is the first step toward meaningful digital transformation.
The market is certainly reflecting this urgency. Valued at USD 3.95 billion, the global healthcare integration market is expected to more than double, hitting USD 7.96 billion by 2032. This explosive growth is largely fueled by the massive adoption of electronic health records (EHRs) and the desperate need to make sense of all that fragmented information. You can dig deeper into these numbers in the full research on the healthcare integration market.
To build a modern integration plan, it's helpful to break it down into its core pillars. Each one addresses a critical part of the puzzle, from the underlying technology to the ultimate business goals.
Pillars Of A Modern Integration Strategy
| Pillar | Core Objective | Key Technologies and Standards |
|---|---|---|
| Data Interoperability | Ensure seamless, secure data exchange between disparate systems (EHR, LIS, PACS, etc.). | FHIR, HL7, DICOM, APIs |
| Workflow Automation | Eliminate manual tasks, reduce errors, and accelerate clinical and administrative processes. | RPA (Robotic Process Automation), BPM (Business Process Management) |
| Patient Engagement | Provide patients with unified, on-demand access to their health data and care team. | Patient Portals, Mobile Health Apps, Telehealth Platforms |
| Security & Compliance | Protect sensitive patient health information (PHI) across all connected systems. | HIPAA, GDPR, Encryption, Access Controls |
| Analytics & AI | Convert integrated data into actionable insights for better decision-making and innovation. | Data Warehouses, Machine Learning Models, Predictive Analytics |
These pillars aren't just technical checklists; they represent a strategic shift in how a healthcare organization operates, with data flowing freely and intelligently to where it's needed most.
The Driving Forces Behind Integration
So, what’s really pushing this change? A few powerful forces are compelling healthcare leaders to prioritize connectivity. If you're building a business case for this kind of investment, these are your key talking points.
- The Shift to Value-Based Care: The old fee-for-service model is fading. Now, providers are rewarded for patient outcomes, not just the number of procedures. You can’t succeed in this model without a 360-degree view of the patient, and that’s impossible when your billing, clinical, and pharmacy systems don't talk to each other.
- Rising Patient Expectations: People are used to seamless digital experiences from banking and retail, and they now expect the same from their healthcare providers. They want to book appointments online, view their own records, and communicate easily. None of that happens without tightly integrated backend systems.
- Operational Strain from Consolidation: As health systems grow through mergers and acquisitions, they often inherit a messy patchwork of different technologies. Without a deliberate integration plan, this just creates a massive operational tangle, leading to wasted time, frustrated staff, and clinician burnout.
Key Takeaway: Integration has moved out of the server room and into the boardroom. It's a strategic response to fundamental changes in how healthcare is delivered, paid for, and experienced. The goal is to create a data-fluid environment that supports smarter clinical decisions and leaner operations.
The Regulatory Push for Interoperability
Government mandates are also a huge catalyst. For instance, understanding the impact of healthcare HIPAA Privacy Rule on data practices is foundational. Beyond that, regulations like the 21st Century Cures Act in the U.S. now actively penalize "information blocking" and legally require providers to give patients easy electronic access to their own health information. Simply put, compliance is impossible without robust integration.
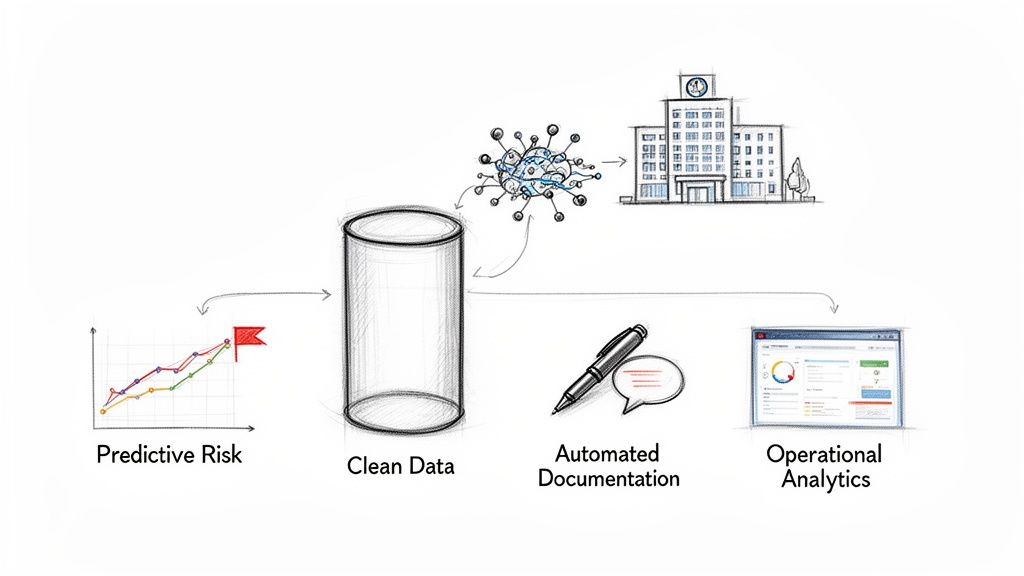
This newly accessible data then becomes the fuel for incredible innovation. Once your systems are connected, you create the clean, reliable data foundation needed for more advanced technologies. This is where modern Healthcare AI Services come in, enabling things like predictive analytics for at-risk patients, automation of tedious administrative work, and truly personalized care plans. The ultimate goal isn't just to connect data—it's to use it intelligently.
