A Guide to Clinical Productivity Improvement in Healthcare
Discover how to approach clinical productivity improvement with AI. Our guide covers workflow audits, AI use cases, and deployment strategies for real results.

The phrase clinical productivity improvement can sound cold, almost like something you’d hear on a factory floor. In healthcare, that just feels wrong. But the reality is much more human. It’s about building a smarter, more supportive environment so clinicians can pour their energy into what they do best: delivering high-quality patient care.
It’s Not Just About the Numbers
Healthcare today is caught in a perfect storm. We’re dealing with crippling staff shortages, epidemic levels of clinician burnout, and an administrative burden that feels like quicksand. These aren’t just buzzwords; they’re daily realities that directly harm patient outcomes, crush team morale, and threaten the financial health of entire organizations.
A huge part of the problem comes down to inefficient workflows. When you have highly skilled clinicians spending huge chunks of their day wrestling with paperwork, it creates a cascade of problems. This isn’t just a feeling; it’s a systemic breakdown.
The True Price of Inefficiency
It’s no surprise that operational efficiency is top-of-mind for healthcare leaders everywhere. In fact, over 70% of C-suite executives see productivity gains as a critical priority. The numbers tell a grim story: nurses often lose 15% to 28% of their shift to low-value tasks, while some ICU doctors spend as little as 15% to 30% of their time in direct patient care. The rest? It's swallowed by documentation and administrative duties. For a deeper dive, check out the global healthcare outlook from Deloitte's 2025 report.
This administrative overload triggers a chain reaction of critical issues:
- Slower Patient Flow: When processes lag, fewer patients can be treated. This means longer wait times and, ultimately, delayed care.
- Accelerated Clinician Burnout: Mind-numbing, repetitive tasks are a massive source of stress and dissatisfaction, pushing good people out of the profession.
- Skyrocketing Operational Costs: Wasted time is wasted money. It hits everything from staffing budgets to the way supplies are managed.
To really get a handle on this, you have to look past the surface-level metrics and focus on establishing baseline metrics for continuous improvement.
The goal isn’t to make clinicians work faster. It’s to clear the roadblocks that stop them from working smarter. Real productivity improvement is about giving them back their time to focus on patients.
A Fresh Take on a Stubborn Problem
In this new era, especially with the shift to value-based care, strategic improvements aren't just nice-to-haves—they're essential for survival. This is where smart AI solutions can make a massive difference by tackling these deep-rooted inefficiencies head-on. Our Healthcare AI Services are designed to do just that.
Imagine automating documentation or optimizing complex schedules. The right technology can hand back precious hours to your clinical team. Making this shift happen, though, requires a clear plan, starting with a solid AI strategy consulting framework. Once you grasp the real stakes and the opportunities in front of you, your organization can start making meaningful, sustainable improvements.
Auditing Your Clinical Workflows to Find Hidden Bottlenecks
You can't fix what you can't see. Before you even think about new technologies or overhauling processes, you have to start with an honest, clear-eyed look at how things actually work right now. A thorough clinical workflow audit isn't just a box to check; it’s the essential first step toward making any real, lasting improvements to your clinical productivity.
The goal here is to map your core operations from end to end. Think about it: from the second a patient first contacts you to schedule an appointment, all the way through their visit, follow-up, and the final billing cycle. We're on a mission to find the hidden bottlenecks, the redundant steps, and the administrative black holes that are secretly draining your team's time and your organization's resources. Essentially, you're building a 'productivity heatmap' to pinpoint exactly where the friction is.
This visual shows a story we see all the time: administrative overload snowballs, leading directly to staff burnout. It also shows where targeted interventions can break that cycle.