Building Your Strategic Integration Framework
A powerful healthcare systems integration strategy starts with a clear plan, not a purchase order for new software. Before you even think about the technical details, your leadership team needs to get together and define what success actually looks like—both for the business and for your clinical teams. This foundational work ensures every dollar and every hour you invest is tied directly to meaningful outcomes. Our AI strategy consulting services are designed to guide organizations through this critical planning phase.

This initial planning stage is where so many initiatives stumble. It's easy to get caught up in the tactical goal of connecting System A to System B, but the real question you have to answer is why. The most successful projects I've seen always begin by defining goals that resonate with everyone from the C-suite to the frontline staff. For organizations looking for a structured way to tackle this crucial step, our Custom AI Strategy report can provide a solid path forward.
Defining Your Goals and KPIs
Your objectives need to be much bigger than technical metrics like API uptime or data transfer speeds. While those things are important, they're just the plumbing. The real focus should be on KPIs that directly reflect tangible improvements in care delivery, patient experience, and operational efficiency.
Try framing your goals around real-world outcomes:
- Boost Clinical Excellence: Aim to reduce patient readmission rates by 15% within 18 months by giving care teams a single, unified patient history right at the point of care.
- Improve Operational Efficiency: Target a 20% reduction in patient check-in time by automating the data flow between the patient portal and the EHR. No more manual entry.
- Strengthen Financial Health: Set a goal to decrease claim denials by 25% through real-time insurance verification, powered by integrated billing and clinical systems.
These goals are specific, measurable, and they clearly spell out the business value of integration. They also give you a clear benchmark to measure ROI, which makes justifying the investment a whole lot easier.
Mapping Your Stakeholders
Integration is a team sport, and it touches nearly every single department in a healthcare organization. One of the most common and costly mistakes I see is failing to get buy-in from key stakeholders early on. You have to be proactive and map out everyone who will be affected by—or can influence—the project.
Your stakeholder map has to include:
- Clinical Staff: The physicians, nurses, and specialists who will be using the integrated data every day. Their feedback on workflow design is absolutely non-negotiable.
- IT and Data Teams: These are the architects and builders. They need to understand the clinical goals inside and out to design the right technical solution.
- Administrative Leaders: Department heads in billing, scheduling, and operations depend on accurate data to manage their resources. They need a seat at the table.
- Compliance and Security Officers: These are the guardians of your patient data. They must be involved from day one to ensure the entire framework is built to meet HIPAA and other critical regulations.
When you bring these groups in from the very beginning, the project stops being an "IT initiative" and becomes a shared organizational mission. This kind of collaborative approach is a cornerstone of a well-structured AI Product Development Workflow, which is designed to manage exactly these kinds of complex, multi-stakeholder projects.
Mastering Data Governance and Interoperability Standards
At the heart of any integration strategy is the data itself. You have to establish crystal-clear rules for data governance—defining who can access, modify, and use information across your entire ecosystem. This is the only way to guarantee data quality, consistency, and security.
Just as important is choosing the right interoperability standard. For years, HL7v2 was the reliable workhorse of healthcare data exchange. But the future is, without a doubt, centered on FHIR (Fast Healthcare Interoperability Resources).
FHIR isn't just a simple update; it's a completely different way of thinking. It uses modern web standards (like the APIs that power your favorite smartphone apps), which makes it far more flexible, developer-friendly, and scalable than anything that came before it. For any new integration project, FHIR should be your default choice.