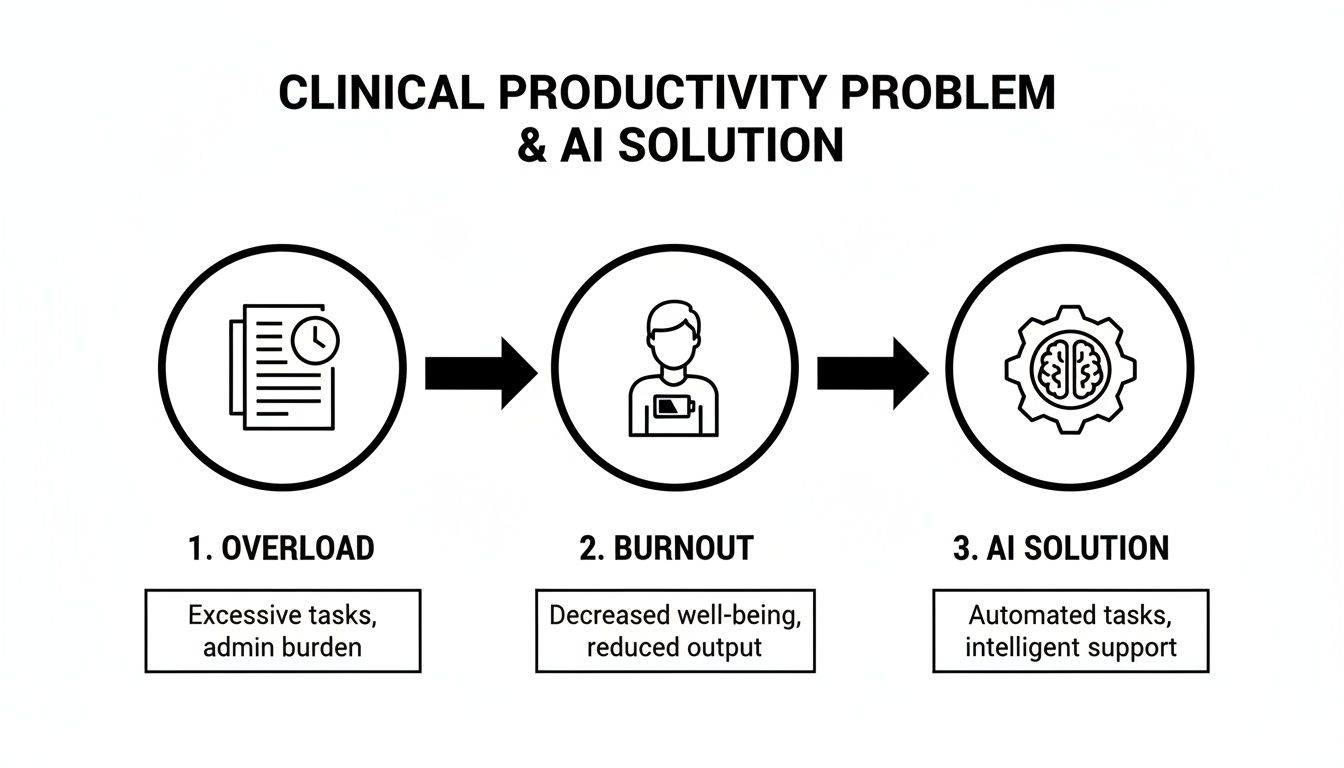
Without a strategic fix, these mounting inefficiencies are a direct line to the exhaustion and high turnover rates that are unfortunately so common in healthcare today.
Combining Hard Data with Human Experience
A truly effective audit isn't just about spreadsheets and metrics. It’s a blend of hard numbers and real human experience. You absolutely need both to get the full story.
Quantitative Data gives you the objective proof of where time is being lost. Start by tracking key metrics like:
- Patient Wait Times: How long are patients really waiting at each step? From check-in to seeing the clinician, to checkout.
- Documentation Hours: What slice of a clinician's day is eaten up by EHR data entry? We've seen this consume a shocking amount of time, which directly cuts into available appointment slots.
- Billing Cycle Length: How many days does it take to get from service delivery to final payment?
- Appointment No-Show Rates: What percentage of your scheduled visits are simply missed? This is a huge indicator of friction in your scheduling and communication process.
On the other side of the coin, Qualitative Feedback gives you the "why" behind those numbers. This is where you have to talk to your people on the front lines—the nurses, physicians, schedulers, and billers who are living these workflows day in and day out. Things like anonymous surveys, one-on-one chats, and quick team huddles are goldmines for capturing their frustrations and, more importantly, their brilliant insights.
I've found that the biggest opportunities for improvement are almost always hiding in plain sight. They're the daily workarounds and frustrations that only the staff who navigate those broken processes know about. Their feedback isn't just helpful—it's absolutely essential.
Categorizing Clinical Workflow Inefficiencies
As you start collecting all this information, you'll begin to see patterns. The next move is to organize these findings so you know where to focus your energy first. A structured approach is key for anyone trying to improve healthcare operational efficiency.
This table provides a simple but effective framework for classifying the bottlenecks you uncover.
Categorizing Clinical Workflow Inefficiencies
A framework to help identify and classify common bottlenecks in clinical operations, enabling targeted improvement efforts.
| Inefficiency Category | Description | Common Examples | Potential Impact Area |
|---|---|---|---|
| Administrative Burden | Non-clinical tasks that eat up clinician time but add little to no value to patient care. | Endless manual data entry, prior authorizations, bloated charting requirements, referral management. | Staff Burnout, Patient Throughput |
| Communication Gaps | Breakdowns in how information flows between departments, different clinicians, or with patients. | Delayed lab results, messy patient handoffs, scheduling mix-ups, poor care coordination. | Patient Safety, Operational Costs |
| Process Redundancies | Unnecessary or duplicated steps in a workflow that just waste time and create frustration. | Asking a patient for the same information multiple times, re-keying data into different systems. | Staff Frustration, Wasted Resources |
| Technology Friction | Clunky, slow, or poorly integrated software that gets in the way of clinical work instead of helping it. | Hard-to-navigate EHRs, systems that don't talk to each other, painfully slow system performance. | Clinician Satisfaction, Data Accuracy |
By classifying problems this way, you move from a vague feeling that "things are inefficient" to a concrete list of problems that you can actually solve.
This audit becomes your strategic roadmap. It points you toward targeted solutions, whether that's redesigning a process or bringing in smart automation. For a deeper dive, our guide on https://www.ekipa.ai/workflow-automation can show you how to start tackling these challenges head-on, creating a much smarter and more efficient environment for your entire team.
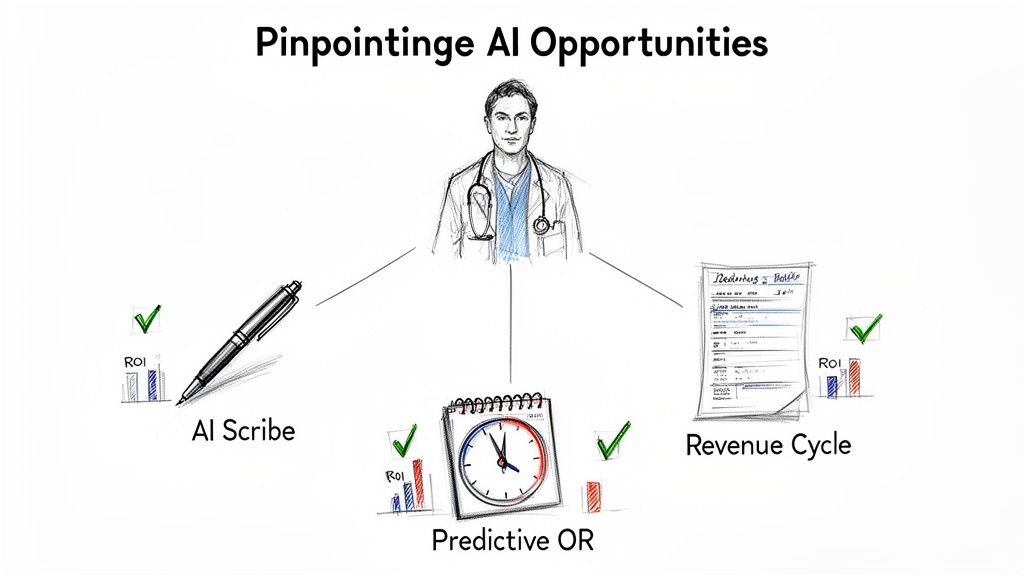
Pinpointing High-Impact AI Opportunities
Alright, so you’ve done the hard work of auditing your clinical workflows. You're no longer guessing—you have a clear map of where things get bogged down and what's causing friction for your staff. Now comes the exciting part: turning that insight into action. The goal isn't to chase every shiny new AI tool but to strategically pick the ones that will make a real difference to your clinical productivity.