The industry has firmly thrown its weight behind this shift. In fact, over 90% of EHR vendors worldwide now support FHIR as the baseline for data exchange, creating a critical tipping point. This momentum, spurred on by regulations like the 21st Century Cures Act, is why the global healthcare IT integration market is projected to skyrocket from USD 5.9 billion to USD 16.58 billion by 2034. You can discover more insights about these integration trends on Talencio.com.
Adopting FHIR isn't just about checking a compliance box; it's about future-proofing your entire digital infrastructure and getting it ready for the next generation of healthcare innovation.
Designing a Future-Proof Integration Architecture
Once you’ve settled on your strategic goals, it’s time to get into the technical weeds and design the backbone that makes it all possible. The architecture you land on will dictate your organization's agility, how well you can scale, and whether you're ready for what's coming next in technology. A smart healthcare systems integration strategy is about more than just hooking up systems; it's about building a flexible foundation for real, sustained innovation.
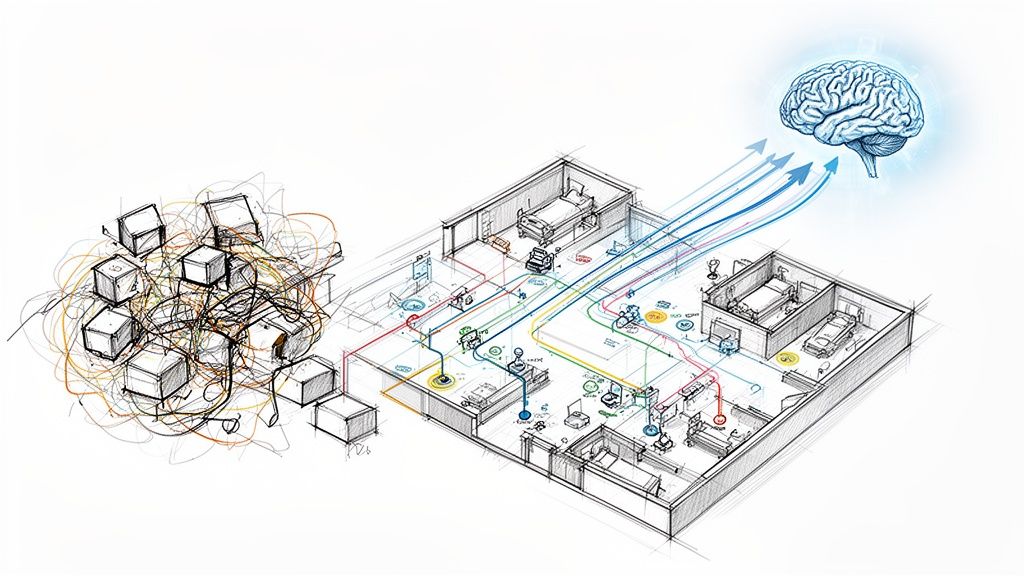
For years, healthcare has been stuck with two common but clumsy models. The first is point-to-point integration, where every system is directly wired to every other system it needs to talk to. It seems simple at first, but it quickly devolves into a tangled, brittle "spaghetti architecture" that's a nightmare to maintain and update.
Then there's the hub-and-spoke model. This was a step up, using a central engine as a go-between. It’s definitely more organized, but it introduces a massive single point of failure. If that central hub goes down or needs an upgrade, everything grinds to a halt.
Moving to a Modern, API-First Approach
Today, a modern, API-first architecture is the way to go. It’s simply a more resilient and scalable way to operate. Instead of those rigid, hard-coded connections, this approach uses Application Programming Interfaces (APIs) to open up data and functions in a secure, standardized way. Think of APIs as controlled gateways that let different applications communicate without needing to know the messy details of how the other system works.
For a healthcare organization, this shift pays off in a few key ways:
- Agility: Need to connect a new patient-facing app or a third-party telehealth platform? You can plug it into existing APIs quickly and securely. No more massive, months-long projects for simple connections.
- Scalability: An API-led architecture is decentralized by nature. You can scale individual services on their own without bringing down the whole network—a must-have for any growing health system.
- Innovation: When you expose data through secure APIs, you empower your own developers and even trusted partners to build new tools. This is how you get everything from custom analytics dashboards to advanced AI tools for business.