The key is to move past the hype. Don't just ask, "Can AI do this?" The much better question is, "Should AI do this for us, right now, in this specific context?" This mindset shift is what separates the successful projects from the expensive failures.
A Vetting Framework for AI Use Cases
You probably have a long list of potential pain points to solve. To narrow it down to a focused project pipeline, you need a practical filter. I've found that running every idea through these three lenses helps prioritize what truly matters.
- Return on Investment (ROI): This is about more than just money. Yes, you need to consider direct financial gains from cost savings or new revenue streams. But don't forget the softer, equally important returns, like boosting staff morale, reducing burnout, or improving patient satisfaction scores.
- Implementation Feasibility: How hard is this really going to be to get off the ground? Think about the technical lift, especially how it will integrate with your existing EHR. You also need to be honest about the resources—time, budget, and people—that you can realistically dedicate to the project.
- Strategic Alignment: Does this initiative push your organization's bigger goals forward? A tool that shaves a few seconds off a minor admin task is nice, but it's far less valuable than one that directly contributes to better patient outcomes or helps you retain top clinical talent.
A common trap is getting drawn to the low-hanging fruit—the technically "easy" projects that don't actually move the needle on your strategic goals. The sweet spot is always a high-impact, strategically aligned solution that is genuinely feasible to implement.
Real-World Examples Beyond the Hype
Let's ground this in reality. Forget the futuristic concepts for a moment and look at what’s working right now to solve tangible problems in clinics and hospitals.
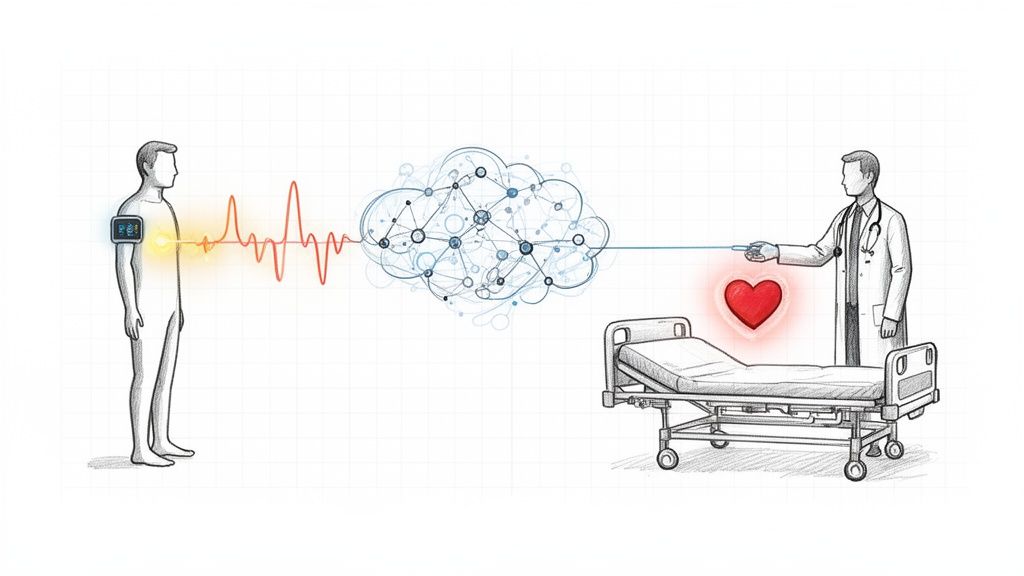
- AI-Powered Scribes: We all know documentation is a massive driver of clinician burnout. AI scribes are no longer a novelty; they're a necessity. These tools listen in on a patient visit and draft the clinical note automatically. This one change can literally give hours back to your clinicians every week.