An API-first strategy isn't just a tech decision. It’s a business decision to build a more adaptable organization. It sets you up to bring in emerging tech, from remote patient monitoring devices to AI algorithms, with minimal friction.
The Inevitable 'Build vs. Buy' Decision
With a clear architectural vision, you’ll hit the classic fork in the road: do you build your own integration solutions or buy an off-the-shelf platform? There’s no single right answer here. It comes down to your organization’s specific needs, your team’s technical firepower, and your long-term roadmap.
Buying a commercial platform can get you moving faster with pre-built connectors for common systems like EHRs. The downside? Customization can be a real pain (and expensive), and you can find yourself locked into one vendor's ecosystem.
On the other hand, building custom solutions gives you total control and flexibility to match your unique workflows. This is often the best path when you have highly specialized needs, but it demands serious in-house talent or a great partner who provides custom healthcare software development.
Many health systems find a happy medium. They use a platform for the common, straightforward integrations and build custom APIs for the proprietary workflows that give them a competitive edge. Running a thorough AI requirements analysis can shed light on which path offers the best return for what you’re trying to achieve.
Setting Your Non-Negotiable Security Guardrails
No matter what you build or buy, security and compliance have to be baked in from the very beginning. In healthcare, a data breach isn't just a financial problem—it's a fundamental breakdown of patient trust that can be impossible to repair. Your risk management plan needs to be aggressive and proactive.
Here are the absolute must-haves:
- HIPAA and GDPR Compliance: Every single data flow, API call, and connection must be bulletproof when it comes to patient data regulations. No exceptions.
- Data Encryption: Patient data must be encrypted always—both in transit (while moving between systems) and at rest (when it's sitting in a database).
- Identity and Access Management (IAM): Implement strict, role-based controls. Only authorized people should be able to access specific data, and only the data they absolutely need (the principle of least privilege).
- Regular Security Audits: Don't set it and forget it. You need to be constantly testing your infrastructure for weak spots through penetration testing and security audits to stay ahead of the bad guys.
Putting together a secure, future-proof architecture is a heavy lift, but it’s the most critical technical decision you'll make in your healthcare systems integration strategy. This is the foundation that every future digital health initiative will stand on.
Putting the Plan in Motion: A Phased Roadmap for Integration
A great strategy on paper is just that—paper. The real test comes when you start turning that blueprint into a functioning, adopted reality. For a healthcare systems integration strategy to succeed, it needs a smart, phased implementation that prioritizes projects, manages the human side of change, and shows value quickly.
Don't even think about a "big bang" rollout where everything changes overnight. That's a surefire way to invite chaos and user revolt. Instead, the most successful projects prioritize initiatives based on a simple matrix: impact versus effort. Start with the quick wins—the high-impact, low-risk projects that build momentum and get people excited.
A perfect first project might be linking the patient portal to the scheduling system for automated appointment reminders. It's a tangible benefit for patients and a time-saver for admin staff. Crucially, it doesn’t mess with core clinical workflows, but it proves the concept works and gets you that all-important early buy-in.
Designing a Practical Rollout Plan
A structured, sequential rollout is your best defense against risk. Think of it as a series of connected projects, where each success paves the way for the next.
Phase 1: Build the Foundation (Months 1-3). Your first move is to stabilize the core data sources. This is where you connect the main EHR to the lab information system (LIS), finally getting rid of manual order entry. The immediate goals here are all about internal efficiency and making sure the data is right.
Phase 2: Lighten the Load (Months 4-9). Now, introduce integrations that directly help your clinical staff. Think about automating prior authorizations with an AI tool or using natural language processing to summarize physician notes. These are solutions that give time back to clinicians and are often powered by better internal tooling.
Phase 3: Focus on the Patient (Months 10-18). With the internal plumbing sorted, you can roll out tools that directly improve the patient experience. This could be an integrated billing portal that makes sense or telehealth services that pull patient history directly from the EHR without any manual input.
Phase 4: Unlock Advanced Insights (Months 19+). Once you have a rich, integrated dataset, the real fun begins. You can finally deploy predictive models for population health management, optimize hospital bed allocation, and explore more sophisticated AI-driven solutions.
This journey from basic wiring to advanced intelligence is a common one, and it's reflected in how integration architecture has matured over the years.
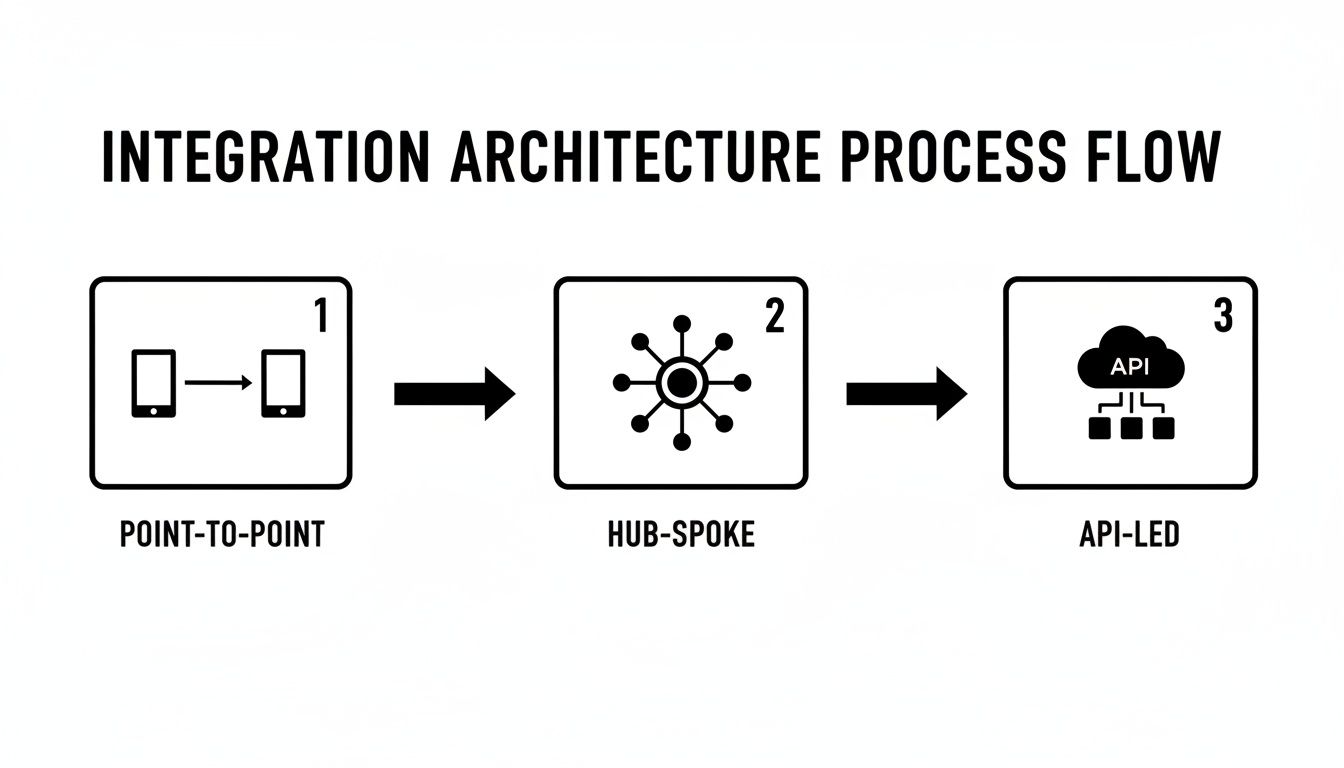
You can see the evolution from tangled, one-off connections to a much cleaner, more flexible API-led approach that allows you to add and change services without breaking everything else.
Don't Forget the People Behind the Screens
Technology is only half the battle. The other, much trickier half is change management. You can build the most elegant system imaginable, but if your clinicians and staff won't use it, the project is a failure. Period.
Overcoming resistance starts with clear communication, hands-on training, and genuine empathy for the teams whose day-to-day work is about to be upended. Frame every change around the benefits they actually care about, like "spending less time on paperwork" or "getting a complete patient history in seconds."
This has never been more critical. The trend of healthcare consolidation is accelerating, with over 2,000 hospital mergers between 1998 and 2023. These newly formed systems are forced to stitch together different technologies and cultures. With 41% of U.S. physicians now working in hospital-owned practices, the need for platforms that can sync clinical and financial data is no longer a luxury—it's a requirement for survival.
My Two Cents: Never underestimate the power of your "super-users." In every department, there are a few tech-savvy people who are curious and respected by their peers. Find them early. Involve them in the design and testing. They will become your most passionate advocates and effective trainers when it's time to go live.