- Predictive Analytics for Scheduling: An empty OR or a chaotic, overbooked clinic is just burning money and stressing everyone out. AI can analyze historical appointment data, patient no-show rates, and even local events to build smarter schedules that maximize room utilization and slash patient wait times.
- Automated Revenue Cycle Management (RCM): Denied claims and coding errors are a huge administrative drain. AI tools can now scrub claims for mistakes before they're submitted, suggest the right billing codes, and even help manage the denials process, which gets you paid faster and with fewer headaches.
Tackling Workforce Shortages with AI Analytics
This isn't just about efficiency; it's about survival. The healthcare industry is facing severe labor gaps, and AI is becoming a critical tool for managing the workforce you have.
Predictive analytics can forecast patient demand, helping you staff appropriately for peak times without being overstaffed during lulls. It’s a game-changer. By automating repetitive tasks, AI is already freeing up 20% more nurse-patient time. And we're seeing real adoption: ambient AI for automated note-taking is now used in 28% of medical groups.
Ultimately, identifying the right opportunities comes down to connecting the dots between the biggest frustrations you uncovered in your workflow audit and the proven AI tools available today. It’s about being methodical. For instance, our Clinic AI Assistant was specifically designed to handle many of these administrative burdens. By taking a structured, evidence-based approach, you can turn that list of operational headaches into a focused project plan that delivers genuine results.
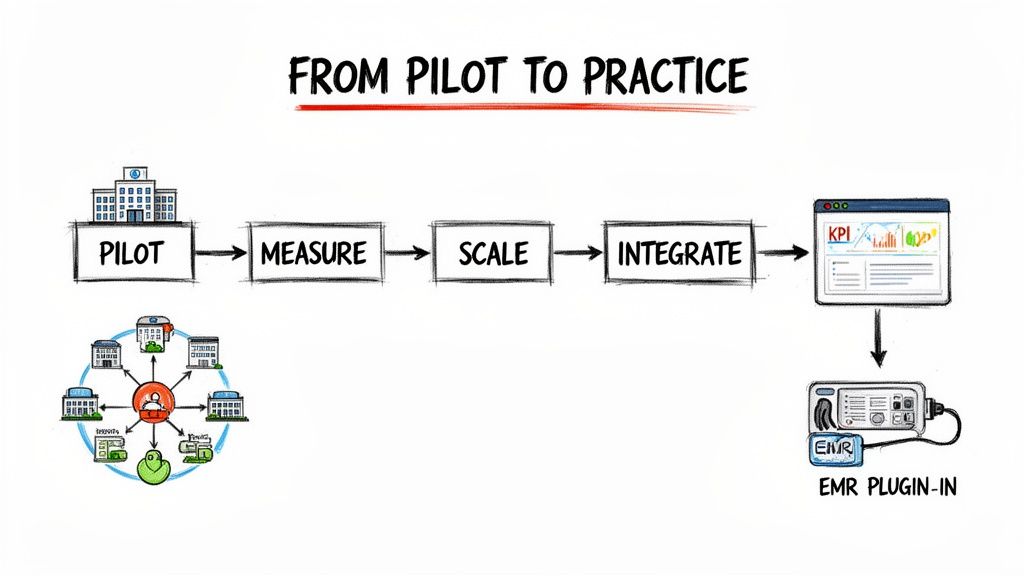
From Pilot to Practice: A Deployment Guide
Having a great idea is one thing; bringing it to life in a busy, high-stakes clinical environment is an entirely different beast. This section is your field guide to designing, piloting, and rolling out productivity solutions—without causing chaos or getting in the way of patient care. A thoughtful, structured approach is the only way to turn a promising concept into a tool your team actually uses and values.
One of the first forks in the road you'll hit is the classic "build vs. buy" decision. Building a custom solution gives you something that fits your unique workflows like a glove, but it's a heavy lift, demanding serious time, money, and technical firepower. On the other hand, buying an off-the-shelf product gets you up and running faster, but you might have to bend your processes to fit its mold.
No matter which path you take, picking the right technology partner is make-or-break. You need a team that gets the nuances of healthcare, not just the code. Their experience with HIPAA, messy EMR integrations, and the realities of clinical life is non-negotiable.
The Art of the Pilot Program
My best advice? Start small. A pilot program is your controlled experiment. It's where you prove the solution's value, gather honest feedback, and build a groundswell of support before going all-in. It de-risks the entire project and helps you win over the skeptics.
A successful pilot needs a few key ingredients:
- A Laser-Focused Scope: Don’t try to boil the ocean. Pick one specific workflow or a single department to test your new solution.
- An Enthusiastic Crew: Find a small group of clinicians and staff who are genuinely open to change and willing to give you the good, the bad, and the ugly feedback. Their passion can be infectious.
- Clear Victory Conditions: How will you know if the pilot actually worked? Define your Key Performance Indicators (KPIs) before you even start.
Setting Clear KPIs and Defining Success
Your KPIs can't be fuzzy goals like "improve efficiency." They need to be specific and directly tied to the bottlenecks you found in your initial audit.
For instance, if you're piloting an AI scribe, you need concrete targets. Think in terms of:
- A 25% reduction in the time a clinician spends on EHR documentation per patient.
- An increase in patient throughput by 1.5 patients per clinician per day.
- A 15% improvement in clinician satisfaction scores related to administrative burdens.
Metrics like these give you hard data to show leadership the ROI and, just as importantly, to show your clinical team the real, tangible benefits of this new tool. Success isn't just about the numbers; it's about making their day-to-day work genuinely better.
A pilot isn't just a test of the technology; it's a test of the change. It's your chance to see how the solution holds up in the human-centric, often chaotic reality of clinical practice.
Planning for a Smooth Rollout
Once your pilot is a proven success, it's time to think bigger. A structured rollout plan ensures nothing gets missed. As you scale, our AI Product Development Workflow can provide a solid roadmap for navigating these complex projects.
One of the biggest technical hurdles you'll face is integrating the new tool with your existing Electronic Medical Record (EMR) system. This is where so many projects get stuck. A clunky, disjointed integration can create more headaches than it solves, leading to frustrated users and dismal adoption rates. This problem is so widespread that specialized services for custom healthcare software development have emerged just to build these crucial bridges between systems. Your deployment plan has to bake in enough time and resources to get this right.
Scaling Your Success and Managing Change
That successful pilot program feels great, doesn't it? It's a huge win, but it's really just the beginning. The real, lasting gains in clinical productivity come when you take those small victories and scale them across the entire organization. This is where you weave those new efficiencies into the very fabric of how you operate.
This is also where the real work of change management kicks in—a crucial step that, from my experience, is almost always underestimated.
Moving from a controlled pilot to a full-scale deployment means your focus has to shift. It's not about proving a concept anymore. Now, it's about making it work for everyone, in every department, every single day. That leap requires a solid game plan for communication, training, and governance to make sure your productivity gains stick around for the long haul.
Creating a Culture of Continuous Improvement
To make these changes last, your clinical staff need to be more than just users; they need to become advocates. This starts with clear, consistent communication that gets straight to the "why." Don't just give them a "how-to" manual. Show them exactly how these new processes will lighten their administrative load, give them more time with patients, and make their days less of a grind.