Ultimately, execution is a mix of solid project management and thoughtful leadership. A well-managed rollout that respects the human element is what delivers a real return on investment and creates a foundation for continuous improvement. If you're managing a complex rollout, our expert team can provide hands-on implementation support.
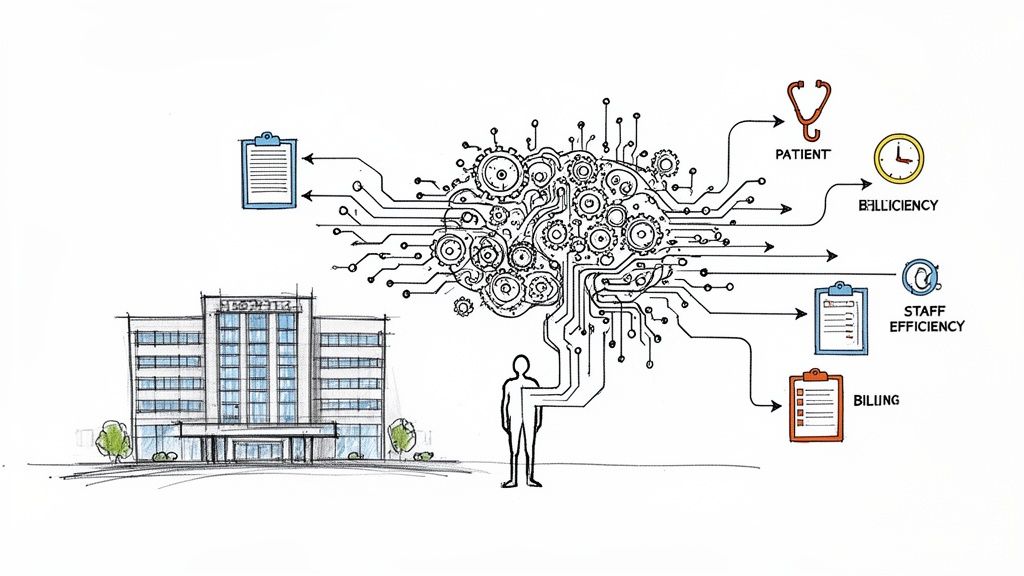
Where AI Fits In: From Connected Data to Intelligent Care
Let's be clear: the whole point of integration isn't just to make IT systems talk to each other. The real prize is creating a clean, reliable stream of data that can power genuinely innovative tools, especially artificial intelligence. This is the ultimate payoff—shifting from a reactive mode of managing data to a proactive one where you can predict patient needs, automate soul-crushing administrative tasks, and fundamentally improve care delivery.
I've seen too many ambitious AI projects stall or fail outright for one simple reason: bad data. If your data is siloed, messy, and inconsistent, any machine learning model you build on top of it will be unreliable at best. A solid integration foundation isn't optional for AI; it's the price of entry.
Turning Connected Data into Predictive Power
Once your data is flowing freely between systems, you can start tackling some of healthcare's biggest headaches with AI. The potential goes way beyond simple efficiency gains.
Here are a few high-impact, real-world use cases I've seen work:
Predicting High-Risk Patients: AI models can comb through integrated EHR, claims, and lab data to flag patients at high risk for sepsis, heart failure, or hospital readmission. This allows care teams to step in before a crisis hits, which is a game-changer for both patient outcomes and costs.
Killing Clinical Documentation Burden: Physician burnout is real, and the endless charting is a primary cause. AI-powered ambient clinical intelligence tools can listen to a patient visit and automatically draft the clinical note. This frees up physicians to actually look at their patients instead of their keyboards.
Optimizing Hospital Operations in Real-Time: Imagine an AI that analyzes live data from your scheduling systems, bed management software, and staffing rosters. It can predict ER wait times, optimize OR schedules on the fly, and prevent patient bottlenecks before they happen.
These aren't science fiction. They are practical applications being used today. The common denominator is that none of them work without the clean, structured data that a well-designed integration strategy provides.
Why Governance Is Non-Negotiable for AI
As you start rolling out AI, you absolutely need a clear governance plan. This is about more than just the tech; it's about ensuring fairness, transparency, and accountability. A solid framework for Artificial Intelligence Governance helps build trust with clinicians and patients, which is critical for adoption.
My Takeaway: Think of integration as building the plumbing. The goal isn't just to have connected pipes; it's to create an intelligent healthcare ecosystem where data works for you—automating tasks, anticipating needs, and giving your teams the insights they need to deliver exceptional care.