The fastest way to get buy-in is to show tangible results. When your clinicians see their colleagues from the pilot spending less time wrestling with paperwork and more time on actual patient care, they won't just accept the change—they'll start asking for it.
Set up simple feedback channels where staff can share what’s working, flag issues, and suggest tweaks. This creates a sense of shared ownership and turns what could feel like a top-down order into a team effort. When you make data-driven improvement an ongoing conversation, you build a culture where everyone feels responsible for making things better. As we've covered in our guide to AI adoption, this kind of inclusive approach is absolutely essential.
Governance and Maintenance for Long-Term Value
Once your new systems are live, the job isn't done. You need a rock-solid governance framework to keep your AI models and automated workflows accurate, secure, and fully HIPAA-compliant. In practice, this means a few key things:
- Regular Model Audits: AI isn't "set it and forget it." Models can drift as patient data or clinical protocols evolve. Schedule routine check-ups to make sure they're still accurate and free of bias.
- Clear Data Governance Policies: Spell out who can access what data, how it can be used, and who is responsible for keeping it clean and secure.
- Proactive Security Monitoring: Healthcare data is a magnet for cyberattacks. You need to be watching your systems constantly to protect patient information and maintain trust.
Let's be honest, the long-term maintenance for these systems can be a heavy lift for an internal team. This is where managed services can be a game-changer. Using a solution like AI Automation as a Service or getting expert support for your internal tooling ensures your systems stay current and perform at their peak, without burning out your IT staff.
Ensuring Your Productivity Gains Are Sustainable
The impact of these projects goes far beyond one clinic or department. Look at the pharmaceutical R&D world for a great example. Recent data shows a real jump in clinical productivity, with IQVIA's Clinical Program Productivity Index climbing to 11.7 from 10.9. A huge part of that was better success rates in Phase III trials, which in turn shortened development timelines and cut costs. You can dig into the specifics in IQVIA's full report on global R&D trends.
This shows how targeted improvements can send positive ripples across the entire healthcare system. By thoughtfully scaling your initiatives and focusing on the human side of change, you're not just installing new software. You're building a more resilient, efficient, and supportive workplace where both your clinicians and your patients can thrive. Our expert team is always here to help you navigate every step of this journey.
Frequently Asked Questions (FAQ)
Here are answers to some of the most common questions we get about improving clinical productivity with AI.
What is the best first step for clinical productivity improvement?
The most crucial first step is a brutally honest audit of your current workflows. Before you even look at new technology, you have to know your baseline. Map out key processes—patient intake, charting, billing—and pinpoint exactly where the delays and administrative drag are. A data-driven approach, mixed with direct feedback from your front-line staff, makes sure you're treating the disease, not just the symptoms. An AI requirements analysis can really help speed this up.
How do we get our clinical staff to adopt new AI tools?
Adoption comes down to three things: inclusion, value, and support. Involve clinicians from day one to ensure the tools solve their actual problems. Use a pilot to show them—don't just tell them—how it saves them time or eliminates tedious work. Then, back it up with great training and accessible, ongoing support. Real adoption happens when your team feels like the technology is working for them, not the other way around. Having an expert team to guide this change can make all the difference.
What kind of ROI can we realistically expect?
The ROI here is about more than just money. Yes, you'll see financial gains from optimized staffing, faster billing cycles, and lower administrative overhead. But the operational wins—like better patient throughput and shorter wait times—are just as important. And maybe the most critical return is on your people. AI tools for business that automate documentation can give back over 20% of a clinician's time, directly fighting burnout and letting them focus on what they do best: caring for patients. Exploring real-world use cases can show you what this looks like in practice.
Ready to turn these ideas into action? At Ekipa AI, we specialize in transforming complex clinical challenges into scalable results. Find out how our AI Strategy consulting tool can help you pinpoint and implement your highest-impact AI opportunities. For a more tailored analysis, ask us about creating a Custom AI Strategy report for your organization, and meet our expert team to learn how we can help.