This is where a dedicated AI Automation as a Service platform can be a massive accelerator. Once the data foundation is solid, you can plug in solutions to automate everything from prior authorizations to medical coding, drastically cutting down on administrative waste.
Building a Smarter, Proactive System
The long-term vision is a healthcare system that actually learns and gets better over time. Your integrated data feeds AI models, those models generate insights, and those insights help you refine clinical protocols and operational workflows. It’s a continuous feedback loop.
This is how you graduate from practicing medicine based on what happened yesterday to delivering care that is predictive, personalized, and proactive.
Getting there is a journey. It takes strategic planning, deep technical skill, and a real-world understanding of how healthcare actually works. Your healthcare systems integration strategy is the non-negotiable first step on that path.
Measuring Success and Planning Your Next Move
So, you’ve connected the systems. The hard part is over, right? Not quite. The real work starts now: proving that your integration strategy is actually delivering value. This is where you shift from building to measuring.
You need a dashboard of metrics that tells the whole story, not just the technical one. Sure, API uptime and data sync speeds are important, but they don't mean much to your CFO or Chief of Medicine. You have to connect the dots between the technology and tangible business results.
Key Metrics for Your Integration Dashboard
Think about what truly matters to your organization. Your metrics should reflect the initial goals you set out to achieve.
- Operational Efficiency: Are you seeing a real drop in manual data entry? Are patient wait times decreasing? Are lab results getting to clinicians faster? These are the numbers that get your administrative leaders excited.
- Clinical Outcomes: This is where the rubber meets the road. Track improvements in core clinical benchmarks, like a reduction in 30-day hospital readmission rates or better adherence to chronic care plans.
- Patient Satisfaction: Look at your patient portal adoption rates and satisfaction scores. A seamless digital experience should make healthcare easier and more accessible for patients, and these numbers will tell you if you're succeeding.
- Financial Health: Keep a close eye on the bottom line. Are you seeing fewer claim denials because of better data accuracy? Is the overall cost per patient episode going down?
Success isn't a static destination. It’s a dynamic process of listening, learning, and adapting. Your best source of truth is the people on the front lines.
Create formal feedback loops with your clinical and administrative staff. They'll be the first to tell you what’s working, what’s not, and where the next big opportunity for improvement lies.
This agile approach is what keeps your strategy relevant. New technologies and shifting regulations will always be part of the landscape. Your goal is to build an ecosystem that can evolve without needing a complete overhaul every few years.
Navigating this complex journey requires deep expertise in both technology and healthcare workflows. By partnering with specialists, you can turn a theoretical integration plan into scalable, measurable business impact. Discover how our expert team helps organizations like yours build future-proof healthcare systems.
Frequently Asked Questions (FAQ)
What is the primary goal of a healthcare systems integration strategy?
The main goal is to create a seamless, interconnected ecosystem where patient data and operational information flow freely and securely between different systems (like EHRs, billing software, and lab systems). This breaks down data silos, improves clinical decision-making, streamlines workflows, enhances patient care, and reduces administrative costs.
Why is FHIR (Fast Healthcare Interoperability Resources) so important?
FHIR is a modern data standard that uses web-based APIs, making it easier, faster, and more flexible to exchange healthcare information. Unlike older, more rigid standards, FHIR is developer-friendly and supports real-time data access, which is crucial for modern applications like mobile health apps, patient portals, and AI-driven analytics.
What are the biggest challenges in implementing a healthcare integration strategy?
The biggest challenges often include:
- Technical Complexity: Dealing with legacy systems that weren't designed to connect with others.
- Data Governance: Ensuring data quality, security, and privacy (especially HIPAA compliance) across all connected systems.
- Change Management: Gaining buy-in from clinical and administrative staff and training them on new workflows.
- Cost: The significant investment required for new platforms, custom development, and skilled personnel.
Should we build our own integration solution or buy a commercial platform?
This depends on your organization's specific needs, budget, and in-house technical expertise.
- Buying a platform is often faster and leverages pre-built connectors for common systems.
- Building a custom solution offers maximum flexibility to fit unique workflows but requires significant technical resources. Many organizations use a hybrid approach, buying a platform for standard integrations and building custom solutions for specialized, high-value processes.
Ready to build an AI-powered healthcare ecosystem? The Ekipa AI team can help you design a future-proof integration strategy that delivers measurable results. Start your journey with our AI Strategy consulting tool